Abstract
Background.
Although life tables provide a basis for estimating remaining life by age, gender, and race, these tables do not consider clinical characteristics or functional status, which can lead to wide variations in remaining years. Inclusion of functional status may permit more precise prognostic estimates of life expectancy and proportion of time in various functional states.
Methods.
We used longitudinal data from the Established Populations for Epidemiologic Studies of the Elderly to determine transition probabilities between three functional states (independent in activities of daily living [ADL] and mobility, dependent in mobility but independent in ADL, and dependent in ADL) and death. These were used to estimate total life expectancy and life expectancy in each functional state.
Results.
In general, the largest proportion of remaining life expectancy was spent in the persons’ baseline functional status category. Persons younger than 80 years with dependencies, however, spend substantial proportions of their remaining years in a better functional status category, and mobility-disabled 70-year-old persons spend the greatest part of their life expectancy in the independent functional state. Functional status has a dramatic impact on life expectancy. For example, 75-year-old men and women without limitations have life expectancies 5 years longer than those with ADL limitation and more than 1 year longer than those limited in mobility. The life expectancy of an ADL-disabled 75-year-old is similar to that of an 85-year-old independent person; thus, the impact of the disability approximates being 10 years older with much more of the remaining life spent disabled.
Conclusions.
Both ADL and mobility disability result in diminished survival and more of that survival period spent in disabled states.
Keywords: Prognosis, Life expectancy, Functional status
LIFE expectancy, the average number of years of life remaining, is an important concept in clinical, policy, and personal planning. The most commonly reported life expectancy is from birth, which was 77.7 years for the United States in 2006 (1), but life expectancy can be calculated for people of any age and sociodemographic description. These calculations assume that death rates at future ages will be the same as the rates for people of that age today, an assumption that is more reasonable for elderly people than infants.
Age has the most important effect on life expectancy, but gender and ethnicity are strong influences. For example, in 2005, the life expectancies for a 65-year-old white woman and black man in the United States were 20.0 and 15.2 years, respectively. In contrast, the life expectancies for a 75-year-old white woman and black man were 12.8 and 10.0 years, respectively (1). Even within a specific sociodemographic group, survival may vary greatly. For example, an 85-year-old man has a 75% chance of surviving 2 years but only a 25% chance of living 9 years (2).
Although such estimates based on age, gender, and ethnicity are valuable, they do not convey the full story about life expectancy in older persons. Standard life tables do not consider clinical characteristics or functional status, which have large impacts on remaining years. Because self-reported functional impairment is strongly linked to subsequent mortality in diverse populations (3–5), life expectancy tables that consider this construct can be particularly useful for older persons, who are much more diverse in functional status than are younger persons (6).
One approach to incorporating functional status uses active life expectancy, which is the remaining life free of disability in activities of daily living (ADL) (7). Community-based estimates of active life expectancy have been generated (8) and used to explore the influence of socioeconomic status on life expectancy (9) and to examine costs of transitioning to dependency (10). Although this two-level classification (active or disabled) can provide both estimates of the duration and functional status of the remaining years of life, it is limited by the relative infrequency of any dependency in ADL function—fewer than 9%, even among those 75 years and older (1). In the previous studies, we have shown that simple mobility questions (ability to walk half a mile and climb a flight of stairs) can identify a much larger proportion of the elderly population with functional limitation and provide further prognostic information on survival (11) and hospital utilization (12). By incorporating a third level of functional status (mobility impairment) in our models, we can generate more precise prognostic estimates of life expectancy and proportion of time in various functional states.
In this study, we used three sites from the Established Populations for Epidemiologic Studies of the Elderly (EPESE) beginning with the sixth follow-up wave (1988) to generate life expectancies for older persons based on three self-reported functional states as well as age and gender.
METHODS
The EPESE was initiated in 1981 and follow-up continued through 1992 (13). Our analysis utilized data from the original sites of the EPESE study–—East Boston, Iowa and Washington Counties in East Central Iowa, and New Haven. The sampling frame for each site differed. East Boston employed a total community census, whereas Iowa used a population list from the local area’s Agency on Aging and a special census conducted by the investigators; both these sites attempted to recruit all enumerated persons 65 years of age or older. New Haven conducted a stratified cluster sampling of three different types of residents: those dwelling in public housing, private housing that is age-restricted to elderly, and private community housing and apartments that is age-restricted to elderly. Participation rates in the baseline EPESE survey in 1981–1982 ranged from 80% to 85% across sites. At the initial baseline interview, there were 10,294 participants aged 65 and older. Follow-ups were conducted at approximately 1-year intervals. Information on vital status came from obituaries, contact with proxies, and the National Death Index.
At each of the follow-ups, complete self-report functional status data were collected. We used the fifth through seventh waves as the inception points for the mortality analysis. By the time of the fifth follow-up, 3,029 participants had died, were lost to follow-up, or refused interview (7,265 remained available for analysis). Similarly, by the time of the sixth follow-up, 3,727 had died, were lost to follow-up, or refused interview (6,567 remained available for analysis). By the seventh follow-up, which did not include East Boston, the sample dropped by 6,362 (3,932 remained available for analysis). Combining the participants remaining at each of the three waves gave a sample of 17,764 person-years for the mortality component of the analysis.
We used transitions between the fifth and sixth waves and between the sixth and seventh waves for subsequent analysis of functional decline. There were 6,248 participants interviewed in both the fifth and the sixth waves and 3,700 interviewed in both the sixth and the seventh waves. This provided a sample of 9,948 for the functional decline component of the analysis.
Measures of disability
Self-reported functional status was measured using selected ADL (14) and mobility-related functional tasks (15). ADL included self-reports of bathing, transferring from bed to chair, dressing, eating, and using the toilet. We dichotomized these variables as being “unable to do or requiring human help” (dependent) versus “able without help” (independent). Mobility-related disability was defined as in a previous EPESE report (16) as two items from the Rosow–Breslau scale: inability to walk half a mile and/or walk up and down stairs to the second floor without help. Reporting inability to perform either of these tasks resulted in a classification of “mobility disabled.”
We established a three-level hierarchical scale for self-reported functional status that included the following:
(A) independent in mobility and all ADLs (58%),
(B) dependent in mobility and independent in all ADLs (26%), and
(C) dependent in mobility and one or more ADLs (16%).
Slightly more than 2% of both the mortality and the functional decline samples were missing status data or could not be classified using this system. These participants were excluded from the analyses, leaving 17,354 cases who could be functionally classified and whose death status was known 1 year after the interview and 9,753 cases who could be functionally classified both before and after a 1-year follow-up.
Analysis of life expectancies by functional status
Using EPESE data, we created single-year increment–decrement life tables for men and women from age 70 to 91 using an approach similar to that of Branch and coworkers (7). In our tables, however, we divided living people of each age and gender into three categories (A, B, and C) by functional status. In each year, survivors transition from any functional state to that state or another or death based on estimated transition probabilities (a Markov process). In reality, the probability of recovery from disability is influenced by the duration of time in the disabled state, but we found results from more complicated models used in other data sets that included the prior year’s functional status as well as the current functional status similar to those of the simple multistage life tables presented here (17). So, at each age a, the people in state j , where i represents the initial states, j = A, B, C, dead represents the final state, N(a − 1)i represents the number of people in cell i in the prior year, and p is the transition probability. Because we only have 17,354 person-years for follow-up on death and 9,753 with follow-up observation on transitions, we smoothed the observed age-specific transition probabilities. The smoothed transition probabilities are estimated using exponential regression models of the form pijas = cijsexp(kij(a − 70)) for i = A, B, C; j = A, B, C, died; s = male or female; and a = age from 70 to 90. This functional form assumes that the probability of each type of transition increases or decreases by a constant percentage with each additional year of age. It fits the data well in this age range and for mortality represents the familiar Gompertz law (18). The kij represent Gompertz-like factors of increase with age. Initially, we estimated 18 equations, one for each possible transition and gender (other than staying in the same state). Inspection of the kij showed that their values fell into three groups: transitions to death, transitions to worse health states, and transition to better health states, so we pooled all these data and reestimated three equations to obtain three values, kbetter, kworse, and kdeath. In those three models, none of the interactions of specific transitions by age or gender with the overall k value were significant. Also the interaction of gender with functional category or age was never significant, and gender was only a significant predictor of transitions to death. We did not estimate the proportion staying in the same state (the most likely result) statistically but calculated it by subtracting the sum of the smoothed probabilities of transitions out of the state from 1.
Above the age of 90 years, our number of cases becomes small, and the increases in mortality with age are known to diminish (19). Accordingly, to represent life expectancy past 90 years, we added an increment based on functional category (5.15 years for women in Class A or B, 4 years for women in Class C, 4.6 years for men in Class A or B, and 2.5 years for men in Class C). The Class C life expectancies were chosen to reflect death rates at age 91, and the others were chosen so the weighted sum of life expectancy in the EPESE sample of those older than 90 years would be equal to national life expectancy at age 91 for that gender in 1989 (4.41 for women and 3.65 for men). We used these life tables to calculate remaining life expectancy in each category for each combination of gender, age, and initial functional status.
RESULTS
Sociodemographic characteristics of the EPESE sample at the inception (1987–1989) for this analysis were mean age, 79.6 years; percentage female, 65.4; percentage African American, 6.0; percentage with fewer than 9 years of education, 42.2; and percentage with more than high school education, 15.7.
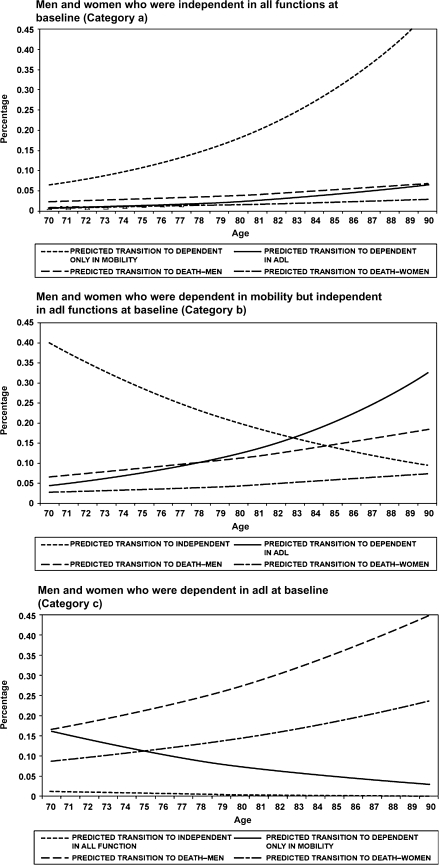
Figure 1 displays smoothed transition probabilities per year according to age and stratified by functional status at the beginning of each year. At each age, the probabilities of transition to different functional status are the same for men and women, but men have a death rate more than twice that of women. Transitions to better health states declined at 7% per year of age, transitions to worse health states increased by 10% a year with age, and transitions to death increased by 5% a year with age within each initial category. For example, in Figure 1, panel B, those dependent in mobility at baseline transition to ADL dependency during the next year at a rate of 4.5% at age 70, but this transition rate is approximately 32% at age 90. Transitions to death follow the same pattern, whereas transitions to independent function are lower with advancing age. In particular, transitions away from ADL dependency are quite unusual for older people in these data (Figure 1, panel C).
Figure 1.
Transition probabilities per year by age and beginning functional status.
In Table 1, we present life expectancy overall and in each functional state for persons at age 70, 75, 80, and 85 by gender and initial functional status. Compared with the functionally independent, total life expectancy for men and women of all ages in the table who are mobility disabled is approximately 1 year less (eg, 16.7 vs 15.7 years for 70-year-old women). People aged 70 years with ADL dependencies lose four more years (eg, 15.7 vs 11.5 years for 70-year-old women), and older people with ADL dependencies lose an additional 2–3 years. In all but one case, the largest proportion of life expectancy will be spent in the person’s baseline functional status category. Mobility-limited 70-year-olds tend to recover and spend more time in independence, and mobility-limited 75-year-olds also spend considerable time in independence. By contrast, older men and women with ADL dependency spend little time in better functional states.
Table 1.
Life Expectancy (years) in Various States of Functional Health According to Age, Gender, and Initial Functional Status Using 1988–1990 Established Populations for Epidemiologic Studies of the Elderly Data
| Age | Initial Functional Category | Life Expectancy in Years in Each Functional Status |
|||||||
| Women |
Men |
||||||||
| Independent Years | Mobility-Disabled Years | ADL-Disabled Years | Total Years | Independent Years | Mobility-Disabled Years | ADL-Disabled Years | Total Years | ||
| 70 | Independent | 10.0 | 4.0 | 2.7 | 16.7 | 8.5 | 2.6 | 1.0 | 12.1 |
| Mobility disabled | 7.3 | 5.6 | 2.8 | 15.7 | 5.6 | 4.1 | 1.1 | 10.7 | |
| ADL disabled | 3.0 | 2.9 | 5.6 | 11.5 | 1.6 | 1.5 | 3.4 | 6.5 | |
| 75 | Independent | 7.0 | 3.6 | 2.6 | 13.2 | 6.0 | 2.4 | 1.0 | 9.4 |
| Mobility disabled | 4.0 | 5.2 | 2.8 | 12.0 | 2.9 | 3.8 | 1.1 | 7.9 | |
| ADL disabled | 1.1 | 1.8 | 5.3 | 8.2 | 0.5 | 0.8 | 3.1 | 4.4 | |
| 80 | Independent | 4.7 | 3.2 | 2.4 | 10.3 | 4.1 | 2.2 | 0.9 | 7.2 |
| Mobility disabled | 2.0 | 4.4 | 2.7 | 9.0 | 1.4 | 3.3 | 1.0 | 5.7 | |
| ADL disabled | 0.4 | 1.0 | 4.7 | 6.0 | 0.2 | 0.4 | 2.6 | 3.1 | |
| 85 | Independent | 3.3 | 2.9 | 1.8 | 8.0 | 2.9 | 2.1 | 0.7 | 5.8 |
| Mobility disabled | 1.0 | 3.6 | 2.3 | 6.9 | 0.7 | 2.8 | 0.9 | 4.4 | |
| ADL disabled | 0.1 | 0.5 | 4.0 | 4.6 | 0.0 | 0.2 | 2.1 | 2.3 | |
Note: ADL = activities of daily living.
DISCUSSION
Including functional status can sharpen estimates of life expectancy compared with those based solely on age and gender. Older persons have wide variations in functional status, and this study confirms and extends previous findings that functional status has a major effect on life expectancy (7,9,18). At any given age, people with worse functional status have higher annual mortality. However, reliance on a one-time assessment of functional status neglects the potential for improvement or worsening. To calculate life expectancy accurately requires models that track transitions between functional states over time. Using such models, we showed, for example, that both 75-year-old men and women without limitations have life expectancy 5 years longer than those with ADL limitations and a little more than 1 year longer than those limited only in mobility. These large differences in life expectancy can be interpreted by noting that an ADL-disabled 75-year-old woman has a life expectancy of 8.2 years, which approximates that of an 85-year-old independent woman. The impact of the disability is akin to being 10 years older for women. Moreover, the situation of the ADL-disabled 75-year-old is worse because she will be disabled in most of her remaining years (5.3 years) compared with only 1.8 ADL-disabled years for the independent 85-year-old woman. The equivalent age offset of disability for men is even greater.
Most previous models that have incorporated functional status to generate life expectancy have relied on disabilities in ADL (6–8), which are rare among community-dwelling older persons (1). As a result, the vast majority of persons who are independent in ADLs have been considered as a homogeneous group. In fact, the survival of these independent persons varies considerably based on self-reported mobility and performance-based measures of function (9). More recently, Lubitz and coworkers (20) used Medicare Current Beneficiary Survey transition probabilities between five functional states to estimate life expectancy and lifetime costs at age 70. In this study, we have built upon this prior research and used two simple questions about mobility to better classify the older population into three groups based on functional status. Including transitions in functional status in a model also allowed us to predict how much of the remaining years of life will be spent in each of three functional status categories—independent, dependent in mobility but independent in ADL, and dependent in ADL.
We have also extended the findings of Lubitz and coworkers to persons aged 70–85 years. Although most remaining years are predicted to be spent in the same functional status as the baseline state, for many subgroups the time spent in other functional states will be considerable. Roughly half of the remaining lifetime of women starting without limitations will be spent with at least mobility limitations. However, functioning often improves, particularly among younger seniors. For example, 70-year-old people who are dependent in mobility on average spend about half of their expected remaining life in a completely independent functional status.
Other approaches to estimating prognosis (Table 2) include a variety of clinical measures but provide only probabilities of surviving for a defined numbers of years (eg, percentage chance of surviving 2 or 4 years), which may be less comprehensible to clinicians and patients. The time frame may also be too short to be clinically meaningful. For example, the median life expectancy for all race and sex groups of 7 5-year-old Americans in 2005 (10.0–12.8 years) (1) greatly exceeds the time frame of all the prognostic indices in Table 2. Moreover, many of these prediction rules include variables that are not commonly measured in clinical practice (eg, timed chair stands, gait speed, grip strength, lack of energy).
Table 2.
Approaches to Prognostication
| Name of Prognostic Tool | Population | Variables | Outcomes | Validity/Accuracy |
| Life tables (2,6) | General | • Age | Life expectancy | N/A |
| • Gender | ||||
| Vulnerable Elders Survey-13 (21,22) | Community based ≥65 y | • Age | 2- and 4.5-y mortality or decline in function | AUC 0.72–0.83 |
| • Self-rated health | ||||
| • Limitations in physical capability | ||||
| • Functional limitations | ||||
| Cardiovascular Health Study (23) | Community based ≥65 y | • Increasing age | 5-y mortality | Similar findings in validation sample |
| • Male sex | ||||
| • Income <$50,000/y, low weight | ||||
| • Lack of moderate or vigorous exercise | ||||
| • Smoking for more than 50 pack-years | ||||
| • High brachial and low tibial systolic blood pressure | ||||
| • Diuretic use by those without hypertension or congestive heart failure | ||||
| • Elevated fasting glucose level | ||||
| • Low albumin level | ||||
| • Elevated creatinine level | ||||
| • Low forced vital capacity | ||||
| • Aortic stenosis and abnormal left ventricular ejection fraction | ||||
| • Major electrocardiographic abnormality | ||||
| • Stenosis of internal carotid artery | ||||
| • Congestive heart failure | ||||
| • Difficulty in any IADL | ||||
| • Low cognitive function by digit symbol substitution test score | ||||
| Health and Retirement Study (24) | Population based ≥50 y | • Age | 4-y mortality | AUC 0.84 (derivation), AUC 0.82 (validation) |
| • Male gender | ||||
| • Diabetes | ||||
| • Cancer | ||||
| • Lung diseases | ||||
| • Heart failure | ||||
| • Current tobacco use | ||||
| • Body mass index | ||||
| • Bathing | ||||
| • Walking several blocks | ||||
| • Managing money | ||||
| • Pushing large objects | ||||
| Frailty Index (25) | Community based ≥65 y | • Unintentional weight loss | 5-y mortality | |
| • Weakness (grip strength) | ||||
| • Poor energy | ||||
| • Slow walk speed | ||||
| • Low physical activity | ||||
| PACE Study (26) | Elderly people who meet criteria for nursing home placement | • Age | 1- and 3-y mortality | AUC 0.66 (derivation), AUC 0.69 (validation) |
| • Male gender | ||||
| • Dependence in toileting | ||||
| • Dependence in dressing | ||||
| • Full dependence | ||||
| • Malignant neoplasm | ||||
| • Congestive heart failure | ||||
| • Chronic obstructive pulmonary disease | ||||
| • Renal insufficiency | ||||
| Asset and Health Dynamics Among the Oldest Old Study (27) | General age ≥70 y | • Age | 2-y mortality | AUC 0.76 (derivation), AUC 0.70 (validation) |
| • Male gender | ||||
| • Dependence in bathing | ||||
| • Dependence in shopping | ||||
| • Dependence in walking several blocks | ||||
| • Difficulty pulling or pushing heavy objects | ||||
| Established Populations for Epidemiological Studies (10) | Community-dwelling aged ≥71 y | • Activities of daily living | 4-y mortality | N/A |
| • Self-reported mobility | ||||
| • Balance testing | ||||
| • 8-ft walk | ||||
| • Rising from a chair five times | ||||
| Osteoporotic Fractures in Men Study (28) | Community-dwelling men aged ≥67 y | • Unintentional weight loss | 3.2-y (average follow-up) mortality | AUC 0.71 |
| • Inability to rise from a chair five times | ||||
| • Poor energy | ||||
| Conselice Study of Brain Ageing (29) | Community-dwelling aged ≥65 y | • Age | 3.8-y (average follow-up) mortality | |
| • Male gender | ||||
| • Physical inactivity | ||||
| • Use of ≥3 drugs | ||||
| • Sensory deficits | ||||
| • Calf circumference <31 cm | ||||
| • IADL disability | ||||
| • Poor gait and balance test | ||||
| • Pessimism about health |
Note: N/A = not applicable; AUC = area under (receiver-operating) curve (c-statistic); IDAL = instrumental activity of daily living.
These findings must be interpreted in the context of the study’s strengths and limitations. We chose the EPESE data set for this analysis because of the data elements that were available and the length of follow-up. Although EPESE included a large and geographically diverse sample, it was confined to three communities where different sampling strategies were used and EPESE did not attempt to weight data to be representative of the general population. In addition, minorities were underrepresented compared with their distribution in the general population. As a result, we were unable to generate life expectancies by race. Moreover, in its recruitment and follow-up procedures, there may have been a slight selection bias toward healthier persons. However, compared with decennial U.S. life tables for 1989–1991 (30), life expectancies in our population differed little. Moreover, the relative effects of limitations are unlikely to be biased. We had fewer than 10,000 observations that could be used to estimate transition probabilities. We attempted to compensate for limitations in sample size (and small numbers in some transitional categories) by using techniques to smooth the observed age-specific transition probabilities. We were also limited to the data elements contained in EPESE, which did not include instrumental ADL (eg, shopping, cooking, managing finances) or difficulty with ADLs; both have been associated with increased risk of mortality (21,23,31). In addition, this life table approach does not consider shorter term variation in disability, including transient disability (32). By design, EPESE and most community-based surveys assess stable populations, and recovery that commonly occurs after acute illness (eg, hospitalization-associated ADL disability) is not captured. Finally, the EPESE data were collected in the late 1980s and early 1990s and life expectancy for the elderly population has increased since then (eg, by 1.5 years for those aged 65 years of age and by 1.1 years for those aged 75 years of age) (1). Accordingly, life expectancy in the table may be slightly shorter than if current data were available.
In summary, simple self-reported information on functional status can increase the precision of life expectancy estimates among older persons. Indeed, the overall survival when stratified by functional status can vary by 50% within a specific age and gender group. Moreover, in models that account for expected functional transitions, both ADL and mobility disability translate into diminished survival and more of that survival period spent in disabled states. Although the actual survival of an individual patient may differ substantially from predicted survival based on this more precise life table, having more precise evidence-based information about prognosis can be valuable in the clinical setting when considering whether to offer preventive services and other long-term strategies and to frame treatment discussions with patients.
FUNDING
Drs. E.K. and D.B.R. received support from the UCLA Older Americans Independence Center, NIH/NIA Grant P30-AG028748, and the content does not necessarily represent the official views of the National Institute on Aging or the National Institutes of Health (NIH). This study was supported in part by the Intramural Research Program, National Institutes on Aging, and NIH.
References
- 1.National Center for Health Statistics Health. United States, 2008 With Chartbook. Hyattsville, MD: 2009. http://www.cdc.gov/nchs/fastats/lifexpec.htm. Accessed July 9, 2009. [Google Scholar]
- 2.Arias E. United States life tables, 2004. Natl Vital Stat Rep. 2007;56(9):1–39. [PubMed] [Google Scholar]
- 3.Ferrucci L, Guralnik JM, Baroni A, Tesi G, Antonini E, Marchionni N. Value of combined assessment of physical health and functional status in community-dwelling aged: a prospective study in Florence, Italy. J Gerontol. 1991;46(2):M52–M56. doi: 10.1093/geronj/46.2.m52. [DOI] [PubMed] [Google Scholar]
- 4.Reuben DB, Rubenstein LV, Hirsch SH, Hays RD. The value of functional status as a predictor of mortality: results of a prospective study. Am J Med. 1992;93:663–669. doi: 10.1016/0002-9343(92)90200-u. [DOI] [PubMed] [Google Scholar]
- 5.Bernard SL, Kincade JE, Konrad TR, et al. Predicting mortality from community surveys of older adults: the importance of self-rated functional ability. J Gerontol Soc Sci. 1997;52:S155–S163. doi: 10.1093/geronb/52b.3.s155. [DOI] [PubMed] [Google Scholar]
- 6. Actuarial Publications, Social Security Online. http://www.ssa.gov/OACT/STATS/table4c6.html. Accessed July 6, 2009. [Google Scholar]
- 7.Katz S, Branch LG, Branson MH, Papsidero JA, Beck JC, Greer DS. Active life expectancy. N Engl J Med. 1983;309:1218–1224. doi: 10.1056/NEJM198311173092005. [DOI] [PubMed] [Google Scholar]
- 8.Branch LG, Guralnik JM, Foley DJ, et al. Active life expectancy for 10,000 Caucasian men and women in three communities. J Gerontol. 1991;56:M145–M150. doi: 10.1093/geronj/46.4.m145. [DOI] [PubMed] [Google Scholar]
- 9.Guralnik JM, Land KC, Blazer D, Fillenbaum G, Branch LG. Educational status and active life expectancy among older blacks and whites. N Engl J Med. 1993;329:110–116. doi: 10.1056/NEJM199307083290208. [DOI] [PubMed] [Google Scholar]
- 10.Guralnik JM, Alecxih L, Branch LG, Wiener JM. Medical and long-term care costs when older persons become more dependent. Am J Public Health. 2002;92(8):1244–1245. doi: 10.2105/ajph.92.8.1244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Reuben DB, Seeman TE, Keeler E, et al. Refining the categorization of physical functional status: the added value of combining self-reported and performance-based measures. J Gerontol Med Sci. 2004;59(10):M1056–M1061. doi: 10.1093/gerona/59.10.m1056. [DOI] [PubMed] [Google Scholar]
- 12.Reuben DB, Seeman TE, Keele E. The effect of self-reported and performance-based functional impairment on future hospital costs of community-dwelling older persons. Gerontologist. 2004;44(3):401–407. doi: 10.1093/geront/44.3.401. [DOI] [PubMed] [Google Scholar]
- 13.Cornoni-Huntley J, Brock DB, Ostfeld AM, editors. Established Populations for Epidemiologic Studies of the Elderly: Resource Data Book. Bethesda, MD: National Institute on Aging; 1986. NIH Publication No. 86-2443. [Google Scholar]
- 14.Katz S, Downs TD, Cash HR, Grotz RC. Progress in development of the index of ADL. Gerontologist. 1970;10:20–30. doi: 10.1093/geront/10.1_part_1.20. [DOI] [PubMed] [Google Scholar]
- 15.Rosow I, Breslau N. A Guttman health scale for the aged. J Gerontol. 1966;21:556–559. doi: 10.1093/geronj/21.4.556. [DOI] [PubMed] [Google Scholar]
- 16.Corti M, Guralnik JM, Salive ME, Sorkin JD. Serum albumin and physical disability as predictors of mortality in older persons. J Am Med Assoc. 1994;272:1036–1042. [PubMed] [Google Scholar]
- 17.Cai L, Schenker N, Lubitz J, Diehr P, Arnold A, Fried LP. Evaluation of a method for fitting a semi-Markov process model in the presence of left-censored spells using the Cardiovascular Health Study. Stat Med. 2008;27(26):5509–5524. doi: 10.1002/sim.3382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gompertz B. On the nature of the function expressive of the law of human mortality. Philos Trans R Soc Lond. 1825;155:513–585. doi: 10.1098/rstb.2014.0379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Manton KG, Stallard E, Woodbury MA, Dowd JE. Time-varying covariates in models of human mortality and aging: multidimensional generalizations of the Gompertz. J Gerontol. 1994;49:B169–B190. doi: 10.1093/geronj/49.4.b169. [DOI] [PubMed] [Google Scholar]
- 20.Lubitz J, Cai L, Kramarow E, Lentzner H. Health, life expectancy, and health care spending among the elderly. N Engl J Med. 2003;349(11):1048–1055. doi: 10.1056/NEJMsa020614. [DOI] [PubMed] [Google Scholar]
- 21.Saliba D, Elliott M, Rubenstein LZ, et al. The Vulnerable Elders Survey: a tool for identifying vulnerable older people in the community. J Am Geriatr Soc. 2001;49:1691–1699. doi: 10.1046/j.1532-5415.2001.49281.x. [DOI] [PubMed] [Google Scholar]
- 22.Min L, Yoon W, Mariano JD, et al. The Vulnerable Elders-13 Survey predicts 5-year functional decline and mortality outcomes among older ambulatory care patients. J Am Geriatr Soc. 2004;57:2070–2076. doi: 10.1111/j.1532-5415.2009.02497.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lee SJ, Lindquist K, Segal MR, Covinsky KE. Development and validation of a prognostic index for 4-year mortality in older adults. JAMA. 2006;295(7):801–808. doi: 10.1001/jama.295.7.801. [DOI] [PubMed] [Google Scholar]
- 24.Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56A:M146–M156. doi: 10.1093/gerona/56.3.m146. [DOI] [PubMed] [Google Scholar]
- 25.Carey EC, Covinsky KE, Lui LY, Eng C, Sands LP, Walter LC. Prediction of mortality in community-living frail elderly people with long-term care needs. J Am Geriatr Soc. 2008;56(1):68–75. doi: 10.1111/j.1532-5415.2007.01496.x. [DOI] [PubMed] [Google Scholar]
- 26.Carey EC, Walter LC, Lindquist K, Covinsky KE. Development and validation of a functional morbidity index to predict mortality in community-dwelling elders. J Gen Intern Med. 2004;19(10):1027–1033. doi: 10.1111/j.1525-1497.2004.40016.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ensrud KE, Ewing SK, Cawthon PM, et al. A comparison of frailty indexes for the prediction of falls, disability, fractures, and mortality in older men. J Am Geriatr Soc. 2009;57(3):492–498. doi: 10.1111/j.1532-5415.2009.02137.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ravaglia G, Forti P, Lucicesare A, Pisacane N, Rietti E, Patterson C. Development of an easy prognostic score for frailty outcomes in the aged. Age Ageing. 2008;37(2):161–166. doi: 10.1093/ageing/afm195. [DOI] [PubMed] [Google Scholar]
- 29.National Center for Health Statistics. US Decennial Life Tables for 1989–91. Hyattsville, MD: DHHS: 1997. DHHS Pub PHS 987-1150-1. [Google Scholar]
- 30.Gill TM, Robison JT, Tinetti ME. Difficulty and dependence: two components of the disability continuum among community-living older persons. Ann Intern Med. 1998;128:96–101. doi: 10.7326/0003-4819-128-2-199801150-00004. [DOI] [PubMed] [Google Scholar]
- 31.Fried LP, Kronmal RA, Newman AB, et al. Risk factors for 5-year mortality in older adults: the Cardiovascular Health Study. JAMA. 1998;279(8):585–592. doi: 10.1001/jama.279.8.585. [DOI] [PubMed] [Google Scholar]
- 32.Gill TM, Guo Z, Allore HG. Subtypes of disability in older persons over the course of nearly 8 years. J Am Geriatr Soc. 2008;56(3):436–443. doi: 10.1111/j.1532-5415.2007.01603.x. [DOI] [PMC free article] [PubMed] [Google Scholar]