Abstract
This study examined the associations among chronic health conditions, sociodemographic factors, and depressive symptomatology in older married couples. Data from the 2004 wave of the Health and Retirement Study (n = 2,184 couples) were analyzed. Results indicated a reciprocal relationship in depressive symptoms between spouses. Additionally, post hoc analyses indicated that husbands’ stroke and high blood pressure were related to increased depressive symptomatology among wives. Beyond the reciprocal relationship, husbands were unaffected by wives’ health. These results suggest sex differences underlying psychological distress in the context of physical health among older adults and that older women with husbands who have high levels of depressive symptomatology, high blood pressure, or a history of stroke may be at particular risk of experiencing depressive symptoms.
Keywords: Chronic illness, Depression, Dyadic, Spouses
SOCIAL contexts, including marital relationships, are important in the development of depressive symptoms. Although being married is typically a protective factor against the development of depressive symptoms (Blazer, Hughes, & George, 1987), it is in this same context that having a spouse with depressive symptoms increases the risk of depression for the partner (Townsend, Miller, & Guo, 2001). The present study examined the relationships among individual and spousal health-related characteristics and depressive symptomatology in older married couples.
A social contextual model of depression
The importance of the shared environment is emphasized in the social contextual model of depression for people in close relationships. By focusing on interactions, this model describes the process and patterns of change experienced by one individual (e.g., diagnosis of chronic illness or increased depressive symptomatology) that might lead to changes in his or her partner (Hays et al., 1997; Siegel, Bradley, Gallo, & Kasl, 2004; Tower & Kasl, 1996). The advantage of the social contextual model of depression is that it accounts for the transactional and interdependent nature of social relationships (Hammen, 1999; Holahan, Moos, & Bonin, 1999) and suggests that individual characteristics and the characteristics of the social context are important to consider.
Marriage is one important social context to consider when examining the interpersonal nature of depression (Peek, Stimpson, Townsend, & Markides, 2006; Siegel et al., 2004; Townsend et al., 2001). This is especially true in older adulthood as environmental and health-related stressors accumulate and spouses become the most important source of support (Cutrona, 1996; Fiske, 2006). Support for a social contextual model of depression among married couples includes findings that living with a depressed spouse led to increased reports of burdens and psychological distress (Coyne, Kessler, Tal, Wortman, & Greden, 1987). In addition, cross-sectional and longitudinal research suggests a reciprocal relationship between the depressive symptomatology of married partners (Bookwala & Schulz, 1996; Tower & Kasl, 1996). Consistent with a social contextual model of depression, our study examined the relationship between spouses’ depressive symptomatology in the context of chronic health conditions.
Physical health and depression
We focused on lung diseases, diabetes, chronic heart conditions, stroke, high blood pressure, cancer, and arthritis, which are associated with depressive symptomatology (Blazer, 2003; Isik, Koca, Ozturk, & Mermi, 2007; Kunik et al., 2005; Spiegel & Giese-Davis, 2003; Whyte, Mulsant, Vanderbilt, Dodge, & Ganguli, 2004; Yang & Jones, 2008). Much of the research examining physical health and depression focuses on general depressive symptomatology and does not account for the multidimensional nature of depression, which can lead to an overestimation or underestimation of depressive symptoms in people with chronic illnesses (Kalichman, Rompa, & Cage, 2000). Our study accounts for this multidimensionality by modeling relationships among chronic health conditions and three dimensions of the Health and Retirement Study (HRS) nine-item Center for Epidemiological Studies–Depression (CES-D) scale (Yang & Jones, 2008): lack of positive affect, dysphoria (presence of depressed affect, e.g., feeling lonely), and somatic (symptoms related to lack of energy and sleep). These dimensions are consistent with the findings by Radloff (1977) and Blazer, Landerman, Hays, Simonsick, and Saunders (1998).
There is a rapidly emerging literature exploring the relationship between health and depression in the context of marriage and how spouses interact and cope when facing health-related stressors (see Berg & Upchurch, 2007, for review). Among older adults, a decline in spousal health was related to an increase in depressive symptoms reported by the partner (Siegel et al., 2004). Tower and Kasl (1996) reported a reciprocal association of depressive symptomatology within older couples and a positive association between husbands’ number of chronic illnesses and the level of depression experienced by their wives. Bookwala and Schulz (1996) found that spouses’ ratings of subjective well-being were significantly associated with one another. Furthermore, husbands’ reported number of medications was associated with increased depression among wives. This research suggests that spousal health is related to depressive symptomatology and mental well-being.
Our study expanded upon this existing literature in two ways. First, much of the previous research analyzed husband and wife data separately or focused primarily on patient characteristics and outcomes and not the spouse. In order to capitalize on and account for the dependency that is inherent in data collected from couples, we used a dyadic analysis approach. This approach provides a method to simultaneously examine how a person’s own health and the health of his or her spouse is related to depressive symptomatology (Kenny, Kashy, & Cook, 2006). Second, research investigating the relationship between health and depressive symptomatology in married couples has tended to focus on broad conceptualizations of health (e.g., number of chronic illnesses, self-rated health) and depressive symptomatology or has investigated a single chronic illness. In order to expand on this research, we examined how multiple chronic health conditions were related to general depressive symptoms and specific dimensions of depressive symptoms of individuals and spouses.
Sociodemographic factors
Age, education, and race and ethnicity are related to depressive symptomatology. Depressive symptomatology increases during older adulthood, perhaps due to a decline in physical health and the accumulation of other stressors (Fiske, 2006). A higher level of education is also related to lower depression (Townsend et al., 2001), likely due to the association between level of educational attainment and socioeconomic status (Blazer, Kessler, & McGonagle, 1994). Many studies suggest that minorities tend to report more depressive symptoms compared with Whites (Plant & Sachs-Ericsson, 2004). The observed race/ethnic differences might reflect disparities in the prevalence of chronic health conditions between Whites and members of minority groups (Stecker, Fortney, Steffick, & Prajapati, 2006).
Present study
Our study had two objectives. First, we addressed the tendency of previous research on couples living with chronic illnesses to examine a single chronic health condition or a general definition of health (e.g., number of chronic illnesses). We addressed this issue by considering the associations of multiple common chronic health conditions (and the accompanying functional limitations) with depressive symptomatology after accounting for race and ethnicity, education, and age. In addition, we expanded upon previous research by simultaneously considering both the general and subdimensions of depressive symptomatology.
Second, we examined how spousal characteristics were related to an individual’s depressive symptomatology using a dyadic analysis approach. These “partner effects” reflect the association between an individual’s characteristics and his or her partner’s outcomes after accounting for the relationship among one’s own characteristics and outcomes (Kenny et al., 2006). This objective addressed the need for additional research that accounts for the interdependent nature of data collected from married dyads.
To address these objectives, we used a structural equation modeling approach to analyzing dyadic data. This approach allowed for the simultaneous examination of how specific chronic health conditions, functional limitations, and sociodemographic information were related to general depressive symptomatology and specific dimensions of depressive symptoms in husbands and wives. Based on a social contextual model of depression and previous literature, we hypothesized that (a) specific health conditions and functional limitations would be related to increased general depressive symptomatology in husbands and wives; (b) Blacks and Hispanic/Latinos would have higher levels of general depressive symptomatology than Whites; and (c) there would be a significant reciprocal relationship between husbands’ and wives’ general depressive symptomatology. Support for these hypotheses is reflected by significant indirect paths in the model and significant paths between husbands’ and wives’ level of general depressive symptomatology.
We used a post hoc approach to model modification to examine a number of relationships involving indirect paths and cross-spouse relationships. Specifically, we examined how chronic health conditions were related to specific dimensions of depressive symptomatology and the relationships between spousal health conditions and depressive symptomatology.
METHODS
Data from the 2004 wave of the HRS were analyzed. The study began in 1992 to collect data on the health and wealth of adults approaching and moving through retirement. Data are collected every 2 years with a new cohort added every 6 years. The original sample included 12,654 individuals born between 1931 and 1941, with Blacks and Hispanics/Latinos being oversampled. In 1998, the HRS merged with the Assets and Health Dynamics of the Oldest Old (AHEAD) study, which used the HRS screening procedures to identify adults born during or before 1923. A multistage area probability sampling design was used to select households that included at least one age-eligible person. If a person was deemed to be age eligible, his or her spouse was enrolled in the study regardless of the age of the spouse.
Participants
The 2004 wave sampled 20,129 individuals, of which 13,291 reported being married. Of these, 353 did not have partner data available and 352 individuals reported a change in marital status since the previous time of measurement and were excluded, resulting in 6,293 couples who did not report a change in marital status and for whom data for each spouse was available. Additional exclusions included (a) either spouse was younger than 65 years (n = 2,670 couples where both spouses were younger than 65 years and n = 918 couples where one spouse was younger than 65 years); (b) either spouse reported a race other than non-Hispanic White, non-Hispanic Black, or Hispanic/Latino (n = 63 couples); (c) either spouse was unable to complete the questionnaires without a proxy (n = 435 couples); or (d) either spouse had missing data on any of the independent variables (n = 23 couples). The final sample included 4,368 married adults over the age of 65 years (n = 2,184 couples). Participant characteristics are presented in Table 1.
Table 1.
Sociodemographic Information by Gender
| Total |
Husbands |
Wives |
||||
| Variable | n (%) | M (SD) | n (%) | M (SD) | n (%) | M (SD) |
| Sociodemographic | ||||||
| Age | 74.16 (6.05) | 75.45 (6.21) | 72.87 (5.88) | |||
| Race and ethnicity | ||||||
| White | 3,727 (85.3) | 1,871 (85.7) | 1,856 (85.0) | |||
| Black | 366 (8.4) | 185 (8.5) | 181 (8.3) | |||
| Hispanic/Latino | 275 (6.3) | 128 (5.9) | 147 (6.7) | |||
| Education | ||||||
| No formal education | 20 (0.5) | 12 (0.5) | 8 (0.4) | |||
| Completed Grades 1–11 | 993 (22.7) | 562 (25.7) | 431 (19.8) | |||
| High school graduate | 1,612 (36.9) | 692 (31.7) | 920 (42.1) | |||
| Completed some college | 8,29 (19.0) | 363 (16.6) | 466 (21.3) | |||
| College graduate | 455 (10.4) | 260 (11.9) | 195 (8.9) | |||
| Post-college | 459 (10.5) | 295 (13.6) | 164 (7.5) | |||
| Physical health | ||||||
| Functional limitations | 2.46 (2.46) | 2.15 (2.36) | 2.76 (2.55) | |||
| High blood pressure | 2,612 (59.1) | 1,280 (57.9) | 1,332 (60.2) | |||
| Heart conditions | 1,372 (31.0) | 860 (38.9) | 512 (23.2) | |||
| Stroke | 359 (8.1) | 217 (9.8) | 142 (6.4) | |||
| Diabetes | 855 (19.3) | 479 (21.7) | 376 (17.0) | |||
| Lung diseases | 437 (9.9) | 226 (10.2) | 211 (9.5) | |||
Measures
Demographic information.—
We used data on age, years of education, and race/ethnicity. Respondents were asked if they consider themselves Hispanic or Latino, or primarily White or Caucasian, Black or African American, American Indian, Asian, or something else. The race and ethnicity variable was dummy coded with Whites as the reference group.
Depressive symptomatology.—
Depressive symptomatology was measured with a modified nine-item version of the CES-D (Radloff, 1977), which we refer as the HRS/CES-D. Participants answered yes or no to items assessing whether for much of the past week he or she felt (a) depressed, (b) everything was an effort, (c) sleep was restless, (d) happy, (e) lonely, (f) that he or she enjoyed life, (g) sad, (h) that he or she could not get going, and (i) that he or she had a lot of energy. The item assessing energy level was included in the HRS/CES-D and was not in the original CES-D. Factor analytic studies have identified three subscales for this measure: somatic (Items 2, 3, 8, and 9), lack of positive affect (Items 4 and 6), and dysphoria (Items 1, 5, and 7; Yang & Jones, 2008). Items 4, 6, and 9 were reversed scored; higher scores reflect less positive affect. These subscales correspond to the somatic, positive affect, and depressive factors of the CES-D that have been identified in community-dwelling older adult samples (e.g., Blazer et al., 1998). Overall, the measure displays acceptable internal consistency (α =.80–.83) for a brief measure (Steffick, Wallace, & Herzog, 2000).
Chronic health conditions.—
We evaluated if a doctor had ever told participants that they had any of the following illnesses: high blood pressure or hypertension, any heart conditions (including heart attacks, angina, congestive heart failure, or coronary heart disease), a recent stroke (within 2 years for HRS respondents or any history for AHEAD respondents), diabetes, chronic lung disease (e.g., chronic bronchitis or emphysema), cancer (excluding skin cancer), or arthritis/rheumatism. If respondents reported “yes” to any of the items in the previous wave of data and “no” in the current wave, their response was coded as “no.”
Physical functioning ability.—
Physical functioning was assessed using 10 items asking if, due to a health problem, a person had any difficulty performing tasks in three domains: (a) mobility (e.g., walking), (b) strength (e.g., lifting 10 lbs), and (c) gross and fine motor skills (e.g., stooping/crouching/kneeling). Items were coded as 0 (no difficulty) or 1 (any difficulty) and summed to create a functional impairment index. Internal consistency for this measure has ranged from 0.81 to 0.87 (Fonda & Herzog, 2000).
Statistical Analyses
Statistical analyses were performed with Mplus version 4.1 (Muthén & Muthén, 1998–2006). Analyses were designed to examine relationships between health and depressive symptomatology and if these relationships were specific to any particular subset of depressive symptoms (i.e., somatic, dysphoric, lack of positive affect). To these ends, an multiple indicators–multiple causes (MIMIC) model approach was used. The MIMIC model is a specific case of structural equation modeling with multiple indicators for each latent variable (analogous to confirmatory factor analysis) and multiple exogenous covariates (Muthén & Muthén).
MIMIC modeling proceeded in two steps. First, a measurement model with a second-order factor structure was specified with items loading on three first-order factors of depressive symptomatology: somatic, lack of positive affect, and dysphoria. These three factors then loaded on a general depressive symptomatology factor. Based on previous research suggesting measurement invariance between males and females on depression measures (O’Rourke, 2005), the factor loadings and item thresholds were constrained to be equal across husbands and wives. The reciprocal pathways between husbands’ and wives’ general depressive symptomatology were also constrained to be equal. The intercepts of wives’ affective symptoms, dysphoric symptoms, and second-order general depressive symptoms were freely estimated to account for possible gender differences.
Second, the baseline structural model was estimated with only indirect relationships between one’s own background variables and level of general depressive symptomatology being estimated. These paths are referred to as “indirect effects” because they represent mediated pathways (through the second-order factor) between the covariates and the first-order factors. Then, using a forward stepwise procedure based on the modification indices, a final model that included significant partner effects and direct effects was fitted, where direct effects are regression paths leading from covariates directly to first-order factors.
MIMIC models were specified using the weighted least squares means and variance adjusted estimator (Muthén & Muthén, 1998–2006). Model fit was assessed with the root mean square error of approximation (RMSEA; Kline, 2005) and the comparative fit index (CFI; Browne & Cudeck, 1993). The RMSEA provides a measure of discrepancy per model degree of freedom and approaches zero as model fit improves. RMSEA values close to 0.06 or less indicate adequate model fit (Hu & Bentler, 1998). The CFI ranges between 0 and 1; values greater than 0.95 generally indicate adequate model fit (Bentler, 1990). The chi-square goodness-of-fit index is reported although the sensitivity of this statistic in analyses with large sample sizes the significant value is not necessarily a reason to reject the specified model (Kline, 2005). To test if the model modifications improved model fit, the Mplus DIFFTEST function was used to calculate the corrected chi-square difference value (Muthén & Muthén).
Our analyses do not make use of the sampling weights because the HRS sampling unit was older individuals and our analyses focused on spouse pairs.
RESULTS
Table 2 presents unstandardized and standardized measurement slopes and path coefficients for the baseline model and final model. Only significant indirect and direct effects between the characteristics of one spouse influencing the other spouse’s depressive symptoms are presented in Table 2. The baseline model constrained partner effects and direct effects to zero, resulting in a model that fit by some indices and not others, χ2(261) = 573.13, p < .001, RMSEA = 0.03, CFI = 0.95.
Table 2.
Multiple Indicators–Multiple Causes Model of Self- and Spousal Influences on Depressive Symptomatology
| Baseline model |
Final model |
|||||||
| Husband |
Wife |
Husband |
Wife |
|||||
| Unstandardized (SE) | Standardized | Unstandardized (SE) | Standardized | Unstandardized (SE) | Standardized | Unstandardized (SE) | Standardized | |
| Measurement slopes | ||||||||
| Somatic | ||||||||
| Could not get going | 0.43 (0.03) | 0.78a,* | 0.43 (0.03) | 0.78a.* | 0.48 (0.02) | 0.86a,* | 0.48 (0.02) | 0.85a,* |
| Full of energy (r) | 0.35 (0.02) | 0.64a,* | 0.35 (0.02) | 0.64a,* | 0.39 (0.02) | 0.71a,* | 0.39 (0.02) | 0.70a,* |
| Everything an effort | 0.49 (0.03) | 0.90a,* | 0.49 (0.03) | 0.90a,* | 0.54 (0.03) | 0.98a,* | 0.54 (0.03) | 0.97a,* |
| Restless sleep | 0.33 (0.02) | 0.60a,* | 0.33 (0.02) | 0.60a,* | 0.36 (0.02) | 0.65a,* | 0.36 (0.02) | 0.64a,* |
| Lack of positive affect | ||||||||
| Was happy (r) | 0.45 (0.04) | 0.94a,* | 0.45 (0.04) | 0.94a,* | 0.44 (0.04) | 0.98a,* | 0.44 (0.04) | 0.99a,* |
| Enjoyed life (r) | 0.45 (0.03) | 0.94a,* | 0.45 (0.03) | 0.94a,* | 0.43 (0.04) | 0.96a,* | 0.43 (0.04) | 0.98a,* |
| Dysphoric | ||||||||
| Felt depressed | 0.30 (0.03) | 0.94a,* | 0.30 (0.03) | 0.94a,* | 0.28 (0.05) | 0.99a,* | 0.31 (0.05) | 0.91a,* |
| Felt lonely | 0.26 (0.03) | 0.78a,* | 0.26 (0.03) | 0.78a,* | 0.23 (0.05) | 0.82a,* | 0.25 (0.04) | 0.77a,* |
| Felt sad | 0.35 (0.04) | 0.95a,* | 0.35 (0.04) | 0.95a,* | 0.27 (0.05) | 0.96a,* | 0.30 (0.05) | 0.89a,* |
| General depression | ||||||||
| Somatic | 1.22 (0.12) | 0.83b,* | 1.22 (0.12) | 0.83b,* | 1.02 (0.07) | 0.67b,* | 1.02 (0.07) | 0.68b,* |
| Lack of positive affect | 1.69 (0.15) | 0.90b,* | 1.69 (0.15) | 0.90b,* | 1.76 (0.19) | 0.91b,* | 1.76 (0.19) | 0.92b,* |
| Dysphoric | 2.13 (0.15) | 0.94b,* | 2.13 (0.15) | 0.94b,* | 2.90 (0.63) | 0.97b,* | 2.90 (0.62) | 0.96b,* |
| Latent variable intercept/mean | ||||||||
| Somatic | 0.00 (0.00) | 0.00 | 0.00 (0.00) | 0.00 | 0.00 (0.00) | 0.00 | 0.00 (0.00) | 0.00 |
| Lack of positive affect | 0.00 (0.00) | 0.00 | 1.01 (1.84) | 0.43 | 0.00 (0.00) | 0.00 | 1.19 (1.97) | 0.52 |
| Dysphoric | 0.00 (0.00) | 0.00 | −0.96 (1.85) | −0.34 | 0.00 (0.00) | 0.00 | −1.07 (2.61) | −0.30 |
| General depression | 0.00 (0.00) | 0.00 | 0.56 (0.92) | 0.45 | 0.00 (0.00) | 0.00 | 0.50 (1.00) | 0.42 |
| Regression coefficients | ||||||||
| General depression | ||||||||
| Husband’s characteristics | ||||||||
| High BP | 0.02 (0.07) | 0.01a | −0.02 (0.08) | −0.02a | ||||
| Lung diseases | 0.48 (0.11) | 0.38a,* | 0.48 (0.10) | 0.40a,* | ||||
| Diabetes | 0.09 (0.08) | 0.07a | −0.02 (0.11) | −0.01a | ||||
| Heart condition | 0.15 (0.07) | 0.12a,* | 0.04 (0.08) | 0.04a | ||||
| Stroke | 0.23 (0.11) | 0.18a,* | 0.29 (0.12) | 0.24a,* | 0.24 (0.10) | 0.20a,* | ||
| Cancer | 0.18 (0.08) | 0.14a,* | 0.17 (0.08) | 0.15a,* | ||||
| Arthritis | 0.09 (0.08) | 0.03a | −0.01 (0.09) | −0.01a | ||||
| Functional limitations | 0.41 (0.03) | 0.41b,* | 0.30 (0.04) | 0.25b,* | ||||
| Education | −0.03 (0.03) | −0.04b | −0.06 (0.03) | −0.05b,* | ||||
| Age | 0.01 (0.01) | 0.05b | 0.01 (0.01) | 0.01b | ||||
| Black | 0.24 (0.12) | 0.19a | 0.23 (0.12) | 0.19a | ||||
| Latino | 0.54 (0.15) | 0.43a,* | 0.51 (0.15) | 0.44a,* | ||||
| General depression | 0.18 (0.02) | 0.18b,* | 0.19(0.02)b,* | 0.19b,* | ||||
| Wife’s characteristics | ||||||||
| High BP | 0.04 (0.07) | 0.03a | 0.04 (0.07) | 0.03a | ||||
| Lung diseases | 0.47 (0.11) | 0.38a,* | 0.46 (0.11) | 0.39a,* | ||||
| Diabetes | −0.03 (0.09) | −0.03a | −0.03 (0.09) | −0.01a | ||||
| Heart condition | 0.24 (0.08) | 0.19a,* | 0.24 (0.08) | 0.20a,* | ||||
| Stroke | 0.33 (0.13) | 0.27a,* | 0.33 (0.13) | 0.28a,* | ||||
| Cancer | 0.08 (0.08) | 0.06a | 0.08 (0.09) | 0.07a | ||||
| Arthritis | 0.05 (0.08) | 0.04a | 0.05 (0.08) | 0.04a | ||||
| Functional limitations | 0.35 (0.03) | 0.36b,* | 0.22 (0.03) | 0.23b,* | ||||
| Education | −0.11 (0.04) | −0.10b,* | −0.14 (0.04) | −0.14b,* | ||||
| Age | 0.01 (0.01) | 0.03b | 0.02 (0.01) | 0.08b | ||||
| Black | 0.21 (0.12) | 0.05a | 0.22 (0.12) | 0.18a | ||||
| Latino | 0.33 (0.15) | 0.06a,* | 0.51 (0.15) | 0.43a,* | ||||
| General depression | 0.18 (0.02) | 0.18b,* | 0.19 (0.02) | 0.19b,* | ||||
| Somatic | ||||||||
| Husband’s characteristics | ||||||||
| High BP | 0.26 (0.10) | 0.15a,* | ||||||
| Diabetes | 0.31 (0.12) | 0.17a,* | ||||||
| Heart condition | 0.33 (0.11) | 0.18a,* | ||||||
| Arthritis | 0.28 (0.11) | 0.16a,* | ||||||
| Functional limitations | 0.34 (0.05) | 0.24b,* | ||||||
| Wife’s characteristics | ||||||||
| Functional limitations | 0.42 (0.05) | 0.30b,* | ||||||
| Latino | −0.67 (0.19) | −0.37a,* | ||||||
| Lack of positive affect | ||||||||
| Husband’s characteristics | ||||||||
| Education | 0.23 (0.09) | 0.14b,* | ||||||
| Wife’s characteristics | ||||||||
| Age | −0.09 (0.03) | −0.16b,* | ||||||
| Education | 0.27 (0.09) | 0.13b,* | ||||||
| Dysphoric | ||||||||
| Husband’s characteristics | ||||||||
| Stroke | −1.22 (0.48) | −0.34a,* | ||||||
| Wife’s characteristics | ||||||||
| None | ||||||||
| Residual variance | ||||||||
| Somatic | 1.00 (0.00) | 0.25 | 1.00 (0.00) | 0.24 | 1.00 (0.00) | 0.31 | 1.00 (0.00) | 0.30 |
| Lack of positive affect | 1.00 (0.00) | 0.20 | 1.00 (0.00) | 0.20 | 1.00 (0.00) | 0.19 | 1.00 (0.00) | 0.19 |
| Dysphoric | 1.00 (0.00) | 0.18 | 1.00 (0.00) | 0.17 | 1.00 (0.00) | 0.08 | 1.00 (0.00) | 0.08 |
| General depression | 1.00 (0.00) | 0.64 | 1.00 (0.00) | 0.63 | 1.00 (0.00) | 0.70 | 1.00 (0.00) | 0.71 |
| Model fit | ||||||||
| χ2 (p value) | 573.13* | 431.53* | ||||||
| Degrees of freedom | 261 | 258 | ||||||
| CFI | 0.95 | 0.97 | ||||||
| RMSEA | 0.03 | 0.02 | ||||||
Notes: BP = blood pressure; CFI = comparative fit index; RMSEA = root mean square error of approximation.
Parameters are standardized with respect to the mean and variance of the dependent variable. The notation (r) indicates the response variable was reverse scored.
Parameters are fully standardized with respect to the means and variances of the independent and dependent variables.
*p < .05.
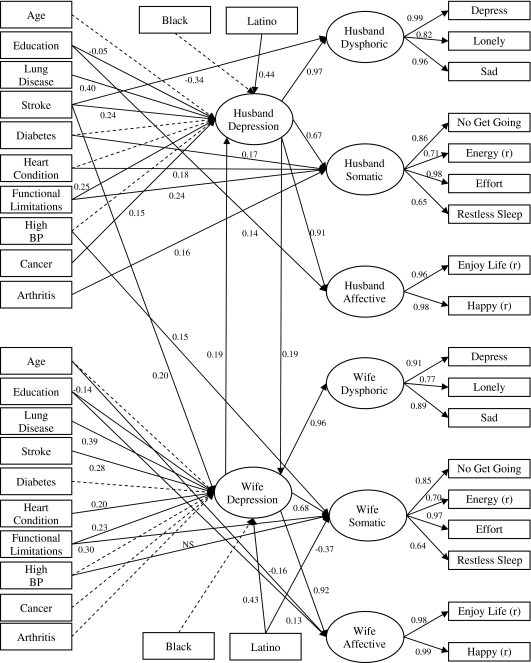
The final model included direct effects to the first-order factors and partner effects that were suggested by post hoc modification indices. These parameters were freed in a forward stepwise progression from the largest chi-square scaled modification indices value to the smallest value that, when the parameter was freely estimated, still resulted in a significantly better fitting model. The final model fit the data well, χ2(258) = 431.53, p < .001, RMSEA = 0.02, CFI = 0.97 (see Figure 1).
Figure 1.
Multiple indicators–multiple causes model using latent constructs. Dashed lines were estimated but were not significant. NS indicates a non-significant path that was estimated to control for actor effect; (r) indicates that item was reverse scored. BP = blood pressure.
There were a number of direct and indirect effects of the exogenous variables for husbands and wives. For husbands, the indirect paths from lung diseases, stroke, cancer, and functional limitations were positive and significant, whereas education was negatively and significantly related to general depressive symptomatology. The mean level of depressive symptomatology was higher for Hispanic/Latino husbands compared with White husbands. In terms of direct effects, husbands who reported having diabetes, heart conditions, arthritis, or functional limitations reported higher mean levels of somatic symptoms relative to dysphoric or affective symptoms while holding constant the level of general depressive symptomatology and the effects of other variables in the model. There was also a positive direct effect of stroke on dysphoric symptoms. Finally, the association between education and affective symptoms was lower than expected given the relationship between education and general depressive symptoms.
Among wives, the following five characteristics and health conditions were positively associated with general depressive symptoms: stroke, lung diseases, heart condition, functional limitations, and Hispanic/Latina ethnicity. Education was negatively related to general depressive symptoms. With regard to direct paths, reported functional limitations were positively related to somatic symptoms, whereas level of education and age were positively related to affective symptoms. There was also a negative direct effect of being Hispanic/Latina on somatic symptoms, which indicates that after controlling for the level of general depressive symptoms, Hispanic/Latina women reported fewer somatic symptoms than would be expected.
Consistent with a social contextual model of depression, there were partner effects even after controlling for the reciprocal pathways between husbands’ and wives’ levels of general depressive symptoms. If a husband reported suffering a stroke, his wife reported a higher level of general depressive symptoms. In addition, husbands’ high blood pressure was positively related to wives’ somatic symptoms. There were no partner effects from the wives’ characteristics to husbands’ depressive symptoms. In addition to these partner effects, we used the MODEL INDIRECT procedure in Mplus (Muthén & Muthén, 1998–2006) to determine if one’s own level of depressive symptomatology mediated the pathway from chronic illness to spousal depressive symptoms. Results indicated that husband lung diseases (indirect effect = 0.09, SE = 0.02), husband stroke (indirect effect = 0.06, SE = 0.02), husband functional limitations (total indirect effect = 0.06, SE = 0.01), and husband cancer (total indirect effect = 0.03, SE = 0.01) were indirectly related to wives’ general depressive symptoms through husbands’ general depressive symptoms. Wives’ lung diseases, stroke, heart conditions, and functional limitations were indirectly related to husbands’ general depressive symptoms (total indirect effects = 0.06 [SE = 0.02], 0.05 [SE = 0.02], 0.03 [SE = 0.01], and 0.04 [SE = 0.01], respectively). Although statistically significant, the total indirect effects are relatively small and may not necessarily be clinically significant.
DISCUSSION
The objectives of this study were to examine the pattern of relationships among chronic health conditions (and accompanying functional limitations), sociodemographic factors, and depressive symptomatology in older married couples and to determine if partner characteristics were related to one’s level of depressive symptoms. Results indicated a complex pattern of relationships among chronic health conditions, functional limitations, and depressive symptomatology for husbands and wives. Results also indicated that chronic illness was related to spousal depressive symptomatology, but these associations were only present between husbands’ chronic health conditions and wives’ depressive symptoms. The findings from this study not only confirm Tower and Kasl’s (1996) conclusions that there is a positive association between husbands’ number of chronic illnesses and the level of depressive symptomatology experienced by their wives but also extend their study by examining specific chronic health conditions among husbands that are related to specific dimensions of depressive symptoms among wives.
For husbands, lung diseases, cancer, stroke, and functional limitations were positively related to general depressive symptomatology. Additionally, diabetes, heart conditions, arthritis, and functional limitations were positively related to somatic symptoms for husbands after controlling for general depressive symptoms levels. These relationships are consistent with notions of measurement noninvariance or differential item functioning in the psychometric literature. But rather than indicating bias, these results may be an expected consequence of specific illnesses that limit a person’s energy. Alternatively, being diagnosed with a heart condition, stroke, or diabetes might alter a person’s perception of his or her functional ability, which is related to an increase in somatic symptoms (Huprich, Porcerelli, Binienda, & Karana, 2005). This overlap in symptoms makes it particularly difficult to diagnose depressive symptoms for groups of people who have illnesses that include somatic symptoms and may lead to overestimation of depressive symptoms in people who have chronic illnesses (Kalichman et al., 2000). Stroke was directly and negatively related to dysphoric symptoms, suggesting that the relationship between stroke and dysphoric symptoms was less strong than the relationship between stroke and latent general depressive symptoms implies.
Hispanic/Latino husbands and wives reported a greater level of general depressive symptoms than Whites. Other studies using diverse samples (e.g., National Comorbidity Survey and Epidemiologic Catchment Area Study) have reported similar results, with Hispanics/Latinos having higher prevalence rates of depression than Whites (Kessler et al., 1994). Possible reasons for this increased prevalence in Hispanic/Latinos include a greater number of health problems compared with non-Hispanic Whites (Federal Interagency Forum on Aging-related Statistics, 2004), a tendency to have lower expectations for aging than non-Hispanic Whites, acculturation (Escobar, Nervi, & Gara, 2000), and the cumulative effects of discrimination (Alderte, Vega, Kolody, & Aguilar-Gaxiola, 1999).
For wives, lung diseases, heart condition, stroke, and functional limitations were related to increased general depressive symptomatology. Research suggests that heart conditions and stroke are related to depressive symptomatology (Siegel et al., 2004; Whyte et al., 2004), but it is unclear why these relationships were only significant for women in our study. One possibility is that for men, the variance in general depressive symptoms attributable to heart conditions and stroke was accounted for by functional limitations. In addition, self-report of heart disease and/or stroke may be associated with a fair degree of measurement error, thus making it less likely those relationships involving this variable will be found significant.
After controlling for general depressive symptoms, Hispanic/Latina wives reported lower levels of somatic complaints. This is interesting in light of previous observations that Hispanics/Latinos typically present with somatic symptoms as opposed to affective symptoms (Guarnaccia, Canino, Rubio-Stipec, & Bravo, 1993). Our findings do not support this view. We found that Hispanic/Latina wives were less likely to report the somatic symptoms captured by the HRS/CES-D after controlling for underlying level of general depression and other covariates in the model. We note that there is great heterogeneity in the Hispanic population (Yang, Carzola-Lancaster, & Jones, 2008) and inferences regarding a nonspecific Hispanic group are not warranted.
Among wives, there was a negative relationship between age and affective symptoms, suggesting that older women reported fewer affective symptoms. This finding is consistent with research suggesting that age is associated with an increased focus on the emotional quality of their lives (Kennedy, Fung, & Carstensen, 2001) and that increasing age is related to the experience of positive affect (Carstensen, Pasupathi, Mayr, & Nesselroade, 2000).
For husbands and wives, education was negatively related to general depressive symptoms, which might be due to its relationship with future income and life satisfaction (Blazer et al., 1994). After controlling for general depressive symptoms, the direct path from education to affective symptoms was also significant. This does not imply that education leads to less happiness. Instead, this finding suggests that affective symptoms were less strongly related to level of education than were the other symptoms of depression.
With regard to the partner effects, women’s somatic symptoms were positively related to husbands’ high blood pressure and wives had higher levels of general depressive symptoms if their husbands had experienced a stroke. These partner effects might be due to caregiving strain (Revenson & Majerovitz, 1990). In some cases, spousal distress may actually exceed the distress of the patient (Baider, Perez, & De-Nour, 1989), which appears to be the case in this study as there is not a relationship between high blood pressure or stroke with depressive symptomatology for husbands. Unfortunately, the data could not adequately address the role of caregiving within married couples.
Implications
There are several implications for these findings. Primary care physicians should consider the potentially different patterns of relationships among chronic health conditions, functional limitations, sociodemographic factors, and depressive symptomatology in men and women. For example, it appears that women are at risk for experiencing depressive symptoms when diagnosed with a heart condition. Care providers should also be particularly aware of the increased likelihood of Latinos experiencing depressive symptomatology and screen patients accordingly. In addition, attention should be paid to the specific dimensions of depressive symptomatology that are associated with chronic health conditions. Not unexpectedly, somatic symptoms in particular seem to be the most related to specific chronic health conditions among older adults. This is important given that many of the chronic conditions in our model are not related to general depressive symptomatology but are related to somatic symptoms. Examining how individual and spousal health conditions are related to both general depressive symptomatology and specific dimensions of depressive symptoms could be used to help primary care providers assess and identify subclinical depressive symptomatology among patients and spouses.
Health care professionals should also recognize that the spouses of men who have been diagnosed with high blood pressure or a stroke might be at a higher risk for experiencing depressive symptoms. This is important for two reasons. First, spousal mood and level of psychological distress are related to patient outcomes (Coyne & Smith, 1991). Second, depression is associated with mortality (Wulsin, Vaillant, & Wells, 1999). Thus, in the case where husbands are diagnosed with a chronic illness, it would behoove health professionals to attend to the mental health of the patient’s spouse. In addition, husbands and wives may share environmental or behavioral risk factors for poor cerebrovascular health (e.g., poor diet, lack of exercise) that may manifest clinically as stroke or high blood pressure at an earlier age among men but nevertheless signals increased risk for cardiovascular disease and possibly vascular depression among spouses.
Limitations and Future Directions
A number of limitations should be considered when interpreting these results. First, there were no data available that adequately addressed caregiving in this data set. Future research should explore the possible mediating role of caregiving burden in the relationships between a person’s own level of depressive symptoms and the health status of his or her spouse. Future research should also further explore how the quality of the marital relationship affects how spousal characteristics are related to an individual’s and his or her partner’s outcomes. Additionally, we did not consider the seriousness of the illness or if it was under control or being treated.
There were also limitations associated with the analyses. First, our analyses were cross sectional, which precludes any causal conclusions. Second, there is the potential for overfitting the model to the data, thus potentially limiting the generalizability of the findings. Third, as discussed previously, there may be important variables that are not included in our model. Fourth, the lack of positive affect factor had only two indicators, which could result in unreliable error estimates. Fifth, the partner effects and the direct paths in the model were based on post hoc modification indices, which run the risk of capitalizing on chance. Finally, we used a single group MIMIC model to explain the complex relationship between spousal and individual endorsement of general and specific dimensions of depressive symptoms based on differences in sociodemographic characteristics and chronic health conditions. However, there may be equivalent models that fit the data as well as our final model, such as the multiple group MIMIC model that allows for testing the significant differences between husbands and wives in their endorsement of depressive symptomatology based on sociodemographic characteristics and chronic health conditions.
There were also limitations related to the study sample. The HRS was a population-based study, designed to be broadly representative of adults living in the United States. We excluded sampling weights, but our results are at least representative of a national convenience sample of older married couples. A number of participants were dropped due to one of the spouses’ missing data. Although the estimator used in the analyses can handle missing data in the dependent variable under missing at random assumptions, missing data for predictor variables cannot be accounted for in these analyses. In addition, using a later wave of data collection could potentially introduce a selection bias due to attrition based on illness or death.
Finally, some of the associations found in our analyses were of relatively small magnitude. Additional work is needed to examine the clinical significance of the identified relationships, including the role of spousal health on depressive symptomatology.
Conclusions
Based on a social contextual model of depression, the current study expands the literature on the relationship among health conditions, functional limitations, sociodemographic factors, and depressive symptomatology by taking a dyadic approach to these associations in older adult married couples. Using a large national sample, our results indicated that chronic health conditions were related to general depressive symptomatology and specific dimensions of depressive symptoms, even while controlling for important sociodemographic variables, functional limitations, and the relationship between the levels of depressive symptoms of husbands and wives. Women were at higher risk of experiencing depressive symptoms if their husbands are diagnosed with certain chronic health conditions (stroke, high blood pressure). Thus, health care professionals need to be sensitive to the possibility that a patient’s spouse will also be affected when a patient is diagnosed with a chronic illness.
FUNDING
This research was made possible through the National Institutes of Health (NIH)/National Institute on Aging (NIA) 5-T35 AG026781, 5-T32 AG023480 award, NIH/NIA 5 R01 AG025308-02, NIH/NIA 5 R01 AG025308-02 Diversity Supplement, NIH/NIA P60AG008812, Harvard Medical School Livingston Fellowship, and the NARSAD Young Investigator Award.
References
- Alderte E, Vega WA, Kolody B, Aguilar-Gaxiola S. Depressive symptomatolgy: Prevalence and psychosocial risk factors among Mexican migrant farm workers in California. Journal of Community Psychology. 1999;27:457–471. [Google Scholar]
- Baider L, Perez T, De-Nour AK. Gender and adjustment to chronic disease: A study of couples with colon cancer. General Hospital Psychiatry. 1989;11:1–8. doi: 10.1016/0163-8343(89)90018-2. [DOI] [PubMed] [Google Scholar]
- Bentler PM. Comparative fit indexes in structural models. Psychological Bulletin. 1990;107:238–246. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- Berg CA, Upchurch R. A developmental-contextual model of couples coping with chronic illness across the adult life span. Psychological Bulletin. 2007;133:920–954. doi: 10.1037/0033-2909.133.6.920. [DOI] [PubMed] [Google Scholar]
- Blazer DG. Depression in late life: Review and commentary. Journal of Gerontology: Medical Sciences. 2003;58A:249–265. doi: 10.1093/gerona/58.3.m249. [DOI] [PubMed] [Google Scholar]
- Blazer DC, Hughes DC, George LK. The epidemiology of depression in an elderly community population. The Gerontologist. 1987;27:281–287. doi: 10.1093/geront/27.3.281. [DOI] [PubMed] [Google Scholar]
- Blazer DC, Kessler RC, McGonagle KA. The prevalence and distribution of major depression in a national community sample: The National Comorbidity Survey. American Journal of Psychiatry. 1994;11:979–986. doi: 10.1176/ajp.151.7.979. [DOI] [PubMed] [Google Scholar]
- Blazer DG, Landerman LR, Hays JC, Simonsick EM, Saunders WB. Symptoms of depression among community-dwelling elderly African American and White older adults. Psychological Medicine. 1998;28:1311–1320. doi: 10.1017/s0033291798007648. [DOI] [PubMed] [Google Scholar]
- Bookwala J, Schulz R. Spousal similarity in subjective well-being: The cardiovascular health study. Psychology and Aging. 1996;11:582–590. doi: 10.1037//0882-7974.11.4.582. [DOI] [PubMed] [Google Scholar]
- Browne M, Cudeck R. Alternative ways of assessing model fit. Thousand Oaks, CA: Sage; 1993. [Google Scholar]
- Carstensen LL, Pasupathi M, Mayr U, Nesselroade JR. Emotional experience in everyday life across the adult life span. Journal of Personality and Social Psychology. 2000;79:644–655. [PubMed] [Google Scholar]
- Coyne JC, Kessler RC, Tal MTJ, Wortman CB, Greden J. Living with a depressed person. Journal of Consulting and Clinical Psychology. 1987;55:347–352. doi: 10.1037//0022-006x.55.3.347. [DOI] [PubMed] [Google Scholar]
- Coyne JC, Smith DA. Couples coping with a myocardial infarction: A contextual perspective on wives’ distress. Journal of Personality and Social Psychology. 1991;61:404–412. doi: 10.1037//0022-3514.61.3.404. [DOI] [PubMed] [Google Scholar]
- Cutrona CE. Social support in couples: Marriage as a resource in times of stress. Thousand Oaks, CA: Sage; 1996. [Google Scholar]
- Escobar JI, Nervi CH, Gara MA. Immigration and mental health: Mexican Americans in the United States. Harvard Review of Psychiatry. 2000;8:64–72. [PubMed] [Google Scholar]
- Federal Interagency Forum on Aging-related Statistics. Older Americans 2004: Key indicators of well-being. Washington, DC: Government Printing Office; 2004. [Google Scholar]
- Fiske A. The nature of depression in later life. In: Qualls S, Knight B, editors. Psychotherapy for depression in older adults. Hoboken, NJ: John Wiley & Sons; 2006. pp. 29–44. [Google Scholar]
- Fonda S, Herzog AR. Documentation of physical functioning measured in the Health and Retirement Study and the Asset and Health Dynamics among the Oldest Old Study. Survey Research Center, University of Michigan; 2000. Retrieved January 8, 2008, from http://hrsonline.isr.umich.edu/docs/userg/dr-009.pdf. [Google Scholar]
- Guarnaccia PJ, Canino G, Rubio-Stipec M, Bravo M. The prevalence of ataques de nervios in the Puerto Rico disaster study. The role of culture in psychiatric epidemiology. Journal of Nervous and Mental Disorders. 1993;181:157–165. doi: 10.1097/00005053-199303000-00003. [DOI] [PubMed] [Google Scholar]
- Hammen C. The emergence of an interpersonal approach to depression. In: Joiner TE, Coyne JC, editors. The interactional nature of depression: Advances in interpersonal approaches. Washington, DC: American Psychological Association; 1999. pp. 21–35. [Google Scholar]
- Hays JC, Krishnan KRR, George LK, Pieper CF, Flint EP, Blazer DG. Psychosocial and physical correlates of chronic depression. Psychiatry Research. 1997;72:149–159. doi: 10.1016/s0165-1781(97)00105-4. [DOI] [PubMed] [Google Scholar]
- Holahan CJ, Moos RH, Bonin LA. Social context and depression: An integrative stress and coping framework. In: Joiner TE, Coyne JC, editors. The Interactional Nature of Depression: Advances in Interpersonal Approaches. Washington, DC: American Psychological Association; 1999. pp. 39–63. [Google Scholar]
- Hu LT, Bentler PM. Fit indices in covariance structure modeling: Sensitivity to underparameterized model misspecification. Psychological Methods. 1998;3:424–453. [Google Scholar]
- Huprich SK, Porcerelli J, Binienda J, Karana D. Functional health status and its relationship to depressive personality disorder, dysthymia, and major depression: Preliminary findings. Depression and Anxiety. 2005;22:168–176. doi: 10.1002/da.20116. [DOI] [PubMed] [Google Scholar]
- Isik A, Koca SS, Ozturk A, Mermi O. Anxiety and depression in patients with rheumatoid arthritis. Clinical Rheumatology. 2007;26:872–878. doi: 10.1007/s10067-006-0407-y. [DOI] [PubMed] [Google Scholar]
- Kalichman SC, Rompa D, Cage M. Distinguishing between overlapping somatic symptoms of depression and HIV disease in people living with HIV-AIDS. Journal of Nervous and Mental Disease. 2000;188:662–670. doi: 10.1097/00005053-200010000-00004. [DOI] [PubMed] [Google Scholar]
- Kennedy Q, Fung HH, Carstensen LL. Aging, time estimation, and emotion. In: McFadden SH, Atchley RC, editors. Aging and the meaning of time: A multidisciplinary exploration. New York: Springer; 2001. pp. 51–74. [Google Scholar]
- Kenny D, Kashy D, Cook W. Dyadic data analysis. New York: The Guilford Press; 2006. [Google Scholar]
- Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, Wittchen H, Kendler KS. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: Results from the National Comorbidity Survey. Archives of General Psychiatry. 1994;51:8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- Kline R. Principles and practices of structural equation modeling. New York: The Guilford Press; 2005. [Google Scholar]
- Kunik ME, Roundy K, Veazey C, Souchek J, Richardson P, Wray NP, Stanley MA. Surprisingly high prevalence of anxiety and depression in chronic breathing disorders. Chest. 2005;127:1205–1211. doi: 10.1378/chest.127.4.1205. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus Version 4.1. Los Angeles, CA: Muthén & Muthén; 1998–2006. [Google Scholar]
- O’Rourke N. Factor structure of the Center for Epidemiological Studies-Depression Scale (CES-D) among older men and women who provide care to persons with dementia. International Journal of Testing. 2005;5:265–277. [Google Scholar]
- Peek MK, Stimpson JP, Townsend AL, Markides KS. Well-being in older Mexican American spouses. The Gerontologist. 2006;46:258–265. doi: 10.1093/geront/46.2.258. [DOI] [PubMed] [Google Scholar]
- Plant EA, Sachs-Ericsson N. Racial and ethnic differences in depression: The roles of social support and meeting basic needs. Journal of Consulting and Clinical Psychology. 2004;72:41–52. doi: 10.1037/0022-006X.72.1.41. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Revenson TA, Majerovitz SD. Spouses’ support provision to chronically ill patients. Journal of Social and Personal Relationships. 1990;7:575–586. [Google Scholar]
- Siegel MJ, Bradley EH, Gallo WT, Kasl SV. The effect of spousal mental and physical health on husbands’ and wives’ depressive symptoms, among older adults: Longitudinal evidence from the health and retirement survey. Journal of Aging and Health. 2004;16:398. doi: 10.1177/0898264304264208. [DOI] [PubMed] [Google Scholar]
- Spiegel D, Giese-Davis J. Depression and cancer: Mechanisms and disease progression. Biological Psychiatry. 2003;54:269–282. doi: 10.1016/s0006-3223(03)00566-3. [DOI] [PubMed] [Google Scholar]
- Stecker T, Fortney JC, Steffick DE, Prajapati S. The triple threat for chronic disease: Obesity, race, and depression. Psychosomatics. 2006;47:513. doi: 10.1176/appi.psy.47.6.513. [DOI] [PubMed] [Google Scholar]
- Steffick DE, Wallace RB, Herzog AR. Documentation of affective functioning measures in the Health and Retirement Study. 2000. Survey Research Center, University of Michigan. Retrieved January 8, 2008, from http://hrsonline.isr.umich.edu/docs/userg/dr-005.pdf. [Google Scholar]
- Tower RB, Kasl SV. Depressive symptoms across older spouses: Longitudinal influences. Psychology and Aging. 1996;11:683–697. doi: 10.1037//0882-7974.11.4.683. [DOI] [PubMed] [Google Scholar]
- Townsend AL, Miller B, Guo S. Depressive symptomatology in middle-aged and older married couples: A dyadic analysis. Journal of Gerontology: Social Sciences. 2001;56B:S352–S364. doi: 10.1093/geronb/56.6.s352. [DOI] [PubMed] [Google Scholar]
- Whyte EM, Mulsant BH, Vanderbilt J, Dodge HH, Ganguli M. Depression after stroke: A prospective epidemiological study. Journal of the American Geriatrics Society. 2004;52:774–778. doi: 10.1111/j.1532-5415.2004.52217.x. [DOI] [PubMed] [Google Scholar]
- Wulsin LR, Vaillant GE, Wells VE. A systematic review of the mortality of depression. Psychosomatic Medicine. 1999;61:6–17. doi: 10.1097/00006842-199901000-00003. [DOI] [PubMed] [Google Scholar]
- Yang FM, Carzola-Lancaster DO, Jones RN. Within group differences in depression among older Hispanics living in the United States. Journal of Gerontology: Psychological Science. 2008;63B:P27–P32. doi: 10.1093/geronb/63.1.p27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang FM, Jones RN. Measurement differences in depression: Chronic health-related and sociodemographic effects in older Americans. Psychosomatic Medicine. 2008;70:993–1004. doi: 10.1097/PSY.0b013e31818ce4fa. [DOI] [PMC free article] [PubMed] [Google Scholar]