Abstract
Background
A single axial image measured between the 4th and 5th lumbar vertebrae (L4-L5) is most frequently chosen to approximate total abdominal visceral adipose tissue (VAT) volume, but growing evidence suggests that this measurement site is not ideal.
Objective
The objective was to determine the single magnetic resonance (MR) image that best approximates the total VAT volume in a biracial sample of healthy subjects.
Design
We used contiguous abdominal MR images to measure VAT area and summed them to determine total VAT volume. The sample included 820 healthy men and women (n = 692 whites, 128 blacks) aged 18–88 y.
Results
A range of MR images had equally high correlations with total VAT in each race and sex group. The image 6 cm above L4-L5 (L4-L5 +6) was within the best equivalent range for all race and sex groups. The L4-L5 + 6 image crossed the L3 vertebra in 85% of subjects and crossed the L2-L3 intervertebral space or the L2 vertebra for 15% of subjects. Linear regression models indicated that the L4-L5 + 6 image explained 97% of the variance in total abdominal VAT volume, and additional covariates did not increase the R2 value significantly. The L4-L5 image explained 83% of the variance in VAT volume, and the covariates accounted for an additional 7% of the variance. Rank-order values for VAT can change if total VAT volume is approximated by a single image area. Whereas 25% of subjects changed rank by ≥10% with the L4-L5 image, only 3% changed rank to that degree with the L4-L5 + 6 image.
Conclusions
A single MR image located approximately at the L3 vertebra can accurately estimate total VAT volume in blacks and whites of both sexes.
Keywords: Visceral adipose tissue, subcutaneous adipose tissue, adipose tissue, adiposity, magnetic resonance imaging, race differences, sex differences
INTRODUCTION
Elevated visceral adipose tissue (VAT; adipose tissue deposited around the internal organs of the abdomen, trunk, and pelvis) is an independent risk factor for type 2 diabetes (1) and all-cause mortality (2), most likely because of its association with increased insulin resistance, dyslipidemia, and systemic inflammation (3–9). VAT is also highly responsive to exercise and dietary interventions (10–15) and to a variety of pharmaceuticals (16, 17). It is therefore increasingly desirable to find cost-effective methods to monitor changes in VAT in both clinical intervention and epidemiologic studies.
Magnetic resonance imaging (MRI) is a well-established validated method for the estimation of VAT that has the advantage of avoiding the exposure of subjects to ionizing radiation, as occurs with computed tomography (CT) (18–21). However, there is as yet no standardized protocol for the measurement of VAT with the use of MRI. Multiple image protocols allow for the estimation of total VAT mass, which is important given the high degree of intraindividual variation in VAT measured at different sites across the abdomen (22, 23). However, image analysis with the multiple-image approach is costly, and, for this reason, a single image (typically the L4-L5 image located at the intervertebral space between the 4th and 5th lumbar vertebrae and near the umbilicus) is often chosen to approximate total VAT volume (24). This convention stemmed from initial landmark studies reporting that the VAT area from the L4-L5 image had the highest correlation with total abdominal VAT volume (21, 25, 26). Many subsequent studies have suggested that images higher in the abdomen (around the L2-L3 region) have significantly greater predictive value for total VAT volume than do images around the L4-L5 region (27–30), but other studies continue to find that images from the L4-L5 region are the most predictive (23). Currently, the convention is to use the L4-L5 image to approximate total VAT (and SAT) volume in epidemiologic and intervention studies (for a review, see 30, 31).
The goals of this analysis were to use a large data set of contiguous abdominal MR images from healthy adults to 1) identify the specific set of abdominal MR images that have the highest correlations with total VAT volume in black and white adults, 2) compare total VAT volumes predicted with the use of different single images, and 3) quantify VAT rank-order changes that occur when single image areas are used in place of total adipose tissue volumes.
SUBJECTS AND METHODS
Subjects
The sample included 820 apparently healthy subjects (300 white men, 392 white women, 48 non-Hispanic black men, and 80 non-Hispanic black women) aged 18–88 y who are enrolled in ongoing studies of body composition and cardiovascular disease (CVD) risk at the Lifespan Health Research Center (Dayton, OH). These 820 study subjects were examined from 2003 to 2006 and have multiple contiguous MR image data. Race was self-reported by the subjects, who were prescreened to ensure that they were free of any contraindications for MRI (eg, pacemakers, metal implants, and claustrophobia). The study protocols and informed consent documents were approved by the Wright State University Institutional Review Board before subject participation.
Anthropometric measures and body composition
The subjects wore light clothing (shorts and sleeveless shirts) during the measurements. Weight was measured to the nearest 0.01 kg and stature to the nearest 0.01 cm with the use of a digital scale and a digital stadiometer. Abdominal circumference was measured at the level of the iliac crest. Dual-energy X-ray absorptiometry (DXA), with the use of a QDR 4500 Elite X-ray densitometer (Hologic Inc, Waltham, MA) was used in the fast whole body scanning mode to estimate total body fat (TBF).
Magnetic resonance imaging
Abdominal MRI was conducted at the Good Samaritan Hospital Greater Dayton MRI Consortium (Dayton, OH). Images were obtained with a Magnetom Vision 1.5 Tesla whole-body scanner (Siemens, Mississauga, Canada) using a T1-weighted fast-spin echo pulse sequence (TR 322 ms, TE 12 ms). The subjects were instructed to lie in the magnet in a supine position with arms extended above the head. A breath-hold sequence (≈22 s per acquisition) was used to minimize the effects of respiratory motion on the images. All images were acquired on a 256 × 256 mm matrix and a 480-mm field of view. Slice thickness was 10 mm, and images were obtained every 10 mm from the 9th thoracic vertebra (T9) to the first sacral vertebra (S1). Depending on the height of the person, this resulted in a total of 21–40 axial images per person. The images were retrieved from the scanner according to a DICOM (Digital Imaging and Communications in Medicine) protocol (National Electrical Manufacturer’s Association, Rosslyn, VA).
Segmentation of the axial images into VAT and subcutaneous adipose tissue (SAT) areas was performed by 2 trained observers using image analysis software (Slice-O-Matic, version 4.2; Tomovision Inc, Montreal, Canada). Tagging of adipose tissue began at the first image, containing the upper margin of the liver and continued down to the L5-S1 image, which increased the likelihood that all intraabdominal adipose tissue was included in the estimate. To calculate VAT and SAT volumes, the VAT and SAT areas for each image were summed across all images. A significant advantage of the contiguous image approach is that no geometrical assumptions have to be made regarding how to interpolate between consecutive slices for the calculation of total volumes (27).
In our hands, interobserver reliabilities for estimation of VAT and SAT volumes are as follows: CV% = 7.75% and intraclass correlation coefficient (ICC) = 0.9941 for VAT, and CV% = 0.90% and ICC = 0.9999 for SAT. The intraobserver reliabilities are CV% = 2.1% and ICC = 0.9996 for VAT and CV% = 0.55% and ICC = 0.9999 for SAT.
Statistical analysis
For all study variables, differences in means between each race-sex group were tested by using a general linear model with pairwise contrasts. Because of the possible type I error inherent in multiple comparison testing, we reexamined the least-squares (LS) means first by using the Bonferroni adjustment (where the critical P value was reduced to 0.05/6 or P = 0.008), and then by using the Tukey-Kramer test. In neither case did the interpretation of pairwise differences change; ie, all previously significant differences remained significant at P ≤ 0.01. Pearson’s product-moment correlations between single-image VAT and SAT areas and total VAT and SAT volumes were calculated and plotted to identify the single-image location with the highest correlations with total VAT and SAT volumes. The strength of each of the other correlations was then compared with the highest correlation by using the method of Steiger (32), which is a variant of the Hotelling test (33), to identify a range of images that were statistically equivalent to the “best” image in the strength of their correlations with total VAT or SAT volume. This procedure was done for each race and sex group separately to determine whether a common set of best single images could be identified for all groups.
A series of linear regression models were then applied to compare how well VAT area from a single image explained total VAT volume. Initially, each image was examined alone and then the covariates were added, including sex, race, age group (<40 compared with ≥40 y), body mass index (BMI; in kg/m2), abdominal circumference, and interaction terms (sex × VAT area, race × VAT area, and age group × VAT area). Fit statistics, including R2, root mean square error (RMSE), and CV (CV%) were generated to guide the choice of the best-fitting models. The variances of the residuals from the regression of L4-L5 images versus the best single image were compared by using Pitman’s test for correlated variances (34).
Assuming that total VAT volume measured with the multiple contiguous image protocol is the “true” VAT volume and that a single VAT area R2 value is a measure of the reliability of estimating VAT volume with a single image, we can calculate the relative loss of power when a single image area is used to approximate the total volume and the corresponding increase in sample size required to offset the increase in measurement error (reduced reliability) (35).
We also compared the best single image to the L4-L5 image in terms of the number of individuals that significantly changed VAT rank order when the single-image VAT area was compared with total abdominal VAT volume. Three levels of significant rank-order change were defined as follows: ≥5% (ie, subject changed ≥41 rank positions out of 820), ≥10% (subject changed ≥82 positions out of 820), and ≥20% (subject changed ≥164 positions out of 820). Lesser rank-order changes (<5%) were considered nonsignificant, because they fall within our own error limits for VAT and the measurement error for VAT reported by others using MRI (36–38). Statistical analyses were carried out by using SAS version 9.2 (SAS Institute, Cary, NC). Two-tailed (α = 0.05) tests of significance were used.
RESULTS
Characteristics of study subjects
Characteristics of the study subjects are summarized by race and sex in Table 1. Mean BMI was in the overweight-obese range for all groups, but black women had a significantly higher mean BMI than did any of the other groups (31 compared with 27). The expected sex differences in TBF (greater in women than in men), SAT (greater in women than in men), and VAT (greater in men than in women) were observed (all P < 0.01). Within sex, black and white men did not differ significantly in mean abdominal circumference, TBF, or SAT, but black men had a lower total VAT than did white men (2.48 compared with 3.40 L; P = 0.0003). Total VAT did not differ between black and white women, but black women had a higher abdominal circumference (102 compared with 93 cm), TBF (31 compared with 26 kg), and SAT (6.58 compared with 4.86 L) than did white women (P < 0.0001 for all).
TABLE 1.
Sample description1
| White men (n = 300) | Black men (n = 48) | White women (n = 392) | Black women (n = 80) | |
|---|---|---|---|---|
| Age (y) | 44.7 ± 16.4 | 46.2 ± 18.4 | 46.5 ± 16.0 | 48.0 ± 14.9 |
| BMI (kg/m2) | 27.6 ± 4.92 | 27.6 ± 4.82 | 27.0 ± 5.92 | 30.8 ± 6.83–5 |
| Stature (cm) | 179.0 ± 6.72,4,5 | 176.3 ± 7.92,3,5 | 164.1 ± 6.63,4 | 163.4 ± 5.73,4 |
| Abdominal circumference (cm) | 100.6 ± 13.85 | 98.2 ± 15.15 | 92.5 ± 13.92–4 | 101.6 ± 16.25 |
| Total body fat (kg) | 20.4 ± 8.02,5 | 19.4 ± 8.42,5 | 25.8 ± 9.72–4 | 31.0 ± 11.73–5 |
| Total VAT (L) | 3.40 ± 2.122.4,5 | 2.48 ± 1.662.3,5 | 1.69 ± 1.243,4 | 1.72 ± 1.033,4 |
| Total SAT (L) | 3.92 ± 2.112,5 | 3.92 ± 2.402,5 | 4.86 ± 2.802–4 | 6.58 ± 3.423–5 |
| L4-L5 VAT (cm2) | 141 ± 902.4,5 | 112 ± 773 | 94 ± 653 | 102 ± 623 |
| L4-L5 SAT (cm2) | 245 ± 1352,5 | 262 ± 1532,5 | 322 ± 1622–4 | 420 ± 1963–5 |
All values are x̄ ± SD. VAT, visceral adipose tissue; SAT, subcutaneous adipose tissue. The significance of pairwise differences was based on the Tukey-Kramer test.
Significantly different from black women, P < 0.01.
Significantly different from white men, P < 0.01.
Significantly different from black men, P < 0.01.
Significantly different from white women, P < 0.01.
The single image with the highest mean VAT area within the anatomical region examined was located 5 cm above L4-L5 in white men [maximum mean (±SD) VAT area = 178 ± 114 cm2], 4 cm above L4-L5 in black men (137 ± 94 cm2), 1 cm above L4-L5 in white women (96 ± 69 cm2), and 2 cm above L4-L5 in black women (103 ± 65 cm2).
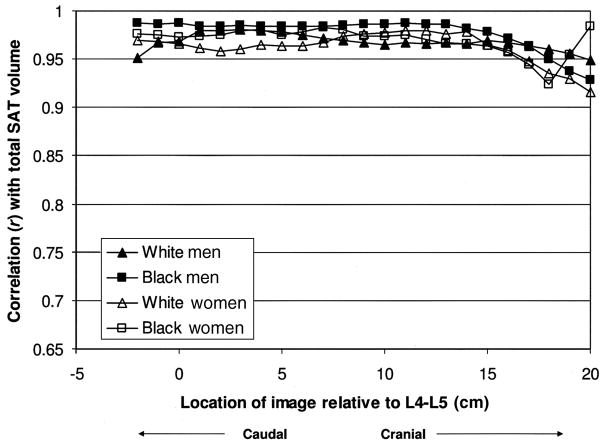
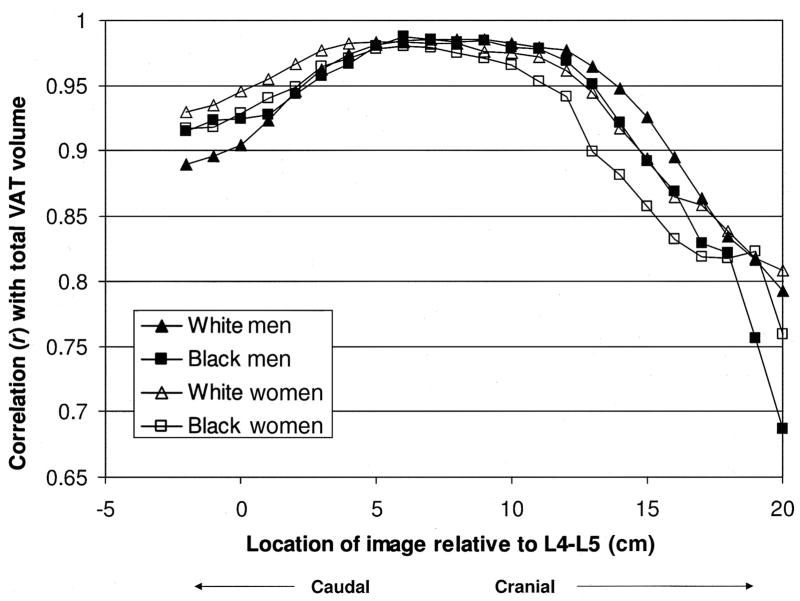
Single image areas with the highest correlations with total SAT and total VAT volumes
Correlations between individual image SAT and VAT areas and total SAT and VAT volumes were very high (generally r > 0.90) in all race and sex groups. The variation in correlations by image location for SAT and VAT are illustrated in Figures 1 and 2. For reference, the site marked “0” is the L4-L5 image, and images collected at 1 cm intervals above that point (toward the head) are labeled 1–20. Images collected at 1-cm intervals below that point (toward the feet) are labeled −1 to −3. Correlations between single-image VAT areas and total VAT volume appeared to peak for each race and sex group between 5 and 10 cm above L4-L5 (Figure 2). Little variation in the magnitude of the correlations by race or sex was observed. The magnitude of the correlations between single-image SAT areas and the total SAT volume was fairly uniform for all measurement sites (Figure 1), and, again, a marked similarity was observed between black and white men and in women in the pattern of the correlations. Because the pattern of correlation between single-image SAT and SAT volume was uniform across the region studied, we focused our remaining analyses on relations between VAT areas and VAT volume.
FIGURE 1.
Correlations between single-slice subcutaneous adipose tissue (SAT) areas and total SAT volume, by sex and race.
FIGURE 2.
Correlations between single-slice visceral adipose tissue (VAT) areas and total VAT volume, by sex and race.
The single image with the highest correlation between its VAT area and VAT volume was located 7 cm above L4-L5 for white men (r = 0.986) and 6 cm above L4-L5 for black men (r = 0.987), white women (r = 0.983), and black women (r = 0.980) (Table 2). Compared with these single best measurement sites, correlations with total VAT volume were significantly lower for VAT area measured at L4-L5 (r = 0.905–0.947), as well as for abdominal circumference (r = 0.797–0.874), in each race and sex group (P < 0.0001 for all differences between L4-L5 and L4-L5 + 6). However, a range of images with equally high correlations with total VAT volume (ie, their correlations were not significantly different from the highest correlation) was observed, and the image located 6 cm above L4-L5 (L4-L5 + 6) was within this best equivalent range in all race and sex groups. We reexamined the sagittal scout images in a random subset of 250 subjects to determine the anatomical location of their L4-L5 + 6 image. The plane of the L4-L5 + 6 image crossed the L3 vertebra in 85% of subjects and crossed the L2-L3 intervertebral space or the L2 vertebra for the remaining 15% of subjects. L4-L5 + 6 was more frequently found to cross L2-L3 or L2 in women (19%) than in men (6%), probably because of their generally shorter stature (ie, 6 cm would cover a greater distance anatomically—toward L2—in women than in generally taller men).
TABLE 2.
Location of single magnetic resonance images and image ranges with the highest correlations with visceral adipose tissue (VAT) volume, by race and sex
| White men | Black men | White men | Black women | |
|---|---|---|---|---|
| Single image location1 | +9 cm | +6 cm | +6 cm | +6 cm |
| Image range2 | +6 cm to +9 cm above L4-L5 | +5 cm to +11 cm above L4-L5 | +4 cm to +8 cm above L4-L5 | +4 cm to +9 cm above L4-L5 |
| r for best image | 0.98578 | 0.98697 | 0.98314 | 0.97990 |
| r for L4-L5 image | 0.904543 | 0.924233 | 0.945883 | 0.928753 |
| r for abdominal circumference | 0.850194 | 0.874194 | 0.860294 | 0.797364 |
Defined as image location, in cm, above (+) or below (−) L4-L5 with the highest linear correlation with total VAT volume.
Defined as the set of image areas with correlations with total VAT volume that were not significantly lower than the best image area correlations (32).
Correlation between total VAT volume and L4-L5 VAT area was significantly lower than the correlation with the best single image, P < 0.005 (Pitman’s test).
Correlation between total VAT volume and abdominal circumference was significantly lower than the correlation with the L4-L5 VAT area, P < 0.0001 (Pitman’s test).
Prediction of total VAT with a single image
Using linear regression models, we compared the prediction of total VAT volume using the VAT area from L4-L5 + 6 with that using the VAT area from L4-L5 and assessed the effect of covariates on these predictions (Table 3). The L4-L5 + 6 image alone explained 97% of the variance in total abdominal VAT volume, and the addition of covariate terms (although some were significant) did not significantly increase the R2 value. In contrast, the L4-L5 image explained 83% of the variance in VAT volume, with covariates (sex, race, age, BMI, abdominal circumference, and their 2-factor interactions) accounting for an additional 7% of the variance. Similarly, the model errors were half as large when the L4-L5 + 6 image was used (RMSE = 0.29 L for VAT, CV = 12.4%) compared with the L4-L5 image (RMSE = 0.75 L for VAT, CV = 31.9%). Adding additional terms to the L4-L5 model decreased the RMSE to 0.57 L; however, the best model using L4-L5, which included all covariates, still did not attain the variance explained or the low RMSE of a simpler model including only the VAT area at L4-L5 + 6.
TABLE 3.
Regression equations to predict total visceral adipose tissue (VAT) volume from VAT area imaged at L4-L5 and at 6 cm above L4-L5 (L4-L5 + 6)1
| Variables in model | R2 | RMSE | CV | AIC |
|---|---|---|---|---|
| L | ||||
| L4-L52 | 0.8269 | 0.754 | 31.9 | 13185 |
| L4-L52 + sex2 + race2 | 0.8678 | 0.660 | 28.0 | 12948 |
| L4-L52 + sex2 + race2 + age group3 | 0.8674 | 0.661 | 28.0 | 12938 |
| L4-L52 + sex2 + race2 + BMI2 | 0.8777 | 0.635 | 26.9 | 12876 |
| L4-L52 + sex2 + race2 + waist2 | 0.8843 | 0.609 | 26.0 | 12732 |
| L4-L52 + sex3 + race3 + age group2 + BMI3 + waist2 + (race × L4-L5)2 + (sex × L4-L5)2 | 0.8983 | 0.573 | 24.4 | 12610 |
| L4-L5 + 62 | 0.9737 | 0.294 | 12.4 | 11644 |
| L4-L5 + 62 + sex2 + race2 | 0.9741 | 0.292 | 12.4 | 11616 |
| L4-L5 + 62 + sex2 + race2 + age group2 | 0.9745 | 0.290 | 12.3 | 11595 |
| L4-L5 + 62 + sex2 + race2 + age group2 + BMI2 | 0.9750 | 0.287 | 12.3 | 11600 |
| L4-L5 + 6 + sex2 + race2 + age group2 + BMI2 + waist2 | 0.9756 | 0.280 | 12.1 | 11493 |
| L4-L5 + 6 + sex3 + race3 + age group2 + BMI3 + waist2 + (race × 6 cm)2 + (sex × 6 cm)2 | 0.9766 | 0.275 | 11.7 | 11426 |
R2, percentage of variance explained by the regression variables; RMSE, root mean squared error; AIC, Akaike information criterion.
Term is significant in the model.
Term is not significant in the model.
Sample size increases required when a single image estimate of VAT is used
Assuming that the total VAT volume is the “true” VAT volume and that the single VAT area R2 values found in the foregoing analysis are a measure of the “reliability” of estimating VAT volume with a single image, we can calculate the relative loss of power when a single image area is used (Table 4). To achieve the same statistical power of a study with the use of a multiple image protocol, using the best-correlated image for each race and sex group, between 2.7% and 4.1% additional subjects would be required. In contrast, between 11.8% and 22.2% more subjects would be required to achieve the same statistical power as a multiple image protocol when only the L4-L5 VAT image is used.
TABLE 4.
Estimated increase in sample size by using a single magnetic resonance image to measure visceral adipose tissue (VAT) volume, by race and sex
| White men | Black men | White women | Black women | |
|---|---|---|---|---|
| % | ||||
| L4-L5 image | 22.22 | 17.07 | 11.77 | 15.93 |
| Best (highest correlated) single image1 | 2.91 | 2.66 | 3.46 | 4.14 |
See Table 2 for location of single image with the highest correlation with VAT volume in each group.
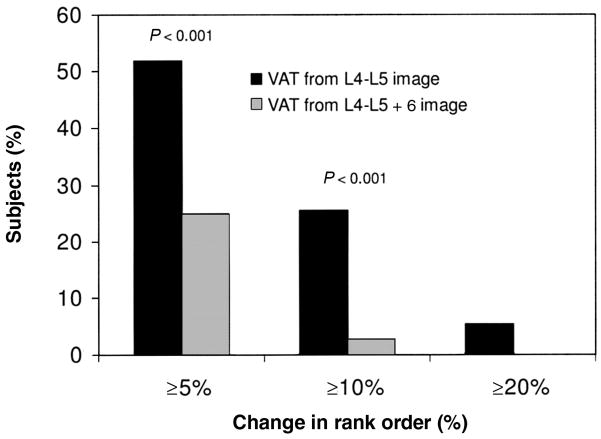
Rank-order changes in VAT in a comparison of single image areas with total volume
To assess the extent of classification error that may occur with the use of a single-image or a multiple-image protocol to approximate VAT, we counted the number of individuals that significantly changed VAT rank order when a single-image VAT area (either at L4-L5 or 6 cm above L4-L5) instead of total abdominal VAT volume was used. Using our own interobserver VAT CV% (7.75%) and error levels typically reported for MRI measures of VAT as our guide (ie, CV% = 5–10%), we tested the effect of measurement location on rank-order differences of ≥5%, ≥10%, and ≥20% (Figure 3). Whereas >50% of subjects experienced a change in rank ≥5% when the L4-L5 image was used compared with when total VAT volume was used, only 25% of subjects experienced the same change in rank when L4-L5 + 6 was used (difference in proportions: P < 0.001). Similarly, 25% of subjects experienced rank changes ≥10% when the L4-L5 image was used, compared with 3% of subjects when L4-L5 + 6 was used (P < 0.001). Marked changes in position (>20%) were not particularly common when either single image was used, and the average change in rank was relatively low. The use of the L4-L5 image produced a mean shift of 58 positions (7%) compared with total volume, and the use of the L4-L5 + 6 image produced a mean shift of 27 positions (3.3%) compared with total volume.
FIGURE 3.
Percentage of subjects who significantly changed rank order in visceral adipose tissue (VAT) when total VAT volume was compared with VAT from a single image. Two single images were used—L4-L5 and 6 cm above L4-L5 (L4-L5 + 6)—estimated for 3 levels of change in rank order: ≥5% (≥41 positions), ≥10% (≥82 positions), and ≥20% (≥164 positions).
DISCUSSION
The key finding of this study is that a range of single MR images located ≈5–10 cm above the L4-L5 image (between the L2 and L3 vertebrae) were very highly correlated with total VAT volume (r >0.95) and provided equivalent predictive power for elevated VAT volume in both men and women and in both blacks and whites. The image located 6 cm above the L4-L5 image fell within this range of best-correlated images for all race and sex groups and alone explained 97% of the variance in VAT volume (R2 = 0.9737, RMSE = 0.29 L). In comparison, VAT area from the L4-L5 image explained 83% of the variance in total VAT volume and was outside the best equivalent range (R2 = 0.8269, RMSE = 0.75 L). The correlation between abdominal circumference and total VAT volume was also outside the best equivalent range (R2 = 0.64–0.76).
Our results are in line with those of many recent studies (22, 23, 39) that showed that measurement site affects the estimation of total VAT volume and that measurement sites located 5–10 cm above (ie, in the cranial direction from L4-L5) the conventional L4-L5 image provide superior prediction of total VAT (27–30, 40). Recently, Kuk et al (40) found that VAT area at L4-L5 accounted for less variance (R2 = 0.80) and had a 2-fold greater error (SEE = 0.65 L) than did measures at both L1-L2 and L2-L3 (R2 = 0.96, SEE = 0.30 L). Similarly, Shen et al (30) found that VAT area measured at L4-L5 + 10 cm for men and at L4–L5 + 5 cm for women had the highest correlation with abdominal VAT.
Not only was the variance explained significantly higher with the use of L4-L5 + 6 than with L4-L5, the addition of race, sex, age, BMI, abdominal circumference, and interaction terms between these factors did not significantly improve the prediction made when the L4-L5 + 6 VAT area alone was used (increase in R2 = 0.0029). From the perspective of research design, the selection of a single image site with this level of accuracy would allow for VAT volume to be estimated in a diverse study sample without the need for statistical correction for sex, race, age, BMI, or other factors. We estimated that, using this image, an increase of only 2–4% in sample size would be required to obtain the precision and statistical power of a multiple slice protocol.
Given the measurement error involved in quantifying VAT with MRI, the question has been raised that measurement site differences may ultimately have a minimal effect on VAT estimation. Lee et al (36) evaluated the influence of image location on the ranking and prediction of abdominal SAT and VAT in 85 men in a preventive medicine program at the Cooper Clinic in Dallas, TX. After being adjusted for the measurement error (±10%), rank-order changes were only marginally lower when the image 5 cm above L4-L5 (L4-L5 + 5) was used rather than the L4-L5 image, and the variance explained in VAT mass was comparable for L4-L5 (R2 = 0.85, SEE 0.59 kg) and L4-L5 + 5 (R2 = 0.91, SEE = 0.44 kg). They concluded that both sites provided excellent surrogate measures of total mass (36) and that, within the anatomical region typically examined in studies of VAT, the particular measurement site may have little analytic relevance.
In contrast, 2 other studies (22, 23) have suggested that any single-image protocol will provide highly unpredictable rank ordering of subjects in terms of VAT area, given the high intra-and interindividual variation in VAT areas within the abdomen. Although it is well-established that adipose tissue traits, including VAT, are highly variable within and between individuals (21–23, 25, 31, 37–39, 41–44), these 2 particular studies (22, 23) did not statistically test their assertion that choice of measurement site affects rank order. The present analysis indicates that the average shift in rankings is low (3–7%) and that large shifts in rank (>20%) are rare regardless of measurement site. Therefore, despite the wide variation in VAT deposition patterns between individuals, a single image may provide an excellent statistical approximation of VAT volume. Our data also indicate, however, that some single images outperform others in predicting and ranking of VAT.
A recent study suggested that sites located significantly above (cranial to) L4-L5 are not only better predictors of total VAT volume than is the umbilical site (L4-L5) but are also better predictors of metabolic risk. Kuk et al (40) found that, although VAT was a strong predictor of the metabolic syndrome in white men at all measurement locations, the odds ratio (OR) for the metabolic syndrome was significantly higher for the VAT area measured at T12-L2 (OR = 8.77) than at the VAT area measured at L4-L5 (OR = 2.99). However, the risk of all-cause mortality due to elevated VAT has been reported to be similar regardless of whether total VAT volume or L4-L5 VAT area are used (2). Further research is needed to clarify whether the statistical advantages of the L4-L5 + 6 site are clinically relevant.
As for the relation between single-SAT areas and total SAT volume, we found that correlations were uniformly high and consistent across slices: r = 0.95–0.99 at all image locations examined (ie, from 3 cm below to 20 cm above L4-L5) and in all race-sex groups. There was again a range of optimum single images for approximating total SAT volume, and images from approximately L4-L5 up to L4-L5 + 11 cm all had statistically equivalent correlations with SAT volume (data not shown). Similar results have been reported by others (2, 23, 36). This suggests that measurement site will have only subtle effects on the prediction of SAT volume, and the same image used as a proxy for VAT volume will most likely be an adequate proxy for SAT volume as well.
Many previous studies have used multiple-image protocols to identify the single-image location that best represents total VAT volume (27–30, 36, 39, 40), but all have been selective in the particular images analyzed or have 5–20-mm gaps between images. An advantage of the present study was the existence of contiguous image data spanning from 20 cm above the L4-L5 area to 3 cm below the L4-L5 area (approximately from T12 to S1), which allowed us to more precisely identify the best set of images for predicting VAT volume within the abdominal region. In addition, the present study included a sufficient number of black subjects to estimate race differences in single-slice predictions, which is uncommon (30, 39). A limitation of the study was that we did not differentiate VAT into the more metabolically active intraperitoneal (mesenteric and omental) adipose tissue (18, 45) and the largely structural extraperitoneal adipose tissue compartments. However, the peritoneum is often difficult to discern with the use of MRI (31, 38, 46), and it was previously shown that VAT area from a single MR image located at L2-L3 had similar correlations with intraperitoneal, extraperitoneal, and total visceral adipose tissue volumes (27). The present study did not include persons of Hispanic or Asian origin, children, or special clinical populations; therefore, our results should be applied cautiously in groups other than healthy white and black adults.
Using a large sample of subjects with contiguous abdominal MR images, we found that a single axial image located 6 cm above L4-L5 (near the L3 vertebra) accurately predicts total VAT volume in both black and white adults. The conventionally used L4-L5 image had significantly lower predictive value for total VAT volume. To improve the likelihood of detecting group and individual differences in total VAT volume, future studies may consider choosing a single MR image located near L2-L3 instead of (or in addition to) the L4-L5 image to represent VAT volume.
Acknowledgments
We thank Robert Ross (Queen’s University) for invaluable assistance with the design of the MRI protocol, Mindy Shelley (MR technologist; Good Samaritan Greater Dayton Area MRI Center) for technical expertise and dedication, Frances Tyleshevski and Keith Wurzbacher (Wright State University) for assistance with data management, Mark Punyanita (New York Obesity Research Center, St Luke’s–Roosevelt Hospital Center) for consultation on the MR image analysis protocol, and the subjects in the Fels Longitudinal Study, the Southwest Ohio Family Study, and the Miami Valley Family Aging Study for their contributions.
Footnotes
Supported by National Institutes of Health grants R01-DK064870, R01-DK 064391, R01-HD12252, and R01-HL69995.
EWD collected and analyzed the MRI data and wrote and edited the manuscript. WS analyzed the data, provided consultation, and edited the manuscript. ML provided statistical consultation and edited the manuscript. ACC provided statistical consultation and edited the manuscript. SAC collected the data and designed the study (Southwest Ohio Family Study). RMS collected the data and designed the study (Southwest Ohio Family Study and Fels Longitudinal Study). BT collected the data and designed the study (Miami Valley Family Aging Study) and wrote and edited the manuscript. None of the authors had a personal or financial relationship to disclose.
References
- 1.Boyko EJ, Fujimoto WY, Leonetti DL, Newell-Morris L. Visceral adiposity and risk of type 2 diabetes: a prospective study among Japanese Americans. Diabetes Care. 2000;23:465–71. doi: 10.2337/diacare.23.4.465. [DOI] [PubMed] [Google Scholar]
- 2.Kuk JL, Katzmarzyk PT, Nichaman MZ, Chruch TS, Blair SN, Ross R. Visceral fat is an independent predictor of all-cause mortality in men. Obesity. 2006;14:336–41. doi: 10.1038/oby.2006.43. [DOI] [PubMed] [Google Scholar]
- 3.Cefalu W, Wang ZM, Webel S, et al. Contribution of visceral fat mass to the insulin resistance of aging. Metabolism. 1995;44:954–9. doi: 10.1016/0026-0495(95)90251-1. [DOI] [PubMed] [Google Scholar]
- 4.Miyazaki Y, Glass L, Triplitt C, Wajcberg E, Mandarino L, DeFronzo RA. Abdominal fat distribution and peripheral and hepatic insulin resistance in type 2 diabetes mellitus. Am J Physiol Endocrinol Metab. 2002;283:E1135–43. doi: 10.1152/ajpendo.0327.2001. [DOI] [PubMed] [Google Scholar]
- 5.Montague CT, O’Rahilly S. The perils of portliness: causes and consequences of visceral adiposity. Diabetes. 2000;49:883–8. doi: 10.2337/diabetes.49.6.883. [DOI] [PubMed] [Google Scholar]
- 6.Motoshima H, Wu X, Sinha MK, et al. Differential regulation of adiponectin secretion from cultured human omental and subcutaneous adipocytes: effects of insulin and rosiglitazone. J Clin Endocrinol Metab. 2002;87:5662–7. doi: 10.1210/jc.2002-020635. [DOI] [PubMed] [Google Scholar]
- 7.Nguyen-Duy TB, Nichaman MZ, Church TS, Blair SN, Ross R. Visceral fat and liver fat are independent predictors of metabolic risk factors in men. Am J Physiol Endocrinol Metab. 2003;284:E1065–71. doi: 10.1152/ajpendo.00442.2002. [DOI] [PubMed] [Google Scholar]
- 8.Wajchenberg BL. Subcutaneous and visceral adipose tissue: their relation to the metabolic syndrome. Endocr Rev. 2000;21:697–738. doi: 10.1210/edrv.21.6.0415. [DOI] [PubMed] [Google Scholar]
- 9.Wajchenberg BL, Giannella-Neto D, da Silva ME, Santos RF. Depot-specific hormonal characteristics of subcutaneous and visceral adipose tissue and their relation to the metabolic syndrome. Horm Metab Res. 2002;34:616–21. doi: 10.1055/s-2002-38256. [DOI] [PubMed] [Google Scholar]
- 10.Giannopoulou I, Ploutz-Snyder LL, Carhart R, et al. Exercise is required for visceral fat loss in postmenopausal women with type 2 diabetes. J Clin Endocrinol Metab. 2005;90:1511–8. doi: 10.1210/jc.2004-1782. [DOI] [PubMed] [Google Scholar]
- 11.Janssen I, Fortier A, Hudson E, Ross R. Effects of an energy-restrictive diet with or without exercise on abdominal fat, intermuscular fat, and metabolic risk factors in obese women. Diabetes Care. 2002;25:431–8. doi: 10.2337/diacare.25.3.431. [DOI] [PubMed] [Google Scholar]
- 12.O’Leary VB, Marchetti CM, Krishnan RK, Stetzer BP, Gonzalez F, Kirwan JP. Exercise-induced reversal of insulin resistance in obese elderly is associated with reduced visceral fat. J Appl Physiol. 2006;100:1584–9. doi: 10.1152/japplphysiol.01336.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ross R, Freeman J, Janssen I. Exercise alone is an effective strategy for reducing obesity and related comorbidities. Exerc Sport Sci Rev. 2000;28:65–70. [PubMed] [Google Scholar]
- 14.Ross R, Rissanen J, Pedwell H, Clifford J, Shragge P. Influence of diet and exercise on skeletal muscle and visceral adipose tissue in men. J Appl Physiol. 1996;81:2445–55. doi: 10.1152/jappl.1996.81.6.2445. [DOI] [PubMed] [Google Scholar]
- 15.Thomas EL, Brynes AE, McCarthy J, et al. Preferential loss of visceral fat following aerobic exercise, measured by magnetic resonance imaging. Lipids. 2000;35:769–76. doi: 10.1007/s11745-000-0584-0. [DOI] [PubMed] [Google Scholar]
- 16.Despres JP, Golay A, Sjostrom L. Effects of rimonabant on metabolic risk factors in overweight patients with dyslipidemia. N Engl J Med. 2005;353:2121–34. doi: 10.1056/NEJMoa044537. [DOI] [PubMed] [Google Scholar]
- 17.Schwartz TL, Nihalani N, Virk S, Jindal S, Chilton M. Psychiatric medication-induced obesity: treatment options. Obes Rev. 2004;5:233–8. doi: 10.1111/j.1467-789X.2004.00149.x. [DOI] [PubMed] [Google Scholar]
- 18.Abate N, Burns D, Peshock RM, Garg A, Grundy SM. Estimation of adipose tissue mass by magnetic resonance imaging: validation against dissection in human cadavers. J Lipid Res. 1994;35:1490–6. [PubMed] [Google Scholar]
- 19.Fowler PA, Fuller MF, Glasbey CA, et al. Total and subcutaneous adipose tissue in women: the measurement of distribution and accurate prediction of quantity by using magnetic resonance imaging. Am J Clin Nutr. 1991;54:18–25. doi: 10.1093/ajcn/54.1.18. [DOI] [PubMed] [Google Scholar]
- 20.Mitsiopoulos N, Baumgartner RN, Heymsfield SB, Lyons W, Gallagher D, Ross R. Cadaver validation of skeletal muscle measurement by magnetic resonance imaging and computerized tomography. J Appl Physiol. 1998;85:115–22. doi: 10.1152/jappl.1998.85.1.115. [DOI] [PubMed] [Google Scholar]
- 21.Ross R, Leger L, Morris D, de Guise J, Guardo R. Quantification of adipose tissue by MRI: relationship with anthropometric variables. J Appl Physiol. 1992;72:787–95. doi: 10.1152/jappl.1992.72.2.787. [DOI] [PubMed] [Google Scholar]
- 22.Greenfield JR, Samaras K, Chisholm DJ, Campbell LV. Regional intra-subject variability in abdominal adiposity limits usefulness of computed tomography. Obes Res. 2002;10:260–5. doi: 10.1038/oby.2002.35. [DOI] [PubMed] [Google Scholar]
- 23.Thomas EL, Bell JD. Influence of undersampling on magnetic resonance imaging measurements of intra-abdominal adipose tissue. Int J Obes Relat Metab Disord. 2003;27:211–8. doi: 10.1038/sj.ijo.802229. [DOI] [PubMed] [Google Scholar]
- 24.Shen W, Wang ZM, Punyanita M, et al. Adipose tissue quantification by imaging methods: a proposed classification. Obes Res. 2003;11:5–16. doi: 10.1038/oby.2003.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kvist H, Chowdhury B, Grangard U, Tylen U, Sjostrom L. Total and visceral adipose-tissue volumes derived from measurements with computed tomography in adult men and women: predictive equations. Am J Clin Nutr. 1988;48:1351–61. doi: 10.1093/ajcn/48.6.1351. [DOI] [PubMed] [Google Scholar]
- 26.Kvist H, Sjostrom L, Tylen U. Adipose tissue volume determinations in women by computed tomography: technical considerations. Int J Obes. 1986;10:53–67. [PubMed] [Google Scholar]
- 27.Abate N, Garg A, Coleman R, Grundy SM, Peshock RM. Prediction of total subcutaneous abdominal, intraperitoneal, and retroperitoneal adipose tissue masses in men by a single axial magnetic resonance imaging slice. Am J Clin Nutr. 1997;65:403–8. doi: 10.1093/ajcn/65.2.403. [DOI] [PubMed] [Google Scholar]
- 28.Han TS, Kelly IE, Walsh K, Greene RM, Lean ME. Relationship between volumes and areas from single transverse scans of intra-abdominal fat measured by magnetic resonance imaging. Int J Obes Relat Metab Disord. 1997;21:1161–6. doi: 10.1038/sj.ijo.0800530. [DOI] [PubMed] [Google Scholar]
- 29.Han TS, McNeill G, Seidell JC, Lean ME. Predicting intra-abdominal fatness from anthropometric measures: the influence of stature. Int J Obes Relat Metab Disord. 1997;21:587–93. doi: 10.1038/sj.ijo.0800446. [DOI] [PubMed] [Google Scholar]
- 30.Shen W, Punyanitya M, Wang ZM, et al. Visceral adipose tissue: relations between single-slice areas and total volume. Am J Clin Nutr. 2004;80:271–8. doi: 10.1093/ajcn/80.2.271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ross R, Janssen I. Computed tomography and magnetic resonance imaging. In: Heymsfield SB, Lohman TG, Wang ZM, Going SB, editors. Human body composition. 2. Champaign, IL: Human Kinetics; 2004. [Google Scholar]
- 32.Steiger JH. Tests for comparing elements of a correlation matrix. Psychol Bull. 1980;87:245–61. [Google Scholar]
- 33.Hotelling H. The selection of variants for use in prediction with some comments on the general problem of nuisance parameters. Ann Math Stat. 1940;11:271–83. [Google Scholar]
- 34.Snedecor GW, Cochran WG. Statistical methods. 8. Ames, IA: Iowa State University Press; 1989. [Google Scholar]
- 35.Muller MJ, Szegedi A. Effects of interrater reliability of psychopathologic assessment on power and sample size calculations in clinical trials. J Clin Psychopharmacol. 2002;22:318–25. doi: 10.1097/00004714-200206000-00013. [DOI] [PubMed] [Google Scholar]
- 36.Lee S, Janssen I, Ross R. Interindividual variation in abdominal subcutaneous and visceral adipose tissue: influence of measurement site. J Appl Physiol. 2004;97:948–54. doi: 10.1152/japplphysiol.01200.2003. [DOI] [PubMed] [Google Scholar]
- 37.Ross R, Shaw KD, Martel Y, de Guise J, Avruch L. Adipose tissue distribution measured by magnetic resonance imaging in obese women. Am J Clin Nutr. 1993;57:470–5. doi: 10.1093/ajcn/57.4.470. [DOI] [PubMed] [Google Scholar]
- 38.Ross R, Shaw KD, Rissanen J, Martel Y, de Guise J, Avruch L. Sex differences in lean and adipose tissue distribution by magnetic resonance imaging: anthropometric relationships. Am J Clin Nutr. 1994;59:1277–85. doi: 10.1093/ajcn/59.6.1277. [DOI] [PubMed] [Google Scholar]
- 39.Warren M, Schreiner PJ, Terry JG. The relation between visceral fat measurement and torso level—is one level better than another? The Atherosclerosis Risk in Communities Study, 1990–1992. Am J Epidemiol. 2006;163:352–8. doi: 10.1093/aje/kwj049. [DOI] [PubMed] [Google Scholar]
- 40.Kuk JL, Church TS, Blair SN, Ross R. Does measurement site for visceral and abdominal subcutaneous adipose tissue alter associations with the metabolic syndrome? Diabetes Care. 2006;29:679–84. doi: 10.2337/diacare.29.03.06.dc05-1500. [DOI] [PubMed] [Google Scholar]
- 41.Baumgartner RN, Heymsfield SB, Roche AF, Bernardino M. Abdominal composition quantified by computed tomography. Am J Clin Nutr. 1988;48:936–45. doi: 10.1093/ajcn/48.4.936. [DOI] [PubMed] [Google Scholar]
- 42.Borkan GA, Gerzof SG, Robins AH, Hults DE, Silbert CK, Silbert JE. Assessment of abdominal fat content by computed tomography. Am J Clin Nutr. 1982;36:172–7. doi: 10.1093/ajcn/36.1.172. [DOI] [PubMed] [Google Scholar]
- 43.Grauer WO, Moss AA, Cann CE, Goldberg HI. Quantification of body fat distribution in the abdomen using computed tomography. Am J Clin Nutr. 1984;39:631–7. doi: 10.1093/ajcn/39.4.631. [DOI] [PubMed] [Google Scholar]
- 44.Ross R, Leger L, Guardo R, De Guise J, Pike BG. Adipose tissue volume measured by magnetic resonance imaging and computerized tomography in rats. J Appl Physiol. 1991;70:2164–72. doi: 10.1152/jappl.1991.70.5.2164. [DOI] [PubMed] [Google Scholar]
- 45.Bjorntorp P. Classification of obese patients and complications related to the distribution of surplus fat. Nutrition. 1990;6:131–7. [PubMed] [Google Scholar]
- 46.van der Kooy K, Leenan R, Seidell JC, Deurenberg P, Visser M. Abdominal diameters as indicators of visceral fat: comparison between magnetic resonance imaging and anthropometry. Br J Nutr. 1993;70:47–58. doi: 10.1079/bjn19930104. [DOI] [PubMed] [Google Scholar]