Abstract
Background
Several studies have been performed to evaluate the efficacy of dietary n-3 fatty acid for patients with renal dysfunction. While about 40% to 80% of patients with end-stage renal disease (ESRD) complain about pruritus and xerosis, there are few reports on the effects of topical n-3 fatty acid on these symptoms.
Objective
In order to investigate the possible beneficial effects of topical n-3 fatty acid, oils extracted from chia (Salvia hispanica) seed were formulated into topical products, the effects of which were measured.
Methods
Five healthy volunteers having xerotic pruritus symptoms and 5 patients with pruritus caused by either ESRD or diabetes were involved in this study. A topical formulation containing 4% chia seed oils were applied for an 8-week duration. Subjective itching symptoms were assessed on a 6-point scale, as were other skin functions, namely transepidermal water loss and skin capacitance.
Results
After the 8 weeks of application, significant improvements in skin hydration, lichen simplex chronicus, and prurigo nodularis were observed in all patients. A similar improvement was also observed among healthy volunteers with xerotic pruritus. Improvement of epidermal permeability barrier function and skin hydration, represented by trans-epidermal water loss and skin capacitance, respectively, were also observed. No adverse effects were observed in all the tested patients and volunteers.
Conclusion
Chia seed oil can be used as an adjuvant moisturizing agent for pruritic skin, including that of ESRD patients.
Keywords: Alpha-linolenic acid, Chia seed oil, End-stage renal failure, Omega-3 fatty acids, Pruritus
INTRODUCTION
Xerotic skins and pruritus are frequently associated with diabetes or patients with end-stage renal disease (ESRD). While the exact mechanisms underlying the pruritic phenomena have not yet fully understood, about 30% of diabetic patients show skin disorders, and more severe pruritic symptoms are generally observed when there is a renal complication1. It was also reported that pruritus affect about 40~85% of patients under hemodialysis maintenance, and that the severity of the pruritus is closely correlated with the dryness of the skin2.
Even with the high incidence of pruritus in diabetic and ESRD patients, objective assessment is relatively difficult. Subjective evaluation, instead, is generally used for measuring the efficacy of treatment. Topical products such as moisturizers or emollients are typically used for alleviating the symptoms of pruritus, but the complete resolution by topical products is rarely accomplished. Since one of the most unbearable symptoms of diabetes and ESRD is pruritus, effective therapeutic modalities need to be developed.
N-3 fatty acid exhibits anti-inflammatory properties for many inflammatory diseases3,4. Oral supplementation of fish oils, rich in n-3 fatty acids, is known to be beneficial for relieving the pruritus5. Oils extracted from the seed of chia (Saliva hispanica L) have been used for long time as a dietary supplement by American Indians and Mexican natives. Recently, it has been reported that chia seed oil is the richest botanical source of 18:3 n-3 fatty acid currently known6. In addition, chia seed oil also contains natural α-linolenic acid and flavonol, which can act as lipid antioxidants. Since the flavonol has anti-oxidant, anti-inflammatory, anti-thrombotic and anti-cancer effects, chia seed oil has been used a lot in the food industry. Recently, topical application of chia seed oil has also received more attention. Unfortunately, to this date there is a lack of published data describing the therapeutic effect of chia seed oil, especially as a topical anti-pruritic agent.
In this study, we assessed the effect of topical chia seed oil on pruritus and xerosis in both the end-stage renal failure patients and healthy volunteers. A topical formulation containing 4% chia seed oil was used for 8 weeks and subjective assessment of dermatologic symptoms and functional measurements were performed.
MATERIALS AND METHODS
Subjects
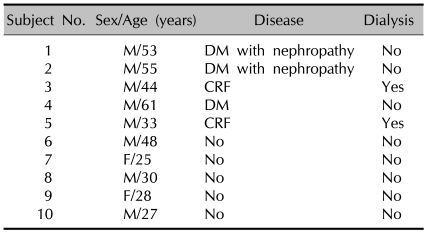
The subjects consist of 11 patients with diabetes, complicated with ESRD, who have been treated in the Department of Dermatology, Endocrinology, or Nephrology in Ansan Hospital, Korea University College of Medicine from Dec, 2007 to Mar, 2008, and 5 healthy volunteers having xerotic pruritus symptoms. Six of the 11 patients withdrew from the study due to personal reasons (and did not experience adverse effects of the tested products). Finally, 5 patients (3 patients with diabetes; 2 patients with ESRD) completed the study for 8 weeks. The 2 patients with ESRD were undergoing hemodialysis. The mean age of the 5 patients (all males) with underlying disease was 49 years. The 5 healthy volunteers with pruritus completed the study for 8 weeks without withdrawing. The mean age (3 males and 2 females) was 31.6 years (Table 1). Patients under dermatological treatment were excluded from the study and no other topical treatments were allowed for the subjects, except the topical chia seed oil containing moisturizers, during the test period.
Table 1.
Demographic property of the human subjects
DM: diabetes mellitus, CRF: chronic renal failure.
Study design
We assessed effectiveness of topical chia seed oil containing moisturizers as oil-in-water lotion formula with 4% chia seed oil for 8 weeks. For the comparison, moisturizers without chia seed oil were used as placebo samples. Subjects were allowed to apply the moisturizers to either the left or right side of body whenever needed, and thoroughly rubbed them in for high absorption of chia seed oil, until the colour of the moisturizer had disappeared. Placebo samples were also applied to the other side of body at the same time and in the same manner.
Subjects completed a questionnaire and rated their pruritus symptoms every 2 weeks. Along with the subjective measurements, functional measurements of skin conditions such as epidermal permeability barrier function, expressed by trans-epidermal water loss (TEWL), skin hydration (expressed by skin capacitance) and skin surface pH were also performed every 2 weeks.
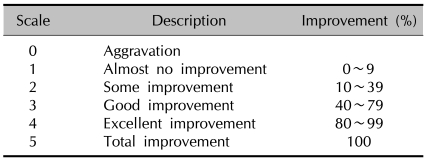
Subjective assessment
In order to evaluate the efficacy of topical chia seed oil containing moisturizers, subjective evaluation of degree of the satisfaction, the improvement of skin dryness, the improvement of pruritus, the improvement of abrasion, the improvement of lichen simplex chronicus, and the improvement of prurigo nodularis were all scored on a 6-point scale (0~5, 0, aggravation; 1, almost no improvement; 2, some improvement; 3, good improvement; 4, excellent improvement; 5, total improvement) (Table 2). Clinical photos were also taken, using a digital camera (DSC-F828®, Sony, Japan).
Table 2.
Questionnaire scales
Objective assessment
Every measurement performed between Dec, 2007 and Mar, 2008 and was carried out in an environmentally controlled room at a constant temperature 23±1℃, relative humidity 40±2%, and same lighting. TEWL values and skin capacitance were measured by the DermaLab (Cortex Technology, Hadsund, Denmark) and the corneometer (Corneometer CM-820, Courage-Khazaka Electronic GmbH, Cologne, Germany), respectively. Skin surface pH was measured by the Skin pH Meter PH900 (Courage-Khazaka Electronic GmbH, Cologne, Germany). All the values were arithmetic mean of 3 measurements. Results were compared for the moisturizer treated sites and placebo treated sites.
Statistical analysis
Statistical analysis was performed for evaluating the statistical significance test of subjective questionnaire and objective test, by non-paired two-tailed t-test. A p-value of less than 0.05 was considered statistically significant.
RESULTS
Subjective assessment
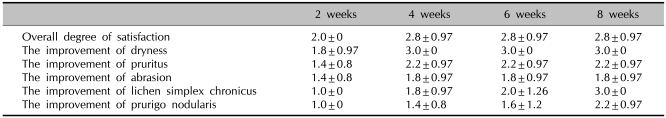
For the patients with end-stage renal failure or diabetes, increase of overall degree of the subjective satisfaction was observed at 2 weeks after treatment and, after 4 weeks, the satisfaction score was maintained till the end of the treatment. The score was improved from 2.0 (at 2 weeks) to 2.8 (at 8 weeks), but this difference was not statistically significant. Individual assessment for each symptom also showed an alleviating effect of chia seed oils. As shown in Table 3, the statistically significant improvement of skin dryness observed at 4 weeks after treatment and maintained (p<0.05). Similar improvement of lichen simplex chronicus and prurigo nodularis was also observed and was statistically significant (p<0.05). While the improvement was also observed for pruritus and abrasion, it was not statistically significant (p>0.05).
Table 3.
Subjective assessment of subjects with underlying disease
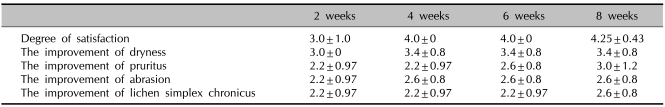
For the healthy volunteers having xerotic pruritus symptoms without underlying disease, a statistically significant increase of the overall degree of satisfaction was observed after 4 weeks of treatment (p<0.05) (Table 4). Similar to the patients with end-stage renal failure or diabetes, each symptom showed improvement in the subjective assessment. Statistical significance, however, was not observed for all the measured symptoms (p>0.05).
Table 4.
Subjective assessment of subjects without underlying disease
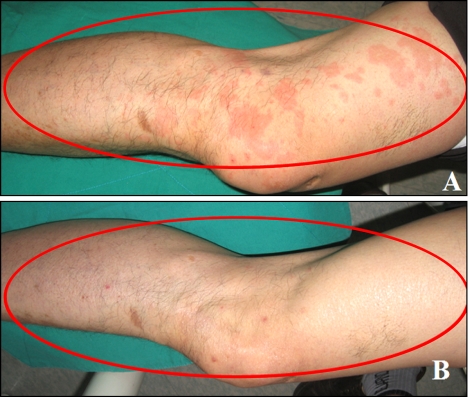
In addition, after 8 weeks of topical treatment, significant alleviation in lichenified brownish patches on the right dorsum of foot (Fig. 1) and erythematous wheal-like eruptions (Fig. 2) were observed in ESRD patients.
Fig. 1.
The severe lichenifed brownish patches on the right dorum of foot were improved after 8 weeks treatment. (A) Before the treatment. (B) After 8 weeks treatment.
Fig. 2.
The erythematous wheal-like eruptions were improved after 8 weeks treatment. (A) Before the treatment. (B) After 8 weeks treatment.
Functional measurement
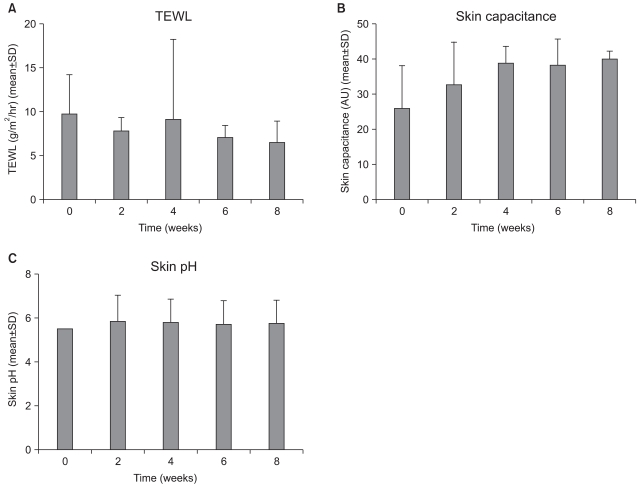
For the diseased patients, TEWL, as a representation of epidermal permeability barrier function, was normal for the applied areas. Topical treatment of either the chia seed oil containing moisturizers or placebos did not induce significant changes in TEWL values during the treatment period (Fig. 3A). However, skin capacitance, which represents the skin hydration, was below the normal values before the treatment, and gradually increased during the treatment time in the chia seed oil containing moisturizer-treated site. After 8 weeks of treatment, statistically significant improvement was observed, compared with basal condition (p<0.05) (Fig. 3B). No significant changes in skin surface pH were observed during the treatment period (Fig. 3C) for both the chia seed containing moisturizers or placebos treated sites.
Fig. 3.
Functional measurement of skin conditions for diseased skin during 8 weeks of treatment. Results of TEWL (A), skin capacitance (B), skin pH (C).
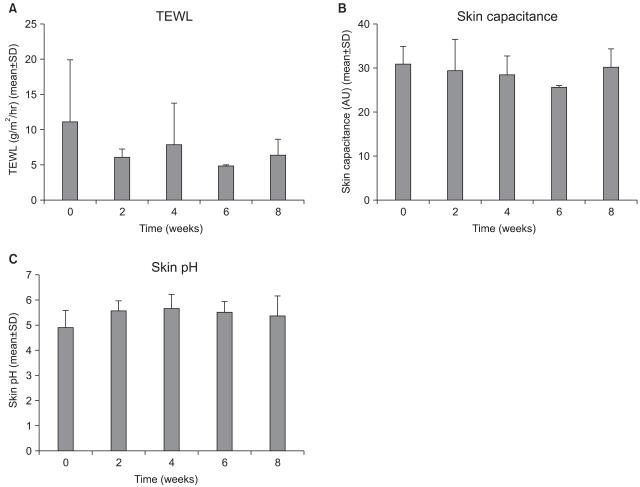
As for healthy volunteers, there were no significant changes in TEWL, skin capacitance or skin surface pH during the application period (Fig. 4).
Fig. 4.
Functional measurement of skin conditions for healthy volunteers during 8 weeks of treatment. Results of TEWL (A), skin capacitance (B), skin pH (C).
DISCUSSION
Pruritus may be experienced by up to 80% of hemodialysis patients7,8 and symptoms may be severe, distressing, and debilitating. The pruritic skin may appear normal except for dryness, but is often complicated by inflammatory lesions secondary to scratching9. Various therapeutic modalities have been developed for pruritus, especially associated with renal failure. The cornerstone of therapy for uremic pruritus is regular, intensive, efficient dialysis. Other non-pharmacologic measures consist of the use of non-complement-activating dialysis membranes, compliance with dietary restrictions, electric-needle (acupuncture) therapy, and ultraviolet light therapy. Pharmacological treatments that have been used include activated charcoal, antihistamines, capsaicin, cholestyramine, emollients and topical corticosteroids, epoetin, pizotyline, ketotifen, and nicergoline10. Efficient dialysis, dietary restrictions, phosphate-binding therapy, and phototherapy are the most effective treatments currently available10.
Essential fatty acids and their derivatives have a protective function, and influence structure and physiological characteristics11. Tamimi et al.7 firstly found that GLA (gamma-linolenic acid)-rich evening primrose oil which is rich in n-6 fatty acid, may be beneficial in alleviating uremic pruritus in some patients. It has been reported that atopic dermatitis patients who received GLA showed gradual improvements in pruritus, erythema, vesiculation and oozing11. N-3 fatty acid exhibits anti-inflammatory properties for many inflammatory diseases3,4, and oral supplementation of fish oils, which is rich in n-3 fatty acid, is known to be beneficial for relieving the pruritus5.
The purpose of this study was to evaluate the potential therapeutic benefits of chia seed oils on pruritic symptoms for ESRD patients and healthy volunteers. The objective evaluation, however, was difficult because pruritus was a subjective symptom. Functional measurement of skin conditions, which are known to be associated with pruritis, was also performed and TEWL, moisture content in stratum corneum, and skin pH were accessed as objective index. While there was no statistically significant difference, TEWL was decreased and the moisture content in the stratum corneum was increased in most patients and healthy volunteers with xerotic pruritus. In addition, these data also suggested that the tested topical formulas did not induce any significant skin disorder, which is verified by the TEWL changes during the treatment.
In conclusion, topical chia seed oil is effective for pruritus and xerosis treatment and is also beneficial for skin moisturization in healthy volunteers with xerotic pruritus, as well as patients with chronic renal failure or diabetes. Further studies with greater numbers of patients are needed, to confirm our promising preliminary results. Additional study is also necessary for evaluating the effectiveness of topical application of chia seed oil as an adjuvant therapy for chronic eczematous dermatitis such as atopic dermatitis with pruritus and xerosis.
References
- 1.Chen YC, Chiu WT, Wu MS. Therapeutic effect of topical gamma-linolenic acid on refractory uremic pruritus. Am J Kidney Dis. 2006;48:69–76. doi: 10.1053/j.ajkd.2006.03.082. [DOI] [PubMed] [Google Scholar]
- 2.Young AW, Jr, Sweeney EW, David DS, Cheigh J, Hochgelerenl EL, Sakai S, et al. Dermatologic evaluation of pruritus in patients on hemodialysis. N Y State J Med. 1973;73:2670–2674. [PubMed] [Google Scholar]
- 3.Bourre JM. Dietary omega-3 fatty acids for women. Biomed Pharmacother. 2007;61:105–112. doi: 10.1016/j.biopha.2006.09.015. [DOI] [PubMed] [Google Scholar]
- 4.Gil A. Polyunsaturated fatty acids and inflammatory diseases. Biomed Pharmacother. 2002;56:388–396. doi: 10.1016/s0753-3322(02)00256-1. [DOI] [PubMed] [Google Scholar]
- 5.Vergili-Nelsen JM. Benefits of fish oil supplementation for hemodialysis patients. J Am Diet Assoc. 2003;103:1174–1177. doi: 10.1016/s0002-8223(03)00984-2. [DOI] [PubMed] [Google Scholar]
- 6.Ayerza R, Jr, Coates W. Effect of dietary alpha-linolenic fatty acid derived from chia when fed as ground seed, whole seed and oil on lipid content and fatty acid composition of rat plasma. Ann Nutr Metab. 2007;51:27–34. doi: 10.1159/000100818. [DOI] [PubMed] [Google Scholar]
- 7.Tamimi NA, Mikhail AI, Stevens PE. Role of gamma-linolenic acid in uraemic pruritus. Nephron. 1999;83:170–171. doi: 10.1159/000045498. [DOI] [PubMed] [Google Scholar]
- 8.Murphy M, Carmichael AJ. Renal itch. Clin Exp Dermatol. 2000;25:103–106. doi: 10.1046/j.1365-2230.2000.00587.x. [DOI] [PubMed] [Google Scholar]
- 9.Ponticelli C, Bencini PL. Uremic pruritus: a review. Nephron. 1992;60:1–5. doi: 10.1159/000186696. [DOI] [PubMed] [Google Scholar]
- 10.Robertson KE, Mueller BA. Uremic pruritus. Am J Health Syst Pharm. 1996;53:2159–2170. doi: 10.1093/ajhp/53.18.2159. [DOI] [PubMed] [Google Scholar]
- 11.Andreassi M, Forleo P, Di Lorio A, Masci S, Abate G, Amerio P. Efficacy of gamma-linolenic acid in the treatment of patients with atopic dermatitis. J Int Med Res. 1997;25:266–274. doi: 10.1177/030006059702500504. [DOI] [PubMed] [Google Scholar]