Abstract
This case report reviews some of the clinical aspects of epidermal growth factor receptor (EGFR) inhibitor-induced rash, and, more importantly, it describes a specific case in which the diagnosis of such a rash occurred by means of a patient-initiated photographic electronic communication. The fact that this electronic communication was patient-initiated suggests that health care providers will likely be asked to make clinical decisions based on this type of communication soon and that this type of seemingly low-cost approach will likely become an important aspect of cancer symptom control and palliative care in the future.
Introduction
Oncologists often prescribe epidermal growth factor receptor (EGFR) inhibitors to patients with colon, lung, head and neck, or pancreas cancer.1,2 Although well-tolerated for the most part, these agents have as their most common side effect an acneiform-like rash that occurs on the face, torso, and extremities.1,2 Such rashes typically arise during the first 7–10 days after the initiation of EGFR inhibitors, occur in up to 80% of patients, and can be especially severe in 10%.1–3 In addition to the physical discomfort of cutaneous burning, these rashes more importantly cause “worry, frustration, and depression.”4 However, despite their appearance, the physical discomfort, and the emotional toll, these rashes are almost never lethal.5 From a palliative standpoint, randomized studies suggest that antibiotics, such as minocycline and tetracycline, might be helpful in lessening rash severity, but, without doubt, the most effective palliative strategy continues to be holding the EGFR inhibitor.6,7
Although oncologists commonly see and manage these rashes, other health care providers might not be as aware of them and may therefore be less comfortable in dealing with them. Moreover, a cancer patient who has only recently initiated therapy with an EGFR inhibitor may be frightened and concerned about the rash, even after having been previously counseled about it. This case report describes a patient-initiated, seemingly time- and cost-efficient diagnostic tool that enables healthcare providers to lend reassurance to patients when a severe EGFR inhibitor-induced rash occurs and when patients, their families, and other health care providers require further counseling on rash etiology and management.
Case Report
A 46-year-old man had started treatment with cetuximab for an incurable malignancy. The patient had been counseled earlier about rash development and, in fact, had been prescribed minocycline 250 mg twice per day as a preventive measure.
Despite this, the patient and his spouse became concerned when a rash developed shortly after starting cetuximab. Because he lived in a rural community, the patient sought help from his primary care provider and even a local dermatologist. The patient's spouse described how she had been told that, in fact, the minocycline was the cause of the rash, and the patient was advised to stop taking this antibiotic. He did so. Reportedly, no instructions were given to hold the cetuximab.
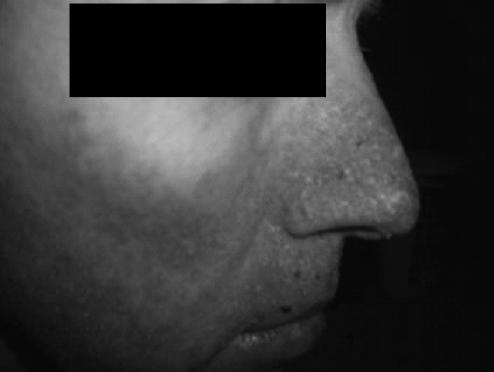
The patient's primary oncologist who practiced in a large, tertiary cancer center 4 hours from the patient's home was out of town when the patient's spouse called. An on-call oncologist, who had never met the patient or his wife, talked with the spouse, learned the information above, and attempted to provide reassurance by phone that the rash was very likely caused by cetuximab. This first phone call was followed by three others, with expressions of continued concern on the part of the spouse and requests for a more definitive confirmation of rash etiology and guidance on its management. Then because the patient was reluctant to drive 8 hours round-trip to have the on-call oncologist assess the rash, the patient's wife used a digital camera to photograph her husband's face and sent the image via electronic mail to the on-call oncologist (Fig. 1). The on-call oncologist reviewed this photograph and reassured the patient that the rash was in fact caused by the EGFR inhibitor. In a follow-up phone call to the patient's home several days later, the patient's spouse reported that the rash was still present but that now, having been reassured of its etiology, the patient was willing to continue with the cetuximab.
FIG. 1.
This figure shows an image (slightly modified to mask the patient's identity) that the patient's spouse had sent to the on-call oncologist.
Discussion
To our knowledge, this case report constitutes the first description of how a patient and family member initiated a highly informative, photographic electronic communication about an EGFR inhibitor-induced rash and thereby gained reassurance on its etiology and information on its management. These days, with the widespread use of cellular camera phones and the easy accessibility of electronic communication, this approach appears to be a rapid, inexpensive means to manage a cancer symptom that requires direct visualization. In this instance, the patient was spared driving 8 hours round-trip to see a medical oncologist who had familiarity with this drug-induced side effect. Although no one knows to what extent such electronic communications may already be taking place, this case report is unique in that the electronic transmission of information was patient-initiated, has not been previously reported in this context, and ultimately provided the necessary reassurance to both the patient and his spouse.
It should be noted that relatively few previous studies have discussed electronic communication in symptom control and palliative medicine. Previous such reports describe successful teleconferencing between health care providers in the setting of sparse health care resources and between patients and health care providers when the former live in rural settings.8–14 However, none of these interventions includes a patient-initiated electronic encounter, such as that reported here. Along similar lines, “tele-dermatology” has been of value in diagnosing rashes with accuracy in a pediatric clinic, in enabling patients with chronic skin conditions to maintain contact with their primary dermatologist with curtailed face-to-face clinic visits, in cutting costs in diagnosing skin cancers, and in reducing the need for a face-to-face dermatology referral by as much as 20% when this type of dermatology consultation was available to primary care providers.15–18 However, again, to our knowledge, none of these circumstances describes a direct, patient-initiated communication, as reported here.
Indeed, this case is unique and interesting largely because of this latter point. The fact that this approach was patient-driven suggests that health care providers will likely be asked to make clinical decisions based on this type of communication soon. In addition, the fact that this type of communication might be cost-effective, as suggested in the earlier reports referenced above,17 suggests that this approach will likely become an increasingly important aspect of cancer symptom control and palliative care in the future.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Lacouture ME. The growing importance of skin toxicity in EGFR inhibitor therapy. Oncology. 2009;23:194. 196. [PubMed] [Google Scholar]
- 2.Solomon BM. Jatoi A. Rash from EGFR inhibitors: Opportunities and challenges for palliation. Curr Oncol Rep. 2008;10:304–308. doi: 10.1007/s11912-008-0048-1. [DOI] [PubMed] [Google Scholar]
- 3.Jatoi A. Green EM. Fowland KM., Jr Clinical predictors of severe cetuximab-induced rash: Observations from 933 patients enrolled in North Central Cancer Treatment Group Study N0147. Oncology. 2009;77:120–123. doi: 10.1159/000229751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wagner LI. Lacouture ME. Dermatologic toxicities associated with EGFR inhibitors: The clinical psychologist's perspective. Impact on health-related quality of life and implications for clinical management of psychological sequelae. Oncology. 2007;21(Suppl 5):34–36. [PubMed] [Google Scholar]
- 5.Jatoi A. Nguyen PL. Do patients die from rashes from epidermal growth factor receptor inhibitors? A systematic review to help counsel patients about holding therapy. Oncologist. 2008;13:1201–1204. doi: 10.1634/theoncologist.2008-0149. [DOI] [PubMed] [Google Scholar]
- 6.Scope A. Agero AL. Disza SW. Myskowski PL. Lieb JA. Saltz L. Kemeny NE. Halpern AC. Randomized double-blind trial of prophylactic oral minocycline and topical tazarotene for cetuximab-associated acne-like eruption. J Clin Oncol. 2007;25:5390–5396. doi: 10.1200/JCO.2007.12.6987. [DOI] [PubMed] [Google Scholar]
- 7.Jatoi A. Fowland K. Sloan JA. Gross HM. Fishkin PA. Kahanic SP. Novotny PJ. Schaefer PL. Johnson DB. Tschetter LK. Loprinzi CL. Tetracycline to prevent epidermal growth factor receptor inhibitor-induced skin rashes: Results of a placebo-controlled trial from the North Central Cancer Treatment Group (N03CB) Cancer. 2008;113:847–853. doi: 10.1002/cncr.23621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Maserat E. Information communication technology: New approach for rural cancer care improvement. Asian Pac J Cancer Prev. 2008;9:811–814. [PubMed] [Google Scholar]
- 9.Phillips JL. Davidson PM. Newton PJ. Digiacomo M. Supporting patients and their caregivers after-hours at the end of life: The role of telephone support. J Pain Symptom Manage. 2008;36:11–21. doi: 10.1016/j.jpainsymman.2007.08.017. [DOI] [PubMed] [Google Scholar]
- 10.Bharadwaj P. Vasava S. Pisharodi S. Los Angeles to Mumbai: providing palliation using technology. J Palliat Med. 2007;10:1037–1039. doi: 10.1089/jpm.2007.0040. [DOI] [PubMed] [Google Scholar]
- 11.Czarnecki ML. Garwood MM. Weisman SJ. Advanced practice nurse-directed telephone management of acute pain following pediatric spinal fusion surgery. J Spec Pediatr Nurs. 2007;12:159–169. doi: 10.1111/j.1744-6155.2007.00109.x. [DOI] [PubMed] [Google Scholar]
- 12.Hebert MA. Paquin MJ. Whitten L. Cai P. Analysis of the suitability of ‘video-visits' for palliative home care: Implications for practice. J Telemed Telecare. 2007;13:74–78. doi: 10.1258/135763307780096203. [DOI] [PubMed] [Google Scholar]
- 13.Teunissen SC. Verhagen EH. Brink M. van der Linden BA. Voest EE. de Graeff A. Telephone consultation in palliative care for cancer patients: 5 years of experience in The Netherlands. Support Care Cancer. 2007;15:577–582. doi: 10.1007/s00520-006-0202-y. [DOI] [PubMed] [Google Scholar]
- 14.Maudlin J. Keen J. Kobb R. A road map for the last journey: Home telehealth for holistic end-of-life care. Am J Hosp Palliat Care. 2006;23:399–403. doi: 10.1177/1049909106290807. [DOI] [PubMed] [Google Scholar]
- 15.Heffner VA. Lyon VB. Brousseau DC. Holland KE. Yen K. Store-and-forward teledermatology versus in-person visits: A comparison in pediatric teledermatology clinic. J Am Acad Dermatol. 2009;60:956–961. doi: 10.1016/j.jaad.2008.11.026. [DOI] [PubMed] [Google Scholar]
- 16.Schreier G. Hayn D. Kastner P. Koller S. Salmhofer W. Hofmann-Wellenhof R. A mobile-phone based teledermatology system to support self-management of patients suffering from psoriasis. Conf Proc IEEE Eng Med Biol Soc. 2008;2008:5338–5341. doi: 10.1109/IEMBS.2008.4650420. [DOI] [PubMed] [Google Scholar]
- 17.Moreno-Ramirez D. Ferrandiz L. Ruiz-de-Casas A. Nieto-Garcia A. Moreno-Alvarez P. Galdeano R. Camacho FM. Economic evaluation of a store-and-forward teledermatology system for skin cancer patients. J Telemed Telecare. 2009;15:40–45. doi: 10.1258/jtt.2008.080901. [DOI] [PubMed] [Google Scholar]
- 18.Eminovic N. de Keizer NF. Wyatt JC. ter Riet G. Peek N. van Weert HC. Bruijnzeel-Koomen CA. Bindels PJ. Teledermatologic consultation and reduction in referrals to dermatologists: A cluster randomized controlled trial. Arch Dermatol. 2009;145:558–564. doi: 10.1001/archdermatol.2009.44. [DOI] [PubMed] [Google Scholar]