Abstract
Intracranial granulocytic sarcomas are rare tumors, which are composed of immature granulocytic cells. Although it has been well known that these tumors are associated with acute myeloblastic leukemia (AML), they have been almost always related to bone marrow relapse. However, isolated recurrence of granulocytic sarcoma following complete remission from prior AML is extremely rare, especially in the central nervous system. A 44-year-old male presented with isolated recurrence of granulocytic sarcoma mimicking a falx meningioma two years after complete remission by allogenic peripheral blood stem cell transfusion (PBSCT) in the acute myelomonoblastic leukemia (FAB, M4). Because of depressed mental state and mass effect, total surgical resection was performed. Pathological findings were compatible with the granulocytic sarcoma. There was no evidence of leukemic relapse in the peripheral blood. We suggest that this phenomenon can be explained by the hypothesis that a certain barrier effect such as blood brain barrier might lead to the proliferation of intracranial leukemic cells which metastasized before PBSCT.
Keywords: Chloroma, Granulocytic sarcoma, Leukemia
INTRODUCTION
Granulocytic sarcoma, of which synonyms are chloroma, myeloblastoma and extramedullary leukemia, is a localized solid mass composed of immature granulocytic cells. Granulocytic sarcoma usually occurs as a complication of acute myeloblastic leukemia (AML), myelodysplastic syndrome, or myeloproliferative disorders1,8,10). It may affect any part of the body such as skin, bone, and soft tissue including central nervous system (CNS)7,10,13,16). Although it has been already reported that granulocytic sarcoma has a relationship with acute myeloblastic leukemia2), isolated recurrence in the CNS after complete remission has been very rare3).
Here, we described a rare case of isolated recurrence of granulocytic sarcoma mimicking a falx meningioma as a first sign of relapse with review of the literature.
CASE REPORT
A 44-year-old male patient presented to the neurosurgical unit complaining of confusion and headache, which were associated with occasional nausea and vomiting. In the past history of the patient, he was originally treated for acute myelomonoblastic leukemia (FAB, M4) 3 years prior to admission. Cytogenetic analysis of leukemic cells showed a 46, XY, inv 16, del (11q23) karyotype. At that time, he underwent induction chemotherapy with AI 7 + 3 (Ara-C 100 mg/m2, Idarubicin 12 mg/m2) followed by 3 cycles of consolidation chemotherapy with high dose Ara-C (Ara-C 3 g/m2), which resulted in complete remission. However, one year later, he revealed relapse in the regular follow up of peripheral blood examination. Therefore, he received allogenic peripheral blood stem cell transfusion (PBSCT) and remained in complete remission for two years.
At present admission, he was drowsy and confused. Peripheral blood examinations including complete blood count (CBC) were within normal limit with no blast. Computed tomography (CT) scans showed a round high density mass in the genu of the corpus callosum with strong enhancement, which was attached to the anterior falx (Fig. 1). In the brain magnetic resonance images (MRI), the lesion demonstrated low signal intensity on T1-weighted images and heterogenous signal intensity on T2-weighted images. After gadolinium administration, the mass showed strong enhancement (Fig. 2). These radiologic findings were compatible with falx meningioma. However, considering the medical history of this patient, we included the granulocytic sarcoma in the differential diagnosis. The patient underwent open surgery through interhemispheric approach. The mass was well-encapsulated and not attached to the falx. The tumor was pinkish in color and friable in consistency. Complete removal of the tumor was achieved by microsurgical dissection. Histological examination revealed that the tumor was composed of proliferation of myeloblast, which was compatible with granulocytic sarcoma. In the immunophenotyping and cytochemical studies, the blast cells were positive for CD68 and C-kit, consistent with relapse of AML (Fig. 3).
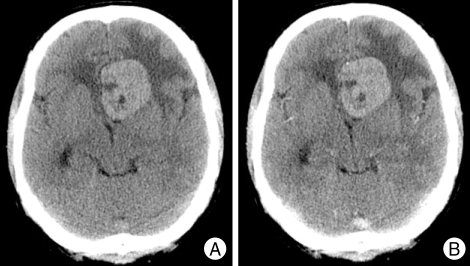
Fig. 1.
Preoperative computed tomography (CT) scans. A : Non-contrast enhanced CT image demonstrates a round high density mass in the left frontal lobe. B : This lesion shows strong enhancement after administration of contrast.
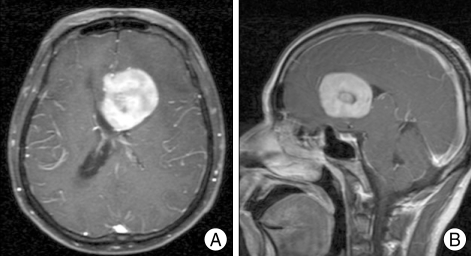
Fig. 2.
Preoperative magnetic resonance images (MRI). Gadolinium enhanced T1-weighted axial (A) and sagittal (B) MRI show a well-enhancing round mass in the genu of the corpus callosum, which was attached to the anterior falx.
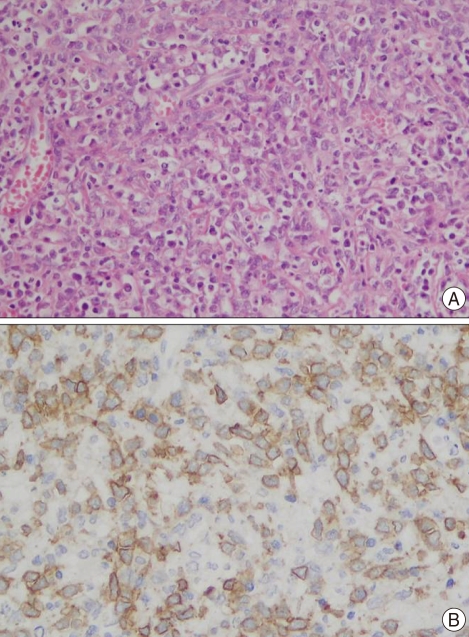
Fig. 3.
Histological examination reveals proliferation of atypical myeloblasic cells and some eosinophilic promyelocytes, which is compatible with granulocytic sarcoma (H & E,×200). B : Immunohistochemical study shows strong positive myeloperoxidase (CD68 stain).
Postoperatively, he regained consciousness and his headache was markedly improved. Therefore, we planned to perform bone marrow biopsy for the evaluation of recurrence of leukemia. However, the patient refused additional bone marrow biopsy. His peripheral blood examinations including CBC remained still within normal limit without any evidence of leukemic relapse. Therefore, we suggested that his intracranial tumor was an isolated recurrence of granulocytic sarcoma. One year after the conventional radiotherapy, he has remained complete remission state and brain MRI demonstrated no radiographic evidence of recurrent intracranial lesion (Fig. 4).
Fig. 4.
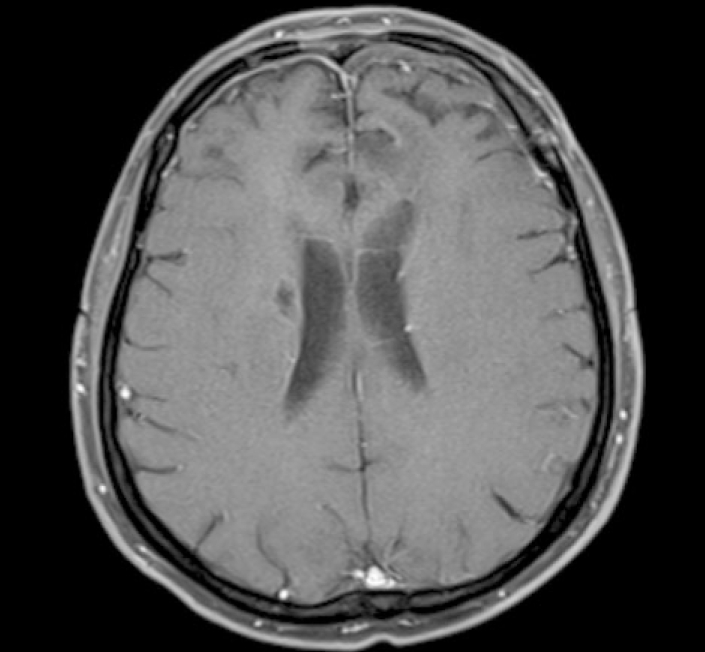
Magnetic resonance image performed one year later demonstrates no residual and recurrent tumor in the operative site.
DISCUSSION
Granulocytic sarcoma, also called chloroma, is a solid tumor composed of immature granulocytic cells. The term 'chloroma' has been derived from the Greek word chloros (green) because of the typical greenish appearance of the lesion. The green color of this tumor is originated from the high expression of myeloperoxidase, but it is not always expressed because it rapidly fades by exposure to oxygen15).
It has been well known that granulocytic sarcoma occurs primarily in patients with AML, myeloproliferative and myelodysplastic syndrome1,8,10) and, which has been almost always followed by bone marrow relapse after 1-19 months12). However, isolated recurrence of granulocytic sarcoma following complete remission from prior AML is extremely rare3).
Although granulocytic sarcoma affects extracranial sites more commonly than the CNS, manifestations of AML in the CNS have been more frequent as results of improved antileukemic therapy and longer remission in the patients with AML18). Signs and symptoms of CNS granulocytic sarcoma are nonspecific and related to increased intracranial pressure or mass effect. Radiographic features of CNS granulocytic sarcoma are typically characterized by isodense or hyperdense mass on precontrast CT scan with bright homogenous enhancement on postcontrast scans17). In the MRI, granulocytic sarcomas are usually hypointense to isotense on both T1-weighted and T2-weighted images with marked enhancement following contrast administration4,14).
The pathogenesis of isolated recurrence of intracranial granulocytic sarcoma without bone marrow relapse is unknown. However, from the result of current study, we suggest the following hypothesis. Although the PBSCT is applied systemically, it may not be able to affect the CNS because of a certain barrier such as blood brain barrier. This limitation could later lead to the proliferation of intracranial tumor cells which metastasized before PBSCT. Therefore, we speculate that periodic regular brain imaging studies should be performed following PBSCT.
The development of granulocytic sarcoma in the leukemia almost always heralds an impending blast crisis9). Therefore, early recognition of granulocytic sarcoma is important. In the therapeutic strategy, although response to the external radiation has been well documented, the best treatment option for the granulocytic sarcoma includes antileukemic chemotherapy containing Ara-C in higher doses5,6). The advantage of surgical excision still remains controversial. It has been reported that surgical excision has no benefit following chemotherapy and irradiation, except in the presence of progressive neurological deficits such as increasing intracranial pressure or disturbance of consciousness which are uncontrollable by the conservative treatment11). Surgical resection and/or irradiation, although highly effective in local control, do not influence survival6). Moreover, surgery would increase the risk of infection and CNS dissemination11). However, some reports noted that surgical decompression might provide rapid improvement and lead to a long symptom-free period19). In our case, because of depressed mental state, he underwent surgical resection followed by radiotherapy. Since there was no systemic relapse, except CNS lesion in our case, we did not perform any more chemotherapy.
CONCLUSION
We suggest that granulocytic sarcoma of CNS may be the first or the only sign of relapse in the patient with complete remission from the AML. The best result can be achieved by the early pathological diagnosis and multimodal treatment including surgery and radiotherapy.
Acknowledgements
This work was supported by clinical research grant from Pusan National University Hospital 2009.
References
- 1.Byrd JC, Edenfield WJ, Dow NS, Aylesworth C, Dawson N. Extramedullary myeloid cell tumors in myelodysplastic-syndromes : not a true indication of impending acute myeloid leukemia. Leuk Lymphoma. 1996;21:153–159. doi: 10.3109/10428199609067593. [DOI] [PubMed] [Google Scholar]
- 2.Byrd JC, Edenfield WJ, Shields DJ, Dawson NA. Extramedullary myeloid cell tumors in acute nonlymphocytic leukemia : a clinical review. J Clin Oncol. 1995;13:1800–1816. doi: 10.1200/JCO.1995.13.7.1800. [DOI] [PubMed] [Google Scholar]
- 3.Byrd JC, Weiss RB. Recurrent granulocytic sarcoma. An unusual variation of acute myelogenous leukemia associated with 8;21 chromosomal translocation and blast expression of the neural cell adhesion molecule. Cancer. 1994;73:2107–2112. doi: 10.1002/1097-0142(19940415)73:8<2107::aid-cncr2820730815>3.0.co;2-w. [DOI] [PubMed] [Google Scholar]
- 4.Freedy RM, Miller KD., Jr Granulocytic sarcoma (chloroma) : sphenoidal sinus and paraspinal involvement as evaluated by CT and MR. AJNR Am J Neuroradiol. 1991;12:259–262. [PMC free article] [PubMed] [Google Scholar]
- 5.Huter O, Brezinka C, Nachbaur D, Schwaighofer H, Lang A, Niederwieser D. Successful treatment of primary extramedullary leukemia (EML) of the uterus with radical therapy, chemotherapy, autologous bone marrow transplantation (bmt) and prophylactic local irradiation. Bone Marrow Transplant. 1996;18:663–664. [PubMed] [Google Scholar]
- 6.Imrie KR, Kovacs MJ, Selby D, Lipton J, Patterson BJ, Pantalony D, et al. Isolated chloroma : the effect of early antileukemic therapy. Ann Int Med. 1995;123:351–353. doi: 10.7326/0003-4819-123-5-199509010-00005. [DOI] [PubMed] [Google Scholar]
- 7.Koehler M. Granulocytic sarcoma of the stomach. Gastrointest Endosc. 1998;48:190. doi: 10.1016/s0016-5107(98)70162-2. [DOI] [PubMed] [Google Scholar]
- 8.Mahendra P, Ager S, Bedlow AJ, Bloxham DM, Green AR, Marcus RE. Two unusual neurological presentations of granulocytic sarcoma in Philadelphia positive chronic myeloid leukemia. Leuk Lymphoma. 1994;15:351–355. doi: 10.3109/10428199409049735. [DOI] [PubMed] [Google Scholar]
- 9.Meis JM, Butler JJ, Osborne BM, Manning JT. Granulocytic sarcoma in nonleukemic patients. Cancer. 1986;58:2697–2709. doi: 10.1002/1097-0142(19861215)58:12<2697::aid-cncr2820581225>3.0.co;2-r. [DOI] [PubMed] [Google Scholar]
- 10.Neiman RS, Barcos M, Berard C, Bonner H, Mann R, Rydell RE, et al. Granulocytic sarcoma : a clinicopathologic study of 61 biopsied cases. Cancer. 1981;48:1426–1437. doi: 10.1002/1097-0142(19810915)48:6<1426::aid-cncr2820480626>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 11.Nishimura S, Kyuma Y, Kamijo A, Maruta A. Isolated recurrence of granulocytic sarcoma manifesting as extra- and intracranial masses--case report. Neurol Med Chir (Tokyo) 2004;44:311–316. doi: 10.2176/nmc.44.311. [DOI] [PubMed] [Google Scholar]
- 12.Parker K, Hardjasudarma M, McClellan RL, Fowler MR, Milner JW. MR features of an intracerebellar chloroma. AJNR Am J Neuroradiol. 1996;17:1592–1594. [PMC free article] [PubMed] [Google Scholar]
- 13.Pomerantz SJ, Hawkins HH, Towbin R, Lisberg WN, Clark RA. Granulocytic sarcoma (chloroma) : CT manifestations. Radiology. 1985;155:167–170. doi: 10.1148/radiology.155.1.3856292. [DOI] [PubMed] [Google Scholar]
- 14.Pui MH, Fletcher BD, Langston JW. Granulocytic sarcoma in childhood leukemia : imaging features. Radiology. 1994;190:698–702. doi: 10.1148/radiology.190.3.8115614. [DOI] [PubMed] [Google Scholar]
- 15.Sandhu GS, Ghufoor K, Gonzalez-Garcia J, Elexpuru-Camiruaga JA. Granulocytic sarcoma presenting as cauda equine syndrome. Clin Neurol Neurosurg. 1998;100:205–208. doi: 10.1016/s0303-8467(98)00021-3. [DOI] [PubMed] [Google Scholar]
- 16.Sao IS, Hull MT, Pak HY. Granulocytic sarcoma of the cervix as a primary manifestation : case without overt leukemia features for 26 months. Cancer. 1977;40:3030–3037. doi: 10.1002/1097-0142(197712)40:6<3030::aid-cncr2820400640>3.0.co;2-#. [DOI] [PubMed] [Google Scholar]
- 17.Sowers JJ, Moody DM, Naidich TP, Ball MR, Laster DW, Leeds NE. Radiographic features of granulocytic sarcoma (chloroma) J Comput Assist Tumogr. 1979;3:226–233. doi: 10.1097/00004728-197904000-00015. [DOI] [PubMed] [Google Scholar]
- 18.Stork JT, Cigtay OS, Schellinger D, Jacobson RJ. Recurrent chloromas in acute myelogenous leukemia. AJR Am J Roentgenol. 1984;142:777–778. doi: 10.2214/ajr.142.4.777. [DOI] [PubMed] [Google Scholar]
- 19.Yamamoto K, Hamaguchi H, Nagata H, Hara M, Tone O, Tomita H, et al. Isolated recurrence of granulocytic sarcoma of the brain : successful treatment with surgical resection, intrathecal injection, irradiation and prophylactic systemic chemotherapy. Jpn J Clin Oncol. 1999;29:214–218. doi: 10.1093/jjco/29.4.214. [DOI] [PubMed] [Google Scholar]