Abstract
While senile plaques injure neurons focally, the functional response of astrocytes to Alzheimer’s disease pathology is unknown. Using multiphoton fluorescence lifetime imaging microscopy in vivo, we quantitatively imaged astrocytic calcium homeostasis in a mouse model of Alzheimer’s disease. Resting calcium was globally elevated in the astrocytic network, but was independent of proximity to individual plaques. Time lapse imaging revealed that calcium transients in astrocytes were more frequent, were synchronously coordinated across long distances, and were uncoupled from neuronal activity. Furthermore, rare intercellular calcium waves were observed, but only in mice with amyloid-β plaques, originating near plaques and spreading radially at least 200 µm. Thus, while neurotoxicity is observed near amyloid-β deposits, there exists a more general astrocyte-based network response to focal pathology.
Growing evidence supports the hypothesis that in Alzheimer’s disease (AD), synapses fail and dendritic spines are lost in the amyloid-β (Aβ) plaque micro-environment through a combination of changes to synaptic drive, calcium overload, and activation of calcium-dependent degenerative processes (1–4). Neurons, however, make up only part of the brain’s volume, with astrocytes making up the bulk of the remaining volume. Astrocytes form a structurally interconnected network that, in vitro, exhibit unique long-distance signaling properties that might be revealed in vivo only after pathological trauma. The idea that neural network dysfunction and degeneration fully mediates the memory loss in AD also does not reflect the growing in vivo evidence that astrocytes play an important role in cortical circuit function (5–7). In AD, pathological studies of human cases and mouse models have shown that astrocytes surround plaques and might play a critical role in Aβ deposition and clearance (8–10). Given the profound impact of Aβ deposition on nearby neuronal calcium homeostasis and synaptic function, it is reasonable to hypothesize that astrocyte networks would also be perturbed and might contribute to cortical dysfunction (11). We sought to test whether senile plaque deposition would similarly impact astrocyte calcium homeostasis or dynamic signaling in vivo in a mouse model of AD.
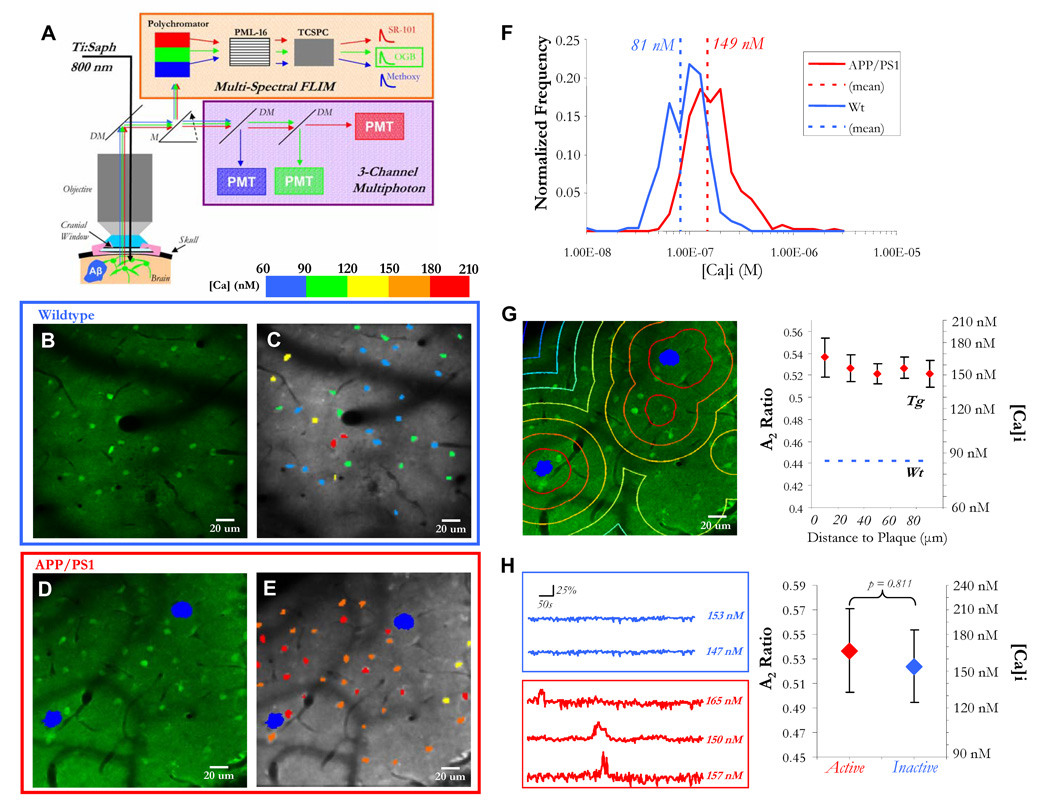
To answer these questions, we used multiphoton fluorescent lifetime imaging microscopy (FLIM) to measure resting calcium levels in astrocytes of live mice with cortical plaques (12). We multiplexed the fluorescent properties of a small molecule calcium dye, Oregon-Green BAPTA-1 AM (OGB), in the same experimental model and for the same group of cells (Fig. 1A); we used OGB both as a relative indicator of astrocytic activity (intensity) and as a quantitative measure of steady-state [Ca]i (lifetime). We used mice that express mutant human Aβ precursor protein (APP, swe) and mutant presenilin 1 (PS1, ΔE9) in neurons. These mutations lead to an increase in Aβ production and plaque deposition beginning at ~4.5 months of age (13, 14). In mice with plaques, resting [Ca]i in astrocytes was higher than in wildtype animals (Fig. 1B–F). The resting [Ca]i of astrocytes in wildtype mice was 81 nM +/− 3 nM whereas in transgenic mice the resting [Ca]i was 149 nM +/− 6 nM (p<0.05). We confirmed that the surrounding neuropil signal minimally contaminated the astrocyte [Ca]i (Fig. S2).
Figure 1. Resting calcium is globally elevated in astrocytic networks.
A) Multiphoton laser illumination simultaneously excited methoxy-XO4 (blue, amyloid-β), OGB (green, neurons and astrocytes), and SR-101 (red, astrocytes) through a cranial window. The resulting fluorescence emission was sent to either (1) a three-channel intensity-based PMT module or (2) a 16-channel multi-spectral FLIM detector. A single-photon counter (tcSPC) recorded fluorescence lifetime data . B–E) Fluorescence decay curves were fit with a calcium bound lifetime (2359 ps) and an unbound calcium lifetime (569 ps) for each pixel. The pixel data were averaged to obtain single- cell calcium levels, depicted with a calibrated colorbar (C,E). Astrocytes in APP/PS1 mice with cortical plaques (in blue, D–E), exhibited significantly higher levels of [Ca]i than in wildtype mice (B–C,F: p < 0.05, Student’s t-test, n = 241 cells in 3 mice (wt), n = 364 cells in 3 mice (Tg)). G) Astrocyte resting [Ca]i did not depend on proximity to a plaque (p = 0.9194, Kruskal-Wallis test, n > 25 cells for each distance group). H) There was no difference in resting calcium between cells that were active versus inactive (p = 0.811, Student’s t-test, n = 209 cells in 3 mice).
We next mapped the spatial distribution of astrocytes versus Aβ plaque location in 3-dimensions (Fig. S3). There was no effect of plaque proximity on resting [Ca]i in individual astrocytes (Fig. 1G, n > 25 cells per bin). It is important to note, however, that plaques deposit rapidly in these mice such that very few astrocytes were further than 100 µm away from a plaque. Because of the long integration times for FLIM (5–10 min per scan), it was possible that our astrocytic FLIM data was reflecting the increased time in the “active” (high-calcium) state rather than a change in baseline resting calcium. To test this, we co-registered FLIM data with spontaneous activity data to allow single-cell identification across imaging modalities. Spontaneously active cells did not have significantly different resting calcium than non-active cells (Fig. 1H, p = 0.811).
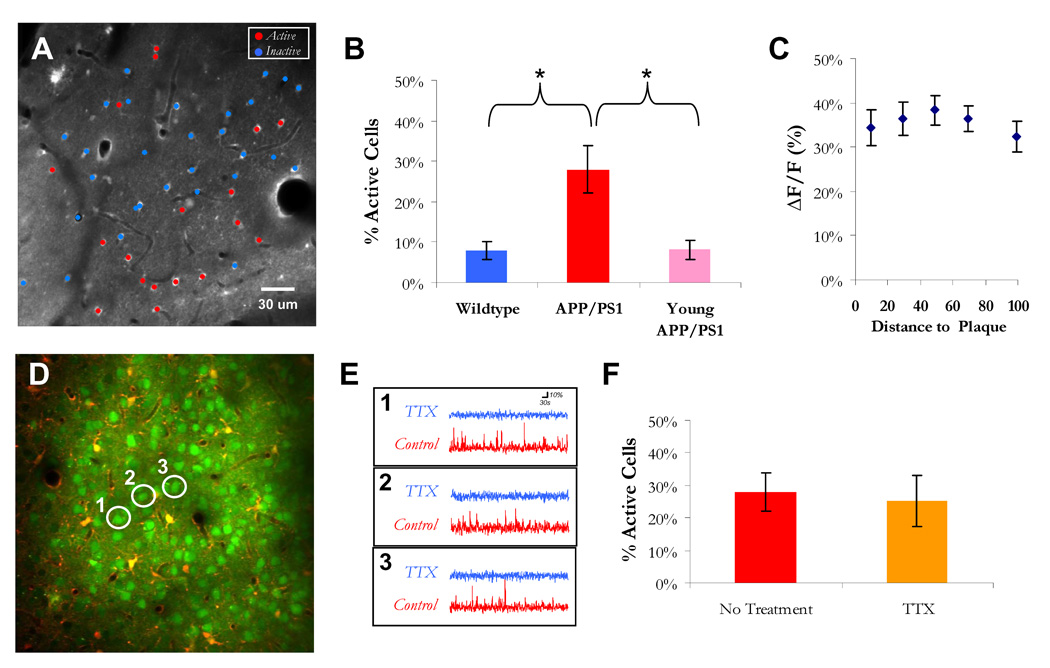
With time-lapse calcium imaging of OGB intensity, we measured spontaneous astrocytic activity. Astrocytes in adult APP/PS1 mice (6–8 mo.-old) with cortical plaques exhibited a significant increase in spontaneous activity (Fig. 2, Movie S1 and S2). 27.9 +/− 6.0 % of all astrocytes were active in APP/PS1 mice when compared with the relatively rare spontaneous events seen in wildtype mice (8.1 ± 2.3%, Fig. 2B, p < 0.05). APP/PS1 mutant mice did not show evidence of altered spontaneous activity before they have developed senile plaques (3–3.5 mo-old, Fig. 2B). Furthermore, the amplitude of the calcium signals was significantly higher in APP/PS1 mice (ΔF/F: 33.6 +/− 1.1%) when compared with wildtype mice (ΔF/F: 23.2 +/− 0.8%, p<0.001, Fig. S4). This change in astrocytic function was also independent of plaque proximity (Fig. 2C and Fig. S4)—again implicating a global astrocytic response to plaque deposition.
Figure 2. Neuron-independent increase in spontaneous activity throughout astrocytic network.
A) Cell activity map overlaid on multiphoton image of astrocytes. B) There were more spontaneously active cells in mice with cortical plaques (*, p < 0.05, Kruskal-Wallis with Tukey-Cramer post-hoc, n = 15 mice, 8 APP/PS1 with plaques, 4 non-transgenic and 3 APP/PS1 before plaque deposition). C) The amplitude of the [Ca]i transients (n = 160 astrocytes) did not depend on proximity to plaque (5 groups, p = 0.9178, Kruskal-Wallis test). D) Multiphoton image of neurons and astrocytes in an APP/PS1 transgenic mouse with cortical plaques. Three neurons are highlighted to show their spontaneous activity traces before and after application of 1 uM TTX in (E). F) There was no reduction in the percentage of active astrocytes in the presence of TTX (27.9 +/− 6.0% in control (n=8 mice, 1,241 astrocytes) vs. 25.4 +/− 7.8% under TTX (n = 4 mice, 818 astrocytes), p = 0.8081, Mann-Whitney U-test).
In this mouse model, astrocytes do not produce Aβ implicating a non-cell autonomous mechanism behind the increased activity. Hyperactive neurons in the plaque penumbra (2) might be responsible by inducing increased activity in functionally connected astrocytes. To test this, we blocked neuronal activity with the sodium-channel blocker, TTX (Fig. 2D–F and Fig. S5). Under these conditions, astrocytic activity persisted (Fig. 2F). Thus, the increase in astrocyte activity does not derive from neuronal hyperactivity near Aβ deposits supporting the hypothesis that Aβ interacts directly with the astrocyte network.
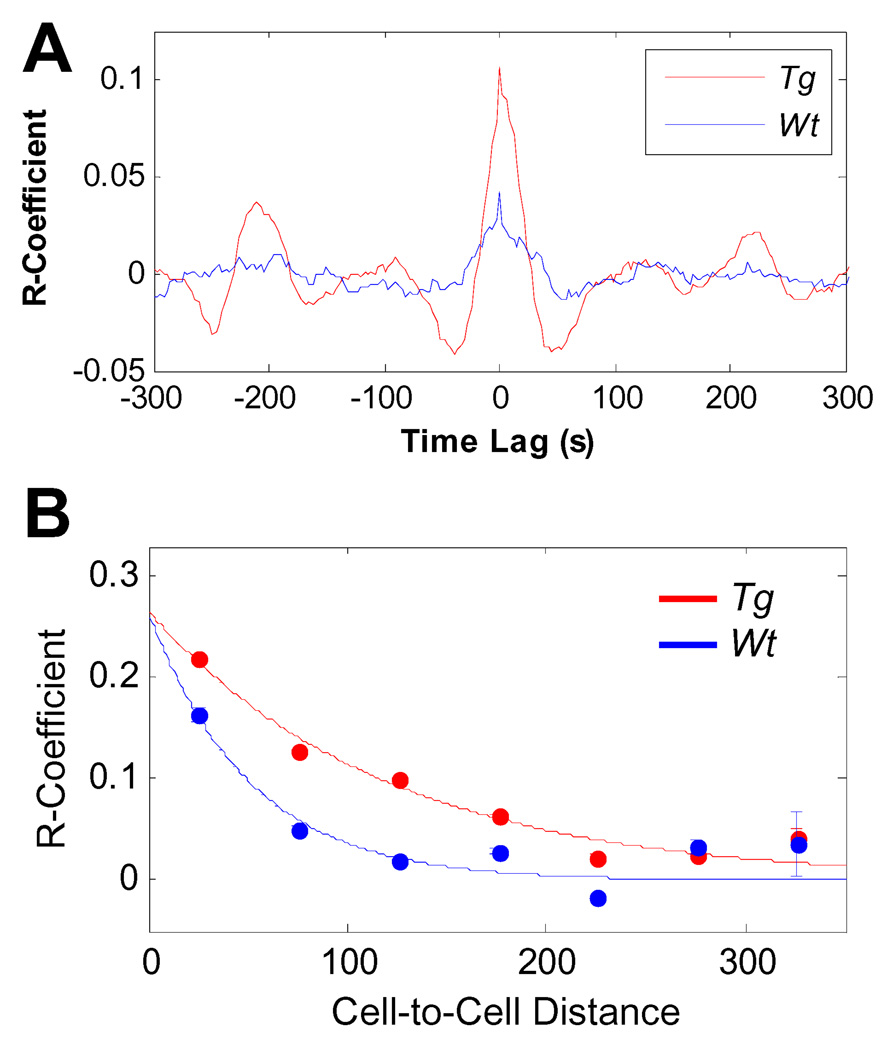
Astrocytes play a local role in supporting neuronal activity and in mirroring neuronal responses to sensory stimuli (6). There is little in vivo evidence supporting the hypothesis that astrocytes form long-range signaling networks (7, 15). To test this in the AD mouse model, we measured the correlation in activity for all active astrocyte cell-pairs in a given imaging field. Two cells that were synchronously active would have a robust central peak in the cross correlogram. There was a significant increase in the central peak of the correlogram for the transgenic astrocyte cell-pairs (Fig. 3A and Fig. S6).
Figure 3. Spatiotemporal synchrony of astrocytic calcium signaling in APP/PS1 mice.
A) The mean cross-correlogram for all cell pairs (excluding autocorrelations) in transgenic and non- transgenic mice. In APP/PS1 mice there was an increase in the probability that two cells had coordinated activity (n = 3 mice for APP/PS1 and Wt, n = 1,257 cell pairs in transgenic and n = 471 cell pairs in Wt). B) Cell-pair distance (x-axis) versus Correlation coefficient (y-axis). Data were fit to a mono-exponential. In transgenic mice (red), cell-pairs exhibited significantly correlated activity at distances up to 200 µm (p < 0.01, Kruskal-Wallis test with Tukey-Cramer post-hoc) whereas in wildtype mice (blue), cell-pairs were not correlated at inter-cellular distances greater than 50 µm (p = 0.65, Kruskal-Wallis with Tukey-Cramer post-hoc).
We next compared the average correlation coefficient as a function of the pair-wise distance of the two cells (Fig. 3B) and modeled the relationship with distance as an exponential function. In wildtype mice, activity was correlated only when cells were within 50 µm of each other (p < 0.05, Kruskal-Wallis test with Tukey-Cramer post-hoc). In transgenic mice there was increased correlated activity when compared to wildtype (p < 0.001, Mann-Whitney U-Test) that persisted at distances beyond 50 µm (p<0.01, Kruskal-Wallis test with Tukey-Cramer post-hoc). Even at cell-to-cell distances up to 200 µm there was a significant elevation in correlated activity compared to wildtype. This can be further seen when comparing the exponential fits—the decay constant was 2.4X longer in transgenic (−0.020) than in wildtype (−0.008).
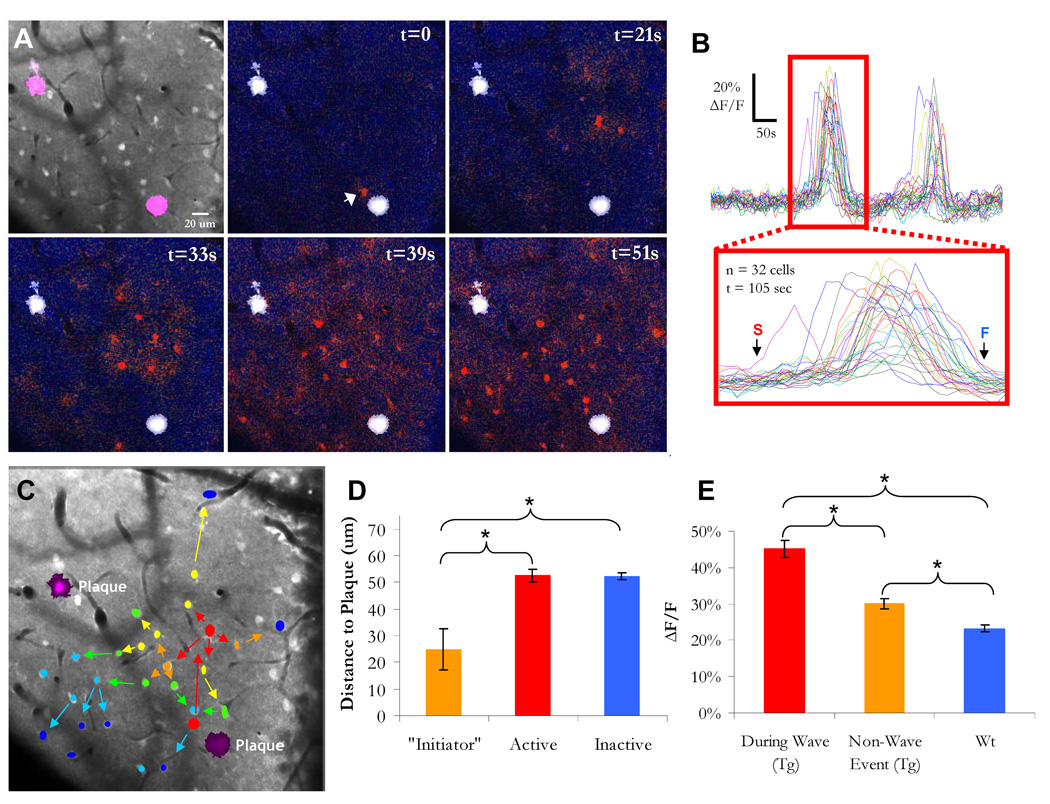
Thus astrocytes in mice with cortical plaques exhibit functional coordination of their intracellular calcium signals at long distances. Indeed, we observed intercellular calcium waves (ICWs) in 6 out of 8 transgenic mice but never in wildtype mice (Fig. 4, n = 8 transgenic and 5 non-transgenic, p < 0.05, Fisher Exact Test). These waves traveled 196 +/− 41 µm at a speed of 22.7 +/− 6.4 um/sec, similar to that observed in cells in culture (16). The “initiator” astrocyte was located 24.8 +/− 7.8 um from the nearest senile plaque—a proximity that has been previously associated with increased synapto- and neuro-toxicity (3, 4). This was significantly closer than the average distance of an astrocyte to the nearest plaque (Fig. 4D, active = 52.5 +/− 2.3 um, inactive = 52.3 +/− 1.2 um, p < 0.05). Calcium transients during an ICW (ΔF/F: 45.2 +/− 2.4%) were higher in magnitude than a typical spontaneous event in transgenic mice (Fig. 4E, ΔF/F: 30.1 +/− 1.5%, p <0.01) suggesting that this signal was different from that spread by non-wave activity.
Figure 4. Intercellular calcium waves in mice with cortical plaques.
A,B) A time-lapse ΔF/F image filmstrip and data of calcium activity in an APP/PS1 transgenic mouse. The white arrow in the second panel points to the “initiator” astrocyte and the sequential panels show the propagation of the wave. C) A summary of (A) in which color denotes temporal sequence and arrows denote spatial propagation. D) Astrocytes that “initiate” ICWs were closer to senile plaques than the average active or inactive astrocyte (*, p < 0.05, Kruskal-Wallis with Tukey-Cramer post-hoc). E) There was a significant increase in the amplitude of the calcium signal during a wave (* = p < 0.001, ANOVA with Tukey- Cramer post-hoc, n = 47 cells in Tg (wave), n = 156 cells in Tg (non-wave), n = 168 in Wt).
Astrocytes, in normal conditions, can have highly localized and independent responses (6). In the AD model, astrocytes exhibited network-wide elevations in resting calcium and increased network-level functional activity. Thus, it appears that astrocytes may represent functionally adaptive cells that play distinct roles in health versus disease. The astrocytic network amplified the effects of focal amyloid deposition across a larger cortical network landscape, perhaps contributing to the global alterations in cortical function, and possibly the memory disorders seen in AD. One mechanism underlining this amplification effect is the propagation of intercellular calcium waves. The observed ICWs typically began in the local plaque micro-environment suggesting that plaques or plaque-associated bioactive species might induce these powerful calcium waves that travel across the cortex. Since the initial discovery of ICWs nearly two decades ago (17), their existence in culture and in acute slices has never been confirmed in vivo (16, 18). Their propagation, through gap junctions (19) or via ATP (20, 21), has been postulated to signal the existence of a pathological insult(16, 18). Our data support this hypothesis since plaque deposition has been linked extensively to neuronal trauma (1, 4, 22).
The increased astrocyte activity cannot be explained by a simple coupling mechanism with neuronal activity. First, neuronal calcium homeostasis is most severely impaired near senile plaques (4) whereas here resting calcium was globally elevated in astrocytes. Second, neurons exhibit a pronounced hyperactivity near plaques (2), while here astrocytes were more active both near and far from plaques. Third, abolishing neuronal activity had no measurable effect on astrocytic calcium oscillations. Thus, whereas senile plaque deposition induces local synapto- and neuro-toxicity, the same Aβ deposits might catalyze astrocytic intra- and inter-cellular signaling events. This idea is supported, in part, by evidence that cultured astrocytes exhibit elevated calcium upon application of Aβ but are surprisingly resistant to cell death (unlike neurons) (23). An important question that remains unanswered is whether modulating astrocytic calcium signaling, via genetic (24) or pharmacological manipulations, will result in dynamic changes in amyloid accumulation (10) or alter neuronal network activity associated with behavioral impairments.
Supplementary Material
References and Notes
- 1.Meyer-Luehmann M, et al. Nature. 2008 Feb 7;451:720. doi: 10.1038/nature06616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Busche MA, et al. Science. 2008 Sep 19;321:1686. doi: 10.1126/science.1162844. [DOI] [PubMed] [Google Scholar]
- 3.Spires TL, et al. J Neurosci. 2005 Aug 3;25:7278. doi: 10.1523/JNEUROSCI.1879-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kuchibhotla KV, et al. Neuron. 2008 Jul 31;59:214. doi: 10.1016/j.neuron.2008.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang X, et al. Nat Neurosci. 2006 Jun;9:816. doi: 10.1038/nn1703. [DOI] [PubMed] [Google Scholar]
- 6.Schummers J, Yu H, Sur M. Science. 2008 Jun 20;320:1638. doi: 10.1126/science.1156120. [DOI] [PubMed] [Google Scholar]
- 7.Hirase H, Qian L, Bartho P, Buzsaki G. PLoS Biol. 2004 Apr;2:E96. doi: 10.1371/journal.pbio.0020096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Maragakis NJ, Rothstein JD. Nat Clin Pract Neurol. 2006 Dec;2:679. doi: 10.1038/ncpneuro0355. [DOI] [PubMed] [Google Scholar]
- 9.Wegiel J, et al. Neurobiol Aging. 2001 Jan–Feb;22:49. doi: 10.1016/s0197-4580(00)00181-0. [DOI] [PubMed] [Google Scholar]
- 10.Wyss-Coray T, et al. Nat Med. 2003 Apr;9:453. doi: 10.1038/nm838. [DOI] [PubMed] [Google Scholar]
- 11.Takano T, Han X, Deane R, Zlokovic B, Nedergaard M. Ann N Y Acad Sci. 2007 Feb;1097:40. doi: 10.1196/annals.1379.004. [DOI] [PubMed] [Google Scholar]
- 12.Wilms CD, Schmidt H, Eilers J. Cell Calcium. 2006 Jul;40:73. doi: 10.1016/j.ceca.2006.03.006. [DOI] [PubMed] [Google Scholar]
- 13.Garcia-Alloza M, et al. Neurobiol Dis. 2006 Dec;24:516. doi: 10.1016/j.nbd.2006.08.017. [DOI] [PubMed] [Google Scholar]
- 14.Borchelt DR, et al. Neuron. 1997 Oct;19:939. doi: 10.1016/s0896-6273(00)80974-5. [DOI] [PubMed] [Google Scholar]
- 15.Agulhon C, et al. Neuron. 2008 Sep 25;59:932. doi: 10.1016/j.neuron.2008.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Scemes E, Giaume C. Glia. 2006 Nov 15;54:716. doi: 10.1002/glia.20374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cornell-Bell AH, Finkbeiner SM, Cooper MS, Smith SJ. Science. 1990 Jan 26;247:470. doi: 10.1126/science.1967852. [DOI] [PubMed] [Google Scholar]
- 18.Fiacco TA, McCarthy KD. Glia. 2006 Nov 15;54:676. doi: 10.1002/glia.20396. [DOI] [PubMed] [Google Scholar]
- 19.Boitano S, Dirksen ER, Sanderson MJ. Science. 1992 Oct 9;258:292. doi: 10.1126/science.1411526. [DOI] [PubMed] [Google Scholar]
- 20.Cotrina ML, Lin JH, Lopez-Garcia JC, Naus CC, Nedergaard M. J Neurosci. 2000 Apr 15;20:2835. doi: 10.1523/JNEUROSCI.20-08-02835.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Guthrie PB, et al. J Neurosci. 1999 Jan 15;19:520. doi: 10.1523/JNEUROSCI.19-02-00520.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Garcia-Alloza M, Dodwell SA, Meyer-Luehmann M, Hyman BT, Bacskai BJ. J Neuropathol Exp Neurol. 2006 Nov;65:1082. doi: 10.1097/01.jnen.0000240468.12543.af. [DOI] [PubMed] [Google Scholar]
- 23.Abramov AY, Canevari L, Duchen MR. J Neurosci. 2003 Jun 15;23:5088. doi: 10.1523/JNEUROSCI.23-12-05088.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Petravicz J, Fiacco TA, McCarthy KD. J Neurosci. 2008 May 7;28:4967. doi: 10.1523/JNEUROSCI.5572-07.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.We would like to thank K.O. Ohki and R.C. Reid for assistance with the MCBL technique. This work was supported by NIH EB000768 (BJB), AG08487 (BTH), and NIH NS580752 (KVK).
- 26.Supporting Online Materialwww.sciencemag.orgMaterials and MethodsFigs. S1–S6Movie S1, S2
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.