Abstract
A shortened version of the ABC 16-item scale (ABC-16), the ABC-6, has been proposed as an alternative balance confidence measure. We investigated whether the ABC-6 is a valid and reliable measure of balance confidence and examined its relationship to balance impairment and falls in older adults. Thirty-five community-dwelling older adults completed the ABC-16, including the six questions of the ABC-6. They also completed the following clinical balance tests: unipedal stance time (UST), functional reach (FR), Timed Up and Go (TUG), and maximum step length (MSL). Participants reported twelve-month falls history. Balance confidence on the ABC-6 was significantly lower than on the ABC-16, however scores were highly correlated. Fallers reported lower balance confidence than non-fallers as measured by the ABC-6 scale, but confidence did not differ between the groups with the ABC-16. The ABC-6 significantly correlated with all balance tests assessed and number of falls. The ABC-16 significantly correlated with all balance tests assessed, but not with number of falls. Test-retest reliability for the ABC-16 and ABC-6 was good to excellent. The ABC-6 is a valid and reliable measure of balance confidence in community-dwelling older adults, and shows stronger relationships to falls than does the ABC-16. The ABC-6 may be a more useful balance confidence assessment tool than the ABC-16.
Keywords: balance confidence, older adults, falls, balance impairment, clinical balance measures
1. Introduction
More than 35% of community-dwelling older adults fall at least once annually (Rubenstein, 2006). As the sequelae of falling are deleterious for this population, including loss of independence, severe injury, and death (Alexander et al., 1992; Cumming et al., 2000), it is important to identify which older adults are at increased risk for falling. Elucidating factors associated with balance impairment and which predispose the older adult to a fall is therefore an area of intense and ongoing investigation. Along with numerous other factors such as home environmental hazards (Northridge et al., 1995) and cognitive impairments (Van Dijk et al., 1993), low balance confidence has been shown to be closely associated with falls in older adults (Lajoie and Gallagher, 2004).
While there is no gold standard for assessing balance confidence, one commonly-used measure is the ABC scale (Powell and Myers, 1995). This 16-item scale, the ABC-16, includes questions addressing levels of balance confidence during performance of daily activities. Lower scores indicate lower levels of balance confidence, and are associated with balance-impairment (Cho et al., 2004) and falls (Lajoie and Gallagher, 2004) in older adults. Despite its utility as a predictor of balance impairment and falls, a significant drawback of the ABC-16 is that it may take up to 20 minutes to administer. Recently, a shortened version of the ABC-16, the ABC-6, has been proposed for clinical or research purposes. The ABC-6 includes the six most balance-challenging tasks from the original 16-item scale, making it considerably less time consuming to administer and more convenient for use in busy clinical or research settings (Peretz et al., 2006).
Though the validity of the ABC-16 as a measure of balance confidence in elderly populations has been established (Powell and Myers, 1995), there is limited research supporting the ABC-6 as a valid and reliable measure of balance confidence in older adults. A recent study in older adults with gait disorders and Parkinson's disease, which showed strong correlations between the two scales (Peretz et al., 2006), suggests that the ABC-6 may be a valid balance confidence measure. However, further studies are needed to validate the ABC-6 as a measure of balance confidence in community-dwelling older adults. Furthermore, the relationship of the ABC-6 to commonly-used clinical balance measures as well as to falls has not been examined. The purpose of this study was to further investigate the validity of the ABC-6 as a measure of balance confidence, examine its relationship to clinical measures of balance impairment and falls, and to determine the reliability of the scale in community-dwelling older adults. Based on previous work (Peretz et al., 2006), we hypothesized that the ABC-6 would be a valid measure of balance confidence in community-dwelling older adults. As the ABC-6 addresses the six most balance-challenging activities contained in the ABC-16, we also hypothesized that it would display stronger relationships with measures of balance impairment and falls in community-dwelling older adults than would the ABC-16.
2. Methods
This research study was approved by the Human Investigation Committee of Wayne State University.
2.1. Participants
Thirty-five community-dwelling older adults were recruited from response to flyers and person-to-person solicitation at senior centers and health fairs. To determine eligibility, a screening process took place prior to study admittance. Inclusionary criteria were: age 60 or older and community dwelling; able to stand bipedally for 30 seconds, and ambulatory (with or without an assistive device or lower extremity orthotic). Participants were excluded if they reported frequent pain in the back or lower extremities, were cognitively impaired as assessed using the Short Orientation-Memory-Concentration test (Wade and Vergis, 1999), were medically unstable as established by medical history (e.g., active and uncontrolled cardiopulmonary, infectious, inflammatory, or terminal conditions), or reported previous stroke or other neurological diseases. Following informed consent, participants' height, weight, and number of falls in the past 12 months were recorded. A fall was defined as inadvertently coming to rest at a lower level including supportive surfaces or the floor. Participants underwent a series of clinical assessments focusing on balance confidence and balance.
2.2. Assessments
2.2.1. The ABC scale
Balance confidence was assessed using the ABC-16, a valid measure of balance confidence in older adults (Powell and Myers, 1995). Thirty-five participants completed the ABC-16 at the first session, and a subset of participants (n = 18) were selected to complete the ABC-16 a second time approximately 30 days later. Participants rated their balance confidence on a scale of 0% (not confident) to 100% (completely confident) following a series of 16 questions regarding balance-challenging tasks. The tasks include the following: Q1. walking around the house, Q2. walking up or down stairs, Q3. bending over to pick up a slipper from the floor, Q4. reaching for a small can off the shelf at eye level, Q5. standing on tip toes reaching for something above your head, Q6. standing on a chair reaching for something, Q7. sweeping the floor, Q8. walking outside the house to a car parked in the driveway, Q9. getting into or out of a car, Q10. walking across a parking lot to the mall, Q11. walking up or down a ramp, Q12. walking in a crowded mall where people rapidly walk past you, Q13. bumped into by people as you walk through the mall, Q14. walking onto or off an escalator while holding onto a railing, Q15. walking onto or off an escalator while holding onto parcels such that you cannot hold onto the railing, and Q16. walking outside on an icy sidewalk. Balance confidence for the ABC-16 was scored as the mean of the 16 responses and was reported as a confidence percentage. Balance confidence for the ABC-6 was determined by taking the mean of 6 responses identified in Peretz et al. (2006): questions 5, 6, and 13 through 16 of the ABC-16, and was reported as a confidence percentage.
2.2.2. Clinical balance measures
UST, a static balance test, is the time a participant can stand on one leg. Single-leg balance is a predictor of injurious falls in older adults (Vellas et al., 1997). UST was administered as described (Goldberg et al., 2005). One practice trial preceded two experimental trials and the best time was recorded as UST. FR, a reliable measure of dynamic balance, postural control, and margin of stability (Duncan et al., 1990), was administered and recorded as described (Goldberg et al., 2005). The TUG test is a reliable measure for quantifying dynamic balance and functional mobility in older adults (Podsiadlo and Richardson, 1991). TUG has a sensitivity and specificity of 87% in predicting falls in older adults (Shumway-Cook et al., 2000). TUG was administered as described (Goldberg et al., 2005). One practice trial preceded two experimental trials and TUG was reported as the mean time of two trials. MSL is a reliable measure of dynamic balance and stepping ability (Medell and Alexander, 2000; Cho et al., 2004). MSL was administered and recorded as described in (Goldberg et al., 2005), however the participants' arms remained at their sides.
2.3. Data analysis
Data were tested for normality using the Kolmogorov-Smirnov test. As the data conformed to a normal distribution, all statistical analyses were conducted using parametric statistics. Descriptive statistics were calculated for demographic and anthropometric variables, clinical balance measures, number of falls, and balance confidence scores. A paired t-test was used to determine whether mean scores on the two forms of the ABC scale differed significantly. Between-group comparisons (i.e., fallers versus non-fallers) for each of the balance confidence scales were evaluated using independent samples t-tests. The relationship between the two forms of the ABC scale, as well as their relationships to clinical balance tests and falls, were evaluated using Pearson's product moment correlation coefficient (Pearson's r). A subset of participants (n=18) were administered the ABC-16 scale on two separate occasions, separated by approximately 30 days to determine intrarater test-retest reliability of the ABC-16 and ABC-6 scales using intraclass correlation coefficients (ICC) (Shrout and Fleiss, 1979). Significance was set at a p ≤ 0.05.
3. Results
3.1. Participant characteristics, clinical balance, and falls
Thirty-five older adults were included in this study (80% female). Demographic and anthropometric characteristics for the sample include mean and standard error of the mean (S.E.M) for age (72.86 ± 1.05 years), body mass index (BMI) (28.82 ± 1.14 kg/m2), height (1.65 ± 0.02 m), and weight (78.45 ± 2.97 kg). Clinical balance and falls data indicate a wide range of balance capabilities (Table 1). Number of falls ranged from zero to three within the last 12 months (excluding a participant reporting daily falls). Nineteen individuals reported no falls, seven reported one fall, seven reported two falls, one reported three falls, and one reported daily falls. The sample included persons at risk for a future fall based on history of falls (n = 16), and a subcategory of those fallers at risk for injurious falls based on UST scores of less than five seconds (n = 8) (Vellas et al., 1997). The range of scores on the FR and MSL tests further highlights the variability of balance capabilities represented within this sample.
Table 1.
Clinical balance measures and falls in 35 older adults
| Mean ± S.E.M | 95% CI | Range | |
|---|---|---|---|
| Clinical balance measures | |||
| UST (sec) | 12.72 ± 1.74 | 9.20 – 16.25 | 0.00 – 30.00 |
| MSL (cm) | 70.17 ± 3.23 | 63.61 – 76.73 | 29.72 – 116.08 |
| MSL (% of height) | 42.27 ± 1.78 | 38.65 – 45.89 | 18.57 – 64.59 |
| FR (cm) | 26.27 ± 1.16 | 23.91 – 28.64 | 15.24 – 42.33 |
| FR (% of height) | 15.83 ± 0.64 | 14.52 – 17.13 | 9.52 - 24.60 |
| TUG (sec) | 12.35 ± 0.49 | 11.35 – 13.34 | 9.17 - 22.40 |
| Number of falls* | 0.71 ± 0.16 | 0.39 – 1.02 | 0.00 – 3.00 |
Number of falls is reported for 34 participants excluding 1 participant who reported daily falls.
3.2. Balance confidence
There was a significantly lower mean (± S.E.M.) balance confidence score on the ABC-6 (74.38 ± 3.54) than on the ABC-16 (84.70 ± 2.30) (p < 0.001). Despite this difference, the ABC-6 score was significantly correlated with the ABC-16 score (r = 0.95; p < 0.001).
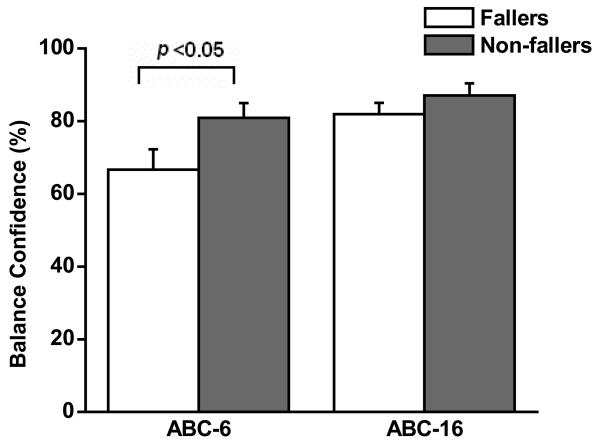
Balance confidence mean score (± S.E.M.) for fallers (66.65 ± 5.56) was significantly lower than that of non-fallers (80.88 ± 4.09) on the ABC-6 (p < 0.05) (Figure 1). However, the mean scores of fallers (81.94 ± 3.10) and non-fallers (87.02 ± 3.32) were not significantly different on the ABC-16 (p > 0.05).
Figure 1.
Balance confidence using two versions of the ABC scale for fallers and non-fallers. Scores on the ABC-6 were significantly lower in fallers than in non-fallers (p<0.05) while scores on the ABC-16 were not significantly different between the groups. Error bars represent S.E.M.
Single rater test-retest reliability of the two ABC scales over a 30 day period was good to excellent. The ICC for the ABC-16 was 0.76 while the ICC for the ABC-6 was 0.82.
3.3. Relationships between balance measures and balance confidence scales
The ABC-6 correlated significantly with all four clinical balance measures (i.e., UST r = 0.48, p ≤ 0.01; MSL r = 0.73, p ≤ 0.001; FR r = 0.34, p ≤ 0.05; and TUG r = −0.69, p ≤ 0.001) such that lower balance confidence was associated with poorer performance on balance tests, while higher balance confidence was associated with better performance on balance tests (Table 2). The ABC-16 also correlated significantly with all clinical balance measures: UST r = 0.46, p ≤ 0.01; MSL r = 0.69, p ≤ 0.001; FR r = 0.33, p ≤ 0.05; and TUG r = −0.65, p ≤ 0.001 (Table 2). ABC-6 correlated significantly with number of falls (r = −0.33, p ≤ 0.05), however, this was not the case for the ABC-16 (r = −0.17, p > 0.05). In summary, these correlations suggest that not only does balance confidence based on the ABC-6 correlate as well as the ABC-16 with balance performance measures, but in contrast to the ABC-16, it also correlates significantly with number of falls.
Table 2.
Pearson correlation coefficients (r) between the clinical balance measures, falls and 2 versions of the ABC scale
| ABC-6 | p ≤ | ABC-16 | p ≤ | |
|---|---|---|---|---|
| Balance measures | ||||
| UST | 0.48 | 0.01 | 0.46 | 0.01 |
| MSL (% of height) | 0.73 | 0.001 | 0.69 | 0.001 |
| FR (% of height) | 0.34 | 0.05 | 0.33 | 0.05 |
| TUG | −0.69 | 0.001 | −0.65 | 0.001 |
| Number of falls | −0.33 | 0.05 | −0.17 | NS |
Notes: MSL and FR were normalized for body height prior to computation of Pearson's r.
NS: not significant
4. Discussion
As the ABC-16 is a valid balance confidence measure (Powell and Myers, 1995), a strong relationship between the ABC-6 and the ABC-16 would support the ABC-6 as a valid measure of balance confidence. Research involving older adults with neurological disease and also healthy community-dwelling older adults has demonstrated a strong correlation between the two scales (Peretz et al., 2006). Strong correlations observed here between the two scales support this finding, confirming the ABC-6 to be a valid measure of balance confidence in community-dwelling older adults. We further analyzed this relationship, revealing that ABC-6 scores for the entire sample were significantly lower than ABC-16 scores, supporting that the items included on the ABC-6 address more balance-challenging activities. In addition, ICCs of 0.76 (ABC-16) and 0.82 (ABC-6) were good to excellent (Portney and Watkins, 2009), suggesting that they are reliable measures of balance confidence.
Associating the ABC-16 scores to balance performance measures revealed strong correlations with all balance measures assessed, indicating a relationship between higher balance confidence and better balance performance. This relationship confirmed results of a previous study (Cho et al., 2004) which showed similar relationships of the ABC-16 with UST, MSL, and TUG. Extending these findings, we found that the ABC-6 also showed strong correlations with all balance measures assessed in this study. As with the ABC-16, these correlations suggest that higher balance confidence as assessed with the ABC-6 is associated with better balance capabilities. Correlation of the ABC-6 and ABC-16 with clinical balance measures indicates that both may be useful as part of an overall screen for balance impairment.
The ABC-6 differentiated between fallers and non-fallers; however the ABC-16 did not. This finding regarding the ABC-16 is contradictory to previous findings (Lajoie and Gallagher, 2004), which showed that the ABC-16 could differentiate between fallers and non-fallers in older adults. This discrepancy may be due to disparities between our sample and the sample of older adults in the previous study (e.g., the previous study included persons from nursing homes whereas ours were community-dwelling). Furthermore, when considering self-reported falls in the past 12 months, there was a significant correlation between the ABC-6 and number of falls, but not between the ABC-16 and number of falls. These findings (i.e., the capability of the ABC-6 to differentiate fallers from non-fallers as well as its significant correlation to number of falls, both of which were not observed for the ABC-16) suggest that the ABC-6 exhibits stronger relationships to falls than does the ABC-16.
Our study revealed clear differences between the two scales in this cohort of community-dwelling older adults: significantly lower mean confidence scores for the ABC-6; ability of the ABC-6 to differentiate between fallers and non-fallers; and significant correlation of the ABC-6 to number of falls. The content of each scale may provide explanation of these differences. The ABC-6 includes activities from a narrow spectrum of difficulty, all of which have consistently received the lowest confidence scores when individually analyzed from the 16-item scale (Powell and Myers, 1995; Peretz et al., 2006). Therefore, the ten additional activities included in the ABC-16 may inflate overall confidence levels reported. For instance, older adults who have extremely poor balance confidence may still express 100% confidence in reaching at eye level (item 4 on the ABC-16, not included on the ABC-6). An inflated number such as this could increase overall percentage confidence reported, potentially resulting in over-estimation of true balance confidence and decreasing the ability to detect older adults who may fall using the ABC-16.
The clinical implications of our findings are encouraging for professionals working with the older adult population. Along with its parent version, the ABC-6 is a valid and reliable measure of balance confidence. Importantly, however, the ABC-6 takes less time to administer, making it more efficient for assessing balance confidence, particularly in busy clinical or research settings. Furthermore, as the ABC-6, but not the ABC-16, detected fallers from non-fallers and also significantly correlated with number of falls, the shortened scale may be more useful than the ABC-16 as a measure of falls risk in community-dwelling older adults.
Though there were significant relationships between all of the clinical balance measures and both balance confidence scales, the strongest relationships resulted from the dynamic balance measures (MSL and TUG) rather than the static balance measure (UST) or the partially dynamic balance measure (FR). We are currently investigating additional balance measures with varying levels of dynamic requirements as predictors of balance confidence. This analysis may provide insight into the balance components most useful to incorporate into interventions aimed at improving balance confidence.
Consideration of this study's findings within the boundaries of its limitations highlights avenues for future research. Participants were asked to report falls in the past 12 months, a retrospective recall which may be inaccurate (Peel, 2000). Future studies should focus on prospective methods of falls report to confirm our finding of a significant relationship between ABC-6 and falls in older adults. A study comparing the ABC-6 to other balance confidence scales such as the Falls Efficacy Scale (Tinetti et al., 1990) will provide further validation of the ABC-6. To detect changes in balance confidence based on the ABC-16 compared to the ABC-6, studies should determine the effectiveness of interventions aimed at improving balance confidence in frail older adults at high risk for a fall. Finally, if the ABC-6 is to be used as a screening tool for balance impairments in clinical settings, sensitivity and specificity analyses should be conducted, particularly with high falls risk populations.
5. Conclusion
These results not only indicate that the ABC-6 is a valid and reliable measure of balance confidence in community-dwelling older adults, but also that the short scale shows stronger relationships to falls than does the ABC-16. The ABC-6 may be a more useful balance confidence assessment tool than the ABC-16 in busy clinical or research settings, where timely, valid, and reliable assessments of balance confidence and screenings for balance impairments and falls risk assessment measures are necessary.
Acknowledgements
Funding for this study was provided by a Del Harder Rehabilitation Award from the Rehabilitation Institute of Michigan to Dr. Allon Goldberg. Stacey Schepens is supported by an NIH/NIA Pre-Doctoral Training Fellowship in Aging and Urban Health. Stacey Schepens and Melissa Wallace are supported by Graduate-Professional Scholarships from the Graduate School of Wayne State University. The financial sponsors played no role in the design, execution, analysis, and interpretation of data, or writing of the study.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest statement: None.
References
- Alexander BH, Rivara FP, Wolf ME. The cost and frequency of hospitalization for fall-related injuries in older adults. Am. J. Publ. Health. 1992;82:1020–1023. doi: 10.2105/ajph.82.7.1020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cho BL, Scarpace D, Alexander NB. Tests of stepping as indicators of mobility, balance, and fall risk in balance-impaired older adults. J. Am. Geriatr. Soc. 2004;52:1168–1173. doi: 10.1111/j.1532-5415.2004.52317.x. [DOI] [PubMed] [Google Scholar]
- Cumming RG, Salkeld G, Thomas M, Szonyi G. Prospective study of the impact of fear of falling on activities of daily living, SF-36 scores, and nursing home admission. J. Gerontol. A: Biol. Sci. Med. Sci. 2000;55:M299–M305. doi: 10.1093/gerona/55.5.m299. [DOI] [PubMed] [Google Scholar]
- Duncan PW, Weiner DK, Chandler J, Studenski S. Functional reach: a new clinical measure of balance. J. Gerontol. 1990;45:M192–M197. doi: 10.1093/geronj/45.6.m192. [DOI] [PubMed] [Google Scholar]
- Goldberg A, Hernandez ME, Alexander NB. Trunk repositioning errors are increased in balance-impaired older adults. J. Gerontol. A: Biol. Sci. Med. Sci. 2005;60:M1310–M1314. doi: 10.1093/gerona/60.10.1310. [DOI] [PubMed] [Google Scholar]
- Lajoie Y, Gallagher SP. Predicting falls within the elderly community: comparison of postural sway, reaction time, the Berg balance scale and the Activities-specific Balance Confidence (ABC) scale for comparing fallers and non-fallers. Arch. Gerontol. Geriatr. 2004;38:11–26. doi: 10.1016/s0167-4943(03)00082-7. [DOI] [PubMed] [Google Scholar]
- Medell JL, Alexander NB. A clinical measure of maximal and rapid stepping in older women. J. Gerontol. A: Biol. Sci. Med. Sci. 2000;55:M429–M433. doi: 10.1093/gerona/55.8.m429. [DOI] [PubMed] [Google Scholar]
- Northridge ME, Nevitt MC, Kelsey JL, Link B. Home hazards and falls in the elderly: the role of health and functional status. Am. J. Public Health. 1995;85:509–515. doi: 10.2105/ajph.85.4.509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peel N. Validating recall of falls by older people. Accident; Analysis and Prevention. 2000;32:371–372. doi: 10.1016/s0001-4575(99)00066-4. [DOI] [PubMed] [Google Scholar]
- Peretz C, Herman T, Hausdorff JM, Giladi N. Assessing fear of falling: Can a short version of the Activities-specific Balance Confidence scale be useful? Mov. Disord. 2006;21:2101–2105. doi: 10.1002/mds.21113. [DOI] [PubMed] [Google Scholar]
- Podsiadlo D, Richardson S. The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J. Am. Geriatr. Soc. 1991;39:142–148. doi: 10.1111/j.1532-5415.1991.tb01616.x. [DOI] [PubMed] [Google Scholar]
- Portney LG, Watkins MP. Foundations of Clinical Research: Applications to Practice. Pearson Education, Inc.; Upper Saddle River, N.J.: 2009. [Google Scholar]
- Powell LE, Myers AM. The Activities-specific Balance Confidence (ABC) Scale. J. Gerontol. A: Biol. Sci. Med. Sci. 1995;50A:M28–M34. doi: 10.1093/gerona/50a.1.m28. [DOI] [PubMed] [Google Scholar]
- Rubenstein LZ. Falls in older people: epidemiology, risk factors and strategies for prevention. Age Ageing. 2006;35(Suppl 2):ii37–ii41. doi: 10.1093/ageing/afl084. [DOI] [PubMed] [Google Scholar]
- Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol. Bull. 1979;86:420–428. doi: 10.1037//0033-2909.86.2.420. [DOI] [PubMed] [Google Scholar]
- Shumway-Cook A, Brauer S, Woollacott M. Predicting the probability for falls in community-dwelling older adults using the Timed Up & Go Test. Phys. Ther. 2000;80:896–903. [PubMed] [Google Scholar]
- Tinetti ME, Richman D, Powell L. Falls efficacy as a measure of fear of falling. J. Gerontol. 1990;45:P239–P243. doi: 10.1093/geronj/45.6.p239. [DOI] [PubMed] [Google Scholar]
- Van Dijk PT, Meulenberg OG, Van de Sande HJ, Habbema JD. Falls in dementia patients. Gerontologist. 1993;33:200–204. doi: 10.1093/geront/33.2.200. [DOI] [PubMed] [Google Scholar]
- Vellas BJ, Wayne SJ, Romero L, Baumgartner RN, Rubenstein LZ, Garry PJ. One-leg balance is an important predictor of injurious falls in older persons. J. Am. Geriatr. Soc. 1997;45:735–738. doi: 10.1111/j.1532-5415.1997.tb01479.x. [DOI] [PubMed] [Google Scholar]
- Wade DT, Vergis E. The short orientation-memory-concentration test: a study of its reliability and validity. Clin. Rehab. 1999;13:164–170. doi: 10.1191/026921599673848768. [DOI] [PubMed] [Google Scholar]