Abstract
Tattooing is becoming more popular around the world. As a result, the reported complications of tattoo are increasing. Local inflammation, infection and allergic reactions are the most common adverse effects. We report here on a healthy 39-year-old woman who developed multiple verruca plana lesions after undergoing semipermanent tattooing. The tattooing had been done 1 year earlier by an amateur.
Keywords: Tattoo, Verruca plana
INTRODUCTION
Tattooing is an art that's been practiced for more than 8,000 years and it is still a common practice in many countries and cultures. Tattooing for cosmetic adornment is becoming increasingly popular. This may be due to broader acceptance, the aesthetic appeal or the availability of laser therapy for removing unwanted tattoos. Yet there are many complications associated with the introduction of pigment into skin. Local inflammation, infection and allergic reactions are the most common adverse affects. The infectious side effects include local bacterial infections and transmission of hepatitis, syphilis and human immunodeficiency virus (HIV). We report here on a case of facial verruca plana that developed after semipermanent tattooing. Our case is the first reported case of facial verruca plana that developed after tattooing in the Korean literature.
CASE REPORT
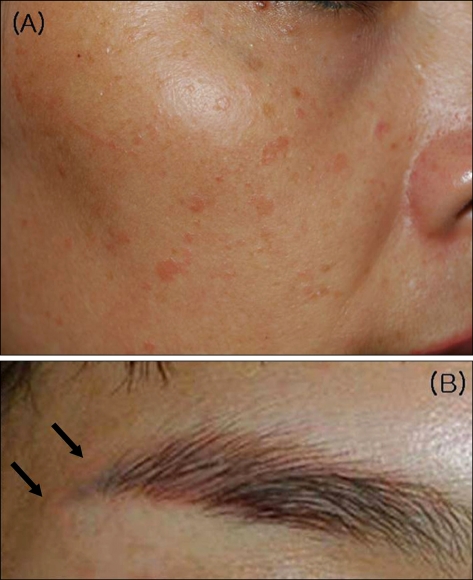
The patient was a healthy 39-year-old woman with multiple flat erythematous pinhead-sized papules on her face (Fig. 1).
Fig. 1.
Verruca plana lesions on the face (A). Close-up view of the lesions on the right eyebrow (B, arrows).
The semipermanent tattoo on her eyebrow, eyeline and lip was performed by an amateur 2 years ago. A solitary flat pinhead-sized papule was first found 1 year ago on her right eyebrow's semipermanent tattoo site. The skin lesion spread to her entire face for 1 year. The patient denied any discomfort within the tattoo or a history of warts, verruca plana, other skin diseases, any trauma or intravenous drug abuse. There was no history of any skin disease at the semipermanent tattoo site.
There were no abnormalities besides the skin lesion seen on the general physical examination. She denied any significant past medical history, and her family history was not remarkable. The routine laboratory studies performed in another hospital, including CBC, LFT, renal function tests and urinalysis, were all within the normal limits. The laboratory tests for human immunodeficiency virus (HIV), syphilis and hepatitis were negative.
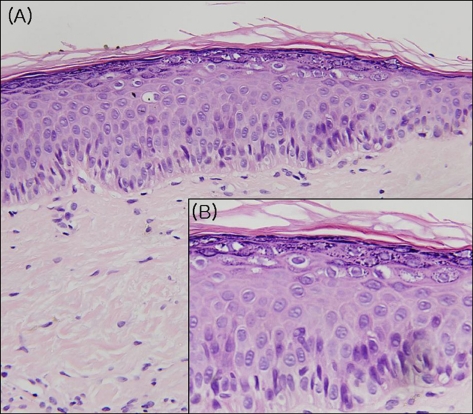
With the clinical suspicion of verruca plana, a punch biopsy was performed. Histologic examination showed acanthosis and koilocytosis that are typical of verruca plana (Fig. 2). Proliferation of dilated capillaries was present within the papillary dermis.
Fig. 2.
There is a prominent viral cytopathic effect affecting the keratinocytes, including vacuolization, enlargement and nuclear basophilia with a prominent granular layer and a pronounced basket-weave appearance of the horny layer (A: H&E, ×200, B: H&E, ×400).
The patient was treated with topical 5% imiquimod cream, but the warts remained unchanged and the patient was lost to follow-up.
DISCUSSION
Tattoos are increasingly popular in today's society. As a result, the reactions observed within tattoos are likely to become more abundant. It is well known that tattoos may cause various systemic and/or cutaneous pathologies. The systemic reactions range from infectious diseases such as hepatitis B or C, AIDS, syphilis, tuberculosis or leprosy to diseases with an immunologic or toxic pathogenic mechanism such as erythema multiforme, toxic shock, urticaria, vasculitis or sarcoidosis1. The skin reactions are mainly infectious: warts, herpes simplex, molluscum contagiosum, cellulitis, erysipelas and erysipeloid. In other less frequent cases, the lesions that are considered coincidental lesions are basal2 or squamous3 cell carcinomas, or even melanomas4. Apart from these complications, tattooing can also flare a Koebner's response in patients with active susceptible disease. It has been demonstrated that tattooed skin is more sensitive to trauma of all types compared with the surrounding normal skin, possibly because they are sites of compromised resistance.
In our case, the lesional skin presented the clinical and histologic hallmarks of verruca plana. The source of the virus implant is unknown, but several possibilities can be suggested. (1) The tattoo instrument (a staple) may have been used on other tattoo recipients and the virus may have been spread in this manner, (2) the ink or melted plastic used in the tattoo may have been contaminated with the virus, (3) the patient may have a verruca in the area of the tattoo when it was placed and it was spread traumatically through placement of the tattoo and (4) the saliva of the tattoo artist may have contained viral particles that were implanted at the time of placement. Attempts to examine the tattoo artist and his instruments were unsuccessful because he and the tattoo shop were out of business by the time the skin lesions developed.
After experimental papilloma virus inoculation, a verruca usually appears within 2 to 9 months5. There have been six reports in the medical literature on inoculation of HPV during tattooing6-11. The time between tattooing and the appearance of verruca varied from 2 months to 8 years, and the mean period was 4.5 years. The latency period of our case was 1 year. In our case, the first verruca lesion developed in the eyebrow semipermanent tattoo placement area. After a few months the lesions spread to the entire face. We think the lesion at the tattoo site was the primary disease focus, and it spread to other sites.
This case report provides support for the belief that HPV can be traumatically inoculated and it can have a long latency period.
References
- 1.Sowden JM, Byrne JP, Smith AG, Hiley C, Suarez V, Wagner B, et al. Red tattoo reactions: X-ray microanalysis and patch-test studies. Br J Dermatol. 1991;124:576–580. doi: 10.1111/j.1365-2133.1991.tb04954.x. [DOI] [PubMed] [Google Scholar]
- 2.Wiener DA, Scher RK. Basal cell carcinoma arising in a tattoo. Cutis. 1987;39:125–126. [PubMed] [Google Scholar]
- 3.McQuarrie DG. Squamous-cell carcinoma arising in a tattoo. Minn Med. 1966;49:799–801. [PubMed] [Google Scholar]
- 4.Khan IU, Moiemen NS, Firth J, Frame JD. Malignant melanoma disguised by a tattoo. Br J Plast Surg. 1999;52:598. doi: 10.1054/bjps.1999.3212. [DOI] [PubMed] [Google Scholar]
- 5.Androphy EJ, Lowy DR. Warts. In: Wolff K, Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, editors. Fitzpatrick's dermatology in general medicine. 7th ed. New York: McGraw-Hill; 2008. p. 1915. [Google Scholar]
- 6.Baxter SY, Deck DH. Tattoo-acquired verruca plana. Am Fam Physician. 1993;47:732. [PubMed] [Google Scholar]
- 7.Miller DM, Brodell RT. Verruca restricted to the areas of black dye within a tattoo. Arch Dermatol. 1994;130:1453–1454. [PubMed] [Google Scholar]
- 8.Ragland HP, Hubbell C, Stewart KR, Nesbitt LT., Jr Verruca vulgaris inoculated during tattoo placement. Int J Dermatol. 1994;33:796–797. doi: 10.1111/j.1365-4362.1994.tb00998.x. [DOI] [PubMed] [Google Scholar]
- 9.Trefzer U, Schmollack KP, Stockfleth E, Sterry W, Kolde G. Verrucae in a multicolored decorative tattoo. J Am Acad Dermatol. 2004;50:478–479. doi: 10.1016/s0190-9622(03)02096-6. [DOI] [PubMed] [Google Scholar]
- 10.Brajac I, Loncarek K, Stojnic-Sosa L, Gruber F. Delayed onset of warts over tattoo mark provoked by sunburn. J Eur Acad Dermatol Venereol. 2005;19:247–248. doi: 10.1111/j.1468-3083.2004.01121.x. [DOI] [PubMed] [Google Scholar]
- 11.Saez M, Rodriguez-Martin M, Sidro-Sarto M, Cabrera de Paz R, Rodriguez-Garcia F, Fagundo-Gonzalez E, et al. Multiple verrucae vulgaris in a young woman's tattoo. J Eur Acad Dermatol Venereol. 2006;20:356–357. doi: 10.1111/j.1468-3083.2006.01438.x. [DOI] [PubMed] [Google Scholar]