Significance of Acute Coronary Syndromes
Coronary heart disease is responsible for more than 7 million deaths each year worldwide 1. However, since 1999 heart disease death rates have decreased by 25.8% in the U.S., exceeding the American Heart Association’s strategic goal of a 25% reduction by 2010 2. Despite these encouraging statistics, nearly 1.4 million Americans are projected to experience an episode of acute coronary syndromes (ACS) in 2009 3.
The Cost of Indecision: Myocardial Necrosis and Poorer Outcomes
Time to treatment for symptoms of ACS can be a matter of life and death. Data suggest up to half of patients with ACS experience sudden death prior to arrival in the emergency department (ED) 3. In addition, degree of myocardial necrosis is related to length of the ischemic episode 4. As a result, there is a rapid diminishing benefit to reperfusion during myocardial infarction. Restoring flow to the affected artery within 30 minutes can abort an infarction. If reperfusion occurs within 2–3 hours some preservation of myocardial function is achieved but after 6 hours there is little or no myocardial salvage 5. Numerous clinical trials have demonstrated that early presentation to the ED is associated with decreased mortality and decreased reinfarction rates for patients receiving thrombolytics 6,7. Additionally, McNamara et al. (2006) found that longer door to balloon time was associated with increased in-hospital mortality in a cohort study of 29,222 patient undergoing percutaneous coronary interventions 8.
Finally, those patients presenting for treatment in less than two hours remain the small minority making group comparisons across time a challenge. Prior research has shown median time to treatment varies from 1.1–24 hours 9–14. Studies show as little as one-fifth of patients present to the hospital within one hour of symptom onset, while up to 40% delay more than 6 hours 15,16. In the Rapid Early Action for Coronary Treatment (REACT) trial, median time from symptom onset to arrival in the ED was 2.33 hours at baseline. Twenty-five percent of patients delayed longer than 5.2 hours. Delay time decreased by only 4.7% (7 min.) per year over the three years of mass media messages targeting EMS utilization and reduced delay in presentation in the ED 17. This delay prevents the majority of patients from receiving optimal benefits of reperfusion therapy. Time to treatment for those with ST-elevation myocardial infarction is of particular concern since patients with complete occlusion benefit most from immediate reperfusion.
Factors Affecting Time to Treatment for Acute Coronary Syndromes
The most important factor impacting increased time to treatment for ACS is the patient’s decision to delay seeking care 18. It is essential to understand the decision-making processes that patients employ that lead to delay in accessing emergency medical services or presentation to the ED, in order to decrease time to treatment. Rosenfeld 10,19 examined decision-making patterns and their predictors in a sample of women with myocardial infarction. Most participants were categorized into one of two groups; those who knew they would seek assistance for symptoms (knowing) or those who decided to manage or minimize symptoms (managing). Those in the knowing group had a shorter median time to treatment of compared to the managing group (0.90 hours vs. 11.25 hours) 10.
Other studies have identified sociodemographic, cognitive/appraisal, behavioral, and illness factors impacting the time to treatment for symptoms of ACS.20 Factors associated with increased time to treatment are older age, female gender, living alone, African American race 9,13,16,21–24, lack of recognition and discounting of symptoms 19,25,26, mismatch between expected and actual symptoms 27, maintaining a sense of normality 28, presence of third parties 19,27, self-treatment 29, stress and emotional states,30 and fear of bothering others,31. Factors associated with decreased time to treatment are higher perceived risk 31, fear of death 31, severity of symptoms 32, and access to emergency medical services 28. It is noteworthy that these data have been gathered in Asia, Europe, the Middle East, and the United States, suggesting that patient indecision and resulting delay in treatment is a global problem.
Identification of variables impacting the decision to seek care has the potential to reduce time to treatment and result in lower rates of sudden cardiac death, increased myocardial muscle preservation, and reduced mortality 33,34. Further, results from studies sampling large heterogeneous populations will build upon the knowledge garnered in small qualitative studies and may lead to effective interventions to hasten recognition of ACS symptoms, reduce time to presentation in the ED, and result in more expeditious treatment. Data for this analysis were part of a larger study examining gender differences in symptoms of ACS 35. An exploratory aim of the study, reported here, was to identify factors associated with a decision to seek care in the ED for symptoms. The goals were to; 1) describe word patterns patients use during acute coronary syndromes; 2) explore reasons for seeking care in the ED, 3) identify categories of decision-making; and 4) describe factors associated with time to presentation in the ED.
Methods
Design
A descriptive, cross-sectional design was used to address study aims. Factors impacting the decision to seek care in the ED were explored by asking two open-ended questions at the beginning of each interview. Patients were also asked when their symptoms began and what time they arrived at the ED. The medical record was searched in the few instances where the patient could not recall times. Time from symptom onset to arrival in the ED was then computed from patient report or medical records.
Sample and Setting
Two hundred eighty-two patients with an admitting diagnosis of ACS were recruited from the cardiac step-down units at two urban, non-academic, medical centers. Both are regional referral centers for local community hospitals with a combined total of over 1200 beds. One serves a large number of minority and indigent patients. Ten patients, six women and four men, declined to participate due to fatigue or lack of interest. One refused to sign the consent form. Six of the ten were Black and ages ranged from 40 to 85. The remaining 272 patients gave written consent and completed the interview. Approval for the study was obtained from the Institutional Review Boards at the sponsoring institution and both hospitals. Patients were eligible for the study if they were admitted through the ED at least 12 hours prior to interview with an admitting diagnosis of ACS, at least 21 years of age, fluent in English, pain free, and had adequate cognitive capacity. ACS was defined as unstable angina (UA), non ST-segment myocardial infarction (NSTEMI), or ST-elevation myocardial infarction (STEMI) 36. Diagnosis was made according to the joint European Society of Cardiology/American College of Cardiology/American Heart Association guidelines. Unstable angina was diagnosed by clinical presentation. NSTEMI was diagnosed by elevation in Troponin I or T above referenced norms. STEMI was diagnosed when ST-segments were elevated by > 1mm in two contiguous leads or when pathologic Q waves were present 37. Data from sixteen patients whose admitting diagnosis of ACS was not sustained and were discharged with a primary diagnosis other than ACS were excluded from analyses. This resulted in a final sample of 256. Possible symptom confounders were controlled for through design. Patients with documentation of prior heart failure, heart failure on admission, elevated brain natriuretic peptide, or cocaine use were excluded from study.
Procedures
Patients were interviewed in their hospital rooms following consent. All rooms on both step-down units are private so confidentiality during interview was assured. Two open-ended questions were asked prior to completion of quantitative tools: 1) What symptoms did you experience prior to coming to the ED for this hospitalization? and 2) What happened that made you decide to come to the hospital? These questions allowed the participants to focus on their personal experience during the episode of ACS and to talk about their symptoms and decisions in their own words without introducing bias from items contained on the 20-item Symptoms of Acute Coronary Syndromes Index 35. In addition, patients were specifically asked to describe only symptoms associated with this acute event and not symptoms that could have been part of the prodrome. All data were collected by the principal investigator (PI) and three research nurses. One research nurse was a master’s prepared clinical instructor and two were master’s students. Inter-rater reliability was confirmed in 10% of interviews by the PI simultaneously completing the research tools while the research nurses conducted the interview. The mean correlation between raters on quantitative tools was 0.96.
Data Analyses
Descriptive Content Analysis
All patient responses during interview were recorded verbatim and transcribed into a Word document. There were a total of 329 responses because many patients gave more than one reason for deciding to seek care in the ED. Data were analyzed by four members of the research team; the PI, a co-investigator and qualitative methods expert, and two research assistants. The team met together to complete data analyses and discuss findings. Descriptive content analysis was used to establish categories in which responses from participants could be displayed 38. This method of analysis is the most straightforward type of qualitative analysis and allows for clear enumeration of data. Methods were employed to enhance creditability and auditability 39 including; data were analyzed by all team members simultaneously; categories were confirmed by all team members; disagreements were resolved through discussion until consensus was reached and finally; further comparisons were made to identify commonalities and differences in the statements which lead to refinement of the categories. We employed an innovative statistical analysis in that the categories identified in the descriptive content analysis were used as predictor variables in a Cox Proportional Hazards model to examine time from symptom onset to arrival in the ED.
Quantitative data
Patient characteristics and time from symptom onset to presentation in the ED, were analyzed using SPSS (version 15). Dichotomous data were analyzed using the chi-square statistic and continuous data were analyzed with independent sample t-tests. The five decision-making factors identified in the descriptive content analyses and other patient characteristics including; age, marital status, income, education, history of heart disease, whether a health care provider was called, presence of a bystander, severity of symptoms, self-treatment of symptoms, and temporal nature of symptoms were treated as predictor variables in an analysis of time from symptom onset to arrival in the ED. Due to the non-normality of the dependent variable (time from symptom onset to arrival in the ED), survival analysis was used to measure the effect of various baseline covariates on the time (measured in hours) from onset of symptoms to admission in the ED. Model selection consisted of initial univariate analysis using a Log-rank test for categorical variables and a Cox Proportional Hazards model for continuous variables. Covariates with a p-value of <0.25 were selected for inclusion in a multivariate model and stepwise selection was then used to attain a final Cox Proportional Hazards model. A p-value of <0.25 was chosen because we wanted to err on the side of inclusion of potential covariates 40. There is no standard for how strong an association between a variable and the outcome of interest should be although investigators often choose a p value of <0.25 based on prior empirical evidence 41. Katz (2002) 40 cautions that in the presence of a suppressor effect, the variable may not even be weakly associated with the outcome in the bivariate analysis. We hypothesized this to be the case for the variables identified by patients in the qualitative analysis and for variables previously associated with time to presentation in the ED. The assumption of proportional hazards was tested including covariate*log(time) effects for all model covariates, with the test supporting the assumption of proportional hazards.
Findings
Clinical Characteristics of the Sample
A heterogeneous sample of nearly equal numbers of women (n=112) and men (n=144) were recruited. Convenience sampling was used and eligible patients were recruited sequentially. We did not over sample for women. The characteristics of women and men in the sample were similar except that women were significantly older and more likely to have a lower family income (Table 1). Both women and men were nearly equally divided into the three diagnostic categories of UA, NSTEMI, and STEMI. The only difference in symptom characteristics was that men were more likely to state that symptoms were caused by exertion.
Table 1.
Characteristics of Patients Seeking Care in the ED for ACS
| Women (n=112) | Men (n=144) | p-value | |
|---|---|---|---|
| Type of Acute Coronary | |||
| Syndrome | |||
| UA | 38 (34%) | 50 (35%) | .64 |
| NSTEMI | 40 (36%) | 44 (30%) | |
| STEMI | 34 (30%) | 50 (35%) | |
| Symptom Characteristics | |||
| Symptoms Constant | 69 (61.6%) | 86 (59.6%) | .66 |
| Self-Treat Symptoms | 67 (59.8%) | 91 (63.2%) | .34 |
| Similar Symptoms in Past | 63 (56.3%) | 82 (56.9%) | .51 |
| Symptoms Brought on by: | |||
| Exertion | 12 (10.7%) | 37 (25.7%) | <.01 |
| Emotional Upset | 26 (23.2%) | 28 (19.4%) | .28 |
| Rest | 23 (20.5%) | 19 (13.2%) | .08 |
| Other Causes* | 65 (58.0%) | 73 (50.7%) | .15 |
| Severity of Chest Pain | |||
| (Mean±SD- scale 0–10) | 6.08±3.37 | 6.84±3.01 | .06 |
| Severity of Worst Symptom | |||
| (Mean±SD- scale 0–10) | 7.56±2.54 | 7.13±2.89 | .21 |
| Total Number of Symptoms | |||
| (Mean±SD) | 8.36±3.62 | 7.48±3.65 | <.06 |
| Age, years | |||
| Mean (SD) | 67.1 (±13.2) | 62.3 (±13.6) | <.01 |
| Range | 39–97 | 24–90 | |
| Race/Ethnicity | |||
| Black | 27 (24%) | 24 (17%) | .28 |
| White (Non-Hispanic) | 80 (71%) | 111 (77%) | |
| Hispanic | 3 (3%) | 5 (3%) | |
| Asian/Pacific Islander | 0 | 3 (2%) | |
| Native American | 2 (2%) | 1 (1%) | |
| Education | |||
| <High School | 27 (24%) | 40 (28%) | .50 |
| High School diploma | 35 (31%) | 51 (35%) | |
| >More than High School | 50 (45%) | 53 (37%) | |
| Income* | |||
| ≤ $20,000 | 48 (43%) | 36 (25%) | .02 |
| $20.001–$50,000 | 35 (31%) | 56 (39%) | |
| >$50,000 | 12 (11%) | 35 (24%) |
Note: UA denotes unstable angina; NSTEMI denotes non ST-elevation myocardial infarction, and STEMI denotes ST-elevation myocardial infarction.
Qualitative Findings
Word Patterns Used by Patients
The manner in which the patient articulated their symptoms sometimes varied significantly from the language of clinicians. For example, patients made a decision to go to the ED because “the chest pain was irritating,” “ I was feeling funny,” “it hurt like hell,” “I had convulsions,” “I couldn’t get out of the chair,” “I got tired unloading pigs from a trailer,” “I got extremely fatigued throughout the day,” “the chest pain didn’t even go away after vomiting,” and “my throat tightened up when I was scraping a window.” However, the majority of patients used language similar to clinicians particularly the words “chest pain” and “shortness of breath.” Chest pain alone or in conjunction with other symptoms was noted in 36.5% of all responses.
Reasons for Seeking Care in the ED for Symptoms
When asked what made them decide to come to the ED, patients revealed specific symptoms, the severity or unremitting nature of the symptoms, and situational factors as reasons for seeking care when they did. Sixteen different symptoms were mentioned including typical symptoms such as chest pain, shortness of breath, and sweating and atypical symptoms such as convulsions, coughing, and upper back pain. Pain was most commonly described as discomfort, tightness, burning, pressure, and ache. Situational factors described related to time of day, location, or presence of a bystander. Nearly all of the 329 responses given by patients fit into one of five categories which were labeled; new onset of chest pain; ongoing evaluation of symptom severity; symptoms other than chest pain that worsened or were unrelieved; externally motivated; and internally motivated. The categories and examples of responses given by patients from each category are found in Table 2.
Table 2.
Reasons for Seeking Care in the Emergency Department.
| Category | Examples of Patient Reasons for Seeking Care in Their Own Words |
|---|---|
| 1. New onset of chest pain |
|
| 2. Ongoing evaluation of symptom severity |
|
| 3. Symptoms other than chest pain that worsened or were unrelieved |
|
| 4. Externally motivated |
|
| 5. Internally motivated |
|
Decision-Making by Category
New onset of chest pain
As expected, patients reported chest pain more than any other symptom. The quality of the pain was described in a number of ways. Descriptors mentioned repeatedly were constant or unrelenting pain, unrelieved pain, pain that increased in intensity, or pain that awakened the patient from sleep. Some patients appeared to reach a tipping point where the severity of pain or unrelenting nature of the pain pushed them into a decision to seek care in the ED. Chest pain alone was mentioned 53 times by patients as the reason they decided to seek care in the ED when they did. It was reported in conjunction with other symptoms another 67 times. Patients also used other chest descriptors including discomfort, tightness, burning, pressure, and aching, another 20 times. Of note, patients seldom reported chest pain in isolation. Rather they indicated that it was the primary symptom (or chief complaint) that caused them to come to the hospital.
Ongoing evaluation of symptom severity
Patients frequently monitored their symptoms but were often uncertain as to when to label their symptoms as serious or life threatening and make the decision to go to the ED. One participant stated that they “knew something was happening, something that could be deadly.” Over the counter medications such as antacids, Tylenol, aspirin, or ibuprofen were used with carbonated beverages or Epsom salts (mixed in water and taken by mouth). When these strategies failed to provide relief, or provided only temporary relief, patients relabeled their condition as serious and decided to go to the ED. Several patients thought that their illness could be fatal and either called 911 or drove to the ED.
Symptoms other than chest pain that worsened or were unrelieved
Other symptoms which caused distress or concern and resulted in a decision to seek care were, in order of most to least frequently reported; shortness of breath, sweating, arm pain, weakness, dizziness, indigestion, and vomiting. Also of note, the words fear, fright, scared, or afraid were frequently mentioned by participants. This sense of fear played a part in their reasoning and final decision to seek care. Symptoms other than chest pain which prompted a decision to go to the ED were mentioned 52 times, representing 15.8% of all reasons for making a decision to seek emergency treatment.
Externally motivated
In some instances the patient allowed others to make the decision to go to the ED for them. Patients were most likely to seek the opinion of family members when they became ill. Of particular interest, female relatives including wives, daughters, and sisters were most often consulted and usually insisted that patients seek emergency care. Rarely did a participant state that they consulted with a male relative. One participant who did consult a male relative stated that his son was a paramedic and was adamant that he call 911.
Internally motivated
Many patients decided early and independently to consult others about the severity of their symptoms. Under these circumstances, they called health care professionals, most often physicians. Without exception, they were told to call 911 or go to the ED. In one case a patient undergoing renal dialysis experienced symptoms and the dialysis nurse called 911. Other patients described monitoring their symptoms and seeking advice if they considered the illness to be serious or they had not previously experienced similar symptoms. One participant reported that “the chest pain was unrelieved with movement and when I started to sweat I felt it was time to go to the hospital”.
Quantitative Findings
Time to Presentation in the Emergency Department
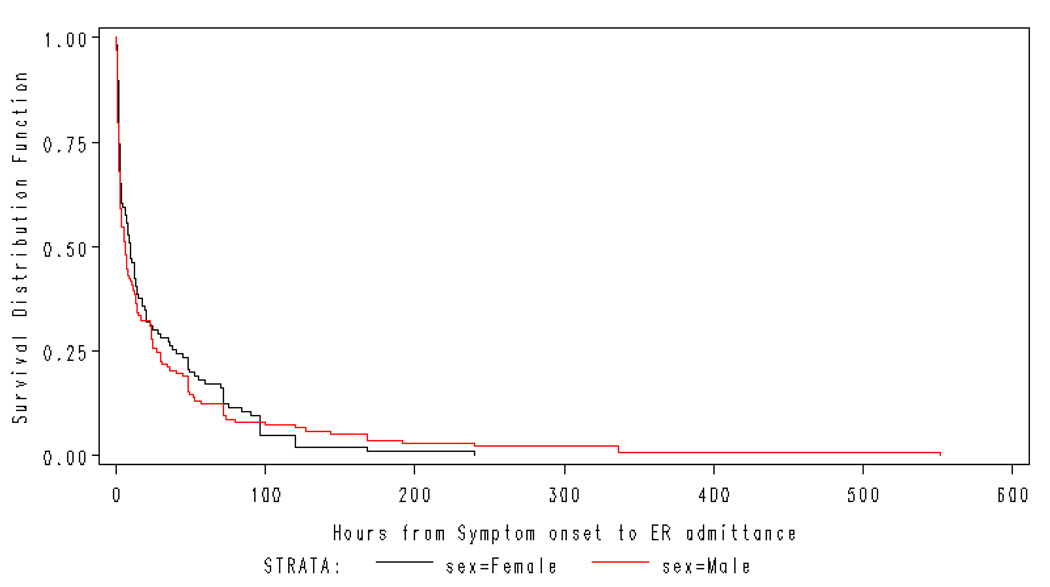
Time from symptom onset until presentation in the ED was available from 243 (95%) patients (Table 3). The majority of both women (61.6%) and men (53.5%) presented to the ED≥6 hours after symptom onset. Although women delayed longer in seeking treatment, there was no significant difference in median time from symptom onset to arrival in the ED between women and men (9.5 hours vs. 6 hours, log-rank test, p=.63). Even though a greater percentage of men arrived in the ED within three hours, they also exclusively delayed greater than 240 hours. The figure shows time to treatment for females and males using a Kaplan Meier Survival Curve.
Table 3.
Time of Symptom Onset to Arrival in Emergency Department
| Time to Presentation |
Female (%) (n=112) |
Male (%) (n=144) |
Total (%) (n=256) |
Cumulative Total (%) |
|---|---|---|---|---|
| < 1 hour | 2 (1.8) | 5 (3.5) | 7 (2.7) | 7 (2.7) |
| 1 to < 2 hours | 16 (14.3) | 29 (20.1) | 45 (17.6) | 52 (20.3) |
| 2 to < 3 hours | 12 (10.7) | 14 (9.7) | 26 (10.1) | 78 (30.4) |
| 3 to < 4 hours | 9 (8.0) | 10 (6.9) | 19 (7.4) | 97 (37.8) |
| 4 to < 5 hours | 4 (3.6) | 4 (2.8) | 8 (3.1) | 105 (40.9) |
| 5 to < 6 hours | 0 | 5 (3.5) | 5 (2.0) | 110 (42.9) |
| 6 to 96 hours | 56 (50) | 55 (38.2) | 111 (43.4) | 221 (86.3) |
| > 96 hours | 7 (6.3) | 15 (10.4) | 22 (8.6) | 243 (94.9) |
| Missing Data | 6 (5.4) | 7 (4.9) | 13 (5.1) | 256 (100) |
Factors Associated with Time to Treatment
Cox Proportional Hazards model showed differences between groups for time to treatment in the ED. Patients exhibiting constant pain sought treatment earlier than those with single instance or intermittent pain (Hazard Ratio=1.44, p=.01). Older patients sought treatment later than younger patients (Hazard Ratio=.99, p=.02). Even though the difference was statistically significant, the Hazard ratio indicates the difference may not be clinically significant. Finally, time to treatment for patients with STEMI was compared to patients with NSTEMI and UA in order to examine differences for patients with a complete occlusion requiring rapid reperfusion to those with an incomplete occlusion requiring medical interventions. Patients diagnosed with STEMI sought treatment earlier than those with unstable angina (Hazard Ratio=1.59, p=.004). The difference in time to presentation did not vary between patients with STEMI and NSTEMI (Hazard Ratio=.82, p=.21) (Table 4).
Table 4.
Patient Characteristics Affecting Time to Treatment in the Emergency Department
| Variable | Hazard Ratio |
P-value | 95% Hazard Ratio Confidence Limits |
|
|---|---|---|---|---|
| Older Age | 0.99 | .02 | 0.98 | .998 |
| Constant vs. Intermittent Symptoms | 1.44 | .01 | 1.10 | 1.89 |
| STEMI vs. Unstable Angina | 1.59 | .004 | 0.46 | 0.86 |
| STEMI vs. NSTEMI | 0.82 | .21 | 0.60 | 1.12 |
Note: STEMI=ST segment elevation myocardial infarction.
Discussion
The most important findings in this study were that intermittent pain and older age were associated with increased time to treatment. No prior studies were found associating the temporal nature of ischemic pain with time to treatment. This is important information for clinicians since the pain of myocardial ischemia can come and go or can be temporarily relieved with vasodilators or analgesics. Therefore nurses should caution patients at risk for an episode of ACS that pain may be intermittent and that they may be tempted to wait to go to the hospital or try to treat their symptoms at home. This additional delay could result in irreversible myocardial damage. Other investigators have reported a link between older age and additional delay in time to treatment 42,43 and this information should also be conveyed to older patients at risk for ACS.
Our findings had commonalities with Rosenfeld’s study of decision-making patterns in women with MI 10 in that we identified patients who decided independently to seek care and who tried to manage symptoms prior to making a decision to go to the ED. However, neither factor influenced time to presentation in the ED. Severity of symptoms, one factor linked to reduced time to treatment in prior studies 21,44 was frequently reported as a reason for seeking care but did not predict time to treatment in the ED. Unlike participants in Noureddine’s study (2008) 26, most of our patients recognized their symptoms as being serious or being of cardiac origin and eventually sought care in the ED. This is most likely attributable to sampling bias as admission to the hospital through the ED was a criterion for inclusion in the study. Even though all patients sought care in the ED, some consulted with a physician, family member, or acquaintance prior to arrival. Consultation has been associated with delayed treatment in previous studies 31,45,46 but was not significant in this sample.
The most troubling finding was that only 20.3 % of patients arrived in the ED in 2 hours or less. This is consistent with prior reports in the literature 15. Fifty-two percent of patients waited 6 or more hours to go to the ED, effectively closing the window of opportunity for reperfusion to rescue an ischemic myocardium. Importantly, women delayed 3.5 hours longer than men. While the difference was not statistically significant, it is clinically significant as demonstrated in the reduction of myocardial preservation and increased mortality 5,7.
An incidental finding was that patients with STEMI sought treatment sooner than patients with NSTEMI or unstable angina. Since type of ACS is not something that the patient could recognize, this finding requires further study. There may be some link between pathophysiological processes and appraisal of symptoms that impacts the decision to seek care more quickly for patients with STEMI.
Limitations
While the sample size, large number of females, and innovative analyses are strengths of the study there were limitations. Convenience sampling was used so it is possible that the sample does not represent the total population of ACS patients. Participants responded to two open-ended questions for the qualitative component of this study. They were permitted to respond at length but the investigators did not probe with follow-up questions in order to elicit more in-depth reasons for presenting to the ED. Access to care 28 was presumed for this sample since all participants presented to the ED, however we did not measure whether or not perceived access affected how quickly patients sought treatment. We also did not assess factors related to emergency medical services and insurance which could factor into a decision to go to the ED.
Recommendations for Future Study
Findings from this study and from other research sampling large heterogeneous populations and utilizing varied methodologies indicate time from symptom onset to presentation in the ED remains dangerously long. In this study, only 30% of patients arrived in the ED <3 hours from symptom onset. The consequences of this decision delay are often irreversible myocardial damage, long term morbidity, or death. Identifying factors that affect patients’ decision making may be the most useful strategy in developing interventions that are effective in changing patients’ propensity for delayed care seeking. Community-based health messages and interventions have not been effective in decreasing decision delay. Future research should focus on designing empirically derived, tailored interventions delivered to patients at high risk for ACS. Our findings suggest that special emphasis be given to women and older persons who are more likely to delay in seeking care and are at higher risk for poor outcomes. Interventions should include content on symptom perceptions and barriers and facilitators to behavior change.
Summary and Implications
Chest pain, alone and in conjunction with other symptoms, was the single most important symptom which factored into a patient’s decision to go to the ED. However, it was not mentioned in 63.5% of responses.
-
Chest pain was not predictive of time to treatment. Therefore, knowledge of chest pain alone as a symptom of heart disease is insufficient to reduce time to treatment.
Nurses should counsel patients with a prior diagnosis of coronary heart disease or who are at high risk that while chest pain is the hallmark symptom of ACS many patients do not experience chest symptoms during an episode.
-
Older patients and those with intermittent pain sought treatment later than younger patients and those with constant pain.
Nurses should caution patients that symptoms may come and go or not seem severe enough to warrant emergent care but delay brings the additional risk of sudden death, complications, or preclude patients from receiving time dependent interventions.
Nurses should reinforce with older patients that pain is not a normal consequence of aging and they should seek immediate treatment for new or suspicious symptoms.
-
New evidence of patients’ decision-making processes and response to symptoms during ACS provide additional evidence nurses need to counsel patients.
Nurses in both acute and non-acute settings can discuss the risk of delayed presentation to the ED, and offer encouragement for behaviors such as calling emergency medical services immediately when symptoms arise.
Note: Dark circle indicates summary of finding. Light circle indicates corresponding recommendation for practice.
Figure.
Kaplan Meier Survival Curve Representing Time to Presentation in the Emergency Department for Women and Men.
Note: Log Rank test, p=.63
Acknowledgements
This study was funded by the National Institute for Nursing Research (NIH)-R15 NR08870 and Loyola University Chicago. The authors would like to thank Dr. Sally Rankin and Dr. Mary Dawn Hennessey for their thoughtful critiques of the manuscript.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Holli A. DeVon, Associate Professor, Loyola University Chicago.
Nancy Hogan, Distinguished Professor, Loyola University Chicago.
Amy L. Ochs, Nurse Practitioner, Northwestern Medical Faculty Foundation, Chicago.
Moshe Shapiro, Biostatistician, Mount Sinai School of Medicine, New York.
References
- 1.World Health Organization. World Health Organization; The Atlas of Heart Disease and Stroke. 2008
- 2.Kung HC, Hoyert DL, Xu J, Murphy SL. [Accessed February 15, 2008];National Vital Statistics Reports: Deaths-Final Data for 2005. http://www.cdc.gov/nchs/deaths.htm. [PubMed]
- 3.American Heart Association. Heart Disease and Stroke Statistics-2008 Update. 2008 [Google Scholar]
- 4.Boersma E, Maas AC, Deckers JW, Simoons ML. Early thrombolytic treatment in acute myocardial infarction: reappraisal of the golden hour. Lancet. 1996;348(9030):771–775. doi: 10.1016/S0140-6736(96)02514-7. [DOI] [PubMed] [Google Scholar]
- 5.Giugliano RP, Braunwald E. Selecting the best reperfusion strategy in ST-elevation myocardial infarction: it's all a matter of time. Circulation. 2003;108(23):2828–2830. doi: 10.1161/01.CIR.0000106684.71725.98. [DOI] [PubMed] [Google Scholar]
- 6.Ribichini F, Steffenino G, Dellavalle A, et al. Comparison of thrombolytic therapy and primary coronary angioplasty with liberal stenting for inferior myocardial infarction with precordial ST-segment depression: immediate and long-term results of a randomized study. J Am Coll Cardiol. 1998;32(6):1687–1694. doi: 10.1016/s0735-1097(98)00446-x. [DOI] [PubMed] [Google Scholar]
- 7.Schomig A, Ndrepepa G, Mehilli J, et al. Therapy-dependent influence of time-to-treatment interval on myocardial salvage in patients with acute myocardial infarction treated with coronary artery stenting or thrombolysis. Circulation. 2003;108(9):1084–1088. doi: 10.1161/01.CIR.0000086346.32856.9C. [DOI] [PubMed] [Google Scholar]
- 8.McNamara RL, Wang Y, Herrin J, et al. Effect of door-to-balloon time on mortality in patients with ST-segment elevation myocardial infarction. J Am Coll Cardiol. 2006;47(11):2180–2186. doi: 10.1016/j.jacc.2005.12.072. [DOI] [PubMed] [Google Scholar]
- 9.Banks AD, Dracup K. Factors associated with prolonged prehospital delay of African Americans with acute myocardial infarction. Am J of Crit Care. 2006;15(2):149–157. [PubMed] [Google Scholar]
- 10.Rosenfeld AG. Treatment-seeking delay among women with acute myocardial infarction: decision trajectories and their predictors. Nurs Res. 2004;53(4):225–236. doi: 10.1097/00006199-200407000-00005. [DOI] [PubMed] [Google Scholar]
- 11.McSweeney JC, Lefler LL, Fischer EP, Naylor AJ, Jr, Evans LK. Women's prehospital delay associated with myocardial infarction: does race really matter? J Cardiovasc Nurs. 2007;22(4):279–285. doi: 10.1097/01.JCN.0000278958.98124.6e. [DOI] [PubMed] [Google Scholar]
- 12.Brieger D, Eagle KA, Goodman SG, et al. Acute coronary syndromes without chest pain, an underdiagnosed and undertreated high-risk group: insights from the Global Registry of Acute Coronary Events. Chest. 2004;126(2):461–469. doi: 10.1378/chest.126.2.461. [DOI] [PubMed] [Google Scholar]
- 13.Moser DK, Kimble LP, Alberts MJ, et al. Reducing delay in seeking treatment by patients with acute coronary syndrome and stroke: a scientific statement from the American Heart Association Council on cardiovascular nursing and stroke council. Circulation. 2006;114(2):168–182. doi: 10.1161/CIRCULATIONAHA.106.176040. [DOI] [PubMed] [Google Scholar]
- 14.Cooper RS, Simmons B, Castaner A, Prasad R, Franklin C, Ferlinz J. Survival rates and prehospital delay during myocardial infarction among black persons. Am J Cardiol. 1986;57(4):208–211. doi: 10.1016/0002-9149(86)90892-1. [DOI] [PubMed] [Google Scholar]
- 15.Taylor DM, Garewal D, Carter M, Bailey M, Aggarwal A. Factors that impact upon the time to hospital presentation following the onset of chest pain. Emerg Med Australasia. 2005;17(3):204–211. doi: 10.1111/j.1742-6723.2005.00724.x. [DOI] [PubMed] [Google Scholar]
- 16.Goldberg RJ, Steg PG, Sadiq I, et al. Extent of, and factors associated with, delay to hospital presentation in patients with acute coronary disease (the GRACE registry) Am J Cardiol. 2002;89(7):791–796. doi: 10.1016/s0002-9149(02)02186-0. [see comment] [DOI] [PubMed] [Google Scholar]
- 17.Luepker RV, Raczynski JM, Osganian S, et al. Effect of a community intervention on patient delay and emergency medical service use in acute coronary heart disease: The Rapid Early Action for Coronary Treatment (REACT) Trial. JAMA. 2000;284(1):60–67. doi: 10.1001/jama.284.1.60. [DOI] [PubMed] [Google Scholar]
- 18.Dracup K, Alonzo AA, Atkins JM, et al. The physician's role in minimizing prehospital delay in patients at high risk for acute myocardial infarction: recommendations from the National Heart Attack Alert Program. Working Group on Educational Strategies To Prevent Prehospital Delay in Patients at High Risk for Acute Myocardial Infarction. Ann Intern Med. 1997;126(8):645–651. doi: 10.7326/0003-4819-126-8-199704150-00010. [Review] [61 refs] [DOI] [PubMed] [Google Scholar]
- 19.Rosenfeld AG, Lindauer A, Darney BG. Understanding treatment-seeking delay in women with acute myocardial infarction: descriptions of decision-making patterns. Am J Crit Care. 2005;14(4):285–293. [PubMed] [Google Scholar]
- 20.Khraim FM, Carey MG. Predictors of pre-hospital delay among patients with acute myocardial infarction. Patient Educ & Counseling. 2008 Nov 24; doi: 10.1016/j.pec.2008.09.019. [DOI] [PubMed] [Google Scholar]
- 21.Goff DC, Jr, Feldman HA, McGovern PG, et al. Prehospital delay in patients hospitalized with heart attack symptoms in the United States: the REACT trial. Rapid Early Action for Coronary Treatment (REACT) Study Group. Am Heart J. 1999;138(6 Pt 1):1046–1057. doi: 10.1016/s0002-8703(99)70069-4. [DOI] [PubMed] [Google Scholar]
- 22.Goldberg R, Goff D, Cooper L, et al. Age and sex differences in presentation of symptoms among patients with acute coronary disease: the REACT Trial. Rapid Early Action for Coronary Treatment. Coron Artery Dis. 2000;11(5):399–407. doi: 10.1097/00019501-200007000-00004. [DOI] [PubMed] [Google Scholar]
- 23.Zerwic JJ, Ryan CJ, DeVon HA, Drell MJ. Treatment seeking for acute myocardial infarction symptoms: differences in delay across sex and race. Nurs Res. 2003;52(3):159–167. doi: 10.1097/00006199-200305000-00005. [DOI] [PubMed] [Google Scholar]
- 24.Noureddine S. Gender differences in the responses to symptoms of acute coronary syndromes in a Lebanese sample. Eur J Cardiovascular Nurs. 2006;5 S29-S29. [Google Scholar]
- 25.Banks AD, Malone RE. Accustomed to enduring: experiences of African-American women seeking care for cardiac symptoms. Heart & Lung. 2005;34(1):13–21. doi: 10.1016/j.hrtlng.2004.08.001. [DOI] [PubMed] [Google Scholar]
- 26.Noureddine S, Arevian M, Adra M, Puzantian H. Response to signs and symptoms of acute coronary syndromes: Differences between Lebanese men and women. Am J Crit Care. 2008;17(1):26–35. [PubMed] [Google Scholar]
- 27.Horne R, James D, Petrie K, Weinman J, Vincent R. Patients' interpretation of symptoms as a cause of delay in reaching hospital during acute myocardial infarction. Heart. 2000;83(4):388–393. doi: 10.1136/heart.83.4.388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kaur R, Lopez V, Thompson DR. Factors influencing Hong Kong Chinese patients' decision-making in seeking early treatment for acute myocardial infarction. Res Nurs Health. 2006;29(6):636–646. doi: 10.1002/nur.20171. [DOI] [PubMed] [Google Scholar]
- 29.Dempsey SJ, Dracup K, Moser DK. Women's decision to seek care for symptoms of acute myocardial infarction. Heart & Lung. 1995;24(6):444–456. doi: 10.1016/s0147-9563(95)80022-0. [DOI] [PubMed] [Google Scholar]
- 30.Perkins-Porras L, Whitehead DL, Strike PC, Steptoe A. Causal beliefs, cardiac denial and pre-hospital delays following the onset of acute coronary syndromes. J Behav Med. 2008;31(6):498–505. doi: 10.1007/s10865-008-9174-3. [DOI] [PubMed] [Google Scholar]
- 31.Pattenden J, Watt I, Lewin RJ, Stanford N. Decision making processes in people with symptoms of acute myocardial infarction: qualitative study. BMJ. 2002;324(7344):1006–1009. doi: 10.1136/bmj.324.7344.1006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Arslanian-Engoren C. Treatment-seeking decisions of women with acute myocardial infarction. Women Health. 2005;42(2):53–70. doi: 10.1300/j013v42n02_04. [DOI] [PubMed] [Google Scholar]
- 33.Antman EM. Time is muscle: translation into practice. J Am Coll Cardiol. 2008;52(15):1216–1221. doi: 10.1016/j.jacc.2008.07.011. [DOI] [PubMed] [Google Scholar]
- 34.De Luca G, van 't Hof AW, de Boer MJ, et al. Time-to-treatment significantly affects the extent of ST-segment resolution and myocardial blush in patients with acute myocardial infarction treated by primary angioplasty. Eur Heart J. 2004;25(12):1009–1013. doi: 10.1016/j.ehj.2004.03.021. [DOI] [PubMed] [Google Scholar]
- 35.DeVon HA, Ryan CJ, Ochs AL, Shapiro M. Symptoms across the continuum of acute coronary syndromes: differences between women and men. Am J Crit Care. 2008;17(1):14–25. [PMC free article] [PubMed] [Google Scholar]
- 36.Lloyd-Jones D, Adams R, Carnethon M, et al. Heart disease and stroke statistics--2009 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2009;119(3):480–486. doi: 10.1161/CIRCULATIONAHA.108.191259. [DOI] [PubMed] [Google Scholar]
- 37.Alpert JS, Thygesen K, Antman E, Bassand JP. Myocardial infarction redefined--a consensus document of The Joint European Society of Cardiology/American College of Cardiology Committee for the redefinition of myocardial infarction. J Am Coll Cardiol. 2000;36(3):959–969. doi: 10.1016/s0735-1097(00)00804-4. [DOI] [PubMed] [Google Scholar]
- 38.Sandelowski M. Whatever happened to qualitative description? Res Nurs Health. 2000;23(4):334–340. doi: 10.1002/1098-240x(200008)23:4<334::aid-nur9>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 39.Polit DF, Beck CT. Nursing research: generating and assessing evidence for nursing practice. 8th ed. Wolters Kluwer Health/Lippincott Williams & Wilkins; [Google Scholar]
- 40.Katz MH. Multivariable Analysis: A Practical Guide for Clinicians. Cambridge, UK: Cambridge University Press; 2002. [Google Scholar]
- 41.Spencer FA, Fonarow GC, Frederick PD, et al. Early withdrawal of statin therapy in patients with non-ST-segment elevation myocardial infarction: national registry of myocardial infarction. Arch Intern Med. 2004;164(19):2162–2168. doi: 10.1001/archinte.164.19.2162. [DOI] [PubMed] [Google Scholar]
- 42.Lefler LL, Bondy KN. Women's delay in seeking treatment with myocardial infarction: a meta-synthesis. J Cardiovasc Nurs. 2004;19(4):251–268. doi: 10.1097/00005082-200407000-00005. [DOI] [PubMed] [Google Scholar]
- 43.Rosenfeld AG. Women's risk of decision delay in acute myocardial infarction: implications for research and practice. AACN Clin Issues. 2001;12(1):29–39. doi: 10.1097/00044067-200102000-00005. [DOI] [PubMed] [Google Scholar]
- 44.Dracup K, Moser DK. Beyond sociodemographics: factors influencing the decision to seek treatment for symptoms of acute myocardial infarction. Heart & Lung. 1997;26(4):253–262. doi: 10.1016/s0147-9563(97)90082-0. [DOI] [PubMed] [Google Scholar]
- 45.Hutchings CB, Mann NC, Daya M, et al. Patients with chest pain calling 9-1–1 or self-transporting to reach definitive care: which mode is quicker? Am Heart J. 2004;147(1):35–41. doi: 10.1016/s0002-8703(03)00510-6. [see comment] [DOI] [PubMed] [Google Scholar]
- 46.Zapka J, Estabrook B, Gilliland J, et al. Health care providers' perspectives on patient delay for seeking care for symptoms of acute myocardial infarction. Health Educ & Behavior. 1999;26(5):714–733. doi: 10.1177/109019819902600511. [DOI] [PubMed] [Google Scholar]