Abstract
Background
Hysterectomy is one of the most common surgical procedures performed in the United States. The purpose of this study is to examine the association between socioeconomic indicators and hysterectomy.
Study Design
We performed a cross-sectional analysis of the 2004 Behavioral Risk Factor Surveillance Survey database. The effect of multiple socioeconomic exposures (education level, annual income, and employment status) on hysterectomy status was evaluated. Logistic regression was used to estimate odds ratios between the multiple exposures and the outcome of hysterectomy status.
Results
Our analytic sample included 180,982 women. Prior hysterectomy was reported by 26.4%. After adjusting for confounders, women who had not graduated from high school had 1.75 times higher odds (95% CI 1.68 to 1.83) of having a hysterectomy compared to women who were college graduates; and women with an annual household income of less than $15,000 had 1.06 times higher odds (95% CI 1.02 to 1.10) of having a hysterectomy compared to women who reported an income of greater than $50,000/year. Women who were unemployed did not have higher odds of having a hysterectomy than women who were employed.
Conclusion
Socioeconomic indicators of education level and income are associated with hysterectomy status, however employment status is not.
Keywords: Hysterectomy, socioeconomic status, education, income, employment
INTRODUCTION
One of the most common surgical procedures performed in the United States is hysterectomy with over 600,000 procedures performed each year.1,2 Ninety-five percent of hysterectomies are performed for benign reasons, including: uterine leiomyomas, abnormal uterine bleeding, and pelvic organ prolapse.3 Although hysterectomies for benign reasons may improve symptoms, other less invasive management strategies do exist: hormonal therapy, levonorgestrel intra-uterine devices, endometrial ablation, and uterine artery embolization. With these newer surgical and medical developments, hysterectomy rates in the United States were noted to have declined nationally between 1980 and 1993.4,5 This trend in declining hysterectomy rates for benign indications was also reported in the membership of the Kaiser Permanente Northern California system with a 15% decline in hysterectomy rates between 1994 and 2003 as well as in Ohio between 1988 and 1994.6,7 Due to newer options, there is some debate whether hysterectomies may be over-performed.8
The relationship of socioeconomic indicators and hysterectomy status has previously been studied. Some studies have suggested that ethnic/racial differences are associated with hysterectomy status; other indicators such as income, education level, and employment status have not been explored in detail.3,9,10 The purpose of this study is to examine the relationship between three indicators of socioeconomic status measured by annual household income, education level, and employment status and past hysterectomy in women in the United States using the 2004 Behavioral Risk Factors Surveillance Survey (BRFSS).
METHODS
Data Source and Population
The Center for Disease Control and Prevention (CDC) conducts an annual ongoing, cross-sectional survey in 49 states, the District of Columbia, Guam, Puerto Rico, and the Virgin Islands of risk factors for chronic diseases and health status in the United States, the BRFSS. The 2004 BRFSS database is available for analysis through the CDC website and was accessed for this study for secondary analysis in February 2007.11 This national telephone survey is designed to collect uniform and reproducible information on perceived health status and preventable risk factors for several chronic diseases, even in people who do not regularly seek medical attention. Data from this survey provide public health officials vital information on obesity, tobacco abuse, and physical activity. In addition, the survey has an annual set of core questions on socioeconomic status that include questions on education, income, and employment.
For the BRFSS, states use a telephone-based survey to collect data from a representative sample of households with telephones. Surveys are administered in Spanish for Spanish-speaking participants. Most states use either a disproportionate stratified sample or a Mitofsky-Waksberg type sample design to draw a random sample from the set of all possible telephone numbers based on area codes and pre-fixes. Finally, data collected can then be weighted to represent the total United States population. 12
The population at risk for this study included all women who participated in the survey. Women with non-responses to the outcome question of “Have you had a hysterectomy?” were excluded. Also, women whose age was not available were excluded, because age can have a large confounding effect on hysterectomy status. This was less than 1% of the total population at risk. Thus there was an analytic sample of women whose age and hysterectomy status were known. The BRFSS does not provide any details regarding the indications for hysterectomy or type of hysterectomy performed; therefore only information on hysterectomy status is available.
Study Variables
Our outcome of interest was prior hysterectomy. Hysterectomy status was defined by a woman's answer to the question “Have you had a hysterectomy?” and was analyzed as a dichotomous variable (yes/no). Independent socioeconomic status variables analyzed included annual household income, highest level of education, and employment status.
For our analysis, income categories were as follows: less than $15,000 (chosen as the poverty level for annual household income for a household of three in the continental United States); $15,000 to $49,999, >$50,000, and refused. Annual household income has repeatedly been shown to be one of the most sensitive questions for participants to answer on surveys. Because of the large number of women who did not provide an answer, did not know their annual household income, or had missing data for this question, all these women were categorized in a separate category as "refused".
Education level in the BRFSS was recorded as a woman's response to the question, “What was the highest grade or year of school you completed?” Women reporting no education, elementary education, and some high school were grouped into one category of “less than high school”. Women completing the 12th grade or reporting attainment of GED were categorized as having “completed high school”. Women reporting additional college level course work or technical school were categorized as having “some college”. Women who reported a college diploma or greater were labeled as a “college graduate”. Less than one percent of our analytic sample had missing data for the category of education and these women were excluded from our final analysis.
Employment status was defined as a woman's response to the question, “Are you currently employed for wages, self-employed, unemployed for less than 12 months, unemployed for more than 12 months, disabled, retired, a homemaker, or a student?” Women employed for wages and self-employed were categorized as “employed.” Women out of work for more than 1 year, less than 1 year, and disabled were grouped into a single category of “unemployed.” Students, homemakers, and retired subjects were grouped into a single category of “not in labor force.” Less than one percent of our analytic sample had missing data for the category of employment status and these women were excluded from our final analysis.
Statistical Analysis
Data from the BRFSS was weighted to represent the total United States population. Descriptive statistics were used to describe demographic and clinical data on subjects. Simple logistic regression was performed to estimate the crude odds ratio between the three indicators of socioeconomic status and hysterectomy status. We then performed multivariable logistic regression using likelihood ratio testing with forward and backward selection (p<.05) of the independent variables to the logistic regression model. All independent variables explored were categorical, and included: education level, annual household income, employment status, insurance status, age, race, and geographic region of the country. Insurance status did not affect the model and was omitted from the final model. Interactions between the three socioeconomic indicators of education level, employment status, and annual household income were assessed. Statistical analysis was performed with the use of STATA SE 9.2 software system (STATACORP, College Station, TX).
RESULTS
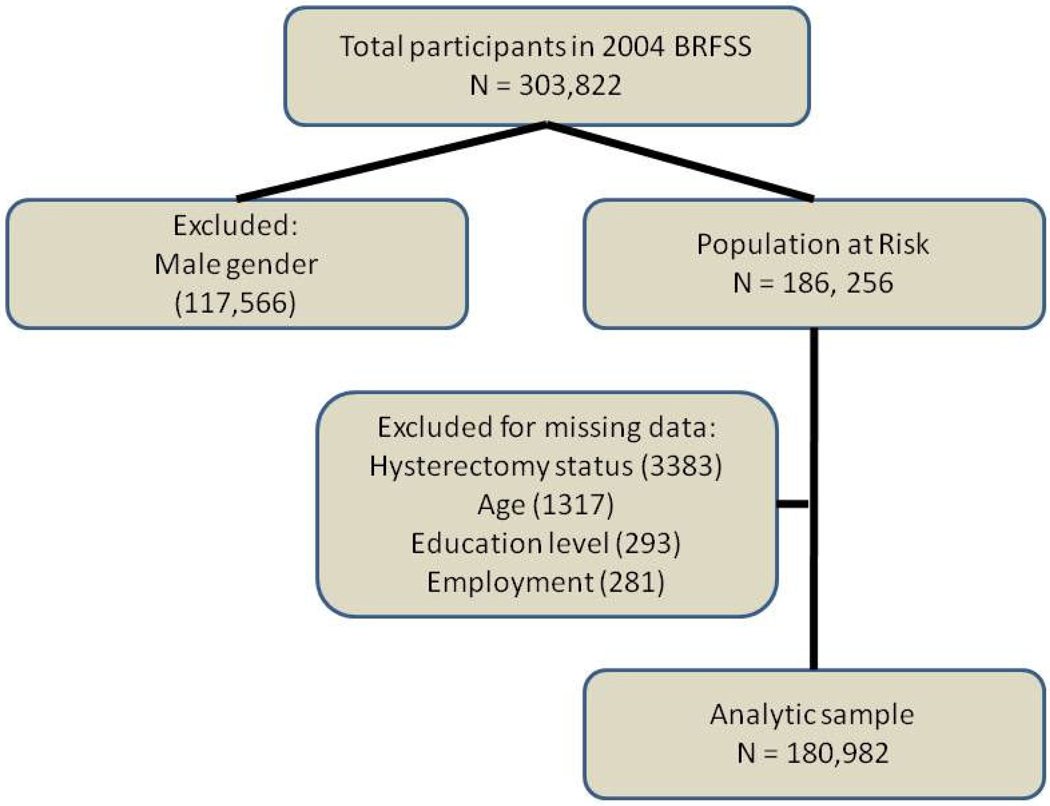
The total number of women meeting our inclusion criteria was 180,982 (Figure 1). The mean age was 50.76 years old (95% CI 50.7 to 50.8). Twenty-six percent (n=47,727) of women reported having had a prior hysterectomy.
Figure 1.
Flowchart of exclusion criteria to arrive at final analytic sample
Women with missing data for education level (n = 293, 0.16%) or employment status (n = 281, 0.15%) were excluded from analysis. A much larger percentage of women were missing data on self-reported annual household income level (n = 26,613, 14.7%). These women were grouped into a separate category, “refused”, for analysis.
The results of our simple and multivariable logistic regression models are summarized in Table I. After adjusting for age, race, and region of the country, women who had not graduated from high school had a 1.75 times higher odds (95% CI 1.68 to 1.83) of having a hysterectomy compared to women who reported graduation from college. Women who were not in the labor force (student, homemaker, or retired) had a 1.23 times higher odds (95% CI 1.20 to 1.27) as women who reported being employed for wages of having a hysterectomy, however women who were unemployed did not have an increased odds of hysterectomy compared to employed women. Compared to women who reported an annual household income of greater than $50,000, women who reported an income of less than $15,000 had a 1.06 times higher odds (95% CI 1.02 to 1.11) of having a hysterectomy.
Table I.
Association between Women’s Characteristics and Hysterectomy Status: Bi-variate analysis and logistic regression
| Women’s characteristics | Total N=180,982 |
Had hysterectomy (%) |
Bi-variate Analysis [Crude OR (95% CI)] |
Multivariable Analysis [Adjusted OR (95% CI)] |
|---|---|---|---|---|
| Age at questionnaire (y) | ||||
| 18 to 45 | 74,583 | 7.6 | Reference | Reference |
| 46 to 54 | 32,792 | 28.2 | 4.76 (4.6 to 4.94) | 5.00 (4.82 to 5.19) |
| 55 & older | 73,607 | 44.6 | 9.76 (9.47 to 10.1) | 8.73 (8.44 to 9.02) |
| Region of country | ||||
| Northeast | 39,762 | 19.1 | Reference | Reference |
| Southeast | 46,912 | 31.9 | 1.98 (1.92 to 2.05) | 2.03 (1.97 to 2.11) |
| Midwest | 40,855 | 26.0 | 1.49 (1.44 to 1.54) | 1.50 (1.44 to 1.56) |
| West | 49,158 | 27.7 | 1.62 (1.57 to 1.68) | 1.80 (1.74 to 1.87) |
| Other | 4,295 | 21.5 | 1.16 (1.07 to 1.26) | 1.33 (1.21 to 1.45) |
| Race | ||||
| White | 141,399 | 27.4 | Reference | Reference |
| Black | 16,756 | 25.6 | .91 (.88 to .95) | 1.08 (1.04 to 1.13) |
| Hispanic | 13,737 | 18.4 | .60 (.57 to 63) | .79 ( .75 to .83) |
| Other | 9,090 | 24.1 | .84 (.80 to .88) | Not significant |
| Education Level | ||||
| College graduate | 54,269 | 17.8 | Reference | Reference |
| Some college | 50,462 | 26.5 | 1.66 (1.61 to 1.71) | 1.51 (1.46 to 1.56) |
| High school graduate | 56,366 | 31.0 | 2.07 (2.01 to 2.13) | 1.61 (1.56 to 1.67) |
| Less than high school | 19,885 | 36.3 | 2.62 (2.53 to 2.72) | 1.75 (1.68 to 1.83) |
| Reported annual income level | ||||
| Greater than 50K | 51,256 | 19.1 | Reference | Reference |
| 15 to 50 K | 79,374 | 27.1 | 1.57 (1.53 to 1.61) | 1.06 (1.03 to 1.10) |
| Less than 15 K | 23,739 | 33.0 | 2.08 (2.02 to 2.16) | 1.06 (1.02 to 1.11) |
| Refused | 26,613 | 32.3 | 2.02 (1.95 to 2.09) | Not significant |
| Employment status | ||||
| Employed | 95,507 | 18.9 | Reference | Reference |
| Out of work | 8,311 | 19.6 | 1.03 ( .98 to 1.10) | Not significant |
| Not in labor force | 77,738 | 36.3 | 2.44 (2.38 to 2.50) | 1.23 (1.20 to 1.27) |
When we stratified for race (white, black, Hispanic, or other), similar results across the three exposures of education level, employment status, and annual household income were obtained in all four categories of race.
We assessed our three socioeconomic indicators (employment status, annual household income, and education level) for interactions. Interactions between education level and employment status as well as education level and income were not observed. An interaction between employment status and reported annual household income was observed, with women reporting a decreasing annual household income and not being in the labor force more likely to report past hysterectomy.
DISCUSSION
Socioeconomic indicators of annual household income and education level are associated with hysterectomy status in United States women. We found that women with less than a high school education have the highest odds of having a hysterectomy compared to other socio-economic indicators.
One possible explanation for these findings is that women of lower socioeconomic status present for medical care later in the disease process and may not be candidates for non-surgical management. Another explanation is women of lower socioeconomic status are less likely to be offered conservative treatments. Hysterectomy is a common and definitive surgical treatment for abnormal uterine bleeding and symptomatic uterine leiomyomas. However, many women wish to retain their uteri even after completion of child-bearing. In addition, some women may desire hysterectomy as a definitive method of birth control. The reasons why some women choose hysterectomy over uterine preservation are poorly understood.
In an analysis of hysterectomies performed in the United States in 2003, the majority are preformed for benign indications( 89%, n/N 538,722/602,457) with cancer being the indication in a minority of procedures (11%, n/N= 63,735/602,457).2 Among hysterectomies performed for benign disease, symptomatic leiomyomas (33%) and menstrual disorders (17%) were the most common indications.2 After failure of medical management for abnormal uterine bleeding and symptomatic leiomyomas, two minimally invasive alternatives to hysterectomy for benign disease are endometrial ablation (EA) and uterine artery embolization (UAE).13 Many of the earlier techniques of EA required hysteroscopic guidance. The development of newer energy modalities and delivery mechanisms have generated renewed interest and an increased use of EA techniques since the 1997 FDA approval of the first non-hysteroscopic endometrial ablation device.14 Unfortunately, some women still require hysterectomy after EA. In a cohort of women from the Kaiser Permanente Northern California insurance system, the probability of hysterectomy at 8 years after EA was 26%.15 UAE is another alternative to hysterectomy for symptomatic uterine leiomyomas treating heavy menstrual bleeding, inter-menstrual pelvic pain, and bulk related symptoms.16 The FIBROID registry has reported 3 year follow up after UAE with a Kaplan-Meier estimate of subsequent hysterectomy at 3 years of 9.79%.17 Although both of these minimally invasive techniques may be appropriate for certain women, there are also women who will elect to defer these options for the definitive surgical procedure of hysterectomy. Reasons for these choices among different women are an area for future study.
Previous studies have examined the association of single indicators of socioeconomic status and hysterectomy. When the single indicator of education was used as a representation of socioeconomic status, higher rates of hysterectomy were observed in black women with lower education levels compared with higher educated counterparts.8 Similarly, we also found that women with lower education levels had increased odds of hysterectomy.
In a previous review by Kjerulff et al. of the 1988 BRFSS dataset evaluating socioeconomic correlates of hysterectomy, only annual household income and education level were examined.18 In the 1988 survey, hysterectomy status was only asked in fifteen states with a total sample of 12,465 women; however similar associations of education level and income were observed. Our study explored employment status as an additional socioeconomic indicator to obtain a better reflection of actual socioeconomic status.
Our study has many strengths. The BRFSS is a large telephone survey that seeks to capture all individuals in the United States, not just individuals who actively seek or have access to healthcare services. The BRFSS also provides information on a large cross-section of women across the United States and its territories. Another advantage of examining the BRFSS database is the comprehensive information collected on three indicators of socioeconomic status commonly used in the United States, namely: education, income, and employment.
Many studies noting declining hysterectomy rates have not had complete information on race, and fewer have had socioeconomic indicators to include in their analysis. Keshavarz et al. reported the association between race and hysterectomy rate, but was missing racial/ethnicity data on 20% of their study population.1 Farquhar et al. did not report any racial/ethnicity data because of extensive amounts of missing data.5 We were able to categorize over 94% of our study population through self reported categories of white, black or Hispanic. Consistent with others, we did find black women more likely to have undergone hysterectomy than white women. Interestingly, we found Hispanic women less likely to report past hysterectomy than white women.
Our study has several limitations. Because the BRFSS is a cross-sectional survey, causality of socioeconomic status and hysterectomy cannot be determined. The woman's socioeconomic status at the time of the survey is known, but the socioeconomic status at the time of hysterectomy is unknown. However, our study was able to capture three separate indicators of socioeconomic status in the women studied. This study was also limited by the restrictions of a secondary database; data on indications for hysterectomy, route of hysterectomy, and conservative treatment offered prior to hysterectomy are not available. For example, the number of women undergoing hysterectomy for the indication of uterine leiomyomas is unknown. Other datasets, such as the Nationwide Inpatient Sample, have reported on indications for hysterectomy. Previous investigators have found indications for hysterectomy vary by race. Leiomyomas are the primary indication for hysterectomy in 70% of African americian women, but only 33% of white women in the United States in 2003.2 However, these datasets are not able to provide as much information on socioeconomic status.
In conclusion, hysterectomy is a surgical procedure with many valid indications. However, we found differences exist in education level and current annual household income among women in the United States who have had hysterectomy.
Acknowledgments
Supported by grant T32 HD0406740-04; Women and Infants Hospital/Brown Epidemiology/Clinical Trials; DHHS & grant 5-K12-HD050108-02; WIH/Brown Women’s Reproductive Health Research Career Development Award; National Institute of Child Health and Human Development.
Footnotes
Presented at the 56th Annual Clinical Meeting of the American College of Obstetrics and Gynecology in New Orleans, LA May 3rd to 7th, 2008
References
- 1.Keshavarz H, Hillis SD, Kieke BA, Marchbanks PA. Hysterectomy surveillance—United States. 1994–1999. Morbidity and Mortality World Report Center for Disease Control Surveillance Summary. 2002;51(SS-5):1–8. [Google Scholar]
- 2.Wu JM, Wechter ME, Geller EJ, Nguyen TV, Visco AG. Hysterectomy Rates in the United States, 2003. Obstetrics and Gynecology. 2007;110:1091–1095. doi: 10.1097/01.AOG.0000285997.38553.4b. [DOI] [PubMed] [Google Scholar]
- 3.Powell LH, Meyer P, Weiss G, Matthews KA, Santoro N, Randolph JF, Schocken M, Skurnick J, Ory MG, Sutton-Tyrrell K. Ethnic differences in past hysterectomies for benign conditions. Women’s Health Issues. 2005;15:179–186. doi: 10.1016/j.whi.2005.05.002. [DOI] [PubMed] [Google Scholar]
- 4.Hillis SD, Koonin LM, Morrow B, Kieke BA. Hysterectomy surveillance—United States. 1980–1993. Morbidity and Mortality World Report Center for Disease Control Surveillance Summary. 1997;46(SS-4):1–15. [PubMed] [Google Scholar]
- 5.Farquhar CM, Steiner CA. Hysterectomy rates in the United States: 1990–1997. Obstetrics and Gynecology. 2002;99:229–234. doi: 10.1016/s0029-7844(01)01723-9. [DOI] [PubMed] [Google Scholar]
- 6.Jacobson GF, Shaber RE, Armstrong MA, Hung YY. Hysterectomy rates for benign indications. Obstetrics and Gynecology. 2006;107:1278–1283. doi: 10.1097/01.AOG.0000210640.86628.ff. [DOI] [PubMed] [Google Scholar]
- 7.Weber AM, Lee JC. Use of alternative techniques of hysterectomy in Ohio, 1988–1994. The New England Journal of Medicine. 1996;335:483–489. doi: 10.1056/NEJM199608153350706. [DOI] [PubMed] [Google Scholar]
- 8.Hakim RB, Benedict B, Merrick NJ. Quality of Care for Women Undergoing a Hysterectomy: Effects of Insurance and Race/Ethnicity. American Journal of Public Health. 2004;98:1399–1405. doi: 10.2105/ajph.94.8.1399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Weaver F, Hynes D, Goldberg JM, Khuri S, Daley J, Henderson W. Hysterectomy in Veterans Affairs Medical Centers. Obstetrics and Gynecology. 2001;97:880–884. doi: 10.1016/s0029-7844(01)01350-3. [DOI] [PubMed] [Google Scholar]
- 10.Palmer JR, Rao RS, Adams-Campbell LL, Rosenberg L. Correlates of hysterectomy among African-American women. American Journal of Epidemiology. 1999;150:1309–1315. doi: 10.1093/oxfordjournals.aje.a009962. [DOI] [PubMed] [Google Scholar]
- 11.Center for Disease Control. Behavioral Risk Factors Surveillance Survey (BRFSS) database 2004. [Accessed February 2, 2007];2004 http://www.cdc.gov/brfss/technical_infodata/surveydata/2004.htm. [Google Scholar]
- 12.Center for Disease Control. Behavioral Risk Factor Surveillance System Operational and User’s guide. [Accessed December 27, 2007];Version 3.0. 2004 http://ftp.cdc.gov/pub/Data/Brfss/userguide.pdf. [Google Scholar]
- 13.ACOG Practice Bulletin. Alternatives to Hysterectomy in the Management of Leiomyomas. Clinical Management Guidelines for Obstetrician-Gynecologists. 2008;(No. 96) [Google Scholar]
- 14.ACOG Practice Bulletin. Endometrial Ablation. Clinical Management Guidelines for Obstetrician-Gynecologists. 2007;(No 81) [Google Scholar]
- 15.Longinotti MK, Jacobson GF, Hung YY, Learman LA. Probability of Hysterectomy After Endometrial Ablation. Obstetrics and Gynecology. 2008;112(6):1214–1220. doi: 10.1097/AOG.0b013e31818c1766. [DOI] [PubMed] [Google Scholar]
- 16.Spies JB, Myers ER, Worthington-Kirsh R, Mulgund J, Goodwing S, Mauro M. The FIBROID registry. Obstetrics and Gynecology. 2005;106(6):1309–1318. doi: 10.1097/01.AOG.0000188386.53878.49. [DOI] [PubMed] [Google Scholar]
- 17.Goodwin SC, Spies JB, Worthing-Kirsch R, Peterson E, Pron G, Li S, Myers ER. Uterine Artery Embolization for Treatment of Leiomyomata. Long-term outcomes from the FIBROID Registry. Obstetrics and Gynecology. 2008;111(1):22–33. doi: 10.1097/01.AOG.0000296526.71749.c9. [DOI] [PubMed] [Google Scholar]
- 18.Kjerulff K, Langenberg P, Guzinski G. The socioeconomic correlates of hysterectomies in the United States. American Journal of Public Health. 1993;83:106–108. doi: 10.2105/ajph.83.1.106. [DOI] [PMC free article] [PubMed] [Google Scholar]