SYNOPSIS
Objectives
Education has long been considered a protective factor against sexual risk behaviors and sexually transmitted infections (STIs) among adolescents; however, few have explored this association and determined differences across racial/ethnic groups of young adult females on a national scale. The purpose of this study was to (1) describe the association between education and STI diagnosis among a national sample of black and white young adult females and (2) examine racial differences in this association.
Methods
We used data from the National Longitudinal Study of Adolescent Health (Add Health) to assess the association between education and chlamydia, gonorrhea, and/or trichomoniasis (self-reported and assay-diagnosed) in 2001–2002 using logistic regression analysis.
Results
After adjustment for risk behaviors, education was inversely associated with any assay-diagnosed STI, but this association was nonsignificant among black women for self-reported STI. Additionally, black females enrolled in, or who graduated from, college had significantly higher predicted probabilities of having an STI (12.4% self-reported; 13.4% assay-diagnosed) compared with white females who had less than a high school diploma (6.4% self-reported; 2.3% assay-diagnosed).
Conclusions
Educational status was not uniformly protective against STIs for black and white females in this sample. Particularly for young black women, other factors may play a more prominent role in determining STI risk. Social determinants, such as education, should be viewed as important factors associated with STI prevalence, but their differential impact on various racial/ethnic groups should also be considered when addressing the disproportionate rates of STIs in the U.S.
With nearly 20 million cases occurring annually, sexually transmitted infections (STIs) continue to persist as a major public health issue in the United States. Half of these infections occur among adolescents and young adults aged 15 to 24 years, and of these, minority women are disproportionately affected.1 In 2007, three of the most common STIs—chlamydia, gonorrhea, and trichomoniasis—were significantly more prevalent among 20- to 24-year-old black females than among their counterparts of any other race/ethnicity. During this year, chlamydia rates among non-Hispanic black females were more than seven times that of white females, and rates for gonorrhea were nearly 15 times the rate of non-Hispanic white females of the same age, with rates for both infections on the rise from previous years. Although trend data for trichomoniasis are limited, data on initial physician visits suggest that rates may be on the decline.2
Despite these high rates of reported STIs, up to two times as many new infections are estimated to occur annually than are reported.2 As a result, many who suffer from STIs may do so for extended periods of time, enhancing the probability for other infections to occur. In fact, individuals who contract at least one STI are almost five times as likely to also contract human immunodeficiency virus (HIV). Additionally, STIs can have numerous lifelong health consequences, which can prove much more deleterious for women than for men.2–5 For STIs that go undetected, reproductive health effects for women can include infertility, cervical cancer, pelvic inflammatory disease, or possible STI transmission from mother to child during childbirth.3,6
The relationship between education and sexual risk has been studied extensively in the adolescent population;7–11 yet, the research on young adults often presumes education is a protective factor against risk outcomes or minimizes the role of key social determinants, such as education, on engagement in sexual risk behaviors and STI diagnosis. The transition to adulthood, however, is often accompanied by significant changes in social roles, environments, and individual achievement, making it an optimal time to understand how education influences STI risk. During this transition, social and economic trajectories often diverge.12 These divergent trajectories can result in a range of social environments that may be more or less “risky.” For example, although attending college may result in a college degree that leads to more optimal economic outcomes, it may also provide a social environment where young adults engage in risky health behaviors. 13–16 Moreover, studies suggest that the extent to which college students engage in risky behaviors may differ by race/ethnicity,17–19 suggesting the need to pursue research examining the social context that may predict or facilitate engagement in these behaviors and reasons for differences by race/ethnicity.
Of the few studies that have been conducted with young adults to assess the relationship between educational factors and sexual risk, findings are inconsistent. This inconsistency may be due, in part, to the specialized populations sampled, the use of limited measures of sexual risk without direct assessment of STI diagnoses, and the use of less rigorous statistical techniques. For example, using the National Acquired Immunodeficiency Syndrome (AIDS) Behavioral Survey, Binson et al.20 found that white young adults (aged <25 years) who completed 12 or more years of education were more likely to have multiple sex partners than white young adults with fewer than 12 years of education. The authors found no association between education and the number of sexual partners among Hispanic and black individuals. In another study using a small clinic sample of black people who were currently or previously diagnosed with an STI in one metropolitan city, Irwin and colleagues21 found that symptomatic patients with at least a high school education were more likely to report “always” using condoms, compared with those with less than a high school education. A final example involved a sample of incarcerated women (aged ≥18 years) in Rhode Island.22 Findings revealed that women with more years of education were less likely to engage in risky sexual and nonsexual behaviors, such as having sex without a condom and sharing intravenous drug equipment, in the last three months, compared with those with less education.
Additionally, extant research has not adequately explored the possibility that race may moderate the relationship between education and STI risk. Yet, a growing body of evidence documents that black people derive fewer economic and health benefits at equivalent levels of education and income than white people.23–25 For example, white college graduates' median net worth is more than three times the median net worth of black college graduates.24 Similarly, research has shown that income is unrelated to rates of overweight among black women, but is significantly associated with reductions of overweight among white women. Among women aged ≥20 years, the infant mortality rate of black college graduates is higher than it is for white people with less than a high school diploma.26 Thus, it is possible that education may also have a stronger association with STI diagnosis among white women than among black women.
Given the significant processes occurring during the transition to adulthood, understanding the influence of education on STI risk is warranted. Thus, the purpose of our study was to (1) describe the association between education and STI diagnosis (self-reported and clinically assessed) among a national sample of black and white young adult females and (2) examine racial differences in this association.
METHODS
Study sample
We used data from the National Longitudinal Study of Adolescent Health (Add Health), a nationally representative sample of adolescents in grades seven through 12 in 1994–1995. Baseline interviews occurred in 1994–1995, with follow-up interviews in 1995–1996 (Wave II) and 2001–2002 (Wave III). A detailed description of the sampling design is provided elsewhere.27 Our measures of STI diagnosis were obtained from Wave III, when respondents were aged 18 to 26 years. We also used data from previous waves to construct measures of family background and adolescents' sexual and nonsexual risk behaviors.
We restricted our sample to female respondents interviewed in 2001–2002 who had ever had sexual intercourse and self-reported as non-Hispanic black or non-Hispanic white. Males and those identifying as Asian/Pacific Islander, Native American, and Hispanic did not have enough cases of STI diagnosis across education levels to provide stable estimates. We utilized case-wise deletion in our analyses, resulting in a loss of 6.4% of our sample; item “missingness” on covariates was higher among black respondents, those with less education, and older respondents, but unrelated to self-reported STI diagnosis or the STI assay results. Finally, item missingness on our dependent variables differed—less than 1% of our sample refused to self-report STI diagnosis; however, approximately 7% of our sample refused to consent to the STI assay test. In addition, 10% of respondents who consented did not receive an STI diagnosis, due to specimen deterioration or because the sample was not returned within the specified time frame. Thus, our analytic sample differed by dependent variable. Analyses using self-reported STI diagnosis included 4,821 females (1,414 were non-Hispanic black and 3,407 were non-Hispanic white). Analyses using the STI assay diagnosis included 4,045 females (1,199 were non-Hispanic black and 2,846 were non-Hispanic white). All of our analyses used the sampling weights developed by Add Health and the svy commands in Stata® version 10.028 to account for the complex sampling design and respondent attrition.
Measures
Dependent variables.
In 2001–2002, respondents were asked if, in the previous 12 months, a doctor had diagnosed them with chlamydia, gonorrhea, or trichomoniasis. We created a binary measure of self-reported STI diagnosis, which we coded 1 if the respondent reported that she had been diagnosed with any of these three STIs, and 0 if she reported “no” to all three of these STIs. Respondents were also asked to provide a urine specimen that was subsequently tested for the same three STIs. We created a binary measure of STI assay diagnosis, coded 1 if the respondent tested positive for chlamydia, gonorrhea, or trichomoniasis, and 0 if the respondent tested negative for all three of these STIs.
Independent variables.
Respondents' educational status was categorized as less than a high school diploma, a high school diploma only, or enrolled in/graduated from a four-year college as of 2001–2002. Race of respondents was a self-reported measure categorized as non-Hispanic black or non-Hispanic white (hereafter referred to as black or white).
Covariates.
We included a number of covariates in our analyses that had previously shown an association with STI diagnosis, educational status, or both. These included age of respondent in 2001–2002, parent education (1 = at least one parent with a high school diploma or higher; 0 = otherwise), and family structure in 1994–1995 (1 = lived with both biological parents; 0 = otherwise). Sexual risk behaviors included lifetime number of sexual partners as of 2001–2002, age at sexual initiation, condom use in the past 12 months (categorized as never, sometimes, most of the time, and all of the time), ever having sex with a person who shoots street drugs, ever having sex in exchange for money, ever getting into a sexual situation due to drinking, and ever getting into a sexual situation due to the use of drugs. Nonsexual risk behaviors included indicators that measure if a respondent ever came into contact with the justice system (defined as being on probation or detention or both as a juvenile, or on probation or sent to jail/prison as an adult), respondents' smoking status (categorized as never smoked, past smoker, and current smoker), drinking behavior (categorized as never engaged in binge drinking, infrequently binge drink, sometimes binge drink, and frequently binge drink), and use of any illegal drugs (defined as use of marijuana, cocaine, crystal methamphetamine, lysergic acid diethylamide, phencyclidine, ecstasy, mushrooms, inhalants, ice, heroin, or prescription drugs not prescribed to the respondent). All nonsexual risk-behavior variables were measured in 2001–2002.
Analytic approach
First, we explored the bivariate relationships between educational status and the sample characteristics by race. Logistic regression was then used to examine the relationship between educational status and our two dependent variables, where a p<0.05 was considered statistically significant. We present logistic regression results as log-odds. Additionally, we transformed the log-odds estimates for various subgroups (e.g., white females with a high school diploma and black females with a high school diploma) into predicted probabilities and plotted the predicted probabilities to better understand how the association between educational status and STI diagnosis varied by race. We used the following formula to calculate the predicted probabilities of each subgroup:
 |
where P̂ is the predicted probability of STI diagnosis, β0 represents the constant, and βx represents the individual variable(s) of interest (e.g., race and high school education).
RESULTS
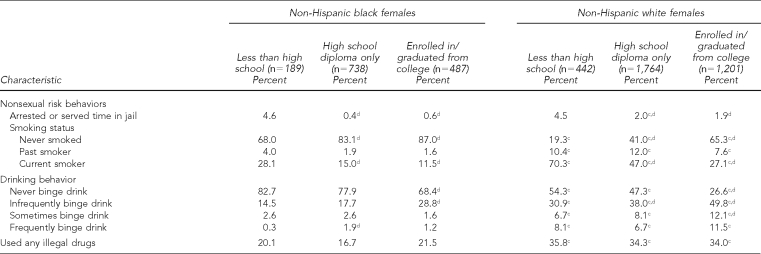
Table 1 presents characteristics of the study sample by race and educational status. Regarding educational status, among black and white females, similar proportions of respondents had less than a high school education (13.4% of black respondents and 13.0% of white respondents), had earned a high school diploma (52.2% of black respondents and 51.8% of white respondents), and had enrolled in or completed college (34.4% of black respondents and 35.3% of white respondents). Respondents also were comparable in age, with a mean age of 22 years for black and white respondents. Regarding family background, respondents were significantly different on measures of both parental education and family structure. Parents of white respondents achieved higher levels of education, and a greater proportion of respondents lived with both biological parents, compared with their black counterparts.
Table 1.
Sample characteristics by race and educational status, National Longitudinal Study of Adolescent Health (Add Health), Wave III, 2001–2002 (n=4,821), weighted dataa,b
aVariables are dummy coded and can be interpreted as percents, unless otherwise noted. Chi-square tests were used to test for significance with categorical and dichotomous variables. Two-sided t-tests were used to test for significance with continuous variables.
bAll estimates are weighted to adjust for the complex sampling design of Add Health and for nonresponse.
cSignificant (p<0.05) race differences within educational status (reference = white)
dSignificant (p<0.05) educational differences within race (reference = less than high school)
eSample size for Chi-square tests of STI assay diagnosis was 4,045. All other covariates used larger sample size based on self-reported STI diagnosis (n=4,821).
STI = sexually transmitted infection
To demonstrate how respondents' risk behaviors and STI diagnoses differed by race and educational status, we also present bivariate associations in Table 1. In regard to STI diagnosis, black females had significantly higher rates of both self-reported STIs and STI assay diagnosis, compared with their white counterparts. While rates of self-reported STIs did not vary significantly by educational status for black respondents, the rates of self-reported STIs declined among white females with increasing levels of education. However, the same pattern was not found for STI assay diagnosis. As educational level increased, rates of STI assay diagnosis declined for both black and white respondents, but only for those who were enrolled in or had graduated from college.
Significant within- and between-race differences were found by educational status for parental education, family structure, age at sexual initiation, having had sex for money, having been arrested or served time in jail, smoking status, and binge drinking. At higher levels of education, respondents were more likely to have had a parent with at least a high school diploma, lived in a family with two biological parents in 1994–1995, initiated sex at an earlier age, never had sex for money, never smoked, and never been arrested or served time in jail; but they were less likely to have never engaged in binge drinking, regardless of race. Compared with black females, white females were more likely to have parents who had at least a high school diploma, have lived in families with both biological parents, have initiated sex at a later age, never have had sex for money, be a current smoker, or frequently binge drink.
Table 2 presents models of self-reported and assay-diagnosed STIs, testing for independent and interactive effects of race and educational status. We present the odds ratios (ORs) for the association between education and race in Columns 1–4. The base model adjusts for race, education, and age. The final model adjusts for all covariates. Columns 1 and 2 present the results for self-reported STI diagnosis; Columns 3 and 4 present the results for STI assay diagnosis. For both the self-report and assay results, black respondents had higher odds of being diagnosed with an STI, compared with white respondents. We also found a negative association with education—higher education was associated with lower odds of STI diagnosis. Although the association was significant for those with a high school diploma or higher education level in the self-reported models, it was only significant for those who were enrolled in or had graduated from college in the assay-diagnosed models.
Table 2.
Logit models of self-reported STI and STI assay diagnoses, testing for the independent association of race and education (Columns 1–4) and for interaction effects of race and educational status (Columns 5–8), National Longitudinal Study of Adolescent Health (Add Health), Wave III, 2001–2002, non-Hispanic white and non-Hispanic black female respondents, weighted dataa,b,c
aAll estimates are weighted to adjust for the complex sampling design of Add Health and for nonresponse.
bBase model adjusted for age; final model adjusted for age, parental education, family structure in 1994, number of sexual partners as of 2001, age at sexual initiation, condom use in past 12 months, ever had sex for money, ever had sex with a person who shoots street drugs, ever in a sexual situation because of drinking or drugs, ever arrested or served time in jail, smoking status in 2001, drinking behavior in 2001, and illegal drug use.
cAll covariates are centered at their grand mean, except for race and educational status.
dp≤0.05
STI = sexually transmitted infection
To test if educational status was associated with STI diagnosis similarly for white and black females, we included a set of variables interacting race and educational status (Table 2, Columns 5–8). For both dependent variables, black respondents were more likely to have an STI diagnosis than white respondents. As education increased, the log-odds of STI diagnosis decreased. This association was only significant among white people, however, when self-reported STI diagnosis was the dependent variable. Indeed, the significant and positive black-×-education interaction terms -canceled out the main effects of education. This pattern held after adjustment for all covariates (Final model, Column 6). In comparison, respondents who where enrolled in or had graduated from college experienced lower log-odds of an STI assay diagnosis, regardless of race. Adjustment for all covariates (Final model, Column 8) attenuated the association between college enrollment/degree and STI assay diagnosis; however, the race-×-education terms were also nonsignificant, suggesting that at least for STI assay diagnosis, the association with education was similar for black and white respondents.
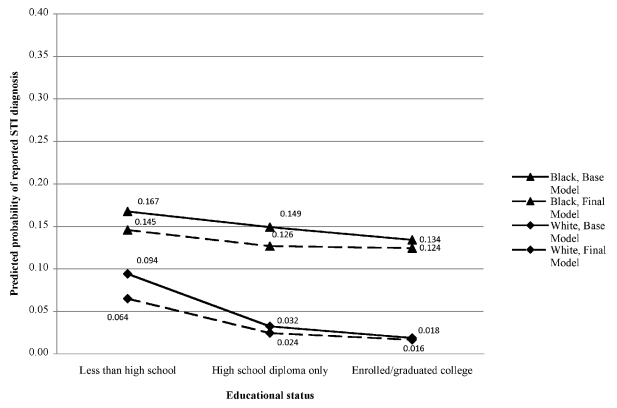
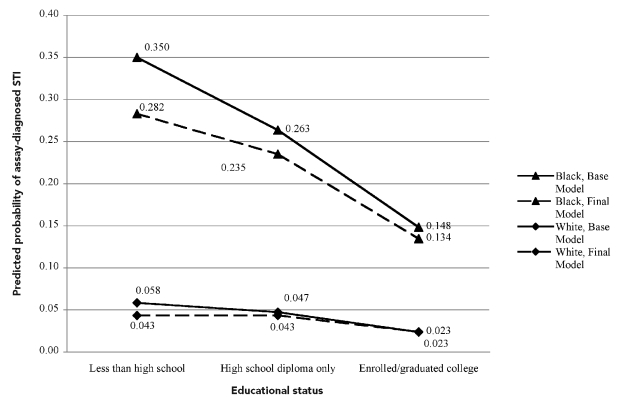
Figures 1 and 2 depict the predicted probabilities by race and educational status for self-reported STI diagnosis and STI assay diagnosis, respectively. As shown in Figure 1, black females had a higher probability than white females of self-reported STI diagnosis at all levels of educational status. White females also experienced a significant decline in their predicted probability of self-reported STI diagnosis with increasing education, while black females did not. This pattern did not hold in Figure 2. Both black and white females experienced a significantly lower predicted probability of STI assay diagnosis if they were enrolled in or had graduated from college than if they had completed less than a high school diploma. Moreover, regardless of the dependent variable, black females who were enrolled in or had graduated from college had a significantly higher predicted probability than white females with less than a high school diploma. For example, approximately 12.4% of black respondents enrolled in/graduated from college self-reported an STI diagnosis, compared with 6.4% of white respondents with less than a high school diploma. For assay diagnosis, the predicted probabilities were 13.4% and 4.3% for black vs. white respondents, respectively.
Figure 1.
Predicted probability of self-reported STI diagnosis in previous 12 months for an average female respondent, by race and educational status, National Longitudinal Study of Adolescent Health (Add Health), Wave III, 2001–2002a
aBase model is adjusted for age; final model is adjusted for age, parental education, family structure in 1994, number of sexual partners as of 2001, age at sexual initiation, condom use in past 12 months, ever had sex for money, ever had sex with a person who shoots sheet drugs, ever in a sexual situation because of drinking or drugs, ever arrested or served time in jail, smoking status in 2001, drinking behavior in 2001, and illegal drug use.
STI = sexually transmitted infection
Figure 2.
Predicted probability of assay-diagnosed STI for an average female respondent, by race and educational status, National Longitudinal Study of Adolescent Health (Add Health), Wave III, 2001–2002a
aBase model is adjusted for age; final model is adjusted for age, parental education, family structure in 1994, number of sexual partners as of 2001, age at sexual initiation, condom use in past 12 months, ever had sex for money, ever had sex with a person who shoots sheet drugs, ever in a sexual situation because of drinking or drugs, ever arrested or served time in jail, smoking status in 2001, drinking behavior in 2001, and illegal drug use.
STI = sexually transmitted infection
DISCUSSION
Our study provides evidence that (1) there is an inverse association between education and STI diagnosis among young adult females; (2) this inverse association is stronger for white females than for black females, when assessed using self-reported STI diagnosis; and (3) black females who were enrolled in or had graduated from college have significantly higher predicted probabilities of having an STI than white females with less than a high school diploma, regardless of STI measure used. Unlike previous studies focused on the adolescent population,9,10,29 our bivariate results suggest that education is associated with decreased engagement in sexual risk behaviors, but that this association may vary by race. For example, education was unrelated to the number of sexual partners or getting into a sexual situation due to drinking or drugs among black respondents, but was inversely associated with these risk factors among white respondents. We did, however, find that for both black and white respondents, education was associated with a decreased risk of early sexual initiation, having sex with a person who shoots street drugs, having sex for money, and using condoms. The latter findings appear consistent with a recent study by Spriggs et al. in which the authors found that college enrollment was associated with later timing of sexual debut among a national sample of young adult women; however, they did not examine this association by race.30 Nonetheless, our results provide additional evidence that education may reduce some sexual risk behaviors among women during the transition to adulthood, but that additional research investigating the differential impact of education across racial groups is warranted.
Our finding that race differentially influences the association between education and self-reported STI diagnosis is consistent with prior research examining racial differences in the relationship between social determinants of health—such as socioeconomic status (SES)—and health.23,25,31 This research suggests that, in general, measures of SES (including education) are not equivalent across racial groups, and black individuals often derive fewer economic and health benefits at equivalent levels of SES. A possible reason for this non-equivalence lies in the conceptualization and measurement of SES—a measure of education, income, and/or occupational status.26,31–33
Education is often viewed as a fixed attribute that represents human capital achievement.34 Yet, race-based stratification still occurs within the educational system,35,36 often resulting in differences in the quality37–39 and quantity of education that black students receive. For example, black students at the primary and secondary education levels are more likely to attend segregated and economically disadvantaged schools that provide fewer educational opportunities—they are more likely to suffer from overcrowded classrooms, outdated books and supplies, fewer advanced placement courses, and fewer laboratories,40,41 as well as less qualified teachers.42 At the post-secondary level, examples of this stratification include prestige of educational institution attended,43,44 access to resources to facilitate the educational experience and mitigate stressors associated with achieving higher educational status (i.e., financial support and social support of family members who may also be college educated),45,46 and levels of stress that may be differentially borne as a consequence of obtaining higher education.47–49 These contextual factors may impact educational achievement and are likely confounded in traditional measures of education. Thus, it is important to note that our measure of education may actually be capturing disparities in social and physical environments occurring earlier in life, and may in part explain why highly educated black women in our study still experience higher levels of STI diagnosis than less educated white women.
As expected, based on U.S. surveillance data, STI prevalence rates (self-reported vs. biologically confirmed STI rates, respectively) among black females in our sample averaged three to six times those among white females.2 However, an unexpected and quite notable finding was that black females engaged in a substantially lower proportion of sexual or nonsexual risk behaviors compared with white females. For instance, although white respondents with at least a high school diploma were older than their black counterparts the first time they engaged in sexual intercourse, white females with less than a high school diploma reported more sexual partners than their black counterparts. Moreover, regardless of educational status, white respondents were less likely than black respondents to use a condom and more likely to get into a sexual situation due to drinking, smoking, binge drinking, or using illegal drugs. This is contrary to extant research that depicts clear associations between sexual risk behavior and STI prevalence, as well as higher levels of sexual risk-taking among black young adults compared with their white counterparts.50–53 While some researchers have suggested nonbehavioral, contextual factors that may impact STI prevalence (e.g., differential access to condoms, awareness of STI-prevention information, beliefs about invulnerability to negative health outcomes, partners' sexual risk, and partner concurrency),54–59 few have shown as weak an association between risk behavior and STI diagnosis as that found in our study.
A partial explanation of our findings may be that black women, although engaging in fewer sexual risk behaviors, may be selecting behaviors that put them at the greatest risk of infection. Alternatively, black and white women may be engaging in comparable levels of some risk activities, but black women may be doing so with riskier partners, in which case these women unknowingly take on their partners' risk status and sexual networks.55,57–61 In fact, research has shown that the low sex ratio among black people may inadvertently promote overlapping sexual networks and partner concurrency.55 In these cases, men may more easily choose to engage in multiple relationships with little concern that their primary partner will leave the relationship because of the difficulty that women may encounter in finding a replacement partner who is mutually monogamous.62 Future research efforts must elucidate the mechanism for the differences in risk behavior shown between black and white women and why this relates differentially to STI outcomes.
One final finding of interest is the difference in rates of self-reported vs. biologically confirmed STIs among the study sample. A possible explanation for the difference is that the reference point for each measure was unique. That is, for the self-report measure, respondents were asked to report STI diagnosis in the previous 12-month period, while the biological assay assessed STI status at the time of the interview. Additionally, post-hoc analyses (data available upon request) revealed that item missingness may have also contributed to these differences; respondents with a high school diploma or who were enrolled in/graduated from college were more likely to refuse to give consent, compared with those who consented to the STI assay, regardless of race. Thus, item missingness on the STI assay variable was related to educational status and may be one reason why we did not find consistent results across dependent variables. Although clinically assessed measures of STIs are viewed as the gold standard,63–65 our analyses suggest caution in interpreting these measures, especially if consent is nonrandom. Given these findings, we elected to present both sets of results.
Limitations
In addition to those previously mentioned, several other limitations apply to our findings. First, sexual risk behaviors in this study were measured via self-report, which could have introduced recall bias or underreporting. However, respondents reported on sexual risk behaviors via computer-assisted personal interviewing, a method that has been demonstrated to decrease the likelihood of social desirability bias,66 particularly when asking about sensitive topics.67 Second, we were unable to include men and other racial/ethnic groups in our analysis, due to small cell sizes. Nonetheless, we believe that our findings contribute to the literature on social determinants of STIs, particularly as they relate to addressing the disquieting STI rates among black women.
CONCLUSION
Our findings provide evidence that although education may decrease STI risk, the extent to which it does so may vary by race. Additionally, while individual-level risk behaviors are important precursors to STI rates, among some groups, contextual-level factors may play an even more significant role as contributors to disease rates. Policies and interventions should, therefore, not only focus on less educated populations or on individual risk behaviors, but also on contextual-level factors that may influence STI risk differentially by race. Specifically, efforts aimed at reducing STI prevalence and/or risk among black females should be offered, regardless of educational status, and may need to begin early and in concert with administrators at secondary and post-secondary educational institutions. Overall, social determinants, such as education, should be viewed as important factors associated with STI risk, but their differential impact on various racial/ethnic groups should also be considered when addressing the disproportionate rates of STIs in the U.S.
Footnotes
This research was supported in part by the University of Michigan's Robert Wood Johnson Foundation Health & Society Scholars Program small grant #N008885, awarded to Katrina Walsemann.
This research uses data from the National Longitudinal Study of Adolescent Health (Add Health), a program project directed by Kathleen Mullan Harris and designed by J. Richard Udry, Peter S. Bearman, and Kathleen Mullan Harris at the University of North Carolina at Chapel Hill, and funded by grant P01-HD31921 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, with cooperative funding from 23 other federal agencies and foundations. Special acknowledgment is due Ronald R. Rindfuss and Barbara Entwisle for assistance in the original design. Information on how to obtain the Add Health data files is available on the Add Health website (http://www.cpc.unc.edu/addhealth). No direct support was received from grant P01-HD31921 for this analysis.
REFERENCES
- 1.Weinstock H, Berman S, Cates W. Sexually transmitted diseases among American youth: incidence and prevalence estimates, 2000. Perspect Sex Reprod Health. 2004;36:6–10. doi: 10.1363/psrh.36.6.04. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention (US) Sexually transmitted disease surveillance, 2007. Atlanta: CDC; 2008. [Google Scholar]
- 3.Cates JR, Herndon NL, Schulz SL, Darroch JE. Chapel Hill (NC): University of North Carolina at Chapel Hill, School of Journalism and Mass Communication; 2004. Our voices, our lives, our futures: youth and sexually transmitted diseases. [Google Scholar]
- 4.CDC (US) CDC HIV/AIDS fact sheet. Atlanta: CDC; 2009. HIV/AIDS among African Americans. [Google Scholar]
- 5.Fleming DT, Wasserheit JN. From epidemiological synergy to public health policy and practice: the contribution of other sexually transmitted diseases to sexual transmission of HIV infection. Sex Transm Infect. 1999;75:3–17. doi: 10.1136/sti.75.1.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mills N, Daker-White G, Graham A, Campbell R. Population screening for Chlamydia trachomatis infection in the UK: a qualitative study of the experiences of those screened. Fam Pract. 2006;23:550–7. doi: 10.1093/fampra/cml031. [DOI] [PubMed] [Google Scholar]
- 7.Halpern CT, Joyner K, Udry JR, Suchindran C. Smart teens don't have sex (or kiss much either) J Adolesc Health. 2000;26:213–25. doi: 10.1016/s1054-139x(99)00061-0. [DOI] [PubMed] [Google Scholar]
- 8.Zweig JM, Phillips SD, Lindberg LD. Predicting adolescent profiles of risk: looking beyond demographics. J Adolesc Health. 2002;31:343–53. doi: 10.1016/s1054-139x(02)00371-3. [DOI] [PubMed] [Google Scholar]
- 9.Ford CA, Pence BW, Miller WC, Resnick MD, Bearinger LH, Pettingell S, et al. Predicting adolescents' longitudinal risk for sexually transmitted infection: results from the National Longitudinal Study of Adolescent Health. Arch Pediatr Adolesc Med. 2005;159:657–64. doi: 10.1001/archpedi.159.7.657. [DOI] [PubMed] [Google Scholar]
- 10.Ohannessian CM, Crockett LJ. A longitudinal investigation of the relationship between educational investment and adolescent sexual activity. J Adolesc Res. 1993;8:167–82. [Google Scholar]
- 11.Scott-Jones D, White AB. Correlates of sexual activity in early adolescence. J Early Adolesc. 1990;10:221–38. [Google Scholar]
- 12.Shanahan MJ. Pathways to adulthood in changing societies: variability and mechanisms in life course perspective. Annu Rev Sociol. 2000;26:667–92. [Google Scholar]
- 13.Caron SL, Davis CM, Halteman WA, Stickle M. Predictors of condom-related behaviors among first-year college students. J Sex Res. 1993;30:252–9. [Google Scholar]
- 14.Shapiro J, Radecki S, Charchian AS, Josephson V. Sexual behavior and AIDS-related knowledge among community college students in Orange County, California. J Community Health. 1999;24:29–43. doi: 10.1023/a:1018713231400. [DOI] [PubMed] [Google Scholar]
- 15.Fromme K, Corbin WR, Kruse MI. Behavioral risks during the transition from high school to college. Dev Psychol. 2008;44:1497–504. doi: 10.1037/a0012614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Annang L, Johnson S, Pepper-Washington M. The context of sexual risk among African American female college students. J Health Dispar Res Pract. 2009;3:99–114. [Google Scholar]
- 17.Youth risk behavior surveillance: National College Health Risk Behavior Survey—United States, 1995. MMWR Surveill Summ. 1997;46(6):1–56. [PubMed] [Google Scholar]
- 18.Flannery D, Ellingson L, Votaw KS, Schaefer EA. Anal intercourse and sexual risk factors among college women, 1993–2000. Am J Health Behav. 2003;27:228–34. doi: 10.5993/ajhb.27.3.4. [DOI] [PubMed] [Google Scholar]
- 19.American College Health Association. American College Health Association—National college health assessment spring 2007 reference group data report (abridged) J Am Coll Health. 2008;56:469–79. doi: 10.3200/JACH.56.5.469-480. [DOI] [PubMed] [Google Scholar]
- 20.Binson D, Dolcini MM, Pollack LM, Catania JA. Data from the National AIDS Behavioral Surveys. IV. Multiple sexual partners among young adults in high-risk cities. Fam Plann Perspect. 1993;25:268–72. [PubMed] [Google Scholar]
- 21.Irwin DE, Thomas JC, Spitters CE, Leone PA, Stratton JD, Martin DH, et al. Self-reported sexual activity and condom use among symptomatic clients attending STD clinics. Sex Transm Dis. 1999;26:286–90. doi: 10.1097/00007435-199905000-00009. [DOI] [PubMed] [Google Scholar]
- 22.Paasche-Orlow MK, Clarke JG, Herbert MR, Ray MK, Stein MD. Educational attainment but not literacy is associated with HIV risk behavior among incarcerated women. J Womens Health. 2005;14:852–9. doi: 10.1089/jwh.2005.14.852. [DOI] [PubMed] [Google Scholar]
- 23.Williams DR, Williams-Morris R. Racism and mental health: the African American experience. Ethn Health. 2000;5:243–68. doi: 10.1080/713667453. [DOI] [PubMed] [Google Scholar]
- 24.Shapiro TM. The hidden cost of being African American: how wealth perpetuates inequality. New York: Oxford University Press; 2004. [Google Scholar]
- 25.Pearson JA. Can't buy me whiteness: new lessons from the Titanic on race, ethnicity, and health. DuBois Review: Social Science Research on Race. 2008;5:27–47. [Google Scholar]
- 26.Williams DR. Racial/ethnic variations in women's health: the social embeddedness of health. Am J Public Health. 2002;92:588–97. doi: 10.2105/ajph.92.4.588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chantala K, Tabor J. Chapel Hill (NC): University of North Carolina at Chapel Hill, Carolina Population Center; 1999. Strategies to perform a design-based analysis using the Add Health data. [Google Scholar]
- 28.StataCorp LP. Stata®: Version 10.0. College Station (TX): StataCorp LP; 2007. [Google Scholar]
- 29.Miller BC, Sneesby KR. Educational correlates of adolescents' sexual attitudes and behavior. J Youth Adolesc. 1988;17:521–30. doi: 10.1007/BF01537829. [DOI] [PubMed] [Google Scholar]
- 30.Spriggs AL, Halpern CT. Timing of sexual debut and initiation of postsecondary education by early adulthood. Perspect Sex Reprod Health. 2008;40:152–61. doi: 10.1363/4015208. [DOI] [PubMed] [Google Scholar]
- 31.Williams DR, Collins C. U.S. socioeconomic and racial differences in health: patterns and explanations. Annu Rev Sociol. 1995;21:349–86. [Google Scholar]
- 32.Schoendorf KC, Hogue CJ, Kleinman JC, Rowley D. Mortality among infants of black as compared with white college-educated parents. N Engl J Med. 1992;326:1522–6. doi: 10.1056/NEJM199206043262303. [DOI] [PubMed] [Google Scholar]
- 33.Kaufman JS, Cooper RS, McGee DL. Socioeconomic status and health in blacks and whites: the problem of residual confounding and the resiliency of race. Epidemiology. 1997;8:621–8. [PubMed] [Google Scholar]
- 34.Krieger N, Fee E. Social class: the missing link in U.S. health data. Int J Health Serv. 1994;24:25–44. doi: 10.2190/2JG7-YMD5-WCP2-XXNT. [DOI] [PubMed] [Google Scholar]
- 35.Lewis AE. Race in the schoolyard: negotiating the color line in classrooms and communities. Piscataway (NJ): Rutgers University Press; 2003. [Google Scholar]
- 36.Walsemann KM, Geronimus AT, Gee GC. Accumulating disadvantage over the life course: evidence from a longitudinal study investigating the relationship between educational advantage in youth and health in middle age. Res Aging. 2008;30:169–99. [Google Scholar]
- 37.Card D, Krueger AB. Does school quality matter? Returns to education and the characteristics of public schools in the United States. J Polit Econ. 1992;100:1–40. [Google Scholar]
- 38.Clarke M. Weighing things up: a closer look at U.S News & World Report's ranking formulas. Coll Univ. 2004;79:3–9. [Google Scholar]
- 39.Dill DD, Soo M. Academic quality, league tables, and public policy: a cross-national analysis of university ranking systems. High Educ. 2005;49:495–533. [Google Scholar]
- 40.Kane T. The price of admission: rethinking how Americans pay for college. Washington: Brookings/Russell Sage Foundation; 1999. [Google Scholar]
- 41.Lucas SR. Tracking inequality: stratification and mobility in American high schools. New York: Teachers College Press; 1999. [Google Scholar]
- 42.Darling-Hammond L. Inequality and the right to learn: access to qualified teachers in California's public schools. Teach Coll Rec. 2004;106:1936–66. [Google Scholar]
- 43.Brewer DJ, Gates SM, Goldman CA. higher education. Piscataway (NJ): Transaction Publishers; 2002. In pursuit of prestige: strategy and competition in the U.S. [Google Scholar]
- 44.Astin AW, Oseguera L. The declining “equity” of American higher education. Rev High Educ. 2004;27:321–41. [Google Scholar]
- 45.Adelman C. The toolbox revisited: paths to degree completion from high school through college. Washington: Department of Education (US); 2006. [Google Scholar]
- 46.Pearce J, Witten K, Bartie P. Neighbourhoods and health: a GIS approach to measuring community resource accessibility. J Epidemiol Commun Health. 2006;60:389–95. doi: 10.1136/jech.2005.043281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Geronimus AT. The weathering hypothesis and the health of African-American women and infants: evidence and speculations. Ethn Dis. 1992;2:207–21. [PubMed] [Google Scholar]
- 48.Thomas SL. Deferred costs and economic returns to college quality, major, and performance: an analysis of recent graduates in baccalaureate and beyond. Res High Educ. 2000;41:281–313. [Google Scholar]
- 49.Meijer J. Correlates of student stress in secondary education. Educ Res. 2007;49:21–35. [Google Scholar]
- 50.Warren CW, Santelli JS, Everett SA, Kann L, Collins JL, Cassell C, et al. Sexual behavior among U.S. high school students, 1990–1995. Fam Plann Perspect. 1998;30:170–2. 200. [PubMed] [Google Scholar]
- 51.Miller HG, Cain VS, Rogers SM, Gribble JN, Turner CF. Correlates of sexually transmitted bacterial infections among U.S. women in 1995. Fam Plann Perspect. 1999;31:4–9. 23. [PubMed] [Google Scholar]
- 52.Ku L, St Louis M, Farshy C, Aral S, Turner CF, Lindberg LD, et al. Risk behaviors, medical care, and chlamydial infection among young men in the United States. Am J Public Health. 2002;92:1140–3. doi: 10.2105/ajph.92.7.1140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Grunbaum JA, Kann L, Kinchen S, Ross J, Hawkins J, Lowry R, et al. Youth risk behavior surveillance—United States, 2003. MMWR Surveill Summ. 2004;53(2):1–96. [PubMed] [Google Scholar]
- 54.Ellen JM, Aral SO, Madger LS. Do differences in sexual behaviors account for the racial/ethnic differences in adolescents' self-reported history of a sexually transmitted disease? Sex Transm Dis. 1998;25:125–9. doi: 10.1097/00007435-199803000-00002. [DOI] [PubMed] [Google Scholar]
- 55.Adimora AA, Schoenbach VJ. Contextual factors and the black-white disparity in heterosexual HIV transmission. Epidemiology. 2002;13:707–12. doi: 10.1097/00001648-200211000-00016. [DOI] [PubMed] [Google Scholar]
- 56.Hallfors DD, Iritani BJ, Miller WC, Bauer DJ. Sexual and drug behavior patterns and HIV and STD racial disparities: the need for new directions. Am J Public Health. 2007;97:125–32. doi: 10.2105/AJPH.2005.075747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Aral SO, Adimora AA, Fenton KA. Understanding and responding to disparities in HIV and other sexually transmitted infections in African Americans. Lancet. 2008;372:337–40. doi: 10.1016/S0140-6736(08)61118-6. [DOI] [PubMed] [Google Scholar]
- 58.Adimora AA, Schoenbach VJ, Doherty IA. HIV and African Americans in the southern United States: sexual networks and social context. Sex Transm Dis. 2006;33(Suppl 7):S39–45. doi: 10.1097/01.olq.0000228298.07826.68. [DOI] [PubMed] [Google Scholar]
- 59.Morris CN, Morris SR, Ferguson AG. Sexual behavior of female sex workers and access to condoms in Kenya and Uganda on the Trans-Africa highway. AIDS Behav. 2009;13:860–5. doi: 10.1007/s10461-008-9431-z. [DOI] [PubMed] [Google Scholar]
- 60.Anderson RM. Transmission dynamics of sexually transmitted infections. In: Holmes KK, Sparling PF, Stamm WE, Piot P, Wasserheit JN, Corey L, et al., editors. 3rd ed. New York: McGraw-Hill; 1999. [Google Scholar]
- 61.Halpern CT, Hallfors D, Bauer DJ, Iritani B, Waller MW, Cho H. Implications of racial and gender differences in patterns of adolescent risk behavior for HIV and other sexually transmitted diseases. Perspect Sex Reprod Health. 2004;36:239–47. doi: 10.1363/psrh.36.239.04. [DOI] [PubMed] [Google Scholar]
- 62.Thomas JC, Thomas KK. Things ain't what they ought to be: social forces underlying racial disparities in rates of sexually transmitted diseases in a rural North Carolina county. Soc Sci Med. 1999;49:1075–84. doi: 10.1016/s0277-9536(99)00197-5. [DOI] [PubMed] [Google Scholar]
- 63.Grimley DM, Annang L, Houser S, Chen H. Prevalence of condom use errors among STD clinic patients. Am J Health Behav. 2005;29:324–30. doi: 10.5993/ajhb.29.4.4. [DOI] [PubMed] [Google Scholar]
- 64.Annang L, Grimley D, Hook EW., 3rd Vaginal douche practices among black women at risk: exploring douching prevalence, reasons for douching, and sexually transmitted disease infection. Sex Transm Dis. 2006;33:215–9. doi: 10.1097/01.olq.0000205046.11916.c5. [DOI] [PubMed] [Google Scholar]
- 65.Grimley DM, Annang L, Lewis I, Smith RW, Aban I, Hooks T, et al. Sexually transmitted infections among urban shelter clients. Sex Transm Dis. 2006;33:666–9. doi: 10.1097/01.olq.0000223285.18331.4d. [DOI] [PubMed] [Google Scholar]
- 66.Bradburm N, Sudman S, Wansink B. 2nd ed. San Francisco: Jossey-Bass; 2004. Asking questions: the definitive guide to questionnaire design—for market research, political polls, and social and health questionnaires. [Google Scholar]
- 67.Turner CF, Ku L, Rogers SM, Lindberg LD, Pleck JH, Sonenstein FL. Adolescent sexual behavior, drug use, and violence: increased reporting with computer survey technology. Science. 1998;280:867–73. doi: 10.1126/science.280.5365.867. [DOI] [PubMed] [Google Scholar]