Abstract
Hydroxyurea is a cytostatic agent that has recently become the drug of choice in the treatment of various myeloproliferative diseases. The cutaneous side effects of hydroxyurea include xerosis, hyperpigmentation, nail discoloration, and scaling. Leg ulcers have only rarely been reported in association with hydroxyurea treatment. A 75-year-old woman presented with leg ulcers, nail discoloration, and xerosis. The leg ulcers were refractory to conventional treatment. She had been taking oral hydroxyurea since being diagnosed with essential thrombocytosis in 2002. Hence, we suspected hydroxyurea-induced leg ulcers and discontinued her hydroxyurea treatment; the ulcers gradually healed thereafter. We present a rare case of hydroxyurea-induced leg ulcers in Korea.
Keywords: Cutaneous side effects, Hydroxyurea, Leg ulcer
INTRODUCTION
Hydroxyurea is a cytostatic agent that is currently the treatment of choice for various myeloproliferative diseases, such as chronic myelogenous leukemia, polycythemia vera, and essential thrombocytosis1. It acts during cellular replication and inhibits DNA synthesis by blocking ribonucleotide reductase2.
The most common adverse effects of hydroxyurea include mild fatigue, headache, nausea, vomiting, diarrhea, and fever. Severe side effects are rare and appear to be linked to long-term administration3. Adverse cutaneous effects include xerosis, diffuse hyperpigmentation, nail discoloration, alopecia, scaling, skin atrophy, skin tumors, lichen planus-like eruptions, and dermatomyositis-like eruptions1,3. In addition, a rare cutaneous manifestation, leg ulceration, has been reported in a few studies1. We report a case of a 75-year-old woman with essential thrombocytosis who developed painful leg ulcers, xerosis, and nail discoloration after hydroxyurea therapy.
CASE REPORT
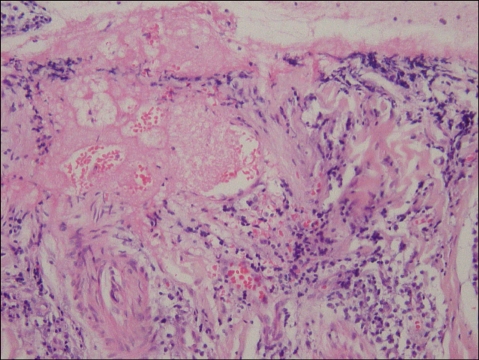
A 75-year-old woman presented with leg ulcers and xerosis. She had been diagnosed with essential thrombocytosis and had been receiving hydroxyurea therapy, 2 g/day, for 4 years. Scaly, hyperkeratotic patches and fissures were present on both of her heels. After she had rubbed her right heel, an erythematous ulcerative patch had developed (Fig. 1). The skin lesion on the right heel had progressed to become a deeper, severely painful, hemorrhagic ulcer; a similar lesion soon developed on her left heel (Fig. 1). Complete blood cell count revealed a hemoglobin of 9.2 g/dl, and a platelet count of 788×103/µl. No bacteria was found on Gram stains from the right heel wound. Bacterial and fungal cultures revealed no growth. Histologic examination of the specimen taken from the right heel showed mixed inflammatory cell infiltration around the dermal vessels, along with disruption of the epidermis (Fig. 2).
Fig. 1.
Erythematous ulcerative skin lesions developed on both heels.
Fig. 2.
Histologic examination of the specimen taken from the right heel wound showed a mixed inflammatory cell infiltration around the dermal vessels, along with disruption of the epidermis (H&E stain, ×40).
Although no definitive diagnosis was made, the patient started conservative treatment with antibiotics, analgesics, and occlusive dressings. However, the lesions did not improve during 5 weeks of treatment, and a new, painful ulcerative skin lesion developed on the left malleolus (Fig. 3). Longitudinal linear streaks and hyperpigmentation were noted in both the toenails and fingernails. The ulcers on both heels and the right malleolus became enlarged and more painful.
Fig. 3.
After 5 weeks of conservative treatment, a new, painful, ulcerative skin lesion developed on the patient's right malleolus.
We began to suspect the side effects of long-term hydroxyurea administration, and we therefore discontinued the drug. The ulcerative skin lesions improved within 3 weeks (Fig. 4). We subsequently diagnosed the patient with hydroxyurea-induced leg ulcers. The cutaneous ulcers and xerosis completely disappeared within 2 months without recurrence, and the nail hyperpigmentation improved gradually.
Fig. 4.

The ulcerative skin lesions began to improve within 3 weeks after discontinuation of hydroxyurea.
DISCUSSION
Hydroxyurea is a cytostatic agent that serves as the drug of choice in the treatment of myeloproliferative disease. Because it acts during cellular replication (S phase) by blocking ribonucleotide reductase, the conversion of ribonucleotide to deoxynucleotide is inhibited1,2. Adverse cutaneous effects associated with hydroxyurea have been occasionally described in the literature. Xerosis, diffuse hyperpigmentation, nail discoloration, alopecia, scaling, skin atrophy, skin tumors, lichen planus-like eruptions, and dermatomyositis-like eruptions represent the majority of adverse effects1,3. In addition, leg ulcers have been noted in association with long-term hydroxyurea administration. Nine percent of patients taking hydroxyurea medication develop this complication4.
There is still controversy concerning the origin of the cutaneous ulcers-whether they are disease-related or treatment-related. Myeloproliferative disorders can impair cutaneous microcirculation. One theory says that the hyperviscosity resulting from blood dyscrasias may itself be a further risk factor for leg ulceration5,6. However, ulcerative skin lesions appear after the myeloproliferative disorder is well controlled with hydroxyurea. Furthermore, the lesions disappear after hydroxyurea is discontinued. Paradoxically, the ulcers have been shown to improve when the blood dyscrasia recurs1. So, in our opinion, hyperviscosity can be ruled out as a major contributor to ulcer formation.
Hydroxyurea treatment induces ulcerative skin lesion formation secondary to direct cytologic damage. Because hydroxyurea kills proliferating cells during the synthesis phase of the cell cycle, keratinocyte and collagen fiber synthesis could be impaired7. This hydroxyurea-induced compromise of skin formation could cause ulceration if followed by minor trauma, like rubbing in the present case8. A recent study showed that hydroxyurea can lead to increases in red blood cell volume and a reduction in red blood cell susceptibility to deformation. Therefore, it may cause impaired microcirculation and cutaneous anoxia, which then lead to ulcerative skin lesions and severe pain9,10. Bader et al11 proposed some criteria to help in diagnosis and differentiation. First, the duration of treatment should be at least 1 year, and the dose of hydroxyurea should be at least 1 g/day. Most ulcers are found on the malleoli (77%) or in neighboring regions (e.g. the Achilles tendon). Healing is slow (1~9 months) but spontaneous in 85% of patients after discontinuation of hydroxyurea therapy, and when hydroxyurea therapy is resumed, the ulcers do not resolve spontaneously and are difficult to treat. Ulcers are small, and size seems to be correlated with the hydroxyurea dose.
The treatment of choice for hydroxyurea-induced leg ulcers is discontinuation of the drug. Other reported therapies including topical granulocyte macrophage colonystimulating factor (GM-CSF), recombinant human erythropoietin (r-HuEPO), or bilayered bioengineered skin substitute12. In one report, a patient was successfully treated with prostaglandin E1 and pentoxifylline while hydroxyurea was continued13. In the present case, the cutaneous ulcers and xerosis completely healed within 2 months without recurrence, and nail hyperpigmentation gradually improved after hydroxyurea was discontinued.
The present case shows that long-term administration of hydroxyurea can result in ulcerative skin lesions of the lower legs, like other cases that have been reported in Korea14,15. Because hydroxyurea has long been the treatment of choice for myeloproliferative disorders, the possibility that cutaneous side effects will occur in patients treated with hydroxyurea always exists. Leg ulcers represent 9% of these side effects. Therefore, physicians should not overlook this adverse effect and must perform careful history-taking. In addition, because discontinuation of hydroxyurea can cause a hematologic crisis, a hematooncologist should be consulted, and periodic laboratory examinations should be performed.
References
- 1.Sirieix ME, Debure C, Baudot N, Dubertret L, Roux ME, Morel P, et al. Leg ulcers and hydroxyurea: forty-one cases. Arch Dermatol. 1999;135:818–820. doi: 10.1001/archderm.135.7.818. [DOI] [PubMed] [Google Scholar]
- 2.Park JH, Kim CD, Ryoo YW, Kim BC, Lee KS. Chronic hydroxyurea-induced dermatomyositis-like eruption showing epidermal dysmaturation. Ann Dermatol. 2002;14:28–30. [Google Scholar]
- 3.Weinlich G, Schuler G, Greil R, Kofler H, Fritsch P. Leg ulcers associated with long-term hydroxyurea therapy. J Am Acad Dermatol. 1998;39:372–374. doi: 10.1016/s0190-9622(98)70394-9. [DOI] [PubMed] [Google Scholar]
- 4.Najean Y, Rain JD. Treatment of polycythemia vera: the use of hydroxyurea and pipobroman in 292 patients under the age of 65 years. Blood. 1997;90:3370–3377. [PubMed] [Google Scholar]
- 5.Yarbro JW. Mechanism of action of hydroxyurea. Semin Oncol. 1992;19:1–10. [PubMed] [Google Scholar]
- 6.Demircay Z, Comert A, Adiguzel C. Leg ulcers and hydroxyurea: report of three cases with essential thrombocythemia. Int J Dermatol. 2002;41:872–874. doi: 10.1046/j.1365-4362.2002.01623.x. [DOI] [PubMed] [Google Scholar]
- 7.Best PJ, Daoud MS, Pittelkow MR, Petitt RM. Hydroxyurea-induced leg ulceration in 14 patients. Ann Intern Med. 1998;128:29–32. doi: 10.7326/0003-4819-128-1-199801010-00005. [DOI] [PubMed] [Google Scholar]
- 8.Nguyen TV, Margolis DJ. Hydroxyurea and lower leg ulcers. Cutis. 1993;52:217–219. [PubMed] [Google Scholar]
- 9.Engstrom KG, Lofvenberg E. Treatment of myeloproliferative disorders with hydroxyurea: effects on red blood cell geometry and deformability. Blood. 1998;91:3986–3991. [PubMed] [Google Scholar]
- 10.Rodgers GP, Dover GJ, Uyesaka N, Noguchi CT, Schechter AN, Nienhuis AW. Augmentation by erythropoietin of the fetal-hemoglobin response to hydroxyurea in sickle cell disease. N Engl J Med. 1993;328:73–80. doi: 10.1056/NEJM199301143280201. [DOI] [PubMed] [Google Scholar]
- 11.Bader U, Banyai M, Boni R, Burg G, Hafner J. Leg ulcers in patients with myeloproliferative disorders: disease- or treatment-related? Dermatology. 2000;200:45–48. doi: 10.1159/000018315. [DOI] [PubMed] [Google Scholar]
- 12.Dissemond J, Hoeft D, Knab J, Franckson T, Kroger K, Goos M. Leg ulcer in a patient associated with hydroxyurea therapy. Int J Dermatol. 2006;45:158–160. doi: 10.1111/j.1365-4632.2004.02450.x. [DOI] [PubMed] [Google Scholar]
- 13.Stagno F, Guglielmo P, Consoli U, Fiumara P, Russo M, Giustolisi R. Successful healing of hydroxyurea-related leg ulcers with topical granulocyte-macrophage colony-stimulating factor. Blood. 1999;94:1479–1480. [PubMed] [Google Scholar]
- 14.Yun SJ, Lee JB, Kim SJ, Lee SC, Won YH. A case of hydroxyurea-induced cutaneous ulceration and squamous cell carcinoma. Korean J Dermatol. 2002;40:433–436. [Google Scholar]
- 15.Jang SJ, Moon YJ, Choi YH, Kim JH, Won JY. A case of cutaneous manifestations associated with hydroxyurea therapy. Korean J Dermatol. 2003;41:965–967. [Google Scholar]