Abstract
Trochlear nerve palsy associated with spontaneous subarachnoid hemorrhage (SAH) is known to be a rare malady. We report here on a patient who suffered with left trochlear nerve palsy following rupture of a right posterior communicating artery aneurysm. A 56-year-woman visited our emergency department with stuporous mental change. Her Hunt-and-Hess grade was 3 and the Fisher grade was 4. Cerebral angiography revealed a ruptured aneurysm of the right posterior communicating artery. The aneurysm was clipped via a right pterional approach on the day of admission. The patient complained of diplopia when she gazed to the left side, and the ophthalmologist found limited left inferolateral side gazing due to left superior oblique muscle palsy on day 3. Elevated intracranial pressure, intraventricular hemorrhage or a dense clot in the basal cisterns might have caused this trochlear nerve palsy.
Keywords: Posterior communicating artery aneurysm, Trochlear nerve paresis, Subarachnoid hemorrhage
INTRODUCTION
There have been several reports on cranial nerve palsies related to extraocular movement and their association with spontaneous subarachnoid hemorrhage (SAH). In particular, oculomotor and abducens nerve palsies following SAH have been frequently reported on. However, trochlear nerve palsy associated with SAH represents a rare clinical entity. We present here an interesting case of isolated contralateral trohlear nerve palsy as one of symptoms of a ruptured aneurysm of the posterior communicating artery.
CASE REPORT
A 56-year-old woman was referred to our emergency department with a stuporous mentality. She showed a Glasgow Coma Scale Score (GCS) of 7 points (eye opening 1, verbal response 1 and motor response 5) with a symmetric muscle power grade of IV/V. The left pupil was 4 mm in diameter and it was nonreactive to light; the right pupil was 3 mm in diameter and it was reactive to light. The presence or absence of extra-ocular movement dysfunction and ptosis could not be examined because of the patient's altered consciousness.
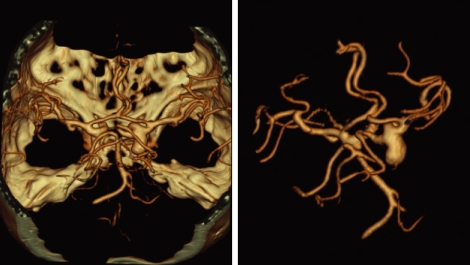
A computed tomography (CT) scan of the head confirmed the SAH with dense clots in the suprasellar, prepontine, ambient, quadrigeminal and both sylvian cisterns, and there was intra-ventricular hemorrhage (IVH) with a high density in the 3rd and 4th ventricles (Fig. 1). Cerebral CT angiography was subsequently performed, which demonstrated a ruptured right posterior communicating artery aneurysm. The ruptured aneurysm was 2 × 1 × 1 cm in size, and it was directed to the infero-postero-medial side and it was the saccular type (Fig. 2).
Fig. 1.
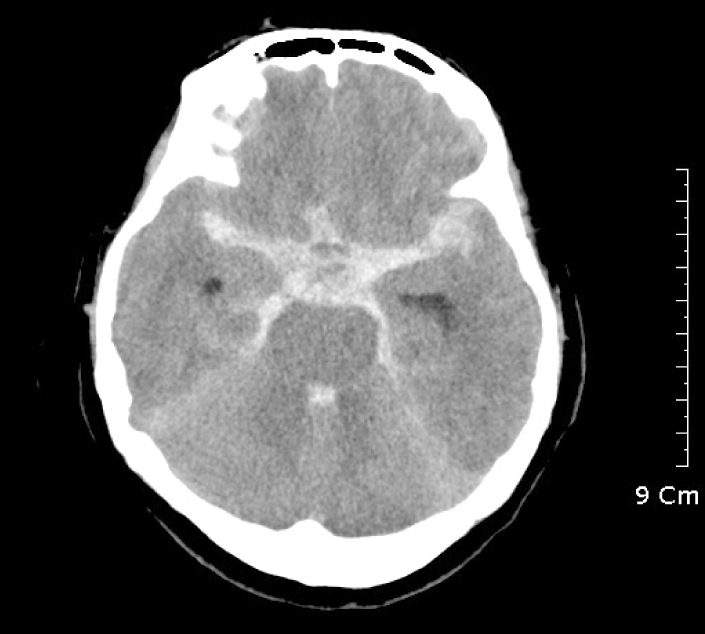
Brain CT on admission. Subarachnoid hemorrhage (SAH) with dense clots in suprasellar cistern, prepontine cistern, ambient cistern, quadrigeminal cistern and both sylvian cisterns, and intra-ventricular hemorrhage (IVH) is present in the third and fourth ventricles.
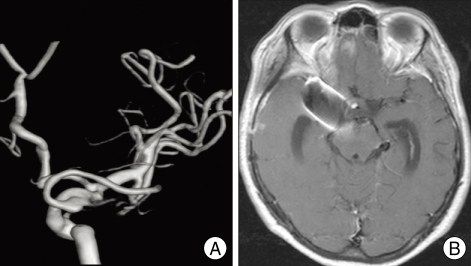
Fig. 2.
Cerebral CT angiography. The right posterior communicating artery aneurysm, a saccular type, is 2×1×1 cm in size, and it is directed to the infero-posterio-medial side. A junctional dilatation of the left posterior communicating artery is also demonstrated.
Shortly after the CT angiography and 3 hours after the onset of mental change, we clipped the aneurysm via a right pterional approach, and rupture of this aneurysm was confirmed intraoperatively.
The immediate postoperative mental status was still stuporous, but both pupils were reduced to 3 mm in diameter and they were reactive to light. She could clearly obey to our commands on the day after craniotomy.
She complained of diplopia when she gazed downward or to the left side on day 3. The ophthalmologist evaluated her ocular signs via an alternative cover test and a diplopia test, and he found an eso-deviated left eyeball and limited left inferolateral side gazing due to left superior oblique muscle palsy.
She recovered uneventfully except for the persistent left trochlear nerve palsy. A follow-up transfemoral cerebral angiogram (TFCA) was performed on day 14 and magnetic resonance imaging (MRI) was done on day 22. There was neither residual aneurysmal neck or sac on the TFCA, nor any abnormal brain parenchymal lesion on MRI (Fig. 3).
Fig. 3.
Follow up TFCA (A) and brain MRI (B). TFCA (A) reveals no residual aneurysmal sac or vascular abnormality. The brain MRI (B) demonstrates no brain parenchymal lesion. TFCA : transfemoral cerebral angiogram.
The signs of left trochlear nerve paresis gradually resolved during the 90 days of the follow up period.
DISCUSSION
The very thin trochlear nerve, consisting of 1,700 to 3,400 fibers, has the longest intracranial course of all the cranial nerves and it has a very slender connection to the brain stem. This morphology accounts for its fragility and susceptibility to trauma or various intracranial lesions10,12,16). The most common cause of acquired isolated fourth cranial nerve palsy is closed head injury3,6,13-15). Aneurysmal rupture is distinctly uncommon as a cause of trochlear nerve paresis, and this accounted for only 1.7% of all the fourth cranial nerve palsies in one study14).
Aneurysms of the ophthalmic artery, posterior communicating artery, internal carotid artery, basilar artery, superior cerebellar artery (SCA) and the posterior cerebral artery (PCA) have been documented to cause trochlear nerve palsy1,3,4,7,14). All of these reports noted the location of aneurysm may itself have placed pressure on the trochlear nerve. However, our patient is unusual in that the trochlear nerve palsy was isolated and it was on the side contralateral to the ruptured aneurysm.
A number of mechanisms have been postulated as potential causes of fourth cranial nerve palsy in patients with an intracranial aneurysm. The direct causes include local pressure by the aneurysm on the nerve or its midbrain nucleus, hemorrhagic dissection of the nerve and hemorrhage into the midbrain parenchyma, whereas the indirect causes include increased intracranial pressure (IICP) from an initial hemorrhage clot, edema or hydrocephalus, with subsequent displacement of the temporal lobes, PCA or SCA against the nerve2,8,9). Vasospasm has also been implicated as an indirect cause of trochlear nerve palsy7).
In our patient, the location of the aneurysm indicates that the palsy could not have been caused from direct pressure by the aneurysm on the trochlear nerve or the midbrain nucleus. Ischemic changes caused by vascular injury or direct dissection of the left trochlear nerve during surgery also seems unlikely. The surgical technique we used was the right pterional approach and the exposed nerves and arteries included the right optic nerve, internal carotid artery anterior choroidal artery and PCA, which are not a significant source of the blood supply to the extra-axial segments of the trochlear nerve. Midbrain parenchymal hemorrhage or infarction was also excluded because the postoperative MRI did not reveal any new lesion.
We can postulate several potential etiologies that alone or in combination may explain our patient's trochlear nerve plasy. The first potential pathogenesis is compression of nerve due to the IICP. Dysfunction of all the cranial nerves was reported in association with IICP with or without herniation11). Since there were several clinical reports of uncal herniation, including a non-reactive left pupil to light and a stuporous mentality on admission, compression of the left trochlear nerve against the tentorial edge can be a possible cause of trochlear nerve palsy. The second plausible mechanisms are believed to be compression of the trochlear nerve against the dura of the skull base, compression of the brainstem or stasis-ischemia of the trochlear nerve from a sudden intraventricular hematoma11). The third potential etiologic factor is compression of the trochlear nerves by a large subarachnoid blood clot within the perimesencepahlic cistern. This has previously been suggested as the mechanism for a unilateral third nerve palsy associated with a remote aneurysm. Cranial nerve palsy may result from the osmotic tonicity of the surrounding blood, the deleterious effects of the concentrated blood breakdown products or ischemia by the compression of the small nutrient arterioles of the nerve5). For our patient, the perimesencephalic clot on the left side, which was revealed on the initial CT, was large enough to warrant consideration of this mechanism as the cause of the patient's left fourth cranial nerve palsy.
The onset of trochlear nerve palsy in our case was obscure, and it wasn't certain whether or not it was combined with the pupil-dilated, third cranial nerve palsy on day 1 or it newly developed alone on day 3. Considering her mentality, it is more likely that the left fourth cranial nerve palsy was overlooked on admission. Initially there might have been pupil-dilated, third cranial nerve palsy and fourth cranial nerve palsy on the left side on admission, and third cranial nerve palsy was improved after clipping and CSF drainage. It has been suggested that a decreased ICP or wash-out of the dense clots from the basal cisterns is effective for treating cranial nerve palsy7).
Vasospasm of the feeding artery of the trochlear nerve is also a possible cause of trochlear nerve palsy. However, the early onset of the palsy shortly after the patient's ictus and that any other neurological signs and symptoms were lacking suggest that vasospasm, which typically has an onset at more than 3 days after SAH, was less likely to be the cause of our patient's condition.
Generally, cranial nerve palsy after SAH gradually improves in a natural course. Our patient's symptoms were also resolved during the 90 days of the follow up period.
CONCLUSION
We have described a patient who suffered a severe SAH after the rupture of a right posterior communicating artery aneurysm, with the clinical picture consisting of isolated, contralateral trochlear nerve palsy. Elevated intracranial pressure without herniation, direct nerve compression by intraventricular hematoma or damage by a large subarachnoid clot alone or in combination have all been suggested as possible mechanisms for this type of palsy.
References
- 1.Burger LJ, Kalvin NH, Smith JL. Acquired lesion of the fourth cranial nerve. Brain. 1970;93:567–574. doi: 10.1093/brain/93.3.567. [DOI] [PubMed] [Google Scholar]
- 2.Collins TE, Mehalic TF, White TK, Pezzuti RT. Trochlear nerve palsy as the sole initial sign of an aneurysm of the superior cerebellar aretery. Neurosurgery. 1992;30:258–261. doi: 10.1227/00006123-199202000-00020. [DOI] [PubMed] [Google Scholar]
- 3.Fahmy JA. Symptoms and signs of intracranial aneurysms with particular reference to retinal haemorrhage. Acta Ophthalmol (Copenh) 1972;50:129–136. doi: 10.1111/j.1755-3768.1972.tb03769.x. [DOI] [PubMed] [Google Scholar]
- 4.Hall JK, Jacobs DA, Movsas T, Galetta SL. Fourth nerve palsy, homonymous hemianopia, and hemisensory deficit caused by a proximal posterior cerebral artery aneurysm. J Neuroophthalmol. 2002;22:95–98. doi: 10.1097/00041327-200206000-00006. [DOI] [PubMed] [Google Scholar]
- 5.Hoya K, Kirino T. Traumatic trochlear nerve palsy following minor occipital impact--four case reports. Neurol Med Chir (Tokyo) 2000;40:358–360. doi: 10.2176/nmc.40.358. [DOI] [PubMed] [Google Scholar]
- 6.Kwartz J, Leatherbarrow B, Davis H. Diplopia following headinjury. Injury. 1990;21:351–352. doi: 10.1016/0020-1383(90)90116-c. [DOI] [PubMed] [Google Scholar]
- 7.Laun A, Tonn JC. Cranial nerve lesions following subarachnoid hemorrhage and aneurysm of the circle of Willis. Neurosug Rev. 1988;11:137–141. doi: 10.1007/BF01794677. [DOI] [PubMed] [Google Scholar]
- 8.Lee CH, Koh YC. Ruptured posterior communicating artery aneurysm causing bilateral abducens nerve paralyses - case report. J Korean Neurosurg Soc. 2000;29:426–429. [Google Scholar]
- 9.Mansour AM, Reinecke RD. Central trochlear palsy. Surv Ophthalmol. 1986;30:279–297. doi: 10.1016/0039-6257(86)90061-5. [DOI] [PubMed] [Google Scholar]
- 10.Marinković S, Gibo H, Zelić O, Nicodijević I. The neurovascular relationships and the blood supply of the trochlear nerve : surgical anatomy of its cisternal segment. Neurosurgery. 1996;38:161–169. doi: 10.1097/00006123-199601000-00036. [DOI] [PubMed] [Google Scholar]
- 11.Plum F, Posner JB. The diagnosis of stupor and coma. 3rd ed. Philadelphia: Fa Davis; 1980. pp. 113–114. [Google Scholar]
- 12.Prosst RL, Majetschak M. Traumatic unilateral trochlear nerve palsy. J Trauma. 2007;62:E1–E3. doi: 10.1097/01.ta.0000232057.36209.03. [DOI] [PubMed] [Google Scholar]
- 13.Rucker CW. The causes of paralysis of ther third, fourth, and sixth cranial nerves. Am J Ophthalmol. 1966;61:1293–1298. doi: 10.1016/0002-9394(66)90258-3. [DOI] [PubMed] [Google Scholar]
- 14.Rush JA, Younge BR. Paralysis of cranial nerves III, IV, and VI. Cause and prognosis in 1,000 cases. Arch Ophthalmol. 1981;99:76–79. doi: 10.1001/archopht.1981.03930010078006. [DOI] [PubMed] [Google Scholar]
- 15.von Noorden GK, Murray E, Wong SY. Superior oblique paralysis. A review of 270 cases. Arch Ophthalmol. 1986;104:1771–1776. doi: 10.1001/archopht.1986.01050240045037. [DOI] [PubMed] [Google Scholar]
- 16.Yasargil MG. Microneurosurgery I. Stuttgart: Georg Thieme Verlag; 1984. pp. 39–46.pp. 133–134. [Google Scholar]