Abstract
The basal ganglia (BG) are composed of several nuclei involved in neural processing related to the execution of motor, cognitive and emotional activities. Preclinical and clinical data have implicated a role for these structures in pain processing. Recently neuroimaging has added important information on BG activation in conditions of acute pain, chronic pain and as a result of drug effects. Our current understanding of alterations in cortical and sub-cortical regions in pain suggests that the BG are uniquely involved in thalamo-cortico-BG loops to integrate many aspects of pain. These include the integration of motor, emotional, autonomic and cognitive responses to pain.
Introduction
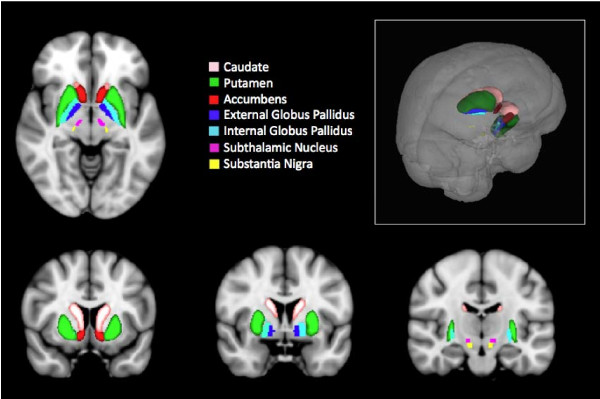
The basal ganglia (BG) consist of the striatum (caudate (C), putamen (Pu) and the core of the nucleus accumbens), the external segment of the globus pallidus (GP), the internal segment of the globus pallidus (GPi), the subthalamic nucleus (STh), and the substantia nigra (SN) [1-3] (Figure 1). Although best known for their role in motor systems, these regions are a major site for adaptive plasticity in the brain, affecting a broad range of normal behaviors [4] and neurological and psychiatric conditions [5].
Figure 1.
Basal Ganglia. Horizontal (A), Coronal (B-D) and (E) 3-D representation of the Basal Ganglia in the Human Brain. Sub-regions are noted in the color-coded key. Brain sections from FMRIB Software Library http://www.fmrib.ox.ac.uk/fsl/.
The first section of this review, Basal Ganglia: Pain Processing, summarizes the role of the BG in pain processing as has been reported in specific research and review papers. In the section titled Basal Ganglia: Functional Imaging Studies of Pain in Humans, we describe functional imaging studies in humans reporting activation of the BG in acute pain, chronic pain, and in response to analgesics. The third section titled Basal Ganglia: Lessons Learned from Functional Imaging attempts to integrate the information about lessons learned from functional imaging. The final section, Basal Ganglia: Imaging and Improved understanding of Clinical Applications, describes how imaging may provide insight to how and why certain therapies may be useful. Future measures of BG function may contribute significantly to our understanding about the brain changes associated with chronic pain and specific therapies that may change the brain in a manner that corresponds with therapeutic effects.
Basal Ganglia: Pain Processing
Both preclinical and clinical data support a role for the BG in pain processing [6,7].
Data supporting a role for the BG in pain and analgesia processing have been derived from numerous preclinical studies. These studies include electrophysiology [8,9], analgesic effects of microinjections into these regions [10], electrolytic lesion studies [11], chemical lesions of dopaminergic terminals [12,13], activation of striatal dopamine systems producing analgesia in rats [14] and imaging drug effects in neuropathic rat models [15]. In addition, novel pain pathways, for example those projecting from the spinal cord to the globus pallidus [16], have been discovered. Since the major review on the involvement of the basal ganglia in pain [6,7], the examples of preclinical studies noted above are not exhaustive and more recent studies have included numerous other contributions (e.g., [9,10,17-19]).
In the clinical domain, two disease patterns epitomize the role of the BG in pain - Parkinson's disease (PD) and Complex Regional Pain Syndrome (CRPS). In PD, the initial pathology involves the BG (i.e., loss of dopaminergic neurons in the substantia nigra [20]) that results in movement disorders, and affected subjects frequently have chronic pain [21-24]. In CRPS the initial event is most often relatively minor damage to a peripheral nerve [25,26], but with time expression of frequently associated movement disorders may become evident, thereby implicating BG involvement [27-30]. Both conditions are associated with movement disorders and both are associated with pain. In chronic pain, alterations of multiple sub-cortical and cortical processing, including sensory, emotional/affective, cognitive and modulatory systems, are present. Independent of specific somatosensory regions and pain modulation (e.g., SI and pain intensity, PAG and pain facilitation/inhibition), recent functional neuroimaging data suggest that the BG appear to be intimately involved in these processes.
Lesions of the BG in patients have offered further insights into the potential role of BG in pain and analgesia. Infarction of the lenticular nucleus (composed of the putamen and globus pallidus) may result in sensory deficits including pain in some patients [31]. Both unilateral and bilateral deep brain stimulation of the globus pallidus have been reported to improve pain by approximately 70%, and this improvement may persist for a significant period of time [32]. In Parkinson's disease, bilateral pallidotomy produces pain relief [33]. Taken together, these data provide insights into the potential contributions of the BG in chronic pain in humans.
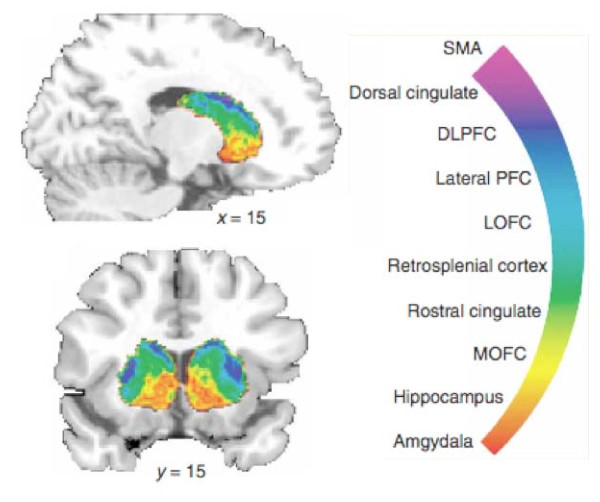
Multisensory integration takes place in the BG [34,35] that serves an important role in behavioral actions including motor responses [36]. The BG receives inputs from all cortical areas (including medial and orbital, prefrontal, dorsolateral, premotor and motor cortex, sensorimotor and parietal cortex) and the thalamus. Multiple cortical areas receive afferents from a single thalamic nucleus and send back information to different thalamic nuclei [37]. Efferent pathways from the BG project to frontal lobe areas including prefrontal, premotor and supplementary motor areas (used in motor planning). Thus the BG are well positioned to have influences on cortical regions involved in motor responses, in behavior relating to predicting events, and involved in attention and learning [38]. Using probabilistic tractography, a recent diffusion tensor imaging (DTI) study on connectivity patterns of the BG in humans [39] showed segregated and overlapping loops that include prefrontal, premotor, and motor networks to BG sub-regions (see Figure 2). In the cat for example, electrophysiological recordings have shown that neurons in the BG respond to visual, auditory and somatosensory information [35]. How this integration takes place is not well understood, but BG circuits are in a unique position to integrate cortical information to increase the speed of data processing tasks [40-42]. Similar processing may take place with emotional and cognitive information. Such processing is relevant to pain because the response to acute or chronic pain involves sensory, motor, autonomic, cognitive and emotional integration.
Figure 2.
Cortical Connectivity and Basal Ganglia. The BG receive multiple inputs from cortical and subcortical regions as noted in the figure. Many of these regions are involved in pain processing (see text). (From [175], Nature Neuroscience, Nature Publishing Group, with permission).
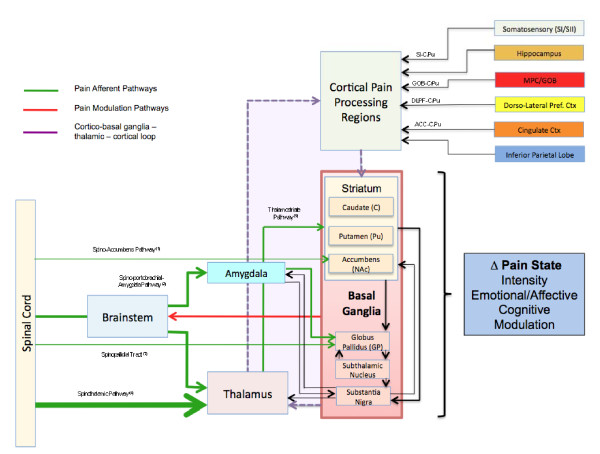
Figure 3 shows the connectivity patterns of the BG with respect to possible pain processing. Pain inputs into the BG may be considered to be from two major sources: (1) Afferent inputs from pain sensing systems via direct (e.g., spino-BG) and indirect (e.g., spino-thalamic-BG) pathways; and (2) from cortical and sub-cortical brain regions that contribute to the BG-Thalamic-Cortical loops. Cortical regions involved in these feedback loops are also known to have important roles in pain processing. These areas include the ACC, regions of the frontal lobe (e.g., dorsolateral prefrontal cortex (DLPF), orbitofrontal cortex (Gob)), parietal, insular, and hippocampal regions. Chudler and Dong have also reported putative nociceptive pathways into and out of the basal ganglia [6,7].
Figure 3.
Basal Ganglia and Pain Systems. Afferent inputs from spinal cord and brainstem have direct and indirect inputs into the BG, most are into the striatum but some input into the globus pallidus and substantia nigra. Thalamic inputs into various cortical regions are then processed and complete the cortico-BG-thalamic loop. Cortical inputs include those from a number of regions known to be involved in pain processing. Key: (1) Spino-accumbens pathway [57]; (2) Spino-parabrachial-amygdala pathways [176]; (3) Spino-thalamic pathway [177]; (4) Thalamo-Striatal pathway [38].
Basal Ganglia: Functional Imaging Studies of Pain in Humans
Functional imaging studies in healthy volunteers and patients with chronic pain have supported a growing role of the BG in pain processing. Previous work has suggested that the BG may be involved in most aspects of pain processing including sensory-discriminative, emotional/affective, cognitive dimension of pain and pain modulation [7]. Given our current understanding of these brain regions in the pain brain phenotype (i.e., functional brain changes in healthy and disease (see [43]) and our understanding of the basic integrative role the BG may play neural processing, it is suggested that the BG play a pivotal role in the behavioral manifestations of chronic pain. Although a large literature exists on the role of the BG in non-motor activities [44], brain imaging studies of acute and chronic pain have contributed to supporting preclinical and clinical work as playing an increasingly important role in acute and chronic pain processing and in the effects of some analgesics on brain function (Tables 1, 2 and 3).
Table 1.
fMRI Studies of Pain and Basal Ganglia Activation.
| Study Type | Condition | Stimulus | C | Pu | NAc | GP | STN | SN | Reference |
|---|---|---|---|---|---|---|---|---|---|
| Acute Pain | |||||||||
| Thermal Pain | Contact Heat | + | + | - | + | + | [45] | ||
| Contact Heat | - | [142] | |||||||
| Contact Heat | - | [58] | |||||||
| Contact Heat | + | [143] | |||||||
| Contact Heat | + | [144] | |||||||
| Contact Heat | + | [145] | |||||||
| Contact Heat | + | + | [146] | ||||||
| Contact Heat | + | [47] | |||||||
| Contact Heat | + | [147] | |||||||
| Laser | + | [148] | |||||||
| Cold | + | [49] | |||||||
| Cold (Prickle) | + | [48] | |||||||
| Electrical Pain | Current | + | [51] | ||||||
| Current | + | [95] | |||||||
| Electroacupuncture | + | [149] | |||||||
| Pressure Pain | + | + | + | [150] | |||||
| Capsaicin Sensitization | Punctate Mechanical | + | [91] | ||||||
| Punctate Mechanical | + | (+) | + | + | [151] | ||||
| Visceral Pain | Fundus Distention | + | + | [152] | |||||
| Esophageal Distention | + | + | [143] | ||||||
| Chronic Pain | |||||||||
| Neuropathic | Trigeminal (cold allodynia) | - | + | [56] | |||||
| Trigeminal (mechanical allodynia) | - | + | + | + | [56] | ||||
| Post Herpetic (spontaneous pain) | + | (+) | [153] | ||||||
| Complex Regional Pain Syndrome | Pediatric | - | [70] | ||||||
| Fibromyalgia | [154] | ||||||||
| Pressure | + | [150] | |||||||
| Catastrophising | + | + | [155] | ||||||
| Back Pain | + | [156] | |||||||
| Osteoarthritis | + | [156] | |||||||
| Visceral | Irritable Bowel Syndrome | - | + | [157] | |||||
| Empathy | |||||||||
| Visual | |||||||||
| Pictures | + | + | [158] | ||||||
| Pictures | + | [159] | |||||||
| Virtual Pain (needles) | + | [160] | |||||||
| Analgesics (phMRI) | |||||||||
| Opioid Agonists | Morphine | + | + | + | [58] | ||||
| Remifentanil | + | + | + | + | [83] | ||||
| Opioid Antagonists | Naloxone | + | + | + | + | [82] | |||
Key: E = evoked stimuli; + = increased BOLD signal; - = decreased BOLD signal
Table 2.
fMRI Measures of the Effects of Analgesics on Pain.
Table 3.
Positron Emission Tomography (PET) studies of Pain.
| Study Type | Condition | Receptor Binding | C | Pu | NAc | GP | STN | SN | Reference |
|---|---|---|---|---|---|---|---|---|---|
| Acute Pain | |||||||||
| Thermal Pain | Contact Heat (15)O-water | + | [161] | ||||||
| Contact Heat (15)O-water | + | [162] | |||||||
| Contact Heat (15)O-water | + | [163] | |||||||
| Contact Heat (Pain Threshold) | Dopamine receptor binding (11C) Raclopride | Binding - inverse correlation to Heat thershold | [133] | ||||||
| Muscle Pain Hypertonic Saline | (15)O-water | + | [164] | ||||||
| Dopamine Receptor Binding (11C) Raclopride | + | + | + | [135] | |||||
| Visceral Pain | Gastric Distenton (15)O-water | + | [165] | ||||||
| Placebo | |||||||||
| Muscle Pain Hypertonic Saline | Opioid and Dopamine receptor binding Placebo (11C) Raclopride (11C) Carfentanil | Increased opioid and dopamine release | [65] | ||||||
| Opioid and Dopamine receptor binding Placebo (11C) Raclopride (11C) Carfentanil | Decrease opioid and dopamine release | [65] | |||||||
| Chronic Pain | |||||||||
| Neuropathic Pain (Burning Mouth) | 6-[(18)F]fluorodopa | Decreased presynaptic dopamine function | [72] | ||||||
| Neuropathic Pain | Motor Cortex Stimulation (15)O-water | + | [141] | ||||||
| Atypical Facial Pain | Dopamine receptor binding [11C]raclopride | Increased D2 binding | [73] | ||||||
| Fibromyalgia | μ receptor (11C) Carfentanil | Decreased Opioid Binding | [166] | ||||||
| Dopamine receptor (11C) Raclopride | Decrease dopamine release | [74] | |||||||
| Analgesics | |||||||||
| Fentanyl | Opioid Effects (15)O-water | + | [167] | ||||||
| Ketamine | NMDA Receptor Binding (n-methyl11C)-ketamine | + | + | [168] | |||||
Since there are multiple sub-regions within the BG, preclinical studies using specific methods cannot easily define how these interact at the same time to integrate such information, including pain. Understanding the functional processing of pain and analgesia in these regions might afford insights into complex behaviors of brain systems in acute and chronic pain and help us understand how analgesics might affect pain processing. Brain imaging in humans includes a number of methods such as functional MRI (fMRI), pharmacological MRI (phMRI), morphometric/anatomical measures (diffusion tensor imaging and gray matter volumetric analysis), and positron emission tomography (functional PET (fPET) and ligand binding/displacement (phPET)) that allow whole brain evaluation of specific circuits.
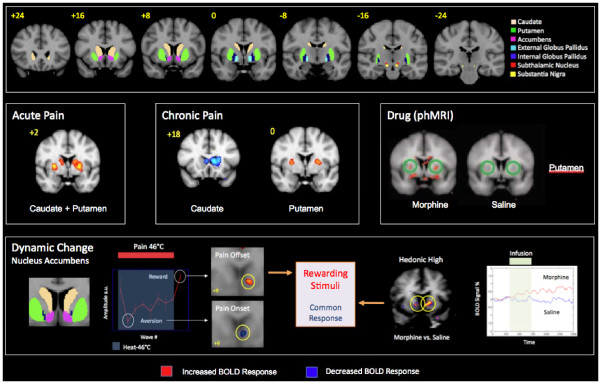
Basal Ganglia Activation in Acute Pain (Figure 4, Tables 1, 2 and 3)
Figure 4.
Examples of Basal Ganglia Activation in Pain and Analgesia. fMRI BOLD Activation in the nucleus accumbens following acute pain, allodynia neuropathic pain to cold and brush, and to morphine.
Noxious Stimuli
Early studies of pain using fMRI indicated activation patterns in the BG including the putamen and globus pallidus. These early observations have now been replicated in a number of functional imaging studies of experimental pain in humans, examples of which are shown in Tables 1 and 2. As noted in the tables, a considerable similarity exists in the activation patterns from multiple stimuli, including thermal (heat and cold), mechanical (in a hyperalgesic capsaicin model), painful electrical and visceral pain. Subsequent studies showed what seemed to be specific regional activation in other BG structures including the nucleus accumbens [45] and putamen [46,47]. However, most studies have evaluated or reported activation patterns and observed striatal involvement in a general context.
Tables 1 and 2 show positive activation is present in the caudate nucleus across multiple studies and across multiple modalities. In addition to those mentioned in the tables, activation in the caudate is present in "prickle" sensation evoked by cold stimuli [48]. In our own studies, cold has previously been shown to activate basal ganglia including the caudate [49]. Activation in the caudate nucleus to noxious stimulation has been suggested to be part of a pain modulatory system [50,51]. In support of this, electrical stimulation of the caudate in non-human primates diminished pain reactivity [52]. The authors suggested that the results indicate that the effect of caudate stimulation is to reduce the affective components of pain elicited by noxious electrocutaneous stimuli.
A few studies have evaluated specific activation in the putamen and nucleus accumbens. As noted in Tables 1 and 2, the putamen is commonly activated across most acute pain imaging studies. Pain activated the putamen bilaterally and a somatotopic organization for hand- and foot-related responses was only present in the contralateral putamen [53]. In healthy women, pain-evoked putaminal activation occurred during their follicular phase [54].
Activation of globus pallidus following painful stimulation has been shown in healthy subjects (Tables 1 and 2). Unlike the caudate and putamen, fewer studies have specifically reported activation in this BG structure. However, like the caudate and putamen, the globus pallidus has neurons that respond to noxious stimulation [9].
The nucleus accumbens (NAc), a brain substrate known to be involved in reward-aversion processing, has been shown to respond with opposite BOLD signal valence to rewarding or aversive stimuli [45,55]. Using a pain onset (aversive) and pain offset (rewarding) prolonged stimulus, a negative signal change with pain onset and a positive signal change with pain offset was observed in the NAc contralateral to the stimulus. The study supports the idea that the NAc fMRI signal may provide a useful marker for the effects of pain and analgesia in healthy volunteers. A parallel study on NAc activation in response to the direct effects of the analgesic (pain offset) morphine, showed the same increased (rewarding) BOLD signal in the structure [56]. Direct afferents from the trigeminal nucleus to the nucleus accumbens have been demonstrated in the rat; these have contralateral projections from lamina I but bilateral with contralateral predominance from lamina V [57]. These anatomical studies seem to agree with other studies showing contralateral activation in the NAc [45,55]. Subsequent studies indicated two components of activation within the NAc - an anterior, superior, and lateral component and another component that was posterior, inferior, and medial within the structure. The anatomical segregation may correlate with the functional components of the NAc (i.e., shell and core) that have been defined in other species (see [58]). The results support heterogeneity of function within the NAc and have implications for understanding the contribution of NAc function in processing of pain and analgesia [58]. The NAc has a pivotal role in aversive and rewarding (hedonic) processing [59].
Given that the reward system is part of the pain network [45], and that the placebo response is clearly involved in analgesia [60,61], it is not surprising that functional imaging has been the ideal technology to better understand neural networks involved in placebo in humans [62,63]. Recent reviews suggest that multiple brain regions (e.g., anterior cingulate cortex, anterior insula, prefrontal cortex and periaqueductal grey) are important in the placebo response [64]. Other studies strongly implicate the NAc and ventral BG in the placebo response [65].
Basal Ganglia Activation in Chronic Pain (Figure 4, Tables 1, 2 and 3)
An increase in gray matter in the BG has been reported in chronic back pain patients [66], in fibromyalgia [67], and in chronic vulval pain [68], suggesting some underlying functional alterations that drive these changes. In other chronic pain conditions, alterations in activation in BG regions have been demonstrated [55,69] where stimulation to the affected neuropathic regions produces significant activation in the BG. Specifically, contrast analysis between the affected and unaffected regions resulted in increased activation in the globus pallidus and putamen to mechanical and cold allodynia, as well as decreased activation in the caudate nucleus to mechanical, cold and heat allodynia [55]. Taken together these data appear to show a consistent decrease in the caudate nucleus to pain produced across multiple painful stimuli. Similarly, functional imaging of pain in a group of pediatric patients with CRPS has shown significant activation in the BG with cold and brush stimuli, and also displays decreased activation in the caudate nucleus [70].
Chronic pain has also been shown to alter BG structure with measures of gray matter volume and white matter tract integrity. In a more recent report, measures of gray matter morphometry and white matter anisotropy were measured in patients with complex regional pain syndrome (CRPS) [71]. Alterations in morphometry indicated atrophy in a single cluster encompassing the right insula, right ventromedial prefrontal cortex (VMPFC), and right NAc. Additionally, decreased connectivity was reported between the ventromedial prefrontal cortices to the BG [71].
Alterations in dopaminergic and opioidergic function in the BG have been reported in clinical pain conditions. In patients with burning mouth syndrome, decreases in dopamine in the putamen suggest reduced dopaminergic inhibition may contribute to the chronic pain condition [72]. In addition, both atypical facial pain [73] and fibromyalgia patients [74] show an abnormal dopamine response. Such data are consistent with other conditions associated with decreased dopamine, including Parkinson's disease [75,76]. In addition to the alterations in dopamine, decreased μ binding in chronic pain conditions such as fibromyalgia may contribute to altered pain processing [77]. In psychiatric disorders, pain produces increased activation in putaminal regions in post traumatic stress disorder, or PTSD, [78] that when considered with the diminished pain sensitivity reported in this patient group may also be caused in part to abnormalities within the BG.
Basal Ganglia Activation and Analgesics (Figure 4, Tables 1, 2 and 3)
Functional imaging of drug effects (also known as pharmacological MRI or phMRI) has been done in the context of BG function in preclinical [79] and clinical [80,81] conditions. The evaluation of direct brain changes in functional activity in response to known analgesic drugs has been limited to a small group that include morphine [55], naloxone [82], remifentanil [83] and buprenorphine [84]. Direct effects of μ opioid agonist or antagonist infusions both show activation in the BG, including the NAc. In these experiments, the direction of BOLD signal is opposite with increased activation following morphine infusion [55] and a decreased activation following infusion of naloxone [82] in healthy volunteers. The opposite direct pharmacological effects indicate some specificity of response but may also underlie NAc drive with respect to pain and analgesia. An increased activation may be part of an endogenous analgesic drive or emotional drive since increased activation patterns within the NAc are also seen in other fMRI experiments on reward [85-87]. The increase (hyperalgesic) pain response (inhibition of tonic opioid drive) to pain was observed in brain regions following naloxone that included concurrent activation in the globus pallidus, caudate and putamen. Opioids may produce changes in the BG including increases in D2 receptor binding [88]. However not all imaging studies report BG activation in response to opioids, either because they were not specifically focused on these regions or they used less sensitive methods (e.g., alfentanil [89]; remifentanil [90]).
Few authors have evaluated the effects of non-opioid analgesics on BG responsiveness. In one example, although not specifically referred to in their paper, gabapentin reduced activation in the BG [91]; specifically, for gabapentin vs. placebo comparison in a hyperalgesic paradigm, deactivation in the caudate was present in the single dose study in healthy volunteers.
Other drugs, considered to be analgesics, have been evaluated using imaging in a similar manner to that noted above, and these studies report alterations in the human striatum. For example tetrahydrocannabinol (known to be an analgesic [92]) produces dopamine release in the striatum [93]. Similar results have been shown for the NMDA antagonist ketamine (reviewed by [94]).
Lessons Learned from Imaging
Based on imaging data of pain as well as a growing literature on pain in conditions with abnormalities of BG function, it is clear that a constellation of brain regions plays an important role in acute and chronic pain (see Tables 1, 2 and 3). With the exception of studies on the NAc and the pallidum (see above), few functional imaging studies in humans have attempted to evaluate other regions of the BG function in pain. Nevertheless there is increasing evidence for the important roles of the region in neural systems' adaptation to pain.
Putamen (P) shows consistent increase in activation across multiple pain imaging studies
The putamen, a structure that shows somatotopic activation to pain [53], is consistently activated during acute and chronic pain conditions and is affected by analgesic administration. Chronic pain has also been shown to increase putamen volume (see [67]) suggesting, perhaps, that a continuous drive producing increased activation may result in processes that enhance gray matter volume in the structure. This region may receive direct inputs from sensory systems, but also from cortical inputs. Some studies (e.g., [83]) have suggested delayed functional activation in BG circuits (e.g., caudate) following remifentanil, implicating that activation in these regions occurs as a consequence or subsequent to initial activation of thalamo-cortical circuits. Activation seems to be present with painful stimuli but missing with non-painful stimuli [95].
Opposite Signal Changes in Caudate and NAc in Acute vs. Chronic Pain
In contrast to increases in putaminal activation for acute pain, BOLD signals are opposite in chronic pain across multiple pain studies. The reason for this observation is not known although the nature of reward processing in acute vs. chronic pain is clearly different [45,59,71].
Smaller Nuclei (ST, SN) are not clearly defined in many fMRI studies
Only a few brain imaging studies have reported activation in the smaller nuclei of the BG even though they may be present. Although there are studies in animals investigating SN mechanisms of pain [96], future brain imaging studies in humans will contribute to our understanding of the role of these nuclei in pain processing. Developments such as accurate automated identification of sub-nuclei within the basal ganglia should be helpful in measures of functional brain changes [97].
Feed-forward and Feedback Loops - Integrating, Modifying, and Modulating the Pain Experience
The BG are involved in the integration of information between cortical and thalamic regions and in particular the three domains of pain processing - sensory, emotional/cognitive and endogenous/modulatory. Some investigators have suggested that these regions have evolved as a "centralized selection device to resolve conflicts over access to limited motor and cognitive resources" [98]. Phylogenetically older, sub-cortical connections exist between the BG and brainstem regions involved in sensorimotor processing [99], and more recent evidence points to BG involvement through direct connections from sensory inputs not involving cortical loops [100]. Dysfunctional cortico-BG-thalamic loops may contribute to the maintenance of chronic pain and the evolution of altered neural processing that may be a basis for co-morbid behaviors. Whether brain processing of pain is dependent on external neural drive (i.e., peripheral/feed-forward inputs) or internal neural drive (i.e., subcortical or cortical drive/feedback), the BG are central processors that may play a role in integrating these divergent inputs that may modify pain over time.
Basal Ganglia: Imaging and Improved Understanding of Clinical Applications
Cortical Stimulation and Chronic Pain - Acting via Cortico-Striatal-Thalamic Loops
Cortical stimulation has been used either directly with electrodes placed on the motor cortex [101] or through the use of repetitive transcranial stimulation (rTMS) [102]. Some investigators have postulated that motor cortex neurostimulation produces an analgesic effect by modulation of the affective components of pain and not of the sensory components [103]. In support of this hypothesis, stimulation of the secondary somatosensory cortex (SII), but not motor cortex, results in increased pain thresholds and altered discriminative capacity to pain [104]. A combination of motor cortex stimulation (MCS) and postoperative fMRI showed an inhibiting effect on the primary sensorimotor cortex as well as on the contralateral primary motor and sensitive cortices [105] without changes in BG. Others have argued that MCS may act through activation of perigenual cingulate and orbitofrontal areas to alter the emotional appraisal of pain or cortical-brainstem (e.g., PAG) activation that enhances inhibition of pain [106] or alterations in endogenous opioid systems [107]. Given the cortico-striatal loops, stimulation of a number of cortical regions may thus be involved in pain reduction. Stimulation of dorsolateral prefrontal cortex, motor cortex or sensory cortices may have different effects based on the specificity of cortico-striatal loops. In addition, connectivity between the BG and modulatory regions including the PAG/brainstem or through the NAc [108-110] may also contribute to the potential mechanism of cortical activation resulting in analgesia.
Anterior Cingulate Lesions and Pain Control
Both clinical [111] and preclinical [112] studies have suggested that the ACC results in alterations of pain processing. The interesting issue seems to be the dissociation of pain intensity from pain affect (caring about the pain) [113,114]. The ACC in humans may be involved with linking reward-related information [115] and with alternative actions, since destruction of the ACC results in errors related to planning [116]. The ACC has projections to the caudate nucleus and the NAc [117], and ACC lesions may produce an attenuation of a negative pain affect [118] through a combination of neural networks that include these circuits.
BG and Learned Behaviors
Pain is clearly a complex process that affects multiple brain systems. It debatable if pain is a learned behavior, but the BG may have a role in learning due to its involvement in habit and stimulus-response learning [119]. Such learning may be derived from pain related regions involved in sensory (e.g., pain intensity coding regions such as SI), affective (e.g., cingulate or anterior insula) or cognitive functioning (medial and lateral prefrontal cortices). Similar to the notion of "chunking action repertoires" for motor action, it may be that pain related repertoires include motor related changes.
BG and Emergence of Central Pain
Aside from CRPS, other conditions including depression and Parkinson's disease have BG pathology that may be important in their clinical presentation of centralized pain [120]. In Parkinson's disease with central pain, electrophysiological measures of pain pathways are normal, but hyperalgesia to repetitive stimuli is present; this is attenuated by L-dopa [121], and altered central processing in these conditions results in generalized pain symptoms. Although the basis for these changes is unknown, it may be the result of altered chemicals in the BG, such as central dopamine, or related to aberrant networks that induce a kindling-like pain [122]. Changes in neural connectivity that produce changes in increased synaptic strength [123] and could include pain facilitatory circuits [124] may also underlie these changes. Although the basis for these changes is unknown, alterations may then lead to other changes such as abnormal gating of sensory-motor function involving parallel changes thalamic regions [125]. Imaging patients with depression in whom non-dermatomal sensory deficits were present shows that hypometabolic patterns (FDG-PET) of activation in the putamen was observed [126].
Regions of the thalamus including the paramedian and anterolateral are known to be involved with central pain (e.g., post stroke pain) [38,127]. The striatum receives excitatory input from the thalamus. The centromedian (CM) and parafascicular (Pf) thalamic nuclei are important sources of thalamostriatal projections [128] and send connections to the putamen and caudate [128,129]. Moreover, the topography of these connections corresponds with cortical sensorimotor territory observed following cortical injections [130].
Basal Ganglia and Opioid Systems
The BG has high levels of endogenous opioids, and high binding of opioid receptors are present within the BG [131]. In a number of chronic pain conditions, receptor-binding studies indicate a decreased opioidergic tone. Many analgesics act at the level of the basal ganglia and may contribute to both analgesic and addictive processes. An understanding of how these functional processes are differentiated by different endogenous chemicals (e.g., opioidergic vs. dopaminergic (see [65])) may contribute to better analgesics since opioidergic tone might be abnormal [77].
Dopaminergic Drugs and Pain
Given that pain now has a functional basis in terms of regions activated including those that are classically involved in reward [45], and that chronic pain may be a reward deficit syndrome [132], modulating dopamine may have important possibilities for pain treatment. Parkinson's disease patients have improved pain control when treated with L-dopa [21,121]. Changes in dopamine are a critical element in Parkinson's disease where abnormal pain processing is present in both conditions. Recent imaging data have reported a direct correlation between striatal dopamine D2/D3 receptors and sensory thresholds as being selective for the modality of pain but not for non-painful stimuli [133]. Striatal dopamine D2/D3 receptors may control a modulatory pathway producing a parallel shift in the stimulus-response function for sensory signals [134]. Others have suggested differential processing of pain within the BG - a more dorsal DA D2 receptor-mediated neurotransmission in the caudate and putamen that correlates with subjective ratings of sensory and affective qualities of the pain, along with a more ventral system involving the NAc, is associated with emotional processing [135]. Such differences may be important in drug effects on pain. The use of antipsychotic medications for pain is not new [136], and the number needed to treat (NNT; this is the number of patients to be treated for the first subject to show a 50% analgesic effect) of 2.6 is very competitive with the best drugs available for chronic pain [137]. However, these drugs have extrapyramidal and sedative effects, and atypical antipsychotics that have fewer side effects may have analgesic properties as assessed in a limited number of studies [138]. Newer drugs that target specific dopamine receptors may prove to be more useful.
BG Deep Brain Stimulation and Strategies for Pain Relief
Brain imaging affords the possibility to measure changes in brain circuits that may be altered as a result of deep brain stimulation. Some of these have shown specific changes in BG circuitry [139]. In the latter, stimulation of the ventroposterior medial thalamus (VPM) resulted in decreases in activation of the substantia nigra when activation prior to stimulation vs. post stimulation that provided pain relief was measured (pain, no stimulation vs. no pain, no stimulation). Thalamic stimulation may activate thalamo-cortical-BG loops that contribute to the analgesic response [140].
Conclusions
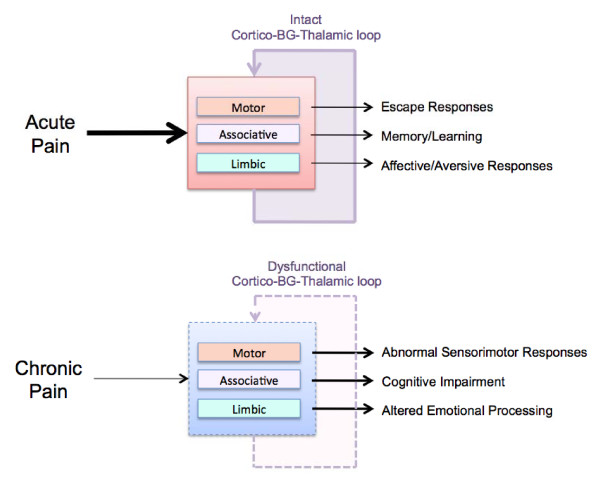
Functional imaging of pain has shown clear and consistent changes in the BG in pain conditions. Table 4 summarizes the salient features of each sub-region of the BG as it pertains to overall putative function and specific functions in pain, and Figure 5 summarizes potential alterations in BG outputs affecting behaviors in acute and chronic pain. Future work should help contribute to further understanding functional and anatomical connectivity of inputs and circuits that show how the BG may be involved in acute and chronic pain. Such findings may present an increasing and important role of these brain regions in the centralization of chronic pain and the contribution to the altered brain in chronic pain conditions. Future studies, using a combination of imaging approaches, will help define the specificity of BG in pain processing. For example, functional connectivity analysis can demonstrate probable correlations between BG subdivisions and other brain regions [141].
Table 4.
Components of the Basal Ganglia - Putative Function in Pain Processing.
| Region | Putative Role in Pain | Reference |
|---|---|---|
| Caudate | Involved in avoidance behavior to pain | [169] |
| Decrease pain sensitivity following apomorphine injections | [14] | |
| Encode noxious stimuli intensity to minimize bodily harm | [9] | |
| Behavioral Reinforcement (? Including Pain) | [3] | |
| Putamen | Somatotopic modulation of pain | [148] |
| Variations in subjective ratings of pain | [135] | |
| Nucleus Accumbens | Affective Valence for Reward and Aversive Stimuli | [45,170] |
| Processing of emotional salience of pain | [135] | |
| Globus Pallidus | Encoding of behavioral repertoires (? Including pain) | [3] |
| Deep brain stimulation inhibits pain | [89,171] | |
| Morphine analgesia | [172] | |
| Subthalamic Nucleus | Functional suppression of neural messages | [173] |
| Behavioral Inhibition | [174] | |
| Regulates level of execution of cortical commands; processing of emotional, cognitive and motor behavior | [3] | |
| Substantia Nigra | Heterogeneous response to aversive stimuli | [96] |
Figure 5.
Basal Ganglia Function in Acute and Chronic Pain. Top: Acute Pain Processing is a normal response where pain produces responses in brain circuits that usually revert to normal. Some of these processes are integrated in the BG and result in escape responses: components of memory and learning of pain and affective responses to pain. Bottom: In chronic pain both inputs from peripheral systems and cortical and subcortical regions are abnormal. The result is that BG functions as well as cortico-BG-thalamic loop functions are altered. The result may be altered integration of sensori-motor responses, cognitive impairment and emotional processing.
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
DB and JU conceptualized the paper. All authors contributed to the drafting of the paper. All authors have read and approved the final manuscript.
Contributor Information
David Borsook, Email: dborsook@partners.org.
Jaymin Upadhyay, Email: jayminu@mclean.harvard.edu.
Eric H Chudler, Email: chudler@u.washington.edu.
Lino Becerra, Email: lbecerra@partners.org.
Acknowledgements
This work was supported by NINDS K24 NS064050 (DB) and the L Herlands Grant for Pain Research (DB and LB). We would like to thank N. Maleki for help with some of the brain images.
References
- Graybiel AM. The basal ganglia: learning new tricks and loving it. Curr Opin Neurobiol. 2005;15:638–644. doi: 10.1016/j.conb.2005.10.006. [DOI] [PubMed] [Google Scholar]
- Kreitzer AC, Malenka RC. Striatal plasticity and basal ganglia circuit function. Neuron. 2008;60:543–554. doi: 10.1016/j.neuron.2008.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yelnik J. Modeling the organization of the basal ganglia. Rev Neurol (Paris) 2008;164:969–976. doi: 10.1016/j.neurol.2008.04.019. [DOI] [PubMed] [Google Scholar]
- Graybiel AM. Network-level neuroplasticity in cortico-basal ganglia pathways. Parkinsonism Relat Disord. 2004;10:293–296. doi: 10.1016/j.parkreldis.2004.03.007. [DOI] [PubMed] [Google Scholar]
- Obeso JA, Rodriguez MC, DeLong MR. Basal ganglia pathophysiology. A critical review. Adv Neurol. 1997;74:3–18. [PubMed] [Google Scholar]
- Barker RA. The basal ganglia and pain. Int J Neurosci. 1988;41:29–34. doi: 10.3109/00207458808985739. [DOI] [PubMed] [Google Scholar]
- Chudler EH, Dong WK. The role of the basal ganglia in nociception and pain. Pain. 1995;60:3–38. doi: 10.1016/0304-3959(94)00172-B. [DOI] [PubMed] [Google Scholar]
- Bernard JF, Huang GF, Besson JM. Nucleus centralis of the amygdala and the globus pallidus ventralis: electrophysiological evidence for an involvement in pain processes. J Neurophysiol. 1992;68:551–569. doi: 10.1152/jn.1992.68.2.551. [DOI] [PubMed] [Google Scholar]
- Chudler EH. Response properties of neurons in the caudate-putamen and globus pallidus to noxious and non-noxious thermal stimulation in anesthetized rats. Brain Res. 1998;812:283–288. doi: 10.1016/S0006-8993(98)00971-8. [DOI] [PubMed] [Google Scholar]
- Tashev R, Belcheva S, Milenov K, Belcheva I. Antinociceptive effect of somatostatin microinjected into caudate putamen. Peptides. 2001;22:1079–1083. doi: 10.1016/S0196-9781(01)00431-4. [DOI] [PubMed] [Google Scholar]
- Saade NE, Shbeir SA, Atweh SF, Jabbur SJ. Effects of cerebral cortical and striatal lesions on autotomy following peripheral neurectomy in rats. Physiol Behav. 1996;60:559–566. doi: 10.1016/S0031-9384(96)80032-1. [DOI] [PubMed] [Google Scholar]
- Saade NE, Atweh SF, Bahuth NB, Jabbur SJ. Augmentation of nociceptive reflexes and chronic deafferentation pain by chemical lesions of either dopaminergic terminals or midbrain dopaminergic neurons. Brain Res. 1997;751:1–12. doi: 10.1016/S0006-8993(96)01164-X. [DOI] [PubMed] [Google Scholar]
- Takeda R, Ikeda T, Tsuda F, Abe H, Hashiguchi H, Ishida Y, Nishimori T. Unilateral lesions of mesostriatal dopaminergic pathway alters the withdrawal response of the rat hindpaw to mechanical stimulation. Neurosci Res. 2005;52:31–36. doi: 10.1016/j.neures.2005.01.005. [DOI] [PubMed] [Google Scholar]
- Lin MT, Wu JJ, Chandra A, Tsay BL. Activation of striatal dopamine receptors induces pain inhibition in rats. J Neural Transm. 1981;51:213–222. doi: 10.1007/BF01248953. [DOI] [PubMed] [Google Scholar]
- Porro CA, Cavazzuti M, Baraldi P, Giuliani D, Panerai AE, Corazza R. CNS pattern of metabolic activity during tonic pain: evidence for modulation by beta-endorphin. Eur J Neurosci. 1999;11:874–888. doi: 10.1046/j.1460-9568.1999.00494.x. [DOI] [PubMed] [Google Scholar]
- Braz JM, Nassar MA, Wood JN, Basbaum AI. Parallel "pain" pathways arise from subpopulations of primary afferent nociceptor. Neuron. 2005;47:787–793. doi: 10.1016/j.neuron.2005.08.015. [DOI] [PubMed] [Google Scholar]
- Chudler EH, Lu Y. Nociceptive behavioral responses to chemical, thermal and mechanical stimulation after unilateral, intrastriatal administration of 6-hydroxydopamine. Brain Res. 2008;1213:41–47. doi: 10.1016/j.brainres.2008.03.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greco R, Tassorelli C, Armentero MT, Sandrini G, Nappi G, Blandini F. Role of central dopaminergic circuitry in pain processing and nitroglycerin-induced hyperalgesia. Brain Res. 2008;1238:215–223. doi: 10.1016/j.brainres.2008.08.022. [DOI] [PubMed] [Google Scholar]
- Heindl-Erdmann C, Axmann R, Kreitz S, Zwerina J, Penninger J, Schett G, Brune K, Hess A. Combining functional magnetic resonance imaging with mouse genomics: new options in pain research. Neuroreport. 2009. [DOI] [PubMed]
- Schapira AH. Neurobiology and treatment of Parkinson's disease. Trends Pharmacol Sci. 2009;30:41–47. doi: 10.1016/j.tips.2008.10.005. [DOI] [PubMed] [Google Scholar]
- Cheon SM, Park MJ, Kim WJ, Kim JW. Non-motor off symptoms in Parkinson's disease. J Korean Med Sci. 2009;24:311–314. doi: 10.3346/jkms.2009.24.2.311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Defazio G, Berardelli A, Fabbrini G, Martino D, Fincati E, Fiaschi A, Moretto G, Abbruzzese G, Marchese R, Bonuccelli U. Pain as a nonmotor symptom of Parkinson disease: evidence from a case-control study. Arch Neurol. 2008;65:1191–1194. doi: 10.1001/archneurol.2008.2. [DOI] [PubMed] [Google Scholar]
- Ford B. Parkinson disease: Pain in Parkinson disease: the hidden epidemic. Nat Rev Neurol. 2009;5:242–243. doi: 10.1038/nrneurol.2009.50. [DOI] [PubMed] [Google Scholar]
- Djaldetti R, Shifrin A, Rogowski Z, Sprecher E, Melamed E, Yarnitsky D. Quantitative measurement of pain sensation in patients with Parkinson disease. Neurology. 2004;62:2171–2175. doi: 10.1212/01.wnl.0000130455.38550.9d. [DOI] [PubMed] [Google Scholar]
- Birklein F. Complex regional pain syndrome. J Neurol. 2005;252:131–138. doi: 10.1007/s00415-005-0737-8. [DOI] [PubMed] [Google Scholar]
- Schwartzman RJ, Alexander GM, Grothusen J. Pathophysiology of complex regional pain syndrome. Expert Rev Neurother. 2006;6:669–681. doi: 10.1586/14737175.6.5.669. [DOI] [PubMed] [Google Scholar]
- Agrawal SK, Rittey CD, Harrower NA, Goddard JM, Mordekar SR. Movement disorders associated with complex regional pain syndrome in children. Dev Med Child Neurol. 2009;51:557–562. doi: 10.1111/j.1469-8749.2008.03181.x. [DOI] [PubMed] [Google Scholar]
- Lang AE, Angel M, Bhatia K, Chen R, Fahn S, Hallett M, Schrag A, Thompson P. Myoclonus in complex regional pain syndrome. Mov Disord. 2009;24:314–316. doi: 10.1002/mds.22355. author reply 316. [DOI] [PubMed] [Google Scholar]
- van Rijn MA, Marinus J, Putter H, van Hilten JJ. Onset and progression of dystonia in complex regional pain syndrome. Pain. 2007;130:287–293. doi: 10.1016/j.pain.2007.03.027. [DOI] [PubMed] [Google Scholar]
- Schott GD. Peripherally-triggered CRPS and dystonia. Pain. 2007;130:203–207. doi: 10.1016/j.pain.2007.04.013. [DOI] [PubMed] [Google Scholar]
- Russmann H, Vingerhoets F, Ghika J, Maeder P, Bogousslavsky J. Acute infarction limited to the lenticular nucleus: clinical, etiologic, and topographic features. Arch Neurol. 2003;60:351–355. doi: 10.1001/archneur.60.3.351. [DOI] [PubMed] [Google Scholar]
- Loher TJ, Burgunder JM, Weber S, Sommerhalder R, Krauss JK. Effect of chronic pallidal deep brain stimulation on off period dystonia and sensory symptoms in advanced Parkinson's disease. J Neurol Neurosurg Psychiatry. 2002;73:395–399. doi: 10.1136/jnnp.73.4.395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Favre J, Burchiel KJ, Taha JM, Hammerstad J. Outcome of unilateral and bilateral pallidotomy for Parkinson's disease: patient assessment. Neurosurgery. 2000;46:344–353. doi: 10.1097/00006123-200002000-00017. discussion 353-345. [DOI] [PubMed] [Google Scholar]
- Chudler EH, Sugiyama K, Dong WK. Multisensory convergence and integration in the neostriatum and globus pallidus of the rat. Brain Res. 1995;674:33–45. doi: 10.1016/0006-8993(94)01427-J. [DOI] [PubMed] [Google Scholar]
- Nagy A, Eordegh G, Paroczy Z, Markus Z, Benedek G. Multisensory integration in the basal ganglia. Eur J Neurosci. 2006;24:917–924. doi: 10.1111/j.1460-9568.2006.04942.x. [DOI] [PubMed] [Google Scholar]
- Markus Z, Eordegh G, Paroczy Z, Benedek G, Nagy A. Modality distribution of sensory neurons in the feline caudate nucleus and the substantia nigra. Acta Biol Hung. 2008;59:269–279. doi: 10.1556/ABiol.59.2008.3.1. [DOI] [PubMed] [Google Scholar]
- Haber SN, Calzavara R. The cortico-basal ganglia integrative network: the role of the thalamus. Brain Res Bull. 2009;78:69–74. doi: 10.1016/j.brainresbull.2008.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herrero MT, Barcia C, Navarro JM. Functional anatomy of thalamus and basal ganglia. Childs Nerv Syst. 2002;18:386–404. doi: 10.1007/s00381-002-0604-1. [DOI] [PubMed] [Google Scholar]
- Draganski B, Kherif F, Kloppel S, Cook PA, Alexander DC, Parker GJ, Deichmann R, Ashburner J, Frackowiak RS. Evidence for segregated and integrative connectivity patterns in the human Basal Ganglia. J Neurosci. 2008;28:7143–7152. doi: 10.1523/JNEUROSCI.1486-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baev KV. Disturbances of learning processes in the basal ganglia in the pathogenesis of Parkinson's disease: a novel theory. Neurol Res. 1995;17:38–48. doi: 10.1080/01616412.1995.11740285. [DOI] [PubMed] [Google Scholar]
- Leyden J, Kleinig T. The role of the basal ganglia in data processing. Med Hypotheses. 2008;71:61–64. doi: 10.1016/j.mehy.2008.02.013. [DOI] [PubMed] [Google Scholar]
- Prodoehl J, Yu H, Wasson P, Corcos DM, Vaillancourt DE. Effects of visual and auditory feedback on sensorimotor circuits in the basal ganglia. J Neurophysiol. 2008;99:3042–3051. doi: 10.1152/jn.01108.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borsook D, Becerra L. Phenotyping central nervous system circuitry in chronic pain using functional MRI: considerations and potential implications in the clinic. Curr Pain Headache Rep. 2007;11:201–207. doi: 10.1007/s11916-007-0191-7. [DOI] [PubMed] [Google Scholar]
- Graybiel AM. Habits, rituals, and the evaluative brain. Annu Rev Neurosci. 2008;31:359–387. doi: 10.1146/annurev.neuro.29.051605.112851. [DOI] [PubMed] [Google Scholar]
- Becerra L, Breiter HC, Wise R, Gonzalez RG, Borsook D. Reward circuitry activation by noxious thermal stimuli. Neuron. 2001;32:927–946. doi: 10.1016/S0896-6273(01)00533-5. [DOI] [PubMed] [Google Scholar]
- Bingel U, Quante M, Knab R, Bromm B, Weiller C, Buchel C. Subcortical structures involved in pain processing: evidence from single-trial fMRI. Pain. 2002;99:313–321. doi: 10.1016/S0304-3959(02)00157-4. [DOI] [PubMed] [Google Scholar]
- Sung EJ, Yoo SS, Yoon HW, Oh SS, Han Y, Park HW. Brain activation related to affective dimension during thermal stimulation in humans: a functional magnetic resonance imaging study. Int J Neurosci. 2007;117:1011–1027. doi: 10.1080/00207450600934432. [DOI] [PubMed] [Google Scholar]
- Davis KD, Pope GE, Crawley AP, Mikulis DJ. Neural correlates of prickle sensation: a percept-related fMRI study. Nat Neurosci. 2002;5:1121–1122. doi: 10.1038/nn955. [DOI] [PubMed] [Google Scholar]
- Tracey I, Becerra L, Chang I, Breiter H, Jenkins L, Borsook D, Gonzalez RG. Noxious hot and cold stimulation produce common patterns of brain activation in humans: a functional magnetic resonance imaging study. Neurosci Lett. 2000;288:159–162. doi: 10.1016/S0304-3940(00)01224-6. [DOI] [PubMed] [Google Scholar]
- Freund W, Klug R, Weber F, Stuber G, Schmitz B, Wunderlich AP. Perception and suppression of thermally induced pain: a fMRI study. Somatosens Mot Res. 2009;26:1–10. doi: 10.1080/08990220902738243. [DOI] [PubMed] [Google Scholar]
- Freund W, Stuber G, Wunderlich AP, Schmitz B. Cortical correlates of perception and suppression of electrically induced pain. Somatosens Mot Res. 2007;24:203–212. doi: 10.1080/08990220701723636. [DOI] [PubMed] [Google Scholar]
- Lineberry CG, Vierck CJ. Attenuation of pain reactivity by caudate nucleus stimulation in monkeys. Brain Res. 1975;98:119–134. doi: 10.1016/0006-8993(75)90513-2. [DOI] [PubMed] [Google Scholar]
- Bingel U, Lorenz J, Glauche V, Knab R, Glascher J, Weiller C, Buchel C. Somatotopic organization of human somatosensory cortices for pain: a single trial fMRI study. Neuroimage. 2004;23:224–232. doi: 10.1016/j.neuroimage.2004.05.021. [DOI] [PubMed] [Google Scholar]
- Choi JC, Park SK, Kim YH, Shin YW, Kwon JS, Kim JS, Kim JW, Kim SY, Lee SG, Lee MS. Different brain activation patterns to pain and pain-related unpleasantness during the menstrual cycle. Anesthesiology. 2006;105:120–127. doi: 10.1097/00000542-200607000-00021. [DOI] [PubMed] [Google Scholar]
- Becerra L, Harter K, Gonzalez RG, Borsook D. Functional magnetic resonance imaging measures of the effects of morphine on central nervous system circuitry in opioid-naive healthy volunteers. Anesth Analg. 2006;103:208–216. doi: 10.1213/01.ane.0000221457.71536.e0. table of contents. [DOI] [PubMed] [Google Scholar]
- Becerra L, Morris S, Bazes S, Gostic R, Sherman S, Gostic J, Pendse G, Moulton E, Scrivani S, Keith D. Trigeminal neuropathic pain alters responses in CNS circuits to mechanical (brush) and thermal (cold and heat) stimuli. J Neurosci. 2006;26:10646–10657. doi: 10.1523/JNEUROSCI.2305-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burstein R, Giesler GJ Jr. Retrograde labeling of neurons in spinal cord that project directly to nucleus accumbens or the septal nuclei in the rat. Brain Res. 1989;497:149–154. doi: 10.1016/0006-8993(89)90981-5. [DOI] [PubMed] [Google Scholar]
- Aharon I, Becerra L, Chabris CF, Borsook D. Noxious heat induces fMRI activation in two anatomically distinct clusters within the nucleus accumbens. Neurosci Lett. 2006;392:159–164. doi: 10.1016/j.neulet.2005.09.054. [DOI] [PubMed] [Google Scholar]
- Borsook D, Becerra L, Carlezon WA Jr, Shaw M, Renshaw P, Elman I, Levine J. Reward-aversion circuitry in analgesia and pain: implications for psychiatric disorders. Eur J Pain. 2007;11:7–20. doi: 10.1016/j.ejpain.2005.12.005. [DOI] [PubMed] [Google Scholar]
- Enck P, Benedetti F, Schedlowski M. New insights into the placebo and nocebo responses. Neuron. 2008;59:195–206. doi: 10.1016/j.neuron.2008.06.030. [DOI] [PubMed] [Google Scholar]
- Hoffman GA, Harrington A, Fields HL. Pain and the placebo: what we have learned. Perspect Biol Med. 2005;48:248–265. doi: 10.1353/pbm.2005.0054. [DOI] [PubMed] [Google Scholar]
- Colloca L, Benedetti F, Porro CA. Experimental designs and brain mapping approaches for studying the placebo analgesic effect. Eur J Appl Physiol. 2008;102:371–380. doi: 10.1007/s00421-007-0593-6. [DOI] [PubMed] [Google Scholar]
- Zubieta JK, Stohler CS. Neurobiological mechanisms of placebo responses. Ann N Y Acad Sci. 2009;1156:198–210. doi: 10.1111/j.1749-6632.2009.04424.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kong J, Kaptchuk TJ, Polich G, Kirsch I, Gollub RL. Placebo analgesia: findings from brain imaging studies and emerging hypotheses. Rev Neurosci. 2007;18:173–190. doi: 10.1515/revneuro.2007.18.3-4.173. [DOI] [PubMed] [Google Scholar]
- Scott DJ, Stohler CS, Egnatuk CM, Wang H, Koeppe RA, Zubieta JK. Placebo and nocebo effects are defined by opposite opioid and dopaminergic responses. Arch Gen Psychiatry. 2008;65:220–231. doi: 10.1001/archgenpsychiatry.2007.34. [DOI] [PubMed] [Google Scholar]
- Schmidt-Wilcke T, Leinisch E, Ganssbauer S, Draganski B, Bogdahn U, Altmeppen J, May A. Affective components and intensity of pain correlate with structural differences in gray matter in chronic back pain patients. Pain. 2006;125:89–97. doi: 10.1016/j.pain.2006.05.004. [DOI] [PubMed] [Google Scholar]
- Schmidt-Wilcke T, Luerding R, Weigand T, Jurgens T, Schuierer G, Leinisch E, Bogdahn U. Striatal grey matter increase in patients suffering from fibromyalgia--a voxel-based morphometry study. Pain. 2007;132(Suppl 1):S109–116. doi: 10.1016/j.pain.2007.05.010. [DOI] [PubMed] [Google Scholar]
- Schweinhardt P, Kuchinad A, Pukall CF, Bushnell MC. Increased gray matter density in young women with chronic vulvar pain. Pain. 2008;140:411–419. doi: 10.1016/j.pain.2008.09.014. [DOI] [PubMed] [Google Scholar]
- Becerra L, Schwartzman RJ, Kiefer RT, Rohr P, Moulton EA, Wallin D, Pendse G, Morris S, Borsook D. CNS Measures of Pain Responses Pre- and Post-Anesthetic Ketamine in a Patient with Complex Regional Pain Syndrome. Pain Med. 2009. [DOI] [PubMed]
- Lebel A, Becerra L, Wallin D, Moulton EA, Morris S, Pendse G, Jasciewicz J, Stein M, Aiello-Lammens M, Grant E. fMRI reveals distinct CNS processing during symptomatic and recovered complex regional pain syndrome in children. Brain. 2008;131:1854–1879. doi: 10.1093/brain/awn123. [DOI] [PubMed] [Google Scholar]
- Geha PY, Baliki MN, Harden RN, Bauer WR, Parrish TB, Apkarian AV. The brain in chronic CRPS pain: abnormal gray-white matter interactions in emotional and autonomic regions. Neuron. 2008;60:570–581. doi: 10.1016/j.neuron.2008.08.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaaskelainen SK, Rinne JO, Forssell H, Tenovuo O, Kaasinen V, Sonninen P, Bergman J. Role of the dopaminergic system in chronic pain -- a fluorodopa-PET study. Pain. 2001;90:257–260. doi: 10.1016/S0304-3959(00)00409-7. [DOI] [PubMed] [Google Scholar]
- Hagelberg N, Forssell H, Aalto S, Rinne JO, Scheinin H, Taiminen T, Nagren K, Eskola O, Jaaskelainen SK. Altered dopamine D2 receptor binding in atypical facial pain. Pain. 2003;106:43–48. doi: 10.1016/S0304-3959(03)00275-6. [DOI] [PubMed] [Google Scholar]
- Wood PB, Schweinhardt P, Jaeger E, Dagher A, Hakyemez H, Rabiner EA, Bushnell MC, Chizh BA. Fibromyalgia patients show an abnormal dopamine response to pain. Eur J Neurosci. 2007;25:3576–3582. doi: 10.1111/j.1460-9568.2007.05623.x. [DOI] [PubMed] [Google Scholar]
- Hagelberg N, Jaaskelainen SK, Martikainen IK, Mansikka H, Forssell H, Scheinin H, Hietala J, Pertovaara A. Striatal dopamine D2 receptors in modulation of pain in humans: a review. Eur J Pharmacol. 2004;500:187–192. doi: 10.1016/j.ejphar.2004.07.024. [DOI] [PubMed] [Google Scholar]
- Wood PB. Role of central dopamine in pain and analgesia. Expert Rev Neurother. 2008;8:781–797. doi: 10.1586/14737175.8.5.781. [DOI] [PubMed] [Google Scholar]
- Harris RE, Clauw DJ, Scott DJ, McLean SA, Gracely RH, Zubieta JK. Decreased central mu-opioid receptor availability in fibromyalgia. J Neurosci. 2007;27:10000–10006. doi: 10.1523/JNEUROSCI.2849-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geuze E, Westenberg HG, Jochims A, de Kloet CS, Bohus M, Vermetten E, Schmahl C. Altered pain processing in veterans with posttraumatic stress disorder. Arch Gen Psychiatry. 2007;64:76–85. doi: 10.1001/archpsyc.64.1.76. [DOI] [PubMed] [Google Scholar]
- Sanchez-Pernaute R, Jenkins BG, Choi JK, Iris Chen YC, Isacson O. In vivo evidence of D3 dopamine receptor sensitization in parkinsonian primates and rodents with l-DOPA-induced dyskinesias. Neurobiol Dis. 2007;27:220–227. doi: 10.1016/j.nbd.2007.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhattacharyya S, Fusar-Poli P, Borgwardt S, Martin-Santos R, Nosarti C, O'Carroll C, Allen P, Seal ML, Fletcher PC, Crippa JA. Modulation of mediotemporal and ventrostriatal function in humans by Delta9-tetrahydrocannabinol: a neural basis for the effects of Cannabis sativa on learning and psychosis. Arch Gen Psychiatry. 2009;66:442–451. doi: 10.1001/archgenpsychiatry.2009.17. [DOI] [PubMed] [Google Scholar]
- Kelly C, de Zubicaray G, Di Martino A, Copland DA, Reiss PT, Klein DF, Castellanos FX, Milham MP, McMahon K. L-dopa modulates functional connectivity in striatal cognitive and motor networks: a double-blind placebo-controlled study. J Neurosci. 2009;29:7364–7378. doi: 10.1523/JNEUROSCI.0810-09.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borras MC, Becerra L, Ploghaus A, Gostic JM, DaSilva A, Gonzalez RG, Borsook D. fMRI measurement of CNS responses to naloxone infusion and subsequent mild noxious thermal stimuli in healthy volunteers. J Neurophysiol. 2004;91:2723–2733. doi: 10.1152/jn.00249.2003. [DOI] [PubMed] [Google Scholar]
- Leppa M, Korvenoja A, Carlson S, Timonen P, Martinkauppi S, Ahonen J, Rosenberg PH, Aronen HJ, Kalso E. Acute opioid effects on human brain as revealed by functional magnetic resonance imaging. Neuroimage. 2006;31:661–669. doi: 10.1016/j.neuroimage.2005.12.019. [DOI] [PubMed] [Google Scholar]
- Upadhyay J, Pendse G, Anderson J, Schwarz AJ, Baumgartner R, Coimbra A, Bishop J, Knudsen J, George E, Grachev I. Improved characterization of BOLD responses for evoked sensory stimuli. Neuroimage. 2009. [DOI] [PubMed]
- Breiter HC, Gollub RL, Weisskoff RM, Kennedy DN, Makris N, Berke JD, Goodman JM, Kantor HL, Gastfriend DR, Riorden JP. Acute effects of cocaine on human brain activity and emotion. Neuron. 1997;19:591–611. doi: 10.1016/S0896-6273(00)80374-8. [DOI] [PubMed] [Google Scholar]
- Schott BH, Minuzzi L, Krebs RM, Elmenhorst D, Lang M, Winz OH, Seidenbecher CI, Coenen HH, Heinze HJ, Zilles K. Mesolimbic functional magnetic resonance imaging activations during reward anticipation correlate with reward-related ventral striatal dopamine release. J Neurosci. 2008;28:14311–14319. doi: 10.1523/JNEUROSCI.2058-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Filbey FM, Schacht JP, Myers US, Chavez RS, Hutchison KE. Marijuana craving in the brain. Proc Natl Acad Sci USA. 2009;106:13016–13021. doi: 10.1073/pnas.0903863106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagelberg N, Kajander JK, Nagren K, Hinkka S, Hietala J, Scheinin H. Mu-receptor agonism with alfentanil increases striatal dopamine D2 receptor binding in man. Synapse. 2002;45:25–30. doi: 10.1002/syn.10078. [DOI] [PubMed] [Google Scholar]
- Adler LJ, Gyulai FE, Diehl DJ, Mintun MA, Winter PM, Firestone LL. Regional brain activity changes associated with fentanyl analgesia elucidated by positron emission tomography. Anesth Analg. 1997;84:120–126. doi: 10.1097/00000539-199701000-00023. [DOI] [PubMed] [Google Scholar]
- Wagner KJ, Sprenger T, Kochs EF, Tolle TR, Valet M, Willoch F. Imaging human cerebral pain modulation by dose-dependent opioid analgesia: a positron emission tomography activation study using remifentanil. Anesthesiology. 2007;106:548–556. doi: 10.1097/00000542-200703000-00020. [DOI] [PubMed] [Google Scholar]
- Iannetti GD, Zambreanu L, Wise RG, Buchanan TJ, Huggins JP, Smart TS, Vennart W, Tracey I. Pharmacological modulation of pain-related brain activity during normal and central sensitization states in humans. Proc Natl Acad Sci USA. 2005;102:18195–18200. doi: 10.1073/pnas.0506624102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guindon J, Hohmann AG. The Endocannabinoid System and Pain. CNS Neurol Disord Drug Targets. 2009;8:403–421. doi: 10.2174/187152709789824660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bossong MG, van Berckel BN, Boellaard R, Zuurman L, Schuit RC, Windhorst AD, van Gerven JM, Ramsey NF, Lammertsma AA, Kahn RS. Delta 9-tetrahydrocannabinol induces dopamine release in the human striatum. Neuropsychopharmacology. 2009;34:759–766. doi: 10.1038/npp.2008.138. [DOI] [PubMed] [Google Scholar]
- Rabiner EA. Imaging of striatal dopamine release elicited with NMDA antagonists: is there anything there to be seen? J Psychopharmacol. 2007;21:253–258. doi: 10.1177/0269881107077767. [DOI] [PubMed] [Google Scholar]
- Downar J, Mikulis DJ, Davis KD. Neural correlates of the prolonged salience of painful stimulation. Neuroimage. 2003;20:1540–1551. doi: 10.1016/S1053-8119(03)00407-5. [DOI] [PubMed] [Google Scholar]
- Brown MT, Henny P, Bolam JP, Magill PJ. Activity of neurochemically heterogeneous dopaminergic neurons in the substantia nigra during spontaneous and driven changes in brain state. J Neurosci. 2009;29:2915–2925. doi: 10.1523/JNEUROSCI.4423-08.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinzon-Morales RD, Garces-Arboleda M, Orozco-Gutierrez AA. Automatic identification of various nuclei in the basal ganglia for Parkinson's disease neurosurgery. Conf Proc IEEE Eng Med Biol Soc. 2009;1:3473–3476. doi: 10.1109/IEMBS.2009.5334611. [DOI] [PubMed] [Google Scholar]
- Redgrave P, Prescott TJ, Gurney K. The basal ganglia: a vertebrate solution to the selection problem? Neuroscience. 1999;89:1009–1023. doi: 10.1016/S0306-4522(98)00319-4. [DOI] [PubMed] [Google Scholar]
- McHaffie JG, Stanford TR, Stein BE, Coizet V, Redgrave P. Subcortical loops through the basal ganglia. Trends Neurosci. 2005;28:401–407. doi: 10.1016/j.tins.2005.06.006. [DOI] [PubMed] [Google Scholar]
- Schulz JM, Redgrave P, Mehring C, Aertsen A, Clements KM, Wickens JR, Reynolds JN. Short-latency activation of striatal spiny neurons via subcortical visual pathways. J Neurosci. 2009;29:6336–6347. doi: 10.1523/JNEUROSCI.4815-08.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lima MC, Fregni F. Motor cortex stimulation for chronic pain: systematic review and meta-analysis of the literature. Neurology. 2008;70:2329–2337. doi: 10.1212/01.wnl.0000314649.38527.93. [DOI] [PubMed] [Google Scholar]
- Lefaucheur JP. Use of repetitive transcranial magnetic stimulation in pain relief. Expert Rev Neurother. 2008;8:799–808. doi: 10.1586/14737175.8.5.799. [DOI] [PubMed] [Google Scholar]
- Andre-Obadia N, Mertens P, Gueguen A, Peyron R, Garcia-Larrea L. Pain relief by rTMS: differential effect of current flow but no specific action on pain subtypes. Neurology. 2008;71:833–840. doi: 10.1212/01.wnl.0000325481.61471.f0. [DOI] [PubMed] [Google Scholar]
- Valmunen T, Pertovaara A, Taiminen T, Virtanen A, Parkkola R, Jaaskelainen SK. Modulation of facial sensitivity by navigated rTMS in healthy subjects. Pain. 2009;142:149–158. doi: 10.1016/j.pain.2008.12.031. [DOI] [PubMed] [Google Scholar]
- Roux FE, Ibarrola D, Lazorthes Y, Berry I. Chronic motor cortex stimulation for phantom limb pain: a functional magnetic resonance imaging study: technical case report. Neurosurgery. 2008;62:978–985. doi: 10.1227/01.neu.0000333765.28198.18. [DOI] [PubMed] [Google Scholar]
- Garcia-Larrea L, Peyron R. Motor cortex stimulation for neuropathic pain: From phenomenology to mechanisms. Neuroimage. 2007;37(Suppl 1):S71–79. doi: 10.1016/j.neuroimage.2007.05.062. [DOI] [PubMed] [Google Scholar]
- Maarrawi J, Peyron R, Mertens P, Costes N, Magnin M, Sindou M, Laurent B, Garcia-Larrea L. Motor cortex stimulation for pain control induces changes in the endogenous opioid system. Neurology. 2007;69:827–834. doi: 10.1212/01.wnl.0000269783.86997.37. [DOI] [PubMed] [Google Scholar]
- Ma QP, Shi YS, Han JS. Further studies on interactions between periaqueductal gray, nucleus accumbens and habenula in antinociception. Brain Res. 1992;583:292–295. doi: 10.1016/s0006-8993(10)80036-8. [DOI] [PubMed] [Google Scholar]
- Altier N, Stewart J. The role of dopamine in the nucleus accumbens in analgesia. Life Sci. 1999;65:2269–2287. doi: 10.1016/S0024-3205(99)00298-2. [DOI] [PubMed] [Google Scholar]
- Gear RW, Aley KO, Levine JD. Pain-induced analgesia mediated by mesolimbic reward circuits. J Neurosci. 1999;19:7175–7181. doi: 10.1523/JNEUROSCI.19-16-07175.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilkinson HA. Bilateral anterior cingulotomy for chronic noncancer pain. Neurosurgery. 2000;46:1535–1536. doi: 10.1097/00006123-200006000-00051. [DOI] [PubMed] [Google Scholar]
- Ren LY, Lu ZM, Liu MG, Yu YQ, Li Z, Shang GW, Chen J. Distinct roles of the anterior cingulate cortex in spinal and supraspinal bee venom-induced pain behaviors. Neuroscience. 2008;153:268–278. doi: 10.1016/j.neuroscience.2008.01.067. [DOI] [PubMed] [Google Scholar]
- LaGraize SC, Borzan J, Peng YB, Fuchs PN. Selective regulation of pain affect following activation of the opioid anterior cingulate cortex system. Exp Neurol. 2006;197:22–30. doi: 10.1016/j.expneurol.2005.05.008. [DOI] [PubMed] [Google Scholar]
- LaGraize SC, Labuda CJ, Rutledge MA, Jackson RL, Fuchs PN. Differential effect of anterior cingulate cortex lesion on mechanical hypersensitivity and escape/avoidance behavior in an animal model of neuropathic pain. Exp Neurol. 2004;188:139–148. doi: 10.1016/j.expneurol.2004.04.003. [DOI] [PubMed] [Google Scholar]
- Bush G, Vogt BA, Holmes J, Dale AM, Greve D, Jenike MA, Rosen BR. Dorsal anterior cingulate cortex: a role in reward-based decision making. Proc Natl Acad Sci USA. 2002;99:523–528. doi: 10.1073/pnas.012470999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams ZM, Bush G, Rauch SL, Cosgrove GR, Eskandar EN. Human anterior cingulate neurons and the integration of monetary reward with motor responses. Nat Neurosci. 2004;7:1370–1375. doi: 10.1038/nn1354. [DOI] [PubMed] [Google Scholar]
- Baleydier C, Mauguiere F. The duality of the cingulate gyrus in monkey. Neuroanatomical study and functional hypothesis. Brain. 1980;103:525–554. doi: 10.1093/brain/103.3.525. [DOI] [PubMed] [Google Scholar]
- LaBuda CJ, Fuchs PN. Attenuation of negative pain affect produced by unilateral spinal nerve injury in the rat following anterior cingulate cortex activation. Neuroscience. 2005;136:311–322. doi: 10.1016/j.neuroscience.2005.07.010. [DOI] [PubMed] [Google Scholar]
- Graybiel AM. The basal ganglia and chunking of action repertoires. Neurobiol Learn Mem. 1998;70:119–136. doi: 10.1006/nlme.1998.3843. [DOI] [PubMed] [Google Scholar]
- Ford B. Pain in Parkinson's disease. Clin Neurosci. 1998;5:63–72. doi: 10.1016/S0967-5868(98)90204-1. [DOI] [PubMed] [Google Scholar]
- Schestatsky P, Kumru H, Valls-Sole J, Valldeoriola F, Marti MJ, Tolosa E, Chaves ML. Neurophysiologic study of central pain in patients with Parkinson disease. Neurology. 2007;69:2162–2169. doi: 10.1212/01.wnl.0000295669.12443.d3. [DOI] [PubMed] [Google Scholar]
- Post RM. Do the epilepsies, pain syndromes, and affective disorders share common kindling-like mechanisms? Epilepsy Res. 2002;50:203–219. doi: 10.1016/S0920-1211(02)00081-5. [DOI] [PubMed] [Google Scholar]
- Ji RR, Kohno T, Moore KA, Woolf CJ. Central sensitization and LTP: do pain and memory share similar mechanisms? Trends Neurosci. 2003;26:696–705. doi: 10.1016/j.tins.2003.09.017. [DOI] [PubMed] [Google Scholar]
- McNally GP. Pain facilitatory circuits in the mammalian central nervous system: their behavioral significance and role in morphine analgesic tolerance. Neurosci Biobehav Rev. 1999;23:1059–1078. doi: 10.1016/S0149-7634(99)00040-8. [DOI] [PubMed] [Google Scholar]
- Kaji R. [Sensory-motor disintegration in the basal ganglia disorders] Rinsho Shinkeigaku. 2001;41:1076–1078. [PubMed] [Google Scholar]
- Egloff N, Sabbioni ME, Salathe C, Wiest R, Juengling FD. Nondermatomal somatosensory deficits in patients with chronic pain disorder: Clinical findings and hypometabolic pattern in FDG-PET. Pain. 2009. [DOI] [PubMed]
- Wessel K, Vieregge P, Kessler C, Kompf D. Thalamic stroke: correlation of clinical symptoms, somatosensory evoked potentials, and CT findings. Acta Neurol Scand. 1994;90:167–173. doi: 10.1111/j.1600-0447.1994.tb01573.x. [DOI] [PubMed] [Google Scholar]
- Sadikot AF, Rymar VV. The primate centromedian-parafascicular complex: anatomical organization with a note on neuromodulation. Brain Res Bull. 2009;78:122–130. doi: 10.1016/j.brainresbull.2008.09.016. [DOI] [PubMed] [Google Scholar]
- Sidibe M, Pare JF, Smith Y. Nigral and pallidal inputs to functionally segregated thalamostriatal neurons in the centromedian/parafascicular intralaminar nuclear complex in monkey. J Comp Neurol. 2002;447:286–299. doi: 10.1002/cne.10247. [DOI] [PubMed] [Google Scholar]
- Francois C, Sintonen H, Sulkava R, Rive B. Cost effectiveness of memantine in moderately severe to severe Alzheimer's disease: a markov model in Finland. Clin Drug Investig. 2004;24:373–384. doi: 10.2165/00044011-200424070-00001. [DOI] [PubMed] [Google Scholar]
- Baumgartner U, Buchholz HG, Bellosevich A, Magerl W, Siessmeier T, Rolke R, Hohnemann S, Piel M, Rosch F, Wester HJ. High opiate receptor binding potential in the human lateral pain system. Neuroimage. 2006;30:692–699. doi: 10.1016/j.neuroimage.2005.10.033. [DOI] [PubMed] [Google Scholar]
- Comings DE, Blum K. Reward deficiency syndrome: genetic aspects of behavioral disorders. Prog Brain Res. 2000;126:325–341. doi: 10.1016/S0079-6123(00)26022-6. full_text. [DOI] [PubMed] [Google Scholar]
- Martikainen IK, Hagelberg N, Mansikka H, Hietala J, Nagren K, Scheinin H, Pertovaara A. Association of striatal dopamine D2/D3 receptor binding potential with pain but not tactile sensitivity or placebo analgesia. Neurosci Lett. 2005;376:149–153. doi: 10.1016/j.neulet.2004.11.045. [DOI] [PubMed] [Google Scholar]
- Pertovaara A, Martikainen IK, Hagelberg N, Mansikka H, Nagren K, Hietala J, Scheinin H. Striatal dopamine D2/D3 receptor availability correlates with individual response characteristics to pain. Eur J Neurosci. 2004;20:1587–1592. doi: 10.1111/j.1460-9568.2004.03622.x. [DOI] [PubMed] [Google Scholar]
- Scott DJ, Heitzeg MM, Koeppe RA, Stohler CS, Zubieta JK. Variations in the human pain stress experience mediated by ventral and dorsal basal ganglia dopamine activity. J Neurosci. 2006;26:10789–10795. doi: 10.1523/JNEUROSCI.2577-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patt RB, Proper G, Reddy S. The neuroleptics as adjuvant analgesics. J Pain Symptom Manage. 1994;9:446–453. doi: 10.1016/0885-3924(94)90201-1. [DOI] [PubMed] [Google Scholar]
- Seidel S, Aigner M, Ossege M, Pernicka E, Wildner B, Sycha T. Antipsychotics for acute and chronic pain in adults. Cochrane Database Syst Rev. 2008. p. CD004844. [DOI] [PubMed]
- Fishbain DA, Cutler RB, Lewis J, Cole B, Rosomoff RS, Rosomoff HL. Do the second-generation "atypical neuroleptics" have analgesic properties? A structured evidence-based review. Pain Med. 2004;5:359–365. doi: 10.1111/j.1526-4637.2004.04054.x. [DOI] [PubMed] [Google Scholar]
- Kupers RC, Gybels JM, Gjedde A. Positron emission tomography study of a chronic pain patient successfully treated with somatosensory thalamic stimulation. Pain. 2000;87:295–302. doi: 10.1016/S0304-3959(00)00295-5. [DOI] [PubMed] [Google Scholar]
- Duncan GH, Kupers RC, Marchand S, Villemure JG, Gybels JM, Bushnell MC. Stimulation of human thalamus for pain relief: possible modulatory circuits revealed by positron emission tomography. J Neurophysiol. 1998;80:3326–3330. doi: 10.1152/jn.1998.80.6.3326. [DOI] [PubMed] [Google Scholar]
- Peyron R, Faillenot I, Mertens P, Laurent B, Garcia-Larrea L. Motor cortex stimulation in neuropathic pain. Correlations between analgesic effect and hemodynamic changes in the brain. A PET study. Neuroimage. 2007;34:310–321. doi: 10.1016/j.neuroimage.2006.08.037. [DOI] [PubMed] [Google Scholar]
- Becerra L, Iadarola M, Borsook D. CNS activation by noxious heat to the hand or foot: site-dependent delay in sensory but not emotion circuitry. J Neurophysiol. 2004;91:533–541. doi: 10.1152/jn.00326.2003. [DOI] [PubMed] [Google Scholar]
- Strigo IA, Duncan GH, Boivin M, Bushnell MC. Differentiation of visceral and cutaneous pain in the human brain. J Neurophysiol. 2003;89:3294–3303. doi: 10.1152/jn.01048.2002. [DOI] [PubMed] [Google Scholar]
- Oshiro Y, Quevedo AS, McHaffie JG, Kraft RA, Coghill RC. Brain mechanisms supporting spatial discrimination of pain. J Neurosci. 2007;27:3388–3394. doi: 10.1523/JNEUROSCI.5128-06.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keltner JR, Furst A, Fan C, Redfern R, Inglis B, Fields HL. Isolating the modulatory effect of expectation on pain transmission: a functional magnetic resonance imaging study. J Neurosci. 2006;26:4437–4443. doi: 10.1523/JNEUROSCI.4463-05.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks JC, Zambreanu L, Godinez A, Craig AD, Tracey I. Somatotopic organisation of the human insula to painful heat studied with high resolution functional imaging. Neuroimage. 2005;27:201–209. doi: 10.1016/j.neuroimage.2005.03.041. [DOI] [PubMed] [Google Scholar]
- Dunckley P, Wise RG, Fairhurst M, Hobden P, Aziz Q, Chang L, Tracey I. A comparison of visceral and somatic pain processing in the human brainstem using functional magnetic resonance imaging. J Neurosci. 2005;25:7333–7341. doi: 10.1523/JNEUROSCI.1100-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bingel U, Glascher J, Weiller C, Buchel C. Somatotopic representation of nociceptive information in the putamen: an event-related fMRI study. Cereb Cortex. 2004;14:1340–1345. doi: 10.1093/cercor/bhh094. [DOI] [PubMed] [Google Scholar]
- Zhang WT, Jin Z, Cui GH, Zhang KL, Zhang L, Zeng YW, Luo F, Chen AC, Han JS. Relations between brain network activation and analgesic effect induced by low vs. high frequency electrical acupoint stimulation in different subjects: a functional magnetic resonance imaging study. Brain Res. 2003;982:168–178. doi: 10.1016/S0006-8993(03)02983-4. [DOI] [PubMed] [Google Scholar]
- Gracely RH, Petzke F, Wolf JM, Clauw DJ. Functional magnetic resonance imaging evidence of augmented pain processing in fibromyalgia. Arthritis Rheum. 2002;46:1333–1343. doi: 10.1002/art.10225. [DOI] [PubMed] [Google Scholar]
- Lee MC, Zambreanu L, Menon DK, Tracey I. Identifying brain activity specifically related to the maintenance and perceptual consequence of central sensitization in humans. J Neurosci. 2008;28:11642–11649. doi: 10.1523/JNEUROSCI.2638-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu CL, Wu YT, Yeh TC, Chen LF, Chang FY, Lee SD, Ho LT, Hsieh JC. Neuronal correlates of gastric pain induced by fundus distension: a 3T-fMRI study. Neurogastroenterol Motil. 2004;16:575–587. doi: 10.1111/j.1365-2982.2004.00562.x. [DOI] [PubMed] [Google Scholar]
- Geha PY, Baliki MN, Wang X, Harden RN, Paice JA, Apkarian AV. Brain dynamics for perception of tactile allodynia (touch-induced pain) in postherpetic neuralgia. Pain. 2008;138:641–656. doi: 10.1016/j.pain.2008.02.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burgmer M, Pogatzki-Zahn E, Gaubitz M, Wessoleck E, Heuft G, Pfleiderer B. Altered brain activity during pain processing in fibromyalgia. Neuroimage. 2009;44:502–508. doi: 10.1016/j.neuroimage.2008.09.008. [DOI] [PubMed] [Google Scholar]
- Gracely RH, Geisser ME, Giesecke T, Grant MA, Petzke F, Williams DA, Clauw DJ. Pain catastrophizing and neural responses to pain among persons with fibromyalgia. Brain. 2004;127:835–843. doi: 10.1093/brain/awh098. [DOI] [PubMed] [Google Scholar]
- Baliki MN, Geha PY, Jabakhanji R, Harden N, Schnitzer TJ, Apkarian AV. A preliminary fMRI study of analgesic treatment in chronic back pain and knee osteoarthritis. Mol Pain. 2008;4:47. doi: 10.1186/1744-8069-4-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song GH, Venkatraman V, Ho KY, Chee MW, Yeoh KG, Wilder-Smith CH. Cortical effects of anticipation and endogenous modulation of visceral pain assessed by functional brain MRI in irritable bowel syndrome patients and healthy controls. Pain. 2006;126:79–90. doi: 10.1016/j.pain.2006.06.017. [DOI] [PubMed] [Google Scholar]
- Gu X, Han S. Attention and reality constraints on the neural processes of empathy for pain. Neuroimage. 2007;36:256–267. doi: 10.1016/j.neuroimage.2007.02.025. [DOI] [PubMed] [Google Scholar]
- Botvinick M, Jha AP, Bylsma LM, Fabian SA, Solomon PE, Prkachin KM. Viewing facial expressions of pain engages cortical areas involved in the direct experience of pain. Neuroimage. 2005;25:312–319. doi: 10.1016/j.neuroimage.2004.11.043. [DOI] [PubMed] [Google Scholar]
- Ushida T, Ikemoto T, Tanaka S, Shinozaki J, Taniguchi S, Murata Y, McLaughlin M, Arai YC, Tamura Y. Virtual needle pain stimuli activates cortical representation of emotions in normal volunteers. Neurosci Lett. 2008;439:7–12. doi: 10.1016/j.neulet.2008.04.085. [DOI] [PubMed] [Google Scholar]
- Jones AK, Brown WD, Friston KJ, Qi LY, Frackowiak RS. Cortical and subcortical localization of response to pain in man using positron emission tomography. Proc Biol Sci. 1991;244:39–44. doi: 10.1098/rspb.1991.0048. [DOI] [PubMed] [Google Scholar]
- Coghill RC, Gilron I, Iadarola MJ. Hemispheric lateralization of somatosensory processing. J Neurophysiol. 2001;85:2602–2612. doi: 10.1152/jn.2001.85.6.2602. [DOI] [PubMed] [Google Scholar]
- Coghill RC, Sang CN, Maisog JM, Iadarola MJ. Pain intensity processing within the human brain: a bilateral, distributed mechanism. J Neurophysiol. 1999;82:1934–1943. doi: 10.1152/jn.1999.82.4.1934. [DOI] [PubMed] [Google Scholar]
- Korotkov A, Ljubisavljevic M, Thunberg J, Kataeva G, Roudas M, Pakhomov S, Radovanovic S, Lyskov E, Medvedev S, Johansson H. Changes in human regional cerebral blood flow following hypertonic saline induced experimental muscle pain: a positron emission tomography study. Neurosci Lett. 2002;335:119–123. doi: 10.1016/S0304-3940(02)01181-3. [DOI] [PubMed] [Google Scholar]
- Ladabaum U, Minoshima S, Hasler WL, Cross D, Chey WD, Owyang C. Gastric distention correlates with activation of multiple cortical and subcortical regions. Gastroenterology. 2001;120:369–376. doi: 10.1053/gast.2001.21201. [DOI] [PubMed] [Google Scholar]
- Schmidt B, Mayr J, Fasching G, Nores H. [Equestrian accidents in children and adolescents] Unfallchirurg. 1994;97:661–662. [PubMed] [Google Scholar]
- Firestone LL, Gyulai F, Mintun M, Adler LJ, Urso K, Winter PM. Human brain activity response to fentanyl imaged by positron emission tomography. Anesth Analg. 1996;82:1247–1251. doi: 10.1097/00000539-199606000-00025. [DOI] [PubMed] [Google Scholar]
- Hartvig P, Valtysson J, Lindner KJ, Kristensen J, Karlsten R, Gustafsson LL, Persson J, Svensson JO, Oye I, Antoni G. Central nervous system effects of subdissociative doses of (S)-ketamine are related to plasma and brain concentrations measured with positron emission tomography in healthy volunteers. Clin Pharmacol Ther. 1995;58:165–173. doi: 10.1016/0009-9236(95)90194-9. [DOI] [PubMed] [Google Scholar]
- Koyama T, Kato K, Mikami A. During pain-avoidance neurons activated in the macaque anterior cingulate and caudate. Neurosci Lett. 2000;283:17–20. doi: 10.1016/S0304-3940(00)00894-6. [DOI] [PubMed] [Google Scholar]
- Borsook D, Becerra L, Hargreaves R. A role for fMRI in optimizing CNS drug development. Nat Rev Drug Discov. 2006;5:411–424. doi: 10.1038/nrd2027. [DOI] [PubMed] [Google Scholar]
- Stancanello J, Romanelli P, Pantelis E, Sebastiano F, Modugno N. Atlas-based functional radiosurgery: early results. Med Phys. 2009;36:457–463. doi: 10.1118/1.3056460. [DOI] [PubMed] [Google Scholar]
- Anagnostakis Y, Zis V, Spyraki C. Analgesia induced by morphine injected into the pallidum. Behav Brain Res. 1992;48:135–143. doi: 10.1016/S0166-4328(05)80149-4. [DOI] [PubMed] [Google Scholar]
- Benabid AL, Wallace B, Mitrofanis J, Xia C, Piallat B, Fraix V, Batir A, Krack P, Pollak P, Berger F. Therapeutic electrical stimulation of the central nervous system. C R Biol. 2005;328:177–186. doi: 10.1016/j.crvi.2004.10.011. [DOI] [PubMed] [Google Scholar]
- Eagle DM, Baunez C. Is there an inhibitory-response-control system in the rat? Evidence from anatomical and pharmacological studies of behavioral inhibition. Neurosci Biobehav Rev. 2010;34:50–72. doi: 10.1016/j.neubiorev.2009.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen MX, Schoene-Bake JC, Elger CE, Weber B. Connectivity-based segregation of the human striatum predicts personality characteristics. Nat Neurosci. 2009;12:32–34. doi: 10.1038/nn.2228. [DOI] [PubMed] [Google Scholar]
- Bernard JF, Carroue J, Besson JM. Efferent projections from the external parabrachial area to the forebrain: a Phaseolus vulgaris leucoagglutinin study in the rat. Neurosci Lett. 1991;122:257–260. doi: 10.1016/0304-3940(91)90872-Q. [DOI] [PubMed] [Google Scholar]
- Hodge CJ Jr, Apkarian AV. The spinothalamic tract. Crit Rev Neurobiol. 1990;5:363–397. [PubMed] [Google Scholar]