Abstract
OBJECTIVE
The objective of this study was to assess the risk of suicide attempts and suicides after initiation of antidepressant medication use by children and adolescents, for individual agents.
METHODS
We conducted a 9-year cohort study by using population-wide data from British Columbia. We identified new users of antidepressants who were 10 to 18 years of age with a recorded diagnosis of depression. Study outcomes were hospitalization attributable to intentional self-harm and suicide death.
RESULTS
Of 20 906 children who initiated antidepressant therapy, 16 774 (80%) had no previous antidepressant use. During the first year of use, we observed 266 attempted and 3 completed suicides, which yielded an event rate of 27.04 suicidal acts per 1000 person-years (95% confidence interval [CI]: 23.9–30.5 suicidal acts per 1000 person-years). There were no meaningful differences in the rate ratios (RRs) comparing fluoxetine with citalopram (RR: 0.97 [95% CI: 0.54–1.76]), fluvoxamine (RR: 1.05 [95% CI: 0.46–2.43]), paroxetine (RR: 0.80 [95% CI: 0.47–1.37]), and sertraline (RR: 1.02 [95% CI: 0.56–1.84]). Tricyclic agents showed risks similar to those of selective serotonin reuptake inhibitors (RR: 0.92 [95% CI: 0.43–2.00]).
CONCLUSION
Our finding of equal event rates among antidepressant agents supports the decision of the Food and Drug Administration to include all antidepressants in the black box warning regarding potentially increased suicidality risk for children and adolescents beginning use of antidepressants.
Keywords: antidepressant medications, fluoxetine, suicide, intentional self-harm, cohort study, epidemiology
WHAT'S KNOWN ON THIS SUBJECT: Antidepressants may be associated with increased risk of suicidality for children, but variations in risk among individual antidepressant agents are unknown.
WHAT THIS STUDY ADDS: This study found no significant variations in rates of suicidal acts among antidepressant agents, which supports the decision of the Food and Drug Administration to require a black box warning regarding potentially increased suicidality risk for all antidepressants.
In October 2004, the US Food and Drug Administration issued an advisory that antidepressants may be associated with increased risks of suicidal thoughts and behaviors among children and adolescents.1 These warnings were prompted by a meta-analysis of all available randomized trials of antidepressants in this age group, in which patients assigned randomly to receive antidepressants had nearly twice the rate of suicidal ideation or behavior, compared with those who received placebo.2 However, the interpretation of the findings of that meta-analysis is limited by a number of factors, including the brief duration of trials, few suicide attempts and almost no completed suicides, varying definitions of suicidal ideation, non-comparable doses, and heterogeneous patient populations.
Epidemiological studies of the safety of antidepressants in pediatric populations are very limited. Studies comparing antidepressant users with nonusers have generally suggested an increased risk of suicidal acts associated with antidepressant use,3–6 but these results could be caused by the channeling of antidepressant agents to children and adolescents who are more likely to attempt suicide, leading to intractable confounding by indication.7 Only 2 studies compared suicide risk across antidepressant agents,8,9 and questions remain regarding whether those studies had adequate statistical power or adequately controlled for prescribing biases caused by preferential avoidance of the use of tricyclic agents for patients at high risk for suicidality.
Although they raised important concerns, Food and Drug Administration meta-analyses and advisories have not provided patients, clinicians, or policymakers with adequate guidance for the treatment decisions they face. In the current study, we sought to address whether the putative link between antidepressants and suicidality applies equally to all antidepressant classes, agents, and durations of use or whether there are particular regimens with safety advantages that should be prescribed preferentially in pediatric and adolescent populations.
METHODS
Patients and Data Source
We conducted a cohort study of all British Columbia residents 10 to 18 years of age who initiated use of an antidepressant medication between January 1, 1997, and December 31, 2005. Children <10 years of age were excluded on the basis of the assumption that they would not attempt suicide.10,11 Initiation was defined as filling an antidepressant prescription without having filled one in the preceding year. We analyzed only the first treatment episode for each patient during the study period. We required evidence of depression, as indicated by a diagnosis of depression recorded during 2 office visits or as a hospital discharge diagnosis during the 6 months before through 2 months after the initiation date. We allowed subjects with diagnoses after the initiation date to be included in the cohort because some practitioners may prescribe an antidepressant as part of diagnosing the condition, in which case the diagnosis may follow the prescription. To ensure complete ascertainment of previous drug use, we required that subjects be residents of British Columbia, as evidenced by enrollment in the provincial Medical Services Plan during the year before initiation. Bupropion was not considered because of its potential use for smoking cessation, and escitalopram was not considered because it was not marketed until December 2004, the end of the study period.
The PharmaNet database (British Columbia Ministry of Health) used to identify antidepressant initiators includes the name, dose, and dispensed quantity for all prescription drugs dispensed in British Columbia pharmacies. This information is entered by pharmacists through a province-wide network that ensures minimal under-reporting and misclassification, and it is recorded for all dispensings, independent of the payor. The British Columbia Ministry of Health also maintains linkable data on all physician services and hospitalizations for all persons in its publicly funded health care system. Up to 25 diagnoses for hospital discharges and 1 diagnosis for each medical service are recorded, with good specificity and completeness.12 These administrative data were further linked to vital statistics data that included information on cause of death, including suicide.
Antidepressant Medication Exposure
Antidepressant medications were grouped into the following categories: selective serotonin reuptake inhibitors (SSRIs), including citalopram, fluoxetine, fluvoxamine, paroxetine, and sertraline; serotonin-norepinephrine reuptake inhibitors (SNRIs), including venlafaxine; tricyclic antidepressants, including amitriptyline, amoxapine, clomipramine, desipramine, doxepin, imipramine, maprotiline, nortriptyline, protriptyline, and trimipramine; other newer and atypical agents, including mirtazapine, nefazodone, and trazodone; and monoamine oxidase inhibitors (MAOIs), including moclobemide, phenelzine, and tranylcypromine. Duloxetine, a SNRI, was not marketed in Canada during the study period.
Exposure status was assigned on the basis of the initiated medication. We determined the availability of antidepressant supply for each patient day by combining consecutive antidepressant dispensings for each patient on the basis of dispensing dates and reported “days supply.”13 When a dispensing occurred before the previous dispensing should have run out, use of the new dispensing was assumed to have begun the day after the end of the old dispensing. Each patient's exposure risk window ended when the subject had been without antidepressant supply for 14 days. Patients underwent censoring at the end of their exposure risk window, the date of switching to or augmenting treatment with another antidepressant medication, emigration from the province, occurrence of a study outcome, death, the end of 1 year, or the end of the study period, whichever came first.
Study End Points
Study outcomes were attempted suicide, completed suicide, and the composite outcome of suicidal acts. Suicide attempt was defined as a hospitalization with an International Classification of Diseases, Ninth Revision (ICD-9), external-cause-of-injury code (E-code) for deliberate self-harm (E950.x–E 958.x). Completed suicides were deaths with an ICD-9 E-code of E950.x to E958.x or an International Classification of Diseases, 10th Revision (ICD-10), diagnosis code of X60 to X84 listed as the cause of death. Violent suicide attempts (ICD-9 E-codes) and completed suicides (ICD-10 codes) were defined as those involving hanging (E953.0; X70), gunshot/explosion (E955; X72–X75), jumping/lying in front of a moving object (E957, E958.0; X80, X81), stabbing/blunt trauma (E956; X78, X79), vehicle collision (E958.5, E958.6; X82), electrocution (E958.4; X83), or self-immolation (E958.1; X76). Assignment and recording of an E-code are mandatory in Canada whenever a diagnosis of poisoning or injury is coded.14 A study of the validity of deliberate self-harm codes for identifying suicide attempts reported a positive predictive value of 86% for deliberate self-harm E-codes.15
Patient Characteristics
Patient characteristics were assessed at treatment initiation, on the basis of medical claims during the year preceding cohort entry. These characteristics included age, gender, calendar year of cohort entry, adjusted family income status (below C$16 000, $16 000–28 000, or above C$28 000, as defined by premium subsidy levels),16 enrollment in an income assistance plan, number of acute hospitalizations, Charlson comorbidity score,17 and number of distinct generic entities prescribed. Psychiatric disorders were defined as the presence of 2 recorded outpatient diagnoses or 1 inpatient diagnosis. Diagnoses included anxiety and obsessive-compulsive disorders, sleep disorders, mania, attention-deficit/hyperactivity disorder (ADHD), substance abuse, psychotic disorders, delirium, personality disorders, and other mental disorders (hysteria, acute reactions to stress, sexual deviations, and disturbances of emotions specific to childhood or adolescence). Additional indicators of psychiatric severity were the number of psychiatric hospitalizations, number of psychiatric visits with a depression diagnosis, suicide attempt in the past year, concurrent stimulant use, and number of psychiatric drug classes (antipsychotic agents, benzodiazepines, and other psychotropic drugs) taken simultaneously. Concurrent stimulant use was defined as having stimulant supply available on the antidepressant initiation date. In addition to psychiatric comorbidities, we measured a number of general medical comorbidities, including malignancy, pain requiring opiates, poisoning or drug toxicity, injury other than poisoning, and seizure disorders. A complete list of covariates and their definitions is provided in Appendix 1.
Statistical Analyses
We used Cox proportional-hazards regression analysis to estimate the effect of antidepressant use on the composite outcome of suicidal acts (attempted or completed suicide). Fluoxetine was used as the reference group for comparisons among the SSRIs, because this drug is widely used and has demonstrated efficacy in children.14,15 For between-class comparisons, SSRIs served as the reference group. To reduce the potential for confounding by indication, a bias that arises when prognostic factors, such as a patient's perceived suicide risk, influence treatment decisions, we adjusted for a number of patient demographic and clinical characteristics (Appendix 1).7 Methods of adjustment included traditional, multivariate, adjusted outcome models, models adjusted for a propensity score including the prespecified covariates in Appendix 1, and models adjusted for a high-dimensional propensity score including empirically identified covariates. These methods are described in Appendix 2.
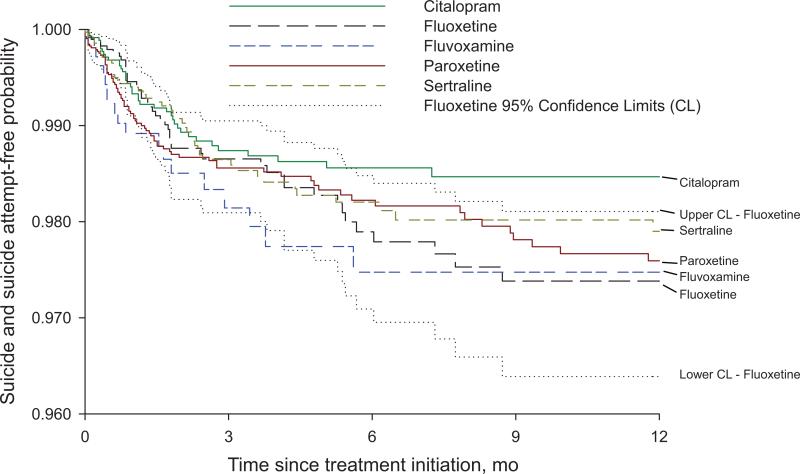
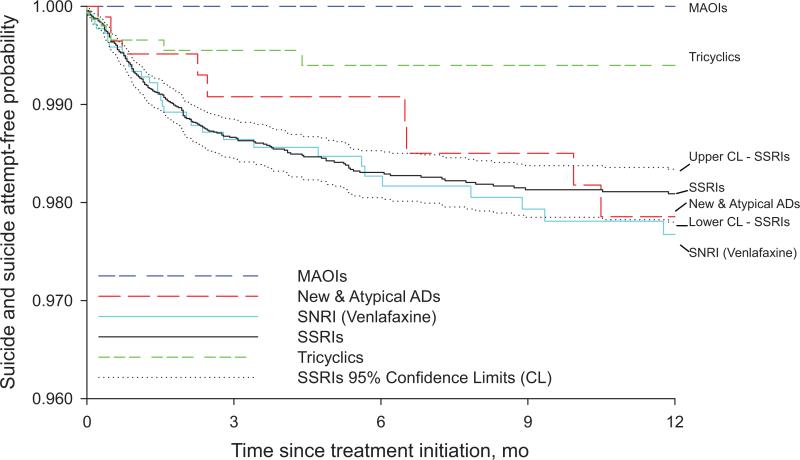
We plotted Kaplan-Meier curves for suicide attempt–free survival as a function of the duration of continuous antidepressant use. We also created multivariate, adjusted, Kaplan-Meier plots by weighting data for each subject by the inverse of his or her probability for treatment, as estimated in the propensity score analysis described above.18
RESULTS
From 1997 to 2005, a total of 20 906 children and adolescents initiated antidepressant therapy. As shown in Table 1, girls accounted for 63% of the population. ADHD (5.1%), manic-depressive illness (2.1%), substance abuse (1.7%), and other mental disorders (8.1%) were the most commonly recorded psychiatric comorbidities; 7.1% of the population had been hospitalized with a psychiatric condition, 2.0% had attempted suicide, and 2.6% were using stimulants at the time of initiation of antidepressant use. SSRIs were the most common class of antidepressants prescribed, accounting for 78% of antidepressant use. Paroxetine, citalopram, and sertraline, the most commonly prescribed drugs, accounted for 25%, 17%, and 17% of overall use, respectively. A total of 16 774 subjects (80%) had no antidepressant use in the past 3 years and contributed to the treatment-naive main analysis. Children and adolescents taking fluvoxamine (5.1%), MAOIs (0.2%), and tricyclic drugs (7.2%) were more likely to be male, to have a diagnosis of ADHD, and to be taking stimulants concurrently, compared with children and adolescents given other agents. There were no other meaningful differences between treatment groups.
TABLE 1.
Distribution of Patient Baseline Characteristics
| SSRIs |
SSRIs | SNRIs | MAOIsa | Other Newer and Atypical Agentsa | Tricyclic Drugsa | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Citalopram | Fluoxetine | Fluvoxamine | Paroxetine | Sertraline | ||||||
| N | 3518 | 2922 | 1068 | 5221 | 3489 | 16 218 | 2197 | 37 | 940 | 1514 |
| Demographic features | ||||||||||
| Age, mean ± SD, y | 15.4 ± 1.6 | 14.8 ± 1.9 | 14.4 ± 2.0 | 15.0 ± 1.8 | 14.9 ± 1.8 | 15.0 ± 1.8 | 15.5 ± 1.5 | 15.1 ± 1.9 | 15.3 ± 1.6 | 14.3 ± 2.2 |
| Female, n (%) | 2406 (68.4) | 1852 (63.4) | 623 (58.3) | 3237 (62.0) | 2197 (63.0) | 10 315 (63.6) | 1352 (61.5) | 20 (54.1) | 576 (61.3) | 807 (53.3) |
| Income, n (%) | ||||||||||
| Below $16 000 | 399 (12.7) | 292 (1 1.4) | 116 (12.9) | 511 (11.5) | 337 (1 1.1) | 1655 (11.7) | 229 (1 1.8) | 7 (21.9) | 129 (16.5) | 197 (15.7) |
| $16 000–28 000 | 55 (1.7) | 60 (2.3) | 23 (2.6) | 92 (2.1) | 68 (2.2) | 298 (2.1) | 33 (1.7) | 1 (3.1) | 13 (1.7) | 30 (2.4) |
| Above $28 000 | 2696 (85.6) | 2209 (86.3) | 761 (84.6) | 3855 (86.5) | 2643 (86.7) | 12 164 (86.2) | 1676 (86.5) | 24 (75.0) | 642 (81.9) | 1030 (81.9) |
| Comorbidities and health services use intensity | ||||||||||
| >6 distinct generic agents used in past year, n (%) | 225 (6.4) | 149 (5.1) | 60 (5.6) | 293 (5.6) | 204 (5.8) | 931 (5.7) | 155 (7.1) | 3 (8.1) | 85 (9.0) | 128 (8.5) |
| Comorbidity score, mean ± SD | 0.028 ± 0.19 | 0.035 ± 0.21 | 0.033 ± 0.19 | 0.039 ± 0.24 | 0.049 ± 0.26 | 0.037 ± 0.23 | 0.031 ± 0.18 | 0.000 ± 0.00 | 0.041 ± 0.21 | 0.046 ± 0.27 |
| Psychiatric visit with depression diagnosis, n (%) | 100 (2.8) | 151 (5.2) | 68 (6.4) | 142 (2.7) | 124 (3.6) | 585 (3.6) | 80 (3.6) | 2 (5.4) | 36 (3.8) | 48 (3.2) |
| Psychiatric hospitalization, n (%) | 230 (6.5) | 194 (6.6) | 131 (12.3) | 337 (6.5) | 277 (7.9) | 1169 (7.2) | 157 (7.2) | 1 (2.7) | 82 (8.7) | 69 (4.6) |
| Recorded psychiatric disorders, n (%)b | ||||||||||
| ADHD | 109 (3.1) | 170 (5.8) | 90 (8.4) | 214 (4.1) | 172 (4.9) | 755 (4.7) | 89 (4.1) | 3 (8.1) | 69 (7.3) | 145 (9.6) |
| Anxiety or sleep disorder | 51 (1.5) | 44 (1.5) | 33 (3.1) | 72 (1.4) | 63 (1.8) | 263 (1.6) | 30 (1.4) | 0 (0.0) | 11 (1.2) | 16 (1.1) |
| Dementia | 0 (0.00) | 2 (0.07) | 1 (0.09) | 6 (0.11) | 3 (0.09) | 12 (0.07) | 1 (0.05) | 0 (0.00) | 1 (0.11) | 1 (0.07) |
| Mania | 72 (2.1) | 65 (2.2) | 43 (4.0) | 89 (1.7) | 98 (2.8) | 367 (2.3) | 60 (2.7) | 1 (2.7) | 15 (1.6) | 2 (0.1) |
| Other psychiatric disorder | 214 (6.1) | 264 (9.0) | 141 (13.2) | 405 (7.8) | 291 (8.3) | 1315 (8.1) | 170 (7.7) | 5 (13.5) | 94 (10.0) | 107 (7.1) |
| Psychotic disorder | 58 (1.7) | 33 (1.1) | 21 (2.0) | 49 (0.9) | 42 (1.2) | 203 (1.3) | 35 (1.6) | 1 (2.7) | 15 (1.6) | 16 (1.1) |
| Substance abuse | 64 (1.8) | 41 (1.4) | 22 (2.1) | 70 (1.3) | 71 (2.0) | 268 (1.7) | 44 (2.0) | 0 (0.0) | 38 (4.0) | 14 (0.9) |
| Suicide attempt | 66 (1.9) | 48 (1.6) | 31 (2.9) | 100 (1.9) | 90 (2.6) | 335 (2.1) | 45 (2.1) | 1 (2.7) | 17 (1.8) | 14 (0.9) |
| Use of ≥1 additional psychiatric medicationc | 440 (12.5) | 329 (11.3) | 158 (14.8) | 748 (14.3) | 400 (11.5) | 2075 (12.8) | 287 (13.1) | 5 (13.5) | 165 (17.6) | 210 (13.9) |
| Concurrent stimulant use | 52 (1.5) | 73 (2.5) | 48 (4.5) | 103 (2.0) | 82 (2.4) | 358 (2.2) | 45 (2.1) | 1 (2.7) | 36 (3.8) | 94 (6.2) |
Baseline covariates were assessed during the year before treatment initiation.
Class lists were as follows: MAOIs, moclobemide, phenelzine, and tranylcypromine; other newer and atypical agents, mirtazapine, nefazodone, and trazodone; tricyclic agents, amitriptyline, amoxapine, clomipramine, desipramine, doxepin, imipramine, maprotiline, nortriptyline, protriptyline, and trimipramine.
Psychiatric disorders were identified on the basis of the presence of 1 inpatient diagnosis code for the disorder or ≥2 outpatient diagnosis codes.
Additional psychiatric medications excluded stimulants.
During the first year of use, we identified a total of 268 children and adolescents who attempted (n = 266) or completed (n = 3) suicide, which yielded a rate of 27.0 suicidal acts (attempted and completed suicides) per 1000 person-years (95% confidence interval [CI]: 23.9–30.5 suicidal acts per 1000 person-years) (Table 2). The suicidal act rates for subgroups of treatment-naive subjects and subjects without a previous suicide attempt were similar to the overall rate (Table 2). Although the hazards were proportional throughout the 1-year follow-up period, most of the events occurred in the first 6 months after initiation (Figs 1 and 2). We identified a total of 43 violent suicide attempts or suicides during the follow-up period, which resulted in a rate of 4.3 cases per 1000 person-years (95% CI: 3.1–5.8 cases per 1000 person-years).
TABLE 2.
Suicide and Attempted Suicide Counts and Rates During 1-Year Follow-up Period
| N | No. of Person-Years | Suicides |
Suicide Attempts |
Suicidal Actsa |
Violent Suicidal Actsb |
|||||
|---|---|---|---|---|---|---|---|---|---|---|
| No. | No. per 1000 Person-Years, Estimate (95% CI) | No. | No. per 1000 Person-Years, Estimate (95% CI) | No. | No. per 1000 Person-Years, Estimate (95% CI) | No. | No. per 1000 Person-Years, Estimate (95% CI) | |||
| All children and adolescents | ||||||||||
| SSRIs | ||||||||||
| Citalopram | 3518 | 1733 | 0 | 0.00 (0.00–2.11) | 39 | 22.50 (16.00–30.76) | 39 | 22.50 (16.00–30.76) | 2 | 1.15 (0.14–4.14) |
| Fluoxetine | 2922 | 1385 | 0 | 0.00 (0.00–2.64) | 42 | 30.32 (21.86–40.99) | 42 | 30.32 (21.86–40.99) | 6 | 4.30 (1.58–9.36) |
| Fluvoxamine | 1068 | 496 | 1 | 1.98 (0.05–11.05) | 18 | 36.29 (21.51–57.35) | 19 | 38.31 (23.06–59.82) | 2 | 3.98 (0.48–14.36) |
| Paroxetine | 5221 | 2417 | 0 | 0.00 (0.00–1.51) | 71 | 29.38 (22.94–37.05) | 71 | 29.38 (22.94–37.05) | 17 | 6.98 (4.06–11.17) |
| Sertraline | 3489 | 1630 | 1 | 0.61 (0.02–3.39) | 45 | 27.61 (20.14–36.94) | 46 | 28.22 (20.66–37.64) | 10 | 6.09 (2.92–11.21) |
| Class | ||||||||||
| SSRI total | 16 218 | 7661 | 2 | 0.26 (0.03–0.93) | 215 | 28.06 (24.44–32.08) | 217 | 28.33 (24.68–32.36) | 37 | 4.79 (3.37–6.61) |
| SNRIs | 2197 | 1126 | 1 | 0.88 (0.02–4.90) | 34 | 30.20 (20.91–42.20) | 34 | 30.20 (20.91–42.20) | 2 | 1.76 (0.21–6.36) |
| MAOIs | 37 | 20 | 0 | 0.00 (0.00–184.44) | 0 | 0.00 (0.00–184.44) | 0 | 0.00 (0.00–184.44) | 0 | 0.00 (0.00–184.44) |
| Other newer and atypical agents | 940 | 409 | 0 | 0.00 (0.00–8.95) | 10 | 24.45 (11.72–44.96) | 10 | 24.45 (11.72–44.96) | 3 | 7.30 (1.51–21.33) |
| Tricyclic drugs | 1514 | 695 | 0 | 0.00 (0.00–5.28) | 7 | 10.07 (4.05–20.75) | 7 | 10.07 (4.05–20.75) | 1 | 1.43 (0.04–7.98) |
| Total (excluding SSRI total) | 20 906 | 9911 | 3 | 0.30 (0.06–0.88) | 266 | 26.84 (23.71–30.27) | 268 | 27.04 (23.90–30.48) | 43 | 4.31 (3.12–5.80) |
| Children and adolescents with no antidepressant use in past 3 y | ||||||||||
| SSRIs | ||||||||||
| Citalopram | 3447 | 1698 | 0 | 0.00 (0.00–2.16) | 39 | 22.97 (16.33–31.40) | 39 | 22.97 (16.33–31.40) | 2 | 1.17 (0.14–4.23) |
| Fluoxetine | 2144 | 1044 | 0 | 0.00 (0.00–3.51) | 28 | 26.82 (17.82–38.76) | 28 | 26.82 (17.82–38.76) | 6 | 5.72 (2.10–12.45) |
| Fluvoxamine | 682 | 325 | 1 | 3.05 (0.08–17.0) | 10 | 30.77 (14.76–56.59) | 11 | 33.85 (16.90–60.56) | 0 | 0.00 (0.00–11.25) |
| Paroxetine | 4041 | 1911 | 0 | 0.00 (0.00–1.92) | 48 | 25.12 (18.52–33.30) | 48 | 25.12 (18.52–33.30) | 12 | 6.24 (3.22–10.90) |
| Sertraline | 2591 | 1244 | 0 | 0.00 (0.00–2.94) | 33 | 26.53 (18.26–37.25) | 33 | 26.53 (18.26–37.25) | 7 | 5.59 (2.25–11.52) |
| Class | ||||||||||
| SSRI total | 12 905 | 6221 | 1 | 0.16 (0.00–0.89) | 158 | 25.40 (21.59–29.68) | 159 | 25.56 (21.74–29.85) | 27 | 4.31 (2.84–6.27) |
| SNRIs | 2019 | 1047 | 1 | 0.95 (0.02–5.27) | 32 | 30.56 (20.91–43.15) | 32 | 30.56 (20.91–43.15) | 1 | 0.95 (0.02–5.27) |
| MAOIs | 17 | 10 | 0 | 0.00 (0.00–368.89) | 0 | 0.00 (0.00–368.89) | 0 | 0.00 (0.00–368.89) | 0 | 0.00 (0.00–368.89) |
| Other newer and atypical agents | 796 | 351 | 0 | 0.00 (0.00–10.48) | 7 | 19.94 (8.02–41.09) | 7 | 19.94 (8.02–41.09) | 2 | 5.70 (0.69–20.58) |
| Tricyclic drugs | 1037 | 492 | 0 | 0.00 (0.00–7.47) | 7 | 14.23 (5.72–29.31) | 7 | 14.23 (5.72–29.31) | 1 | 2.02 (0.05–11.28) |
| Total (excluding SSRI total) | 16 774 | 8120 | 2 | 0.24 (0.03–0.88) | 204 | 25.12 (21.79–28.82) | 205 | 25.25 (21.91–28.95) | 31 | 3.79 (2.58–5.38) |
| Children and adolescents with no previous suicide attempt | ||||||||||
| SSRIs | ||||||||||
| Citalopram | 3452 | 1699 | 0 | 0.00 (0.00–2.16) | 38 | 22.37 (15.83–30.70) | 38 | 22.37 (15.83–30.70) | 2 | 1.17 (0.14–4.23) |
| Fluoxetine | 2874 | 1361 | 0 | 0.00 (0.00–2.69) | 42 | 30.86 (22.24–41.71) | 42 | 30.86 (22.24–41.71) | 6 | 4.38 (1.61–9.53) |
| Fluvoxamine | 1037 | 479 | 1 | 2.05 (0.05–11.44) | 18 | 37.58 (22.27–59.39) | 19 | 39.67 (23.88–61.94) | 2 | 4.12 (0.50–14.87) |
| Paroxetine | 5121 | 2377 | 0 | 0.00 (0.00–1.54) | 68 | 28.61 (22.21–36.27) | 68 | 28.61 (22.21–36.27) | 16 | 6.68 (3.82–10.84) |
| Sertraline | 3399 | 1599 | 1 | 0.62 (0.02–3.46) | 44 | 27.52 (19.99–36.94) | 45 | 28.14 (20.53–37.66) | 10 | 6.22 (2.98–11.43) |
| Class | ||||||||||
| SSRI total | 15 883 | 7515 | 2 | 0.26 (0.03–0.95) | 210 | 27.94 (24.29–31.99) | 212 | 28.21 (24.54–32.27) | 36 | 4.75 (3.33–6.58) |
| SNRIs | 2152 | 1101 | 1 | 0.90 (0.02–5.01) | 33 | 29.97 (20.63–42.09) | 33 | 29.97 (20.63–42.09) | 2 | 1.80 (0.22–6.50) |
| MAOIs | 36 | 19 | 0 | 0.00 (0.00–194.15) | 0 | 0.00 (0.00–194.15) | 0 | 0.00 (0.00–194.15) | 0 | 0.00 (0.00–194.15) |
| Other newer and atypical agents | 923 | 402 | 0 | 0.00 (0.00–9.11) | 10 | 24.88 (11.93–45.75) | 10 | 24.88 (11.93–45.75) | 3 | 7.43 (1.53–21.70) |
| Tricyclic drugs | 1500 | 689 | 0 | 0.00 (0.00–5.34) | 7 | 10.16 (4.08–20.93) | 7 | 7.88 (3.17–16.24) | 1 | 1.45 (0.04–8.06) |
| Total (excluding SSRI total) | 20 494 | 9726 | 3 | 0.31 (0.06–0.89) | 260 | 26.73 (23.58–30.19) | 262 | 26.94 (23.77–30.41) | 42 | 4.29 (3.09–5.79) |
Suicidal acts included suicides and suicide attempts.
Codes for violent suicide attempts (ICD-9 E-codes) and violent completed suicides (ICD-10 codes) included hanging (E953.0; X70), gunshot/explosion (E955; X72–X75), jumping/lying in front of a moving object (E957, E958.0; X80, X81), stabbing/blunt trauma (E956; X78, X79), vehicle collision (E958.5, E958.6; X82), electrocution (E958.4; X83), and self-immolation (E958.1; X76).
FIGURE 1.
Suicide and suicide attempt-free probability according to SSRI agent and time since treatment initiation. Because of the relatively low incidence of suicidal acts, the y-axis scale was inflated to allow for comparisons between agents.
FIGURE 2.
Suicide and suicide attempt-free probability according to antidepressant class and time since treatment initiation. AD indicates antidepressant. Because of the relatively low incidence of suicidal acts, the y-axis scale was inflated to allow for comparisons between agents.
In our primary analysis of treatment-naive children and adolescents, there were no clinically meaningful differences between fluoxetine and the other SSRIs (Table 3). In unadjusted analyses, tricyclic agents were associated with a reduced risk of attempted or completed suicide, compared with SSRIs (rate ratio [RR]: 0.59 [95% CI: 0.28–1.27]). This effect was attenuated to 0.71 (95% CI: 0.33–1.52) in a propensity score-adjusted analysis and was further reduced to 0.92 (95% CI: 0.43–2.00) after adjustment for the high-dimensional propensity score. MAOIs were not investigated because of the small numbers of exposed subjects. Truncation of follow-up time at 6 months after initiation of antidepressant use yielded quantitatively similar results (Appendix 3). Citalopram seemed to be associated with a lower risk of violent suicides and attempts (RR: 0.23 [95% CI: 0.04–1.29]), but the estimate was unstable because of few violent events.
TABLE 3.
Event RRs for Suicidal Acts and Violent Suicidal Acts During 1-Year Follow-up Period
| RR (95% CI) |
||||||
|---|---|---|---|---|---|---|
| Suicidal Acts |
Violent Suicidal Acts |
|||||
| Unadjusted | Adjusted for Age, Gender, and Calendar Year | Adjusted for Propensity Score Decilea | Adjusted for High-Dimensional Propensity Score Decileb | Adjusted for Propensity Score Decilea | Adjusted for High-Dimensional Propensity Score Decileb | |
| Children and adolescents with no antidepressant use in past 3 y | ||||||
| SSRIs | ||||||
| Citalopram | 0.88 (0.54–1.42) | 0.86 (0.51–1.45) | 0.87 (0.51–1.48) | 0.97 (0.54–1.76) | 0.23 (0.04–1.29) | 0.25 (0.04–1.52) |
| Fluvoxamine | 1.28 (0.64–2.57) | 1.18 (0.57–2.43) | 1.10 (0.53–2.27) | 1.05 (0.46–2.43) | 0.00 (0.00–0.00) | 0.00 (0.00–0.00) |
| Paroxetine | 0.94 (0.59–1.50) | 0.76 (0.46–1.24) | 0.76 (0.46–1.24) | 0.80 (0.47–1.37) | 1.41 (0.48–4.13) | 2.19 (0.57–8.43) |
| Sertraline | 1.00 (0.61–1.66) | 0.86 (0.52–1.45) | 0.81 (0.48–1.37) | 1.02 (0.56–1.84) | 1.10 (0.34–3.53) | 1.19 (0.32–4.43) |
| Class | ||||||
| SNRIs | 1.25 (0.86–1.83) | 1.31 (0.89–1.92) | 1.28 (0.87–1.88) | 1.36 (0.89–2.08) | 0.29 (0.04–2.12) | 0.30 (0.04–2.26) |
| Other newer and atypical agents | 0.82 (0.38–1.75) | 0.86 (0.40–1.83) | 0.81 (0.38–1.73) | 1.11 (0.49–2.54) | 1.37 (0.32–5.87) | 1.11 (0.15–8.42) |
| Tricyclic drugs | 0.59 (0.28–1.27) | 0.66 (0.31–1.42) | 0.71 (0.33–1.52) | 0.92 (0.43–2.00) | 0.56 (0.07–4.17) | 0.59 (0.08–4.50) |
| All children and adolescents | ||||||
| SSRIs | ||||||
| Citalopram | 0.76 (0.49–1.18) | 0.77 (0.46–1.29) | 0.79 (0.47–1.33) | 0.87 (0.49–1.53) | 0.23 (0.04–1.30) | 0.25 (0.04–1.63) |
| Fluvoxamine | 1.28 (0.74–2.20) | 1.23 (0.70–2.14) | 1.08 (0.62–1.89) | 1.01 (0.52–1.98) | 1.12 (0.21–5.95) | 0.90 (0.10–8.18) |
| Paroxetine | 0.97 (0.66–1.43) | 0.88 (0.59–1.31) | 0.89 (0.59–1.32) | 0.88 (0.57–1.35) | 2.14 (0.78–5.86) | 3.25 (0.89–11.88) |
| Sertraline | 0.94 (0.62–1.42) | 0.85 (0.56–1.31) | 0.80 (0.52–1.22) | 0.87 (0.54–1.40) | 1.62 (0.56–4.66) | 2.01 (0.57–7.10) |
| Class | ||||||
| SNRIs | 1.12 (0.78–1.61) | 1.22 (0.85–1.77) | 1.20 (0.83–1.74) | 1.29 (0.86–1.94) | 0.50 (0.12–2.10) | 0.57 (0.13–2.41) |
| Other newer and atypical agents | 0.90 (0.48–1.70) | 0.95 (0.51–1.80) | 0.88 (0.47–1.67) | 0.68 (0.28–1.65) | 1.61 (0.49–5.30) | 0.82 (0.11–6.05) |
| Tricyclic drugs | 0.37 (0.18–0.79) | 0.41 (0.19–0.86) | 0.44 (0.21–0.94) | 0.53 (0.24–1.13) | 0.35 (0.05–2.60) | 0.37 (0.05–2.75) |
| Children and adolescents with no previous suicide attempt | ||||||
| SSRIs | ||||||
| Citalopram | 0.75 (0.48–1.16) | 0.76 (0.45–1.27) | 0.78 (0.46–1.32) | 0.77 (0.43–1.37) | 0.22 (0.04–1.22) | 0.28 (0.04–1.74) |
| Fluvoxamine | 1.30 (0.76–2.23) | 1.25 (0.72–2.18) | 1.06 (0.60–1.85) | 1.08 (0.56–2.07) | 0.97 (0.18–5.30) | 1.00 (0.11–9.27) |
| Paroxetine | 0.93 (0.63–1.37) | 0.84 (0.56–1.25) | 0.85 (0.57–1.27) | 0.81 (0.53–1.25) | 1.99 (0.72–5.50) | 2.45 (0.76–7.91) |
| Sertraline | 0.92 (0.60–1.40) | 0.84 (0.54–1.28) | 0.79 (0.51–1.22) | 0.85 (0.53–1.39) | 1.56 (0.54–4.49) | 1.94 (0.52–7.23) |
| Class | ||||||
| SNRIs | 1.11 (0.77–1.61) | 1.22 (0.84–1.77) | 1.20 (0.82–1.74) | 1.34 (0.90–2.00) | 0.53 (0.13–2.21) | 0.56 (0.13–2.39) |
| Other newer and atypical agents | 0.92 (0.49–1.74) | 0.97 (0.52–1.84) | 0.91 (0.48–1.72) | 0.71 (0.29–1.73) | 1.57 (0.48–5.18) | 0.82 (0.11–6.08) |
| Tricyclic drugs | 0.38 (0.18–0.80) | 0.42 (0.20–0.89) | 0.45 (0.21–0.95) | 0.49 (0.22–1.13) | 0.35 (0.05–2.57) | 0.38 (0.05–2.87) |
The reference group for the SSRI comparison was fluoxetine; the reference group for the antidepressant drug class comparisons was SSRIs. MAOIs were not investigated because of the small numbers of exposed subjects.
The propensity score is a patient's estimated probability of treatment with another SSRI versus fluoxetine or a non-SSRI antidepressant versus an SSRI and was estimated with a logistic regression model including the demographic, psychiatric, and general clinical covariates listed in Appendix 1.
The high-dimensional propensity score includes the 500 empirically identified covariates most likely to be confounders, as well as the demographic, psychiatric, and clinical covariates in Appendix 1.
We did not find evidence of multiplicative effect-measure modification by concurrent stimulant use. There was some evidence of sertraline effect-measure modification by ADHD status. The presence of ADHD among sertraline users increased the rate of suicidal acts substantially, relative to the rate observed for fluoxetine users. Sertraline was associated with a 22% reduced risk (RR: 0.68 [95% CI: 0.39–1.18]), compared with fluoxetine, among subjects without ADHD, whereas it was associated with a large increase in risk (RR: 4.70 [95% CI: 0.56–39.25]) among subjects with ADHD, although both estimates lacked precision. Similarly, we found some indication that the initiation of tricyclic antidepressant use increased the risk of suicide and suicide attempt more among patients with previous psychiatric hospitalization (RR: 2.80 [95% CI: 0.84–9.27]) than among those with no such hospitalization (RR: 0.45 [95% CI: 0.17–1.22]).
DISCUSSION
In a population of 20 906 children and adolescents 10 to 18 years of age who were beginning antidepressant therapy in British Columbia between 1997 and 2005, we observed no clinically meaningful variation in the risk of suicidal acts according to antidepressant agent within the class of SSRIs or between antidepressant classes. We observed some numeric variations in the effect sizes between individual agents, but the 95% CIs were substantially overlapping. Because of the small number of patients receiving MAOIs, we did not attempt to compare the risk of suicidal acts between MAOIs and SSRIs. Sertraline might have demonstrated an increased risk of suicidality among children with a recorded diagnosis of ADHD, although this finding was very unstable because of the few events. The majority of events occurred in the first half-year after treatment initiation. Our results are consistent with the findings of several other observational studies that reported small or no differences in rates of suicides and suicide attempts between antidepressant classes,8,9 as well as meta-analyses of randomized, controlled trial data that found no heterogeneity among SSRIs.19–21
Studies that do not find statistically significant differences merit special attention to their statistical power to detect a clinically meaningful difference.22 Because of sample size, we had the greatest power to detect a difference in suicidal act rates between venlafaxine and the SSRI drug class. We could exclude a hazard reduction of >11% and an increase of >108% with a confidence level of 95% for venlafaxine users versus SSRI users. Our estimates of the comparative safety of fluvoxamine versus fluoxetine were the least precise. For the fluvoxamine versus fluoxetine comparison, we could exclude a hazard reduction of >54% and an increase of >143%.
During the 9-year study period, the suicide risk among all British Columbia residents 13 to 17 years of age, as reported by the British Columbia Coroner's Office and British Columbia Statistics, averaged ~0.052 suicide deaths per 1000 people.23–25 The rate we observed after initiation of antidepressant use was 5 times higher, which likely reflects the current depressed state and greater degree of psychiatric comorbidity in our population.
A major strength of our study is that the large, stable, study population allowed us to examine a variety of medications and important subgroups. We had an adequate sample size to restrict our study to new initiators of antidepressants with documented diagnoses of depression. An incident user design reduces the likelihood of missing early adverse events, allows for an evaluation of risks over time, ensures that the assessment of patient baseline characteristics is not influenced by effects of antidepressant treatment, and reduces the likelihood that current treatment assignment is influenced by past drug-related experiences, such as adverse affects and refractory symptoms. Our decision to censor data for subjects at treatment discontinuation and to use a proportional-hazards analysis inherently controls for differences in treatment persistence. To obtain clearly identified exposure groups, we compared monotherapies and censored patient follow-up data as soon as the patient switched drugs or augmented therapy. This analytic strategy makes treatment groups more comparable with respect to initial health state and avoids analytic difficulties associated with comparisons of patients who escalate or change treatment in response to treatment failure or adverse effects with patients who do not. This reduces the generalizability of our findings to patients receiving monotherapy; however, this reduction in generalizability is outweighed by the improvement in validity. The extent of generalizability would depend on the extent to which prescribing by British Columbia physicians and underlying suicide risk and comorbidity patterns among British Columbia children and adolescents are similar to those in other regions and health care settings.
Nonrandomized studies using health care utilization data are particularly scrutinized for their control of confounding and the potential for misclassifying diagnoses.26 Confounding would occur if certain antidepressants were more likely to be given to patients with a greater background risk of suicide. Therefore, we controlled for sociodemographic, clinical, and health care utilization factors likely to be independent predictors of suicidality, by using traditional multivariate and high-dimensional propensity score techniques. However, our ability to adjust fully for mental health status was limited by the measurement and reporting of mental health conditions as ICD-9 codes on insurance claims to the provincial government. Random misclassification of confounders in health care utilization databases leads to incomplete adjustment of confounding bias.27 For example, our finding that expanding the population to include non–treatment-naive subjects increased the apparent protective effect of tricyclic antidepressants, compared with SSRIs, suggests that there may be residual confounding by the presence of treatment-resistant depression or other suicide risk factors in this analysis.
In terms of the validity of our suicide attempt definition, intentional self-harm E-codes do not distinguish between suicidality and self-harm without suicidal intent, despite their widespread use in research and surveillance to identify suicide attempts. However, a study of the validity of deliberate self-harm E-codes to identify suicide attempts reported a positive predictive value of 86% for these codes, relative to the standard method of medical chart review.15 To the extent that suicide attempts are assigned the correct E-codes, these admissions should be captured in the British Columbia hospital discharge database, because this database had an E-coding completeness rate of >95% for the years evaluated. Although it is possible that some suicide attempts were recorded as unintentional injuries or injuries of unknown intent, a Canadian study found that E-codes and medical chart review yielded consistent estimates of the proportions of poisoning-related hospitalizations among subjects 18 to 24 years of age that were attributable to intentional self-harm, and a US study reported 95% agreement between E-codes and physician opinions regarding the intent of injuries that resulted in hospitalization. We did not have data on suicide attempts that were treated in an emergency department without inpatient admission. However, the majority of pediatric and adolescent patients with nonfatal self-harm seen in the emergency department are admitted to the hospital,11 and our inclusion of only more-severe attempts that required hospitalization is likely to increase the specificity of our definition, at some cost in sensitivity. High specificity is desirable, in that relative risk estimates are unbiased if outcomes are assessed with 100% specificity, even if sensitivity is far lower.28
CONCLUSIONS
Our analysis supports the decision of the Food and Drug Administration to include all antidepressants in the black box warning regarding increased suicidality risk for children and adolescents initiating use of antidepressants. Once a decision to initiate pharmacotherapy is made, treatment decisions should be made on the basis of efficacy and less so on the basis of safety. Clinicians should be vigilant in monitoring children and adolescents for whom use of any antidepressant agents is initiated.
ACKNOWLEDGMENT
This project was funded by a grant from the National Institute of Mental Health (grant RO1-MH078708).
Funded by the National Institutes of Health (NIH).
ABBREVIATIONS
- ADHD
attention-deficit/hyperactivity disorder
- CI
confidence interval
- E-code
external-cause-of-injury code
- ICD-9
International Classification of Diseases, Ninth Revision
- ICD-10
International Classification of Diseases, 10th Revision
- MAOI
monoamine oxidase inhibitor
- RR
rate ratio
- SSRI
selective serotonin reuptake inhibitor
- SNRI
serotonin-norepinephrine reuptake inhibitor
APPENDIX 1.
Baseline Covariates and Definitions
| Nonpsychiatric Disordersa | Definition |
|---|---|
| Chronic lung disease | 491.xx |
| 492.x | |
| 493.xx | |
| 494.x | |
| 495.xx | |
| 496 | |
| Diabetes mellitus | 250.xx |
| 357.2 | |
| 362.0 | |
| 362.07 | |
| Plus ≥1 prescription for any of the following: insulin, acarbose, miglitol, metformin, acetahexamide, chlorpropamide, glimepiride, glipizide, glyburide, repaglinide, tolazamide, tolbutamide, pioglitazone, rosiglitazone, troglitazone, or nateglinide | |
| Gastrointestinal hemorrhage | 578.x |
| 531.0, 531.2, 531.4, 531.6 | |
| 532.0, 532.2, 532.4, 532.6 | |
| 533.0, 533.2, 533.4, 533.6 | |
| 534.0, 534.2, 534.4, 534.6 | |
| Ventricular arrhythmia | 427.4x, 427.41, 427.42, 427.5x, 427.1x, 427.69 |
| Other arrhythmia | 427.xx or 426.xx except for 427.4x, 427.41, 427.42, 427.5x, 427.1x, 427.69 |
| Congenital heart diseases | 745.xx, 746.xx |
| Other congenital anomalies of cardiovascular system | 747.xx |
| Cardiomyopathy | 425.xx |
| Rheumatic heart diseases | 393.xx–398.xx except for 398.91 |
| Hypertensive heart and kidney diseases | 402.xx–404.xx except for 402.01, 402.11, 402.91, 404.01, 404.11, 404.91, 404.03, 404.13, 404.93 |
| Nonrheumatic valve | 424.xx |
| Endocarditis, pericarditis, and myocarditis | 420.xx, 421.xx, 422.xx |
| Rheumatic fever | 390.xx, 391.xx, 392.xx |
| Essential hypertension | 401.xx or use of thiazide |
| Secondary hypertension | 405.xx |
| Hypothyroidism | 243, 244.x |
| Injury other than poisoning | 800.xx–959.xx |
| Colorectal cancer | 153.xx, 230.3x, 154.xx(except 154.2, 154.3 and 154.4), 230.4 |
| Lung cancer | 162.xx, 231.2 |
| Breast cancer | 174.xx, 233.0 |
| Prostate cancer | 185.xx, 233.4 |
| Other malignancy | 140.xx–208.xx (hospital diagnosis), excluding lung cancer, breast cancer, prostate cancer, and colorectal cancer codes |
| Other heart disease | 411.xx–414.xx |
| Pain requiring high-potency opiates | Use of diacetylmorphine HCl, fentanyl, hydromorphone, hydroxyephedrine/normethadone, meperidine, methadone, or morphine |
| Pain requiring middle-potency opiates | Use of codeine, hydrocodone, oxycodone, pseudoephedrine, drocodone, or propoxyphene |
| Peptic ulcer disease and related conditions (without hemorrhage) | 531.1, 531.3, 531.5, 531.7, 531.9 532.1, 532.3, 532.5, 532.7, 532.9 533.1, 533.3, 533.5, 533.7, 533.9 534.1, 534.3, 534.5, 534.7, 534.9 |
| Pneumonia | 480.x, 481, 482.xx, 483.x, 484.x, 485, 486 |
| Poisoning or drug toxicity | 960.xx–979.xx |
| 980.xx–989.xx | |
| Rheumatoid arthritis | 714.x plus disease-modifying antirheumatic drug or steroid use |
| Seizure disorders | 345, 345.xx |
| 780.3x | |
| Sepsis | 038.xx |
| 995.91 | |
| Psychiatric disordersb | |
| Depressive illnesses | 293.83 |
| 296.2x | |
| 296.3x | |
| 296.90 | |
| 298.0x | |
| 300.4x | |
| 309.0x | |
| 309.1x | |
| 309.28 | |
| 311 | |
| Anxiety disorders | 300.0x |
| 300.2x | |
| 300.3x | |
| Sleep disorders | 307.4x |
| 347, 347.xx | |
| 780.5x | |
| Manic-depressive illness | 296.0x |
| 296.1x | |
| 296.4x | |
| 296.5x | |
| 296.6x | |
| 296.7x | |
| 296.8x | |
| 296.99 | |
| ADHD | 312.xx, 314.xx |
| Alcohol abuse | 291.0x |
| 291.1x | |
| 291.2x | |
| 291.3x | |
| 291.4x | |
| 291.5x | |
| 291.8x | |
| 291.9x | |
| 303, 303.xx | |
| 305.0x | |
| Drug abuse or dependence | 292.0x |
| 292.1x | |
| 292.2x | |
| 292.8x | |
| 292.9x | |
| 304, 304.xx | |
| 305.2x–305.9x | |
| Psychotic disorders | 290.8x |
| 290.9x | |
| 295, 295.xx | |
| 297, 297.xx | |
| 298, 298.1x–298.9x | |
| 299, 299.xx | |
| 780.1x | |
| Other psychiatric disorders | |
| Delirium | 290.11 |
| 290.3x | |
| 290.41 | |
| 291.0x | |
| 292.81 | |
| 293 | |
| 293.0x | |
| 293.1x | |
| 293.8x | |
| 293.9x | |
| 348.3x | |
| 349.82 | |
| Personality disorders | 301, 301.xx |
| Other mental disorders | 300.1x |
| 300.5x–300.9x | |
| 302, 302.xx | |
| 306, 306.xx | |
| 307.0x–307.3x, 307.5x–307.9x | |
| 308, 308.xx | |
| 309.2x–309.9x | |
| 310, 310.xx | |
| 313, 313.xx | |
| 315, 315.xx | |
| 316, 316.xx |
Defined as having ≥1 hospitalization with the condition as any diagnosis or ≥1 physician claim with the condition recorded unless otherwise noted.
Defined as having ≥1 hospitalization with the condition as any diagnosis or ≥2 physician claims with the condition recorded.
APPENDIX 2: STATISTICAL METHODS
To reduce the potential for confounding by indication, a bias that arises when prognostic factors, such as a patient's perceived suicide risk, influence treatment decisions, we adjusted for a number of patient demographic and clinical characteristics (Appendix 1).7 Because of the anticipated small number of outcomes, we reduced these potential confounders into an exposure propensity score.29 A propensity score is a patient's probability of receiving treatment (in this case, another SSRI versus fluoxetine or a non-SSRI versus a SSRI), adjusted for his or her measured characteristics, and typically is estimated by using a logistic regression model.30 Treatment effects can be estimated within propensity score levels, which define groups of patients who are similar in their probabilities of having received treatment. We estimated propensity scores by using logistic regression models including the patient covariates in Appendix 1; no further variable selection was performed. After plotting and comparing the distribution of propensity scores for the exposed and unexposed patients, we truncated our study population to the area of overlap. Because relative risk estimates varied within deciles of propensity scores, we used exposure propensity score decile as a categorical variable in the Cox proportional-hazards models.
In addition to constructing a propensity score that included the covariates described above, in a secondary analysis we constructed a high-dimensional propensity score that included empirically identified covariates. This technique examined all dispensed drugs, recorded diagnoses, and performed procedures reported for a patient before the initiation of antidepressant therapy and identified codes that might potentially bias the exposure and outcome in question. All identified codes were sorted according to their potential for confounding and were used to create a propensity score that was based on the top 500 identified variables in addition to the variables identified by the investigators (Appendix 1). This new technique has been shown to improve adjustment for confounding.31
We also conducted a multivariate adjusted analysis. This model was constructed by using a backward selection algorithm with the P value for covariate exclusion criteria set to .2, as recommended by simulation studies on variable selection in epidemiology.32 To decrease further the likelihood of confounding by indication,7 we performed the primary analysis among treatment-naive subjects initiating antidepressant use, defined as children and adolescents with no antidepressant use in the past 3 years. This design reduces the likelihood that we analyzed data for children and adolescents initiating use of a medication for recurrent depression. We conducted a subgroup analysis with children and adolescents without a previous suicide attempt. In addition, we tested for effect-measure modification by various covariates, such as concurrent use of stimulants, previous ADHD diagnosis, previous psychiatric hospitalization, and previous suicide attempt.
APPENDIX 3.
Event RRs for Suicidal Acts and Violent Suicidal Acts During 6-Month Follow-up Period
| RR (95% CI) |
||||
|---|---|---|---|---|
| Suicidal Acts |
Violent Suicidal Acts |
|||
| Unadjusted | Adjusted for Age, Gender, and Calendar Year | Adjusted for Propensity Score Decile | Adjusted for Propensity Score Decile | |
| Children and adolescents with no antidepressant use in past 3 y | ||||
| SSRIs | ||||
| Citalopram | 1.02 (0.62–1.70) | 1.00 (0.58–1.74) | 1.02 (0.58–1.80) | 0.23 (0.04–1.29) |
| Fluvoxamine | 1.36 (0.65–2.84) | 1.29 (0.60–2.79) | 1.16 (0.54–2.51) | 0.00 (0.00–0.00) |
| Paroxetine | 1.07 (0.66–1.76) | 0.88 (0.52–1.48) | 0.86 (0.51–1.45) | 1.41 (0.48–4.13) |
| Sertraline | 1.14 (0.67–1.93) | 1.01 (0.58–1.74) | 0.95 (0.55–1.65) | 1.10 (0.34–3.53) |
| Class | ||||
| SNRIs | 1.07 (0.71–1.62) | 1.12 (0.74–1.70) | 1.09 (0.72–1.67) | 0.29 (0.04–2.12) |
| Other newer and atypical agents | 0.37 (0.12–1.17) | 0.39 (0.12–1.21) | 0.36 (0.11–1.14) | 1.37 (0.32–5.87) |
| Tricyclic drugs | 0.63 (0.29–1.34) | 0.70 (0.33–1.51) | 0.75 (0.35–1.62) | 0.56 (0.07–4.17) |
| All children and adolescents | ||||
| SSRIs | ||||
| Citalopram | 0.87 (0.56–1.37) | 0.90 (0.53–1.53) | 0.91 (0.53–1.58) | 0.23 (0.04–1.30) |
| Fluvoxamine | 1.38 (0.79–2.43) | 1.34 (0.75–2.40) | 1.15 (0.64–2.07) | 1.12 (0.21–5.95) |
| Paroxetine | 1.06 (0.71–1.58) | 0.97 (0.64–1.47) | 0.96 (0.63–1.47) | 2.14 (0.78–5.86) |
| Sertraline | 1.02 (0.66–1.58) | 0.94 (0.60–1.48) | 0.88 (0.56–1.38) | 1.62 (0.56–4.66) |
| Class | ||||
| SNRIs | 0.98 (0.66–1.45) | 1.07 (0.72–1.60) | 1.05 (0.70–1.57) | 0.50 (0.12–2.10) |
| Other newer and atypical agents | 0.58 (0.26–1.30) | 0.61 (0.27–1.37) | 0.56 (0.25–1.27) | 1.61 (0.49–5.30) |
| Tricyclic drugs | 0.40 (0.19–0.84) | 0.43 (0.20–0.92) | 0.48 (0.22–1.02) | 0.35 (0.05–2.60) |
| Children and adolescents with no previous suicide attempt | ||||
| SSRIs | ||||
| Citalopram | 0.85 (0.54–1.34) | 0.88 (0.52–1.51) | 0.89 (0.51–1.55) | 0.22 (0.04–1.22) |
| Fluvoxamine | 1.40 (0.80–2.46) | 1.37 (0.77–2.44) | 1.12 (0.62–2.02) | 0.97 (0.18–5.30) |
| Paroxetine | 1.01 (0.68–1.52) | 0.92 (0.60–1.40) | 0.91 (0.60–1.40) | 1.99 (0.72–5.50) |
| Sertraline | 1.00 (0.65–1.56) | 0.92 (0.59–1.45) | 0.86 (0.55–1.36) | 1.56 (0.54–4.49) |
| Class | ||||
| SNRIs | 0.97 (0.65–1.45) | 1.06 (0.70–1.59) | 1.04 (0.69–1.57) | 0.53 (0.13–2.21) |
| Other newer and atypical agents | 0.59 (0.26–1.33) | 0.62 (0.27–1.40) | 0.58 (0.26–1.30) | 1.57 (0.48–5.18) |
| Tricyclic drugs | 0.40 (0.19–0.85) | 0.45 (0.21–0.95) | 0.49 (0.23–1.04) | 0.35 (0.05–2.57) |
The reference group for the SSRI comparison was fluoxetine; the reference group for the antidepressant drug class comparisons was SSRIs.
Footnotes
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
REFERENCES
- 1.Food and Drug Administration [February 1, 2005];Summary minutes of the September 13–14, 2004 Center for Drug Evaluation and Research Pharmachopharmacologic Drugs Advisory Committee and the FDA Pediatric Advisory Committee. Available at: www.fda.gov/ohrms/dockets/ac/04/minutes/2004-4065M1_Final.htm.
- 2.Hammad TA, Laughren T, Racoosin J. Suicidality in pediatric patients treated with anti-depressant drugs. Arch Gen Psychiatry. 2006;63(3):332–339. doi: 10.1001/archpsyc.63.3.332. [DOI] [PubMed] [Google Scholar]
- 3.Tiihonen J, Lönnqvist J, Wahlbeck K, Klaukka T, Tanskanen A, Haukka J. Antidepressants and the risk of suicide, attempted suicide, and overall mortality in a nationwide cohort. Arch Gen Psychiatry. 2006;63(12):1358–1367. doi: 10.1001/archpsyc.63.12.1358. [DOI] [PubMed] [Google Scholar]
- 4.Didham RC, McConnell DW, Blair HJ, Reith DM. Suicide and self-harm following prescription of SSRIs and other antidepressants: confounding by indication. Br J Clin Pharmacol. 2005;60(5):519–525. doi: 10.1111/j.1365-2125.2005.02480.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Olfson M, Marcus SC, Shaffer D. Antidepressant drug therapy and suicide in severely depressed children and adults: a case-control study. Arch Gen Psychiatry. 2006;63(8):865–872. doi: 10.1001/archpsyc.63.8.865. [DOI] [PubMed] [Google Scholar]
- 6.Valuck RJ, Libby AM, Sills MR, Giese AA, Allen RR. Antidepressant treatment and risk of suicide attempt by adolescents with major depressive disorder: a propensity-adjusted retrospective cohort study. CNS Drugs. 2004;18(15):1119–1132. doi: 10.2165/00023210-200418150-00006. [DOI] [PubMed] [Google Scholar]
- 7.Walker AM. Confounding by indication. Epidemiology. 1996;7(4):335–336. [PubMed] [Google Scholar]
- 8.Jick H, Kaye J, Jick S. Antidepressants and the risk of suicidal behaviors. JAMA. 2004;292(3):338–343. doi: 10.1001/jama.292.3.338. [DOI] [PubMed] [Google Scholar]
- 9.Martinez C, Rietbrock S, Wise L, et al. Antidepressant treatment and the risk of fatal and non-fatal self-harm in first episode of depression: nested case-control study. BMJ. 2005;330(7488):389. doi: 10.1136/bmj.330.7488.389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.British Columbia Injury Research and Prevention Unit [March 18, 2009];BCIRPU online data tool. Available at: www.injuryresearch.bc.ca/categorypages.aspx?catid=10&catname=Online%20Data%20Tool.
- 11.Centers for Disease Control and Prevention [March 18, 2009];Web-based Injury Statistics Query and Reporting System (WISQARS) Available at: www.cdc.gov/injury/wisqars/index.html.
- 12.Williams JI, Young W. Inventory of Studies on the Accuracy of Canadian Health Administrative Databases. Institute for Clinical Evaluative Sciences; Toronto, Canada: 1996. [Google Scholar]
- 13.Dormuth CR, Glynn RJ, Neumann P, Maclure M, Brookhart AM, Schneeweiss S. Impact of two sequential drug cost-sharing policies on the use of inhaled medications in older patients with chronic obstructive pulmonary disease or asthma. Clin Ther. 2006;28(6):964–978. doi: 10.1016/j.clinthera.2006.06.007. [DOI] [PubMed] [Google Scholar]
- 14.Canadian Institute for Health Information . Abstracting Manual. Canadian Institute for Health Information; Ottawa, Canada: 1999. [Google Scholar]
- 15.Iribarren C, Sidney S, Jacobs DR, Jr, Weisner C. Hospitalization for suicide attempt and completed suicide: epidemiological features in a managed care population. Soc Psychiatry Psychiatr Epidemiol. 2000;35(7):288–296. doi: 10.1007/s001270050241. [DOI] [PubMed] [Google Scholar]
- 16.Warburton RN. Takeup of income-tested health-care premium subsidies: evidence and remedies for British Columbia. Can Tax J. 2005;53(1):1–28. [Google Scholar]
- 17.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chron Dis. 1987;40(5):373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 18.Robins JM. Marginal structural models. In: 1997 Proceedings of the American Statistical Association, Section on Bayesian Statistical Science. American Statistical Association; Alexandria, VA: 1998. [May 5, 2009]. pp. 1–10. Available at: www.biostat.harvard.edu/%7Erobins/msm-web.pdf. [Google Scholar]
- 19.Mosholder AD, Willy M. Suicidal adverse events in pediatric randomized, controlled clinical trials of antidepressant drugs are associated with active drug treatment: a meta-analysis. J Child Adolesc Psychopharmacol. 2006;16(1–2):25–32. doi: 10.1089/cap.2006.16.25. [DOI] [PubMed] [Google Scholar]
- 20.Dubicka B, Hadley S, Roberts C. Suicidal behaviour in youths with depression treated with new-generation antidepressants: meta-analysis. Br J Psychiatry. 2006;189(5):393–398. doi: 10.1192/bjp.bp.105.011833. [DOI] [PubMed] [Google Scholar]
- 21.Hetrick S, Merry S, McKenzie J, Sindahl P, Proctor M. Selective serotonin reuptake inhibitors (SSRIs) for depressive disorders in children and adolescents. Cochrane Database Syst Rev. 2007;(3):CD004851. doi: 10.1002/14651858.CD004851.pub2. [DOI] [PubMed] [Google Scholar]
- 22.Freiman JA, Chalmers TC, Smith H, Jr, Kuebler RR. The importance of β, the type II error and sample size in the design and interpretation of the randomized control trial: survey of 71 “negative” trials. N Engl J Med. 1978;299(13):690–694. doi: 10.1056/NEJM197809282991304. [DOI] [PubMed] [Google Scholar]
- 23.British Columbia Coroner's Office [November 18, 2008];Teen deaths: 1997 to 2004. Available at: www. pssg.gov.bc.ca/coroners/publications/docs/stats-youth-youngadult-deaths-1997-2004.pdf.
- 24.British Columbia Coroner's Office [November 18, 2008];Suicide statistics: 1997 to 2004. Available at: www.pssg.gov.bc.ca/coroners/publications/docs/stats-suicide-1997-2004.pdf.
- 25.BC Stats [November 18, 2008];British Columbia population by selected age groups. Available at: www.bcstats.gov.bc.ca/data/pop/pop/project/bc0806tab3.csv.
- 26.Schneeweiss S, Avorn J. A review of uses of health care utilization databases for epidemiologic research on therapeutics. J Clin Epidemiol. 2005;58(4):323–337. doi: 10.1016/j.jclinepi.2004.10.012. [DOI] [PubMed] [Google Scholar]
- 27.Greenland S, Robins J. Confoundingandmisclassification. Am J Epidemiol. 1985;122(3):495–506. doi: 10.1093/oxfordjournals.aje.a114131. [DOI] [PubMed] [Google Scholar]
- 28.Kelsey JL, Whittemore AS, Evans AS, Thompson WD. Methods in Observational Epidemiology. 2nd ed. Oxford University Press; New York, NY: 1996. [Google Scholar]
- 29.Braitman LE, Rosenbaum PR. Rare outcomes, common treatments: analytic strategies using propensity scores. Ann Intern Med. 2002;137(8):693–695. doi: 10.7326/0003-4819-137-8-200210150-00015. [DOI] [PubMed] [Google Scholar]
- 30.Rosenbaum P, Rubin D. The central role of the propensity score in observational studies for causal effects. Biometrika. 1983;70(1):41–55. [Google Scholar]
- 31.Schneeweiss S, Rassen JA, Glynn RJ, Avorn J, Mogun H, Brookhart MA. High-dimensional propensity score adjustment in studies of treatment effects using health care claims data. Epidemiology. 2009;20(4):512–522. doi: 10.1097/EDE.0b013e3181a663cc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Maldonado G, Greenland S. Simulation study of confounder-selection strategies. Am J Epidemiol. 1993;138(11):923–936. doi: 10.1093/oxfordjournals.aje.a116813. [DOI] [PubMed] [Google Scholar]