Abstract
Objective
Although a transradial angiography is accepted as the gold standard for cardiovascular procedures, cerebral angiography has been performed via transfemoral approach in most institutions. The purpose of this study is to present our experience concerning the feasibility, efficacy, and safety of a transradial approach to cerebral angiography as an alternative to a transfemoral approach.
Methods
Between February 2007 and October 2009, a total of 1,240 cerebral angiographies were performed via a transradial approach in a single center. The right radial approach was used as an initial access route. The procedure continued only after the ulnar artery was proven to provide satisfactory collateral perfusion according to two tests (a modified Allen's test and forearm angiography).
Results
The procedural success rate was 94.8% with a mean duration of 28 minutes. All supra-aortic vessels were successfully catheterized with a success rate of 100%. The success rates of selective catheterization to the right vertebral artery, right internal carotid artery, left internal carotid artery, and left vertebral artery were 96.1%, 98.6%, 82.6% and 52.2%, respectively. The procedure was performed more than twice in 73 patients (5.9%), including up to 4 times in 2 patients. The radial artery occlusion was found in 4 patients (5.4%) on follow-up cerebral angiography, but no ischemic symptoms were observed in any of the cases.
Conclusion
This study suggests that cerebral angiography using a transradial approach can be performed with minimal risk of morbidity. In particular, this procedure might be useful for follow-up angiographies and place less stress on patients.
Keywords: Radial artery, Follow-up, Angiography, Cerebral angiography
INTRODUCTION
Catheterized cerebral angiography remains the gold standard method for examining the vasculature of patients with cerebrovascular disease, although other imaging methods, including magnetic resonance angiography and computerized tomography angiography, are more commonly used. The femoral artery is the most common puncture site used for cerebral angiography, because most clinicians know how to easily access this artery and because the size of the femoral artery allows a wide diameter catheter to be inserted. However, a transfemoral approach is not possible in all patients, and there are several limitations to this approach. For example, transfemoral access cannot be used when patients have extensive atherosclerotic disease in their aortic arch, atypical anatomy of their aortic or brachiocephalic vessels, dissection of the thoracic aorta, iliofemoral occlusive disease, or groin infections2,6). Additionally, transfemoral cerebral angiography requires patients to tolerate uncomfortable compression of the groin in addition to a several hours of bed rest after the procedure. Finally, this procedure may lead to serious complications, including pseudoaneurysm formation, arteriovenous fistula formation, retroperitoneal hemorrhage, femoral nerve injury, lower limb ischemia, and pulmonary embolism12,17,19,20).
The transradial approach for coronary angiography was first described by Campeau in 19894). Many studies have reported its benefits; it is more comfortable for the patient and more cost effective2,7,10,11,14,16). Transradial angiography has become popular among a majority of interventional cardiologists as a diagnostic and therapeutic tool. However, there have been few reports on the successful application of transradial cerebral angiography6,8,11-13,18,25).
Since February 2007, we shifted the initial access from the right femoral artery to the right radial artery in all patients requiring cerebral angiography. In the present study, we present a single center experience with using the transradial approach for cerebral angiography as an alternative to transfemoral and transbrachial approaches. We aimed to evaluate the feasibility, efficacy, safety, and limitations of a transradial approach for cerebral angiography in comparison with the transfemoral method.
MATERIALS AND METHODS
Between February 2007 and October 2009, 2,086 patients underwent selective cerebral angiography with digital subtraction angiography in our department. For 1,240 patients (59.4%), the procedure was performed via a transradial approach for the evaluation of cerebrovascular disease. These patients ranged in age from 13 to 80 years (mean age, 58.6 years) and included 641 women and 599 men. Patients requiring interventional procedures were excluded. Three operators performed the transradial cerebral angiography procedures. All of the operators were relatively experienced, having performed a minimum of 100 transfemoral cerebral angiographies each.
All transradial approaches used an initial access site on the right arm, as it was more comfortable for right-handed operators. If the right arm was not available, we proceeded with a transfemoral approach. A transradial approach via the left arm was used only in cases requiring follow-up for one-vessel cerebral angiography. All patients underwent an ultrasound examination in order to measure the diameter of the radial artery, as well as a modified Allen's test of the right wrist to evaluate satisfactory collateral perfusion prior to the procedure. Adequate collateral circulation is considered to be present when the hand color returns to normal within 10 seconds after the ulnar artery is released, and when no reactive hyperemia is present after release of radial compression. Patients were prepared and draped with the right radial artery site exposed at the wrist and the right arm abducted at a 70-degree angle. The wrist was fixed in an extended position over a gauze roll. The skin at the puncture site was infiltrated with 1% lidocaine, and the artery was punctured at the point of maximum pulsation using a 20-gauge needle with a modified Seldinger technique. As a 5F introducer sheath (Terumo, Tokyo, Japan) was placed within the artery, and a cocktail solution [comprising a mixture of heparin (5,000 IU/mL), verapamil (2.0 mg), nitroglycerine (200 µg/mL; 0.25 mL)] was infused through the side-port of the introducer, to prevent radial artery spasm and thrombosis. Next, forearm angiography was performed through the side-port of the introducer sheath in order to confirm that there was satisfactory collateral perfusion (Fig. 1). After the ulnar artery was proven to be patent according to both tests (modified Allen's test and forearm angiography), the procedure proceeded. Heparin was systemically administered, except in contraindicated cases because of medical conditions, such as a recent hemorrhage. A 5-F Simmons type II catheter (Cook, Bloomington, IN, USA) with a 0.035-inch guidewire was used for almost all procedures. Simmons Type I catheters were also used for patients who required absolute need of the right vertebral artery (VA) selection. All supra-aortic vessels [4 vessels; right and left common carotid artery (CCA), right and left VA] were evaluated. Branch vessel [right internal carotid artery (ICA), left ICA, right VA, and left VA] evaluation was performed only if the selection of a branch vessel was required, in patients without stenosis of the cervical ICA or the VA orifice. We injected 8-9 mL of non-ionic, dimeric, water-soluble X-ray contrast medium (Visipaque®, Amersham Health, Cork, Ireland) at a rate of 5 mL/s for the CCA, 6-7 mL at a rate of 4 mL/s for the ICA and the VA, and 5 mL at a rate of 3 mL/s for the external carotid artery. In order to obtain a left VA angiography using a catheter placed in the left subclavian artery, we used 10-12 mL of contrast at a rate of 4-6 mL/s, while the patient's left upper arm was fastened with a blood pressure cuff. After the completion of the procedure, the catheters and sheathes were removed, and a superficial pressure dressing using a customized gauze-ball was immediately applied to the puncture site, without further manual hemostasis. Pulsation of the arteries was re-evaluated after adequate homeostasis; however, no further evaluation was performed to confirm the patency of the radial artery during the day of the procedure. Bed rest was not required following the procedure. In order to compare our standard transfemoral cerebral angiography technique with this technique, we recorded the procedure time from puncture to withdrawal of the introducer sheath for cases 995 to 1,094. At 1 day and at 2 weeks after catheterization, a standard physical examination was performed to evaluate the puncture site.
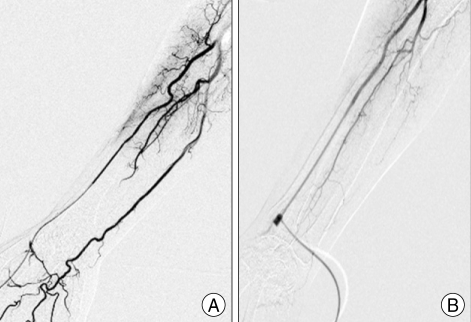
Fig. 1.
Forearm angiography through the side-port of the introducer sheath. A : Excellent collateral perfusion of the hand via the ulnar artery is observed. B : Absent ulnar artery with poor collateral perfusion. Transfemoral angiography was performed for this patient.
We analyzed the success rate of the procedure, the puncture site of the radial artery, repeat examinations using the same radial artery, any complications with the procedure, and the total procedure time.
RESULTS
The transradial approach was successful in 1,178 patients, resulting in a success rate of 94.8%. The mean diameter of the radial artery was 3.02 mm (1.7-4.8 mm; men 3.2 mm, women 2.8 mm). All supra-aortic vessels were successfully catheterized with a success rate of 100%. However, the selective catheterization rates of the left sided branching vessels were lower, as success rates were 96.1% (693/721) for the right VA, 98.6% (770/781) for the right ICA, 52.2% (356/682) for the left VA, and 82.6% (615/744) for the left ICA (Fig. 2). The diagnostic adequacy and quality of images were sufficient using the transradial approach, and none of these cases had to be converted to a transfemoral approach. Puncture of the radial artery was performed on the right side in 1,225 cases (98.9%), and on the left side in 15 cases (1.2%). The left side was used for the initial procedure as a means to better evaluate the left vertebral artery in 8 cases, right radial artery occlusion in 5 cases (1 spontaneous, 4 after the previous procedure) and weak right radial pulsations in 2 cases.
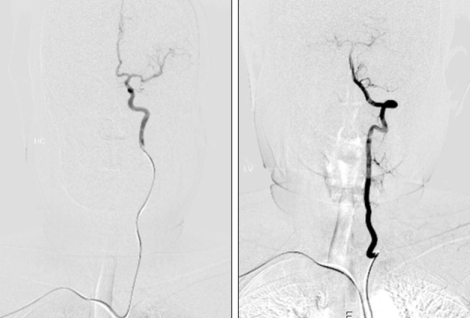
Fig. 2.
Selective catheterized angiography of the left internal carotid artery and left vertebral artery.
Access of the radial artery was not achieved in 65 of 1,240 patients (5.2%). This was attributed to failure of the radial puncture in 51 patients, lack of collateral blood supply via the ulnar artery in 5 patients, radial artery occlusion in 4 patients, loop formation at the proximal end of the radial artery in 3 patients, and severe vasospasm of the radial artery following multiple puncture trials in 2 patients (Fig. 3). A successful transfemoral approach was used for 62 of these 65 cases, with a successful left transradial approach in 2 cases, and a right transulnar approach in 1 case. In one patient, the right radial artery puncture was failed, so we changed the access route to the left radial artery, which was subsequently successfully cannulated, but the procedure was terminated because a preexisting occlusion of the subclavian artery was found. In this case, a transfemoral approach was used to complete the examination.
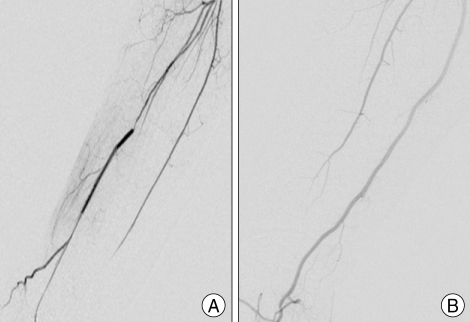
Fig. 3.
Forearm angiography. A : Severe vasospasm of the radial artery following multiple punctures. This could not be resolved by injection of spasmolytic medication. B : Radial artery occlusion after the previous procedure. Transfemoral angiography was performed for both patients.
The mean duration of the procedure was 28 minutes (range, 15-90 minutes). Compared to our standard transfemoral cerebral angiography technique, the procedure time for the transradial approach was almost the same. However, it took about 10 minutes longer to complete the procedure via the transradial approach among patients requiring evaluation of their left ICAs or left VAs.
The procedure was performed more than twice in 73 patients (5.9%). Two procedures using the same radial artery were performed in 64 patients (5.2%), three procedures in 7 patients (0.6%) and four procedures in 2 patients (0.2%). Among these patients, radial artery occlusion was demonstrated in 4 patients (5.4%) on the follow-up cerebral angiography.
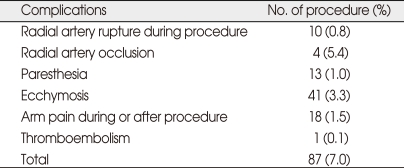
Vasospasm of the radial artery was noted in 174 of the 1,240 procedures (14%). All intra-procedural spasms, except in two cases, could be effectively resolved with the cocktail solution. Minor peri-procedural complications occurred in 87 (7.0%) of these patients, none of whom had permanent sequelae. Details of the complications are demonstrated in Table 1. Procedure-related vascular complications, such as hand ischemia, significant local hematoma, pseudoaneurysm, arteriovenous fistula or functional disability of the hand were not demonstrated in our series. Symptomatic thromboembolism developed in one patient suffering from new-onset left-sided weakness following the procedure. However, the symptom was improved after 1 day without sequelae.
Table 1.
Details of complications
In all patients, the radial artery was pulsatile and the modified Allen test was negative immediately following the procedure, as well as 2 weeks after the procedure. No patients experienced functional disability of the hand, and none reported any discomfort.
DISCUSSION
The transradial approach has a number of theoretical and potential advantages over the transfemoral approach for cerebral angiography. First, the radial artery is easily compressible, thus bleeding can be well controlled, and hemorrhagic complications are significantly minimized. Second, there are no large adjacent major nerves or veins that could be disrupted during the procedure, and the radial artery's relatively fixed position decreases the risk of injuring these structures. Third, the procedure does not require bed rest, allowing for immediate ambulation, which improves the quality of life for the patients. Finally, the transradial approach saves costs as the necessary materials are less expensive, and the patient should not require hospitalization after the procedure1,3,8). Despite these advantages, the transradial approach is more challenging in terms of feasibility and technical success compared to the transfemoral approach, because it also leads to a higher proportion of procedural failures.
The success rate of transradial cerebral angiography is reportedly to be 92.7-99%8,11,17,18,25). The success rate of the transradial approach for the evaluation of cerebrovascular diseases in the present study was 94.8%, which is consistent with previously reported success rates. The main reason for failure in our study was a failed radial puncture. In the initial report of this technique, Campeau noted puncture or cannulation failures (likely because of the use of highprofile catheters) in 10% of patients4). Our failure rate in securing radial access was 5.2%, and was mostly due to puncture errors, though most of these errors occurred during the initial period of the study, when the operators were less experienced with the technique. As the transradial access technique is technically somewhat difficult and challenging, its success increases as learning increases. Although a certain learning curve exists, with sufficient experience, the success rate of the transradial approach improves.
Other causes of failure included severe vasospasm of the radial artery, a lack of collateral blood supply via the ulnar artery, anatomic variation of the artery such as tortuosity and stenosis, an occlusion at the subclavian artery, and congenital abnormalities, such as radioulnar loops and hypoplasia2,5,8,24). In the present study, we failed to initiate the procedure for a total of 12 patients due to reasons other than puncture failure. Our rate of access failure was comparable to rates reported in previous studies12,13,17).
The radial artery is known to be vasoreactive and to have a tendency for spasm, so it is important to achieve entry with the first puncture, although the puncture of this relatively small-caliber artery is not always easy. Furthermore, it is important to administer spasmolytic medication (isosorbide dinitrate, verapamil) intra-arterially immediately after puncture. In our series, vasospasm of the radial artery complicated catheterization in only 2 cases. Most vasospasms in the radial artery were resolved with spasmolytic medication.
In our study, the procedure was performed more than twice in the same arm in 73 patients, and up to 4 times in 2 patients. Repeated cerebral angiography is often necessary for some conditions, such as for follow-ups after percutaneous translumial angioplasty and stenting, or coil embolization of cerebral aneurysms. The transradial approach, which causes less patient stress than the transfemoral approach, would be useful for such cases. However, stenosis and occlusion resulting from previous procedures limits the use of the transradial approach repeatedly in the same vessel, so careful consideration must be taken in such cases.
Radial artery occlusion is not only a major concern, but also important complication after transradial procedures. Radial artery occlusion after transradial coronary angiography and intervention has been reported to occur in 2 to 10% of patients4,9,15,22,23). The explanation for why some patients develop occlusion is unknown. Some authors have emphasized that radial artery occlusion may be related to prolonged cannulation, the small diameter of the radial artery, the ratio of the radial artery diameter to the sheath outer diameter, and to the anticoagulation used during arterial cannulation22,26). The mean radial artery internal diameter is 3.1 ± 0.60 mm in men and 2.8 ± 0.60 mm in women21). In our study, the mean diameter of the radial artery in men and women were similar to those reported previously, and were not associated with subsequent radial artery occlusion. While radial occlusion is usually asymptomatic because of the presence of extensive ulnar collateral supply, the permanent loss of the radial arterial supply is undesirable.
Numerous previous studies have demonstrated that the rate of puncture-related complications is very low for transradial procedures. Authors have experienced some minor peri-procedural complications; however, no permanent complications were observed. Although the radial artery approach is associated with a low morbidity rate, potential complications include digital ischemia, arterial dissection, pseudoaneurysm formation, arterial occlusion, and arteriovenous fistulae formation7). Unlike transradial coronary angiography, transradial cerebral angiography has one relatively significant limitation; if a selection of the left ICA or left VA is required, a right transradial procedure may be more challenging in some patients. Left ICAs were sometimes more difficult to catheterize in patients with high tortuosity of the angles between the right brachiocephalic artery and the ascending aorta. The left VA was also difficult to engage because of the sharp angles between the left subclavian artery and the origin of left VA, and also because of the mismatch between the shape of the catheter and the origin of the left VA. Lee et al.12) reported successful catheterization rates of left ICA (84.1%) and left VA (58.6%). They suggested that a modification of the catheter design for the left ICA and left VA is required to improve vessel selectivity.
Limitations
The primary limitation of the current study was that we did not evaluate the long-term patency of the radial arteries of our patients in order to determine the incidence of radial artery occlusion. Therefore, the rate of asymptomatic radial artery occlusion cannot be determined. Secondly, our study employed three operators, so the rates of minor complications may have depended on the skill level and procedural knowledge of each operator. Thus, we speculate a relatively higher rate of minor complications and procedural failure, resulting from procedures completed by clinicians early in the process of learning the procedure.
CONCLUSION
The results of our study suggest that a transradial approach for cerebral angiography has a high diagnostic success rate and can be performed with a minimal risk of morbidity. Therefore, it could be used as a routine procedure. In particular, transradial procedures might be useful for follow-up angiographies, as it is more straightforward and creates less stress for the patients.
References
- 1.Agostoni P, Biondi-Zoccai GG, de Benedictis ML, Rigattieri S, Turri M, Anselmi M, et al. Radial versus femoral approach for percutaneous coronary diagnostic and interventional procedures; Systematic overview and meta-analysis of randomized trials. J Am Coll Cardiol. 2004;44:349–356. doi: 10.1016/j.jacc.2004.04.034. [DOI] [PubMed] [Google Scholar]
- 2.Bendok BR, Przybylo JH, Parkinson R, Hu Y, Awad IA, Batjer HH. Neuroendovascular interventions for intracranial posterior circulation disease via the transradial approach : technical case report. Neurosurgery. 2005;56:E626. doi: 10.1227/01.NEU.0000154820.28342.38. discussion E626. [DOI] [PubMed] [Google Scholar]
- 3.Benit E, Vranckx P, Jaspers L, Jackmaert R, Poelmans C, Coninx R. Frequency of a positive modified Allen's test in 1,000 consecutive patients undergoing cardiac catheterization. Cathet Cardiovasc Diagn. 1996;38:352–354. doi: 10.1002/(SICI)1097-0304(199608)38:4<352::AID-CCD5>3.0.CO;2-6. [DOI] [PubMed] [Google Scholar]
- 4.Campeau L. Percutaneous radial artery approach for coronary angiography. Cathet Cardiovasc Diagn. 1989;16:3–7. doi: 10.1002/ccd.1810160103. [DOI] [PubMed] [Google Scholar]
- 5.Esente P, Giambartolomei A, Simons AJ, Levy C, Caputo RP. Overcoming vascular anatomic challenges to cardiac catheterization by the radial artery approach : specific techniques to improve success. Catheter Cardiovasc Interv. 2002;56:207–211. doi: 10.1002/ccd.10233. [DOI] [PubMed] [Google Scholar]
- 6.Fessler RD, Wakhloo AK, Lanzino G, Guterman LR, Hopkins LN. Transradial approach for vertebral artery stenting : technical case report. Neurosurgery. 2000;46:1524–1527. doi: 10.1097/00006123-200006000-00044. discussion 1527-1528. [DOI] [PubMed] [Google Scholar]
- 7.Hildick-Smith DJ, Lowe MD, Walsh JT, Ludman PF, Stephens NG, Schofield PM, et al. Coronary angiography from the radial artery--experience, complications and limitations. Int J Cardiol. 1998;64:231–239. doi: 10.1016/s0167-5273(98)00074-6. [DOI] [PubMed] [Google Scholar]
- 8.Iwasaki S, Yokoyama K, Takayama K, Ueda K, Sueyosi S, Nagasawa M, et al. The transradial approach for selective carotid and vertebral angiography. Acta Radiol. 2002;43:549–555. doi: 10.1080/j.1600-0455.2002.430601.x. [DOI] [PubMed] [Google Scholar]
- 9.Kiemeneij F, Laarman GJ, de Melker E. Transradial artery coronary angioplasty. Am Heart J. 1995;129:1–7. doi: 10.1016/0002-8703(95)90034-9. [DOI] [PubMed] [Google Scholar]
- 10.Kiemeneij F, Laarman GJ, Odekerken D, Slagboom T, van der Wieken R. A randomized comparison of percutaneous transluminal coronary angioplasty by the radial, brachial and femoral approaches: the access study. J Am Coll Cardiol. 1997;29:1269–1275. doi: 10.1016/s0735-1097(97)00064-8. [DOI] [PubMed] [Google Scholar]
- 11.Kim JH, Park YS, Chung CG, Park KS, Chung DJ, Kim HJ. Feasibility and utility of transradial cerebral angiography : experience during the learning period. Korean J Radiol. 2006;7:7–13. doi: 10.3348/kjr.2006.7.1.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee DH, Ahn JH, Jeong SS, Eo KS, Park MS. Routine transradial access for conventional cerebral angiography : a single operator's experience of its feasibility and safety. Br J Radiol. 2004;77:831–838. doi: 10.1259/bjr/89933527. [DOI] [PubMed] [Google Scholar]
- 13.Levy EI, Boulos AS, Fessler RD, Bendok BR, Ringer AJ, Kim SH, et al. Transradial cerebral angiography : an alternative route. Neurosurgery. 2002;51:335–340. discussion 340-342. [PubMed] [Google Scholar]
- 14.Lotan C, Hasin Y, Mosseri M, Rozenman Y, Admon D, Nassar H, et al. Transradial approach for coronary angiography and angioplasty. Am J Cardiol. 1995;76:164–167. doi: 10.1016/s0002-9149(99)80050-2. [DOI] [PubMed] [Google Scholar]
- 15.Louvard Y, Krol M, Pezzano M, Sheers L, Piechaud JF, Marien C, et al. Feasibility of routine transradial coronary angiography : a single operator's experience. J Invasive Cardiol. 1999;11:543–548. [PubMed] [Google Scholar]
- 16.Ludman PF, Stephens NG, Harcombe A, Lowe MD, Shapiro LM, Schofield PM, et al. Radial versus femoral approach for diagnostic coronary angiography in stable angina pectoris. Am J Cardiol. 1997;79:1239–1241. doi: 10.1016/s0002-9149(97)00089-1. [DOI] [PubMed] [Google Scholar]
- 17.Matsumoto Y, Hongo K, Toriyama T, Nagashima H, Kobayashi S. Transradial approach for diagnostic selective cerebral angiography : results of a consecutive series of 166 cases. AJNR Am J Neuroradiol. 2001;22:704–708. [PMC free article] [PubMed] [Google Scholar]
- 18.Nohara AM, Kallmes DF. Transradial cerebral angiography : technique and outcomes. AJNR Am J Neuroradiol. 2003;24:1247–1250. [PMC free article] [PubMed] [Google Scholar]
- 19.Park SH, Park JC, Hwang JH, Hwang SK, Hamm IS. Role of Three-dimensional computed tomography angiography in the follow-up of patients with aneurysm clips. J Korean Neurosurg Soc. 2006;39:427–431. [Google Scholar]
- 20.Ricci MA, Trevisani GT, Pilcher DB. Vascular complications of cardiac catheterization. Am J Surg. 1994;167:375–378. doi: 10.1016/0002-9610(94)90119-8. [DOI] [PubMed] [Google Scholar]
- 21.Saito S, Ikei H, Hosokawa G, Tanaka S. Influence of the ratio between radial artery inner diameter and sheath outer diameter on radial artery flow after transradial coronary intervention. Catheter Cardiovasc Interv. 1999;46:173–178. doi: 10.1002/(SICI)1522-726X(199902)46:2<173::AID-CCD12>3.0.CO;2-4. [DOI] [PubMed] [Google Scholar]
- 22.Saito S, Miyake S, Hosokawa G, Tanaka S, Kawamitsu K, Kaneda H, et al. Transradial coronary intervention in Japanese patients. Catheter Cardiovasc Interv. 1999;46:37–41. doi: 10.1002/(SICI)1522-726X(199901)46:1<37::AID-CCD10>3.0.CO;2-Y. [DOI] [PubMed] [Google Scholar]
- 23.Sakai H, Ikeda S, Harada T, Yonashiro S, Ozumi K, Ohe H, et al. Limitations of successive transradial approach in the same arm: the Japanese experience. Catheter Cardiovasc Interv. 2001;54:204–208. doi: 10.1002/ccd.1268. [DOI] [PubMed] [Google Scholar]
- 24.Valsecchi O, Vassileva A, Musumeci G, Rossini R, Tespili M, Guagliumi G, et al. Failure of transradial approach during coronary interventions : anatomic considerations. Catheter Cardiovasc Interv. 2006;67:870–878. doi: 10.1002/ccd.20732. [DOI] [PubMed] [Google Scholar]
- 25.Wu CJ, Hung WC, Chen SM, Yang CH, Chen CJ, Cheng CI, et al. Feasibility and safety of transradial artery approach for selective cerebral angiography. Catheter Cardiovasc Interv. 2005;66:21–26. doi: 10.1002/ccd.20396. [DOI] [PubMed] [Google Scholar]
- 26.Yokoyama N, Takeshita S, Ochiai M, Koyama Y, Hoshino S, Isshiki T, et al. Anatomic variations of the radial artery in patients undergoing transradial coronary intervention. Catheter Cardiovasc Interv. 2000;49:357–362. doi: 10.1002/(sici)1522-726x(200004)49:4<357::aid-ccd1>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]