Abstract
Background
Persons with mental disorders frequently have other co-occurring problems such as substance related disorders and HIV/AIDS. Individuals with co-occurring medical and mental disorders encounter great obstacles to receiving mental health services.
Aims
This paper uses the Behavioral Model of Vulnerable Populations to evaluate use of mental health services among groups with co-occurring disorders (CODs) and other co-morbid relationships. The association between receipt of mental health treatment and traditional/vulnerable predisposing, enabling, and need factors are examined.
Methods
Bivariate analysis and two-stage hierarchical logistic regression were completed.
Resutls
A sample of 553 persons who reported mental health problems within the past year had one or more of the following vulnerabilities: (1) substance disorders; (2) homelessness; (3) victims of violent crime; (4) diagnosed with HIV/AIDS; (5) recipient of public benefits; and 31.3% reported having received some form of mental health treatment. Both traditional and vulnerable characteristics are significant predictors of receipt of mental health treatment. Vulnerable predictors indicated decreased odds of receiving mental health treatment were associated with injection and chronic drug use, (OR = .42, CI: .22 – .77) and (OR = .38, CI: .22 – .64) respectively.
Conclusion
The Behavioral Model of Vulnerable Populations could be employed in future research of CODs and other co-morbid group’s utilization of mental health treatment.
Keywords: behavioral model of health services utilization, co-occurring disorders (CODs), mental health treatment, multiple vulnerabilities
Introduction
Mental disorders are serious and persistent health problems that are common in the general population and often result in reduced access to and utilization of health services. Many people with mental disorders remain untreated despite the distress and impairment associated with their diagnoses and the availability of effective therapies (American Psychiatric Association: APA, 2000; Wang et al., 2005a; 2005b). Approximately half of the US population meets criteria for a form of mental disorder during their life course, (Kessler & Wang, 2008; Ro & Shum, 2001) with onset usually in childhood or adolescence (Kessler et al., 2005a). However, individuals with mental disorders frequently have co-occurring social and/or medical problems such as substance related disorders and HIV/AIDS. As a group, these individuals face obstacles to receiving health care and those with co-occurring medical, social, and psychiatric problems encounter even greater obstacles.
Several community epidemiological surveys over nearly three decades have illustrated stagnant prevalence rates for mental disorders in the adult population (Kessler et al., 2005b; Kessler et al., 2005c; Kessler & Wang, 2008). Data from the 1980’s Epidemiological Catchment Area (ECA) Study (Robins & Regier, 1991), the 1990’s National Co-morbidity Survey (NCS: Kessler et al., 1994), followed by the 2000’s National Co-Morbidity Survey Replication (NCS-R: Kessler & Wang, 2008) indicate a prevalence of approximately 30% among the U.S. adult population has remained constant. While the prevalence of mental disorders has not wavered, the prevalence of treatment has increased in the general population, but not within this population (Kessler et al., 2005b; Kessler et al., 2008; Wang et al., 2005b). As the research presented in this paper was conducted in the US, all of the epidemiology, policies, and treatment discussed are placed in cultural context.
The latest findings from the NCS-R (Kessler et al., 2008) suggest that this unmet need for mental health treatment has resulted in: 1) in an estimated $193 billion annual loss in earnings; 2) delays in seeking initial treatment after the onset of the disorder ranging from 6 to 23 years (Wang et al., 2005a); and 3) indications that unmet need for treatment is greatest among vulnerable traditionally underserved groups (Wang et al., 2005b). Though mental disorders are highly prevalent in the general populace, many of the most serious cases are concentrated among those with co-morbidities (Kessler et al., 2005b), often from vulnerable underserved groups.
Numerous research initiatives have been undertaken in an effort to understand barriers to enrollment and utilization of mental health treatment among those with vulnerable co-morbidities (e.g. Burnam, 2001; Compton et al., 2003; McQuistion et al., 2003). Some of the most notably examined co-morbidities exist between people experiencing mental health disorders and: substance abuse (Curran et al., 2000); homelessness (Compton et al., 2003); who are victims of violent crime (Choe, Teplin, & Abram, 2008); diagnosed with HIV/AIDS (Burnam, 2001); and in receipt of public benefits. While extensive research has been completed on these vulnerable groups and the factors influencing their utilization of mental health services, it is important to point out that these vulnerable categorizations are not mutually exclusive; many with mental illness can experience more than one vulnerability.
This paper uses the Behavioral Model for Vulnerable Populations to evaluate the use of mental health services among a sample of persons with one or more vulnerable health designations who reported mental health problems within the past year. Reported vulnerabilities include persons:
with substance use disorders;
experiencing homelessness;
who are victims of violent crime;
diagnosed with HIV/AIDS;
in receipt of public benefits.
Behavioral Model for Vulnerable Populations
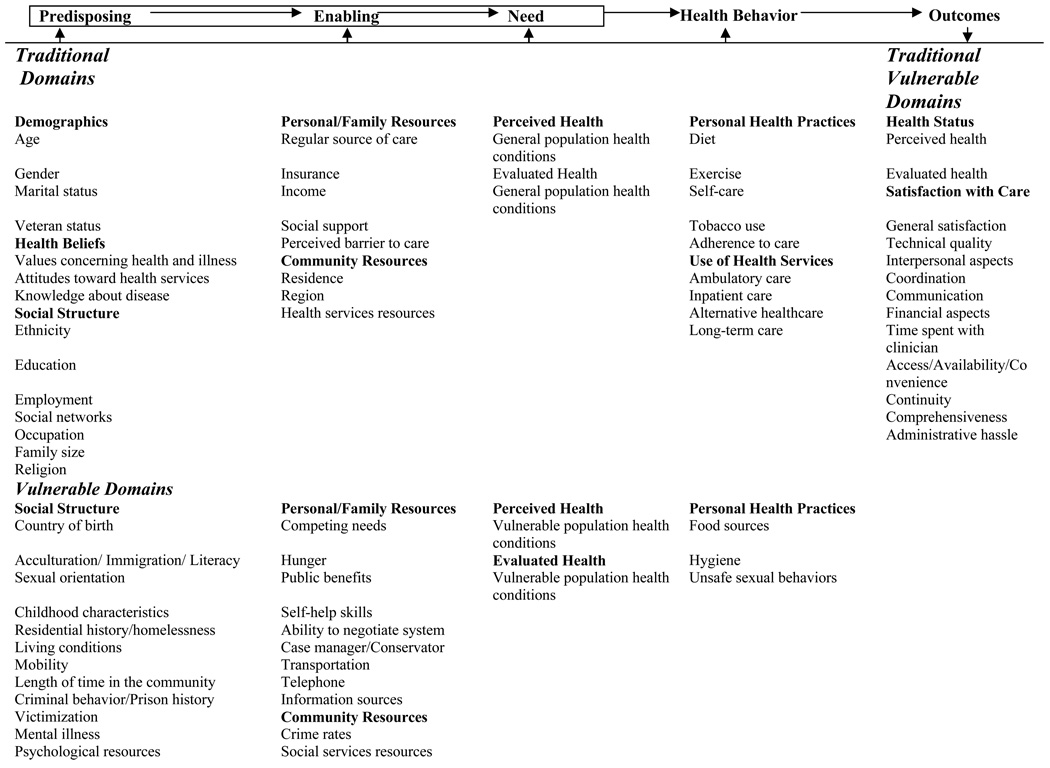
Since its development, the Behavioral Model of Health Services Utilization (Andersen & Newman, 1973) has undergone numerous revisions, updates and variations in response to changing research interests and a changing health care industry (Andersen, 1995; Gelberg et al., 2000). The model describes three distinct categorical determinants of utilization. These major components of the model describe: (a) social determinants or prevailing norms for response to illness; (b) characteristics of the healthcare system; and (c) individual determinants of health care utilization. Individual determinants include predisposing factors, enabling (or impeding) factors, and measures of need for service (Andersen, 1995; Andersen & Newman, 1973). Predisposing factors include demographic factors prior to the onset of illness. Enabling factors permit an individual to secure services and address a health need and include factors such as insurance and income. Lastly, need factors include an individual perception of illness, preferably influenced by physician’s evaluation.
A relatively recent variation of the model, which is central to the research presented here, distinguishes between traditional and vulnerable predisposing, enabling or impeding, and need factors. The Behavioral Model for Vulnerable Populations (see Figure 1), developed by Lillian Gelberg and Ronald Andersen (Gelberg, Andersen, & Leake, 2000), introduces vulnerable domains (predisposing, enabling, and need) that focus on social structure and enabling resources that are especially relevant to understanding the health and health-seeking behavior of vulnerable populations. The premise of this model is that obtaining preventive services and monitoring health problems may have low priority when people experience a multitude of daily problems (Gelberg, Andersen, & Leake, 2000).
Figure 1.
Behavioral Model for Vulnerable Populations
The model suggests that vulnerability influences a person’s ability and opportunity to seek healthcare services. According to the revised model, predisposing factors that place individuals in a vulnerable position with respect to their ability to receive treatment include a history of substance abuse, mental health problems, homelessness, and a history of victimization. Vulnerable enabling factors include receipt of public benefits and use of information resources (Gelberg et al., 1997; Gelberg, Andersen, & Leake, 2000; Lim et al., 2002; Gelberg & Leake, 1993). Much like the original model, vulnerable need factors include perceived and evaluated health needs and conditions.
Numerous factors that influence access to treatment are associated with characterizing persons with mental health disorders as a vulnerable population. (Lu Ann Aday 1994; 1997; 2001; Aday, Fleming, & Anderson, 1984) describes vulnerable health populations as having ‘community and associated individual characteristics that are risk factors predictive of poor physical, psychological, and social health’. Many of the most serious cases of mental health disorders are concentrated among those with co-morbidities (Kessler et al., 2005b) often belonging to vulnerable underserved groups.
This paper uses the Behavioral Model for Vulnerable Populations (Gelberg, Andersen, & Leake, 2000) to evaluate the influence of traditional and vulnerable characteristics on individuals' receipt of mental health services among persons that reported mental health problems within the past year and experienced one or more vulnerable health designations. Respondents who reported mental health problems and who have one or more characterized vulnerabilities (have substance related disorders, have HIV/AIDS, are homeless, have been violently victimized, and are recipients of public benefits) were selected for inclusion.
In contrast to past studies that focus on specific co-morbidities, this study evaluates the effect of both traditional and vulnerable characteristics on the receipt of mental health treatment among persons with reported mental health problems in the past 12 months who have one or more vulnerable health characteristics. As research on barriers and rationale for not entering mental health treatment continues, the multifaceted and often interconnected nature of these vulnerabilities among those with mental health disorders must be evaluated.
Methods
Sample Recruitment
Data used in this study were collected as part of a parent study, Epidemiology of Health Care Utilization Study (EHCUS), and funded by the National Institute of Drug Abuse (NIDA). A primary objective of this study was to investigate health services needs and use patterns of drug users. The sample is tri-ethnic (African American, White, and Hispanic) and comprised of men and women over the age of 18. This sample of 553 includes persons who reported mental health problems within the past year and experienced one or more of the following vulnerable health designations:
1) persons with substance disorders 1(injection and chronic drug users);
2) homeless persons;
3) victims of violent crime;
4) persons diagnosed with HIV/AIDS;
5) or recipients of public benefits.
Participants were initially contacted by outreach workers with an average of five or more years of experience with vulnerable populations in the state of Florida, US. The participants in the study were recruited between April 1996 and September 1997 using a stratified, two-stage, network-based sample (Chitwood et al., 1998, 1999; Chitwood, Comerford, & McCoy, 2002). Qualifying participants were notified that the study concerned their past and present health care, assured confidentiality, and were then invited to participate in the study (Chitwood et al., 1998).
Data Collection
Institutional Review Board (IRB) approval was granted by the University of Miami for this study. Participants were transported to an outreach/assessment center where comprehensive screening was completed. The Health Services Research Instrument (HSRI) was administered by a trained interviewer in a private setting. Interviews took about one-and-a-half hours on average. The interview questions focused on different types of health care needs and utilization. On completion of the study, participants were compensated $20 for participation.
Measures
The dependent variable used in this analysis is a dichotomous measure of mental health treatment that stems from the survey question: ‘In the past twelve months, have you seen a doctor or health care provider for any mental health problems?’ This outcome was examined for persons who reported mental health problems within the past year (n = 553). This variable is coded ‘0’ for not having seen a provider for mental health treatment in the past twelve months and ‘1’ for having seen a provider for mental health treatment in the past twelve months. Sixteen independent variables from the vulnerable and traditional domains of the ‘Gelberg and Andersen Behavioral Model for Vulnerable Populations’ were included in the hierarchal logistic models and were informed by previous research (Booth, Kwiatkowski, & Weissman, 1999; Gelberg, Andersen, & Leake, 2000). The order of entry of variables for analyses is: 1) traditional predisposing, enabling/impeding and need variables (age, gender, race, marital status, educational level, employment status, insurance coverage, income level, regular source of care, and perceived health status); and 2) vulnerable predisposing, enabling/impeding variables (homeless, substance abuse, mental health problem, HIV/AIDS, victimization, receipt of public benefits).
Analyses
To determine the influence of vulnerable and traditional predisposing, enabling/impeding and need factors on the probability of receiving mental health treatment in the past 12 months, a two-stage hierarchical logistic regression was completed using SPSS Version 15. Tolerance levels and variance inflation factors indicated no collinearity issues were associated with any of the models. Linearity of the logit for age was analyzed using the Box–Tidwell transformation tests and was not a violation of logistic regression (Hosmer & Lemeshow, 2002; Menard, 2002; Pampel, 2000). Bonferroni corrections for race were applied, and a p-value of 0.016 was used to establish correlations between race and mental health treatment. This correction is important because multiple comparisons across variables can lead to spurious significance (Perneger, 1998). Odds ratios and 95% confidence intervals are presented for all variables in the final models.
Results
Receipt of mental health treatment in the past 12 months
In Table 1, sixteen independent variables are cross-tabulated with the self-reported receipt of mental health treatment within the past 12 months. Only 173 (31.3%) of the 553 respondents who reported experiencing mental health problems within the past 12 months reported having received some form of mental health treatment. Examination of traditional characteristics indicates that women (38.7%) were more likely to receive mental health treatment than men (24.3%). Likewise, those unemployed (38.2%) reported higher rates of receipt of mental health treatment compared than those who were employed (14.7%).
Table 1.
Respondents receiving mental health treatment in the past 12 months by predisposing, enabling, and need factors
| Characteristics | n = 553 | Mental Health % (number) |
p-values |
|---|---|---|---|
| Traditional Predisposing | |||
| Age (mean years) | 37.3 | ||
| Gender | < 0.001 | ||
| Male | 24.3 (284) | ||
| Female | 38.7 (269) | ||
| Race | .134 | ||
| Non-Hispanic White | 23.2 (168) | ||
| Black | 31.3 (150) | ||
| Hispanic | 37.0 (235) | ||
| Marital Status | .160 | ||
| Married | 25.7 (109) | ||
| Not Married | 32.7 (444) | ||
| Education | .362 | ||
| < High School | 33.0 (291) | ||
| ≥ High School | 29.4 (262) | ||
| Employment | < 0.001 | ||
| Employed | 14.7 (163) | ||
| Not Employed | 38.2 (390) | ||
| Vulnerable Predisposing | |||
| Housing status | .001 | ||
| Homeless | 20.8 (149) | ||
| Not Homeless | 35.1 (404) | ||
| Substance Abuse Status | < 0.001 | ||
| Injection Drug User | 25.2 (155) | ||
| Chronic Drug User | 24.5 (253) | ||
| Non-Drug User | 49.7 (145) | ||
| Ever told has HIV/AIDS | .008 | ||
| No | 29.5 (495) | ||
| Yes | 46.6 (58) | ||
| History of Victimization | .061 | ||
| No | 29.0 (403) | ||
| Yes | 37.3 (150) | ||
| Traditional Enabling/Impeding | |||
| Health Insurance Coverage | < 0.001 | ||
| No | 14.3 (231) | ||
| Yes | 43.6 (321) | ||
| Income | .029 | ||
| < $5,000 | 27.6 (319) | ||
| ≥ $5,000 | 36.3 (234) | ||
| Regular source of care | < 0.001 | ||
| No | 8.0 (188) | ||
| Yes | 43.3 (365) | ||
| Vulnerable Enabling /Impeding | |||
| Receipt of public benefits | < 0.001 | ||
| No | 23.2 (280) | ||
| Yes | 39.6 (273) | ||
| Need | |||
| Perceived health | .399 | ||
| Excellent to good | 29.5 (264) | ||
| Fair to poor | 32.9 (289) |
n = 553 Note: HIV/AIDS= Human Immunodeficiency Virus/Acquired Immune Deficiency Syndrome ~ Applies only to those who experienced mental health problems in the past 12 months.
Overall, findings indicate that respondents possessing traditional enabling characteristics were more apt to report the receipt of mental health treatment. Health insurance, individual income, and having a regular source of care were positively correlated with the receipt of treatment at a p-value of 0.05 or lower. Examination of vulnerable characteristics indicates that those who were not homeless (35.1%) and not persons with substance disorders (49.7%) were more likely to report receiving mental health treatment. Receipt of public benefits (39.6%) was positively correlated with receiving mental health treatment in the past 12 months. First-order interactions between covariates, may be influencing the dependent variable response, therefore all independent variables, including those not significant in the bivariate analysis, were entered into the hierarchical logistic regression models (see Table 2).
Table 2.
Multivariate logistic models of factors that affect the use of mental health treatment in the past 12 months
| Characteristics | Traditional & Need Covariates OR (95%) 1 |
+ Vulnerable Covariates OR (95%) 2 |
|---|---|---|
| Traditional Predisposing | ||
| ≥ 35 years of age | 2.80*** (1.76 – 4.44) | 2.93*** (1.80 – 4.77) |
| Female | 1.94** (1.23 – 3.06) | 1.46 (.86 – 2.46) |
| Non-Hispanic White | .99 (.55 – 1.76) | .96 (.51 – 1.77) |
| Hispanic | 2.21** (1.33 – 3.69) | 2.28** (1.33 – 3.92) |
| Married | .47** (.27 – .83) | .48* (.27 – .85) |
| High School | 1.08 (.70 – 1.66) | 1.12 (.71 – 1.75) |
| Employed | .37*** (.21 – .64) | .39** (.22 – .68) |
| Traditional Enabling | ||
| Uninsured | .48** (.29 – .81) | .53* (.31 – .92) |
| Income≥ $5,000 | 1.55 (.99 – 2.41) | 1.49 (.94 – 2.35) |
| Regular Source of Care | 6.30*** (3.34 – 11.89) | 5.65*** (2.94 – 10.84) |
| Need | ||
| Perceived Health/Poor-Fair | .78 (.50 – 1.20) | .85 (.54 – 1.33) |
| Vulnerable Predisposing | ||
| Homeless | ---- | 1.05 (.60 – 1.85) |
| Injection Drug User | ---- | .42** (.22 – .77) |
| Chronic Drug User | ---- | .38*** (.22 – .64) |
| Ever told has HIV/AIDS | ---- | 1.37 (.70 – 2.73) |
| History of Victimization | ---- | 1.75* (1.00 – 3.05) |
| Vulnerable Enabling | ||
| Receipt of public benefits | ---- | 1.08 (1.00 – 1.71) |
| −2 log likelihood | 527.20 | 509.74 |
| R2 | .35 | .39 |
Chi-Square test: p < .05*, p < .01**, p < .001***; n= 553; Note: Health HIV/AIDS=Human Immunodeficiency Virus/Acquired Immune Deficiency Syndrome −2 log likelihood model 1= joint significant of traditional variables; −2 log likelihood model 2 = joint significant of traditional and vulnerable variables Reference Groups: age ≤ 35 years, Male gender, Blacks, not married, ≤ High School, not Employed, Insured, Income ≤ $5,000; no regular source of care, perceived health-excellent to good; not homeless; non-drug user; no HIV/AIDS; no history of victimization; no receipt of public benefits
Multivariate Analyses
The first logistic model is designed to assess the joint significance of traditional and need covariates on the use of mental health treatment in the past 12 months. Age, race, gender, marital status, employment status, insurance status, and a regular source of care (whether or not respondents have a clinic, health center, doctor’s office, or other place that they usually attend if they are sick or need advice about their health within the past 12 months) remained independently associated with the receipt of mental health treatment in the past 12 months. According to this model, increased odds of receiving mental health treatment are associated with being age 35 years and older, female gender, and being Hispanic. Hispanics reported the receipt of mental health treatment two times more than Blacks and non-Hispanic whites (CI: 1.33 – 3.69). Decreased odds of receiving mental health treatment are associated with being married (OR = .47, CI: .27 – .83), employed (OR = .37, CI: .21 – .64), and uninsured (OR = .48, CI: .29 – .81). Those who reported a regular source of care were more than six times as likely as those without a regular source of care to report use of mental health treatment (OR = 6.30, CI: 3.34 – 11.89).
The second logistic model is designed to assess the joint significance of traditional and vulnerable covariates on the receipt of mental health treatment. Of the newly introduced vulnerable enabling and predisposing covariates in model 2, a history of victimization and substance use remain independent risk factors for the receipt of mental health treatment within the past 12 months. According to the model, substance users are less likely to employ the use of mental health services. Decreased odds of receiving mental health treatment were associated with injection and chronic drug users, (OR = .42, CI: .22 – .77) and (OR = .38, CI: .22 – .64) respectively. Respondents with a history of victimization were nearly twice as likely to receive mental health treatment (OR = 1.75, CI: 1.00 – 3.05). The addition of vulnerable covariates in the second model increases the overall fit of the model (−2 log likelihood of 509.74) and strengthened the association between most traditional (predisposing and enabling) covariates that were predictors of mental health treatment in model one.
Discussion
This study employed Gelberg and Andersen’s Behavioral Model for Vulnerable Populations (Gelberg, Andersen, & Leake, 2000) to investigate the receipt of mental health treatment among persons who reported mental health problems within the past year and experienced additional vulnerable health designation. Although effective treatments are available, many people experiencing mental health disorders, such as those included in this study, will go untreated. It is important to note that among the 553 respondents who reported experiencing mental health problems, very few (31.3%) reported having received some form of mental health treatment. Two primary findings emerged from this study. First, receipt of mental health treatment was predicted by both traditional and vulnerable covariates in the model. Secondly, the use of mental health treatment differed by type of vulnerable co-morbid relationship.
Traditional characteristics that focus on demographic differences among recipients of mental health services are consistent with published reports as to who receives treatment. Decreased odds of obtaining mental health treatment were associated with being married (Berkman, 1995; Berkman & Glass, 2000), employed, and having no health insurance coverage (Wells et al., 2002). The President’s New Freedom Commission on Mental Health (U.S. Department of Health and Human Services: USDHHS, 2003) and the Surgeon General’s Report (USDHHS, 1999) are two national reports that advocate for change to an ailing U.S. mental health system. It is worthy of note that inadequate health insurance coverage for mental health disorders is highlighted in both reports. Consequently, in 2008, policy makers enacted the Wellstone-Domenici Mental Health Parity and Addiction Equity Act (US Congress, 2008; to take effect in 2010) designed to provide equitable access to care and reduce currently restrictive limits to mental health services. Provisions of this act could help increase insurance coverage and reduce financial barriers to treatment leading to a notable increase in use of mental health services. Increased odds of obtaining care were associated with being 35 or older (USDHHS, 1999), and being of female gender (Collins et al., 1999; USDHHS, 1999). Having a regular source of care and help in accessing the formal mental health treatment systems proved to be the most important factor (Koegel et al., 1999; Ro & Shum, 2001) and increased the likelihood of treatment nearly six fold.
The addition of vulnerable predisposing and enabling covariates improved the model’s ability to predict mental health treatment. However, use of mental health services differed according to vulnerable co-morbidities. Respondents with mental health disorders and a history of violent victimization were nearly two times more likely than those not victimized to report receiving mental health treatment. This pattern may be due to fully developed social service programs and informal networks that provide necessary referrals and, sometimes, free access to mental health services for persons who have experienced violent trauma (Ullman & Breclin, 2003; Green et al., 2000). Conversely, respondents with mental health disorders who are chronic and injection drug users (compared to non-drug users) were less likely to receive mental health services. The social service programs that provide mental health services to victims of violent traumas are not readily available to substance users. Thus, it appears that this group has an especially high level of unmet needs. The findings from this study are consistent with previous studies that have demonstrated that drug users (compared with non drug users) are at a disadvantage in regards to receiving needed health care services (Chitwood et al., 1998; Chitwood et al., 1999; McCoy, Metsch, & Chitwood, 2000) and have unmet needs for health care (Chitwood et al., 1999; Metsch et al., 2002). While mental health disorders are recognized as a leading cause of disability, inadequate resources have been dedicated to addressing the issues of behavioral health among those with CODs.
Limitations
The data on health care utilization contained in the EHCUS are based upon participants’ self-reports. Self-reporting can lead to recall bias and prevarication in the data. Moreover a non-probability (affinity) sample was used to recruit study participants, which can limit generalizability. While not representative of vulnerable groups nationwide, this study does depict the mental health treatment utilization patterns of vulnerable groups in the Miami–Dade Florida metropolitan area.
Conclusion
This report addresses a significant gap in existing literature on mental health treatment among members of vulnerable populations. In contrast to previous publications, this study evaluates the effect of multiple traditional and vulnerable characteristics on the receipt of mental health services. Findings from this study suggest the Behavioral Model of Vulnerable Populations (Gelberg, Andersen, & Leake, 2000) could be employed in future research regarding mental health treatment utilization among vulnerable populations. The use of a two-stage hierarchical logistic regression with this model allowed for some interesting findings. First, having a history of violent victimization was not a significant covariate in initial bivariate analysis, but proved to be one of the most significant predisposing vulnerable predisposing variables influencing receipt of mental health treatment. Furthermore, gender proved not to be a significant factor in receipt of mental health treatment as vulnerable covariates were introduced into the analysis. The addition of vulnerable covariates to the model allows for the recognition of differing patterns of mental health treatment utilization and various factors that contribute to this utilization. However, while this study does not categorize vulnerabilities by number, further research is needed to examine the impact of increased numbers of vulnerabilities on mental health treatment.
Similarly, further research should be completed on pathways to mental health treatment in order to investigate why certain factors (such as substance use among CODs) that increase the risk of mental health problems do not simultaneously increase likelihood of receipt of mental health treatment. Since differing types of mental health problems may increase or decrease health care utilization, renewed focus on the type of mental health problems that exist among these vulnerable groups and on how best to increase mental health treatment should be implemented. Issues associated with access to and traversing entrance to mental health treatment (such as stigma) can be reduced by forged partnerships between researchers, state, federal, and other private funding sources and the many sectors (special mental health, human service, and voluntary support sectors) that provide mental health services.
Acknowledgements
Data used for this article were collected from the Epidemiology of Health Care Utilization Study (EHCUS) that was supported by NIDA Grant 1 P50 DA. This research has benefited from the assistance, encouragement and expertise of several mentors and exceptional persons. I would like to thank Drs. Lisa Metsch, Dale Chitwood, Lee Crandall, and Linda Belgrave for their support and guidance throughout this study. Special thanks to Dr. Larry Lawhorne for his continual support, mentorship and review of this manuscript.
Footnotes
Those classified as injection drug users reported injecting on a weekly basis over the past 12 months and tested positive for cocaine or opiates in the urine. The criteria for those classified as “other chronic drug user” included those not injecting drugs, but who were using cocaine or opiates weekly for the past 12 months.
References
- Aday L. Health status of vulnerable populations. Annual Review of Public Health. 1994;15:487–509. doi: 10.1146/annurev.pu.15.050194.002415. [DOI] [PubMed] [Google Scholar]
- Aday L. Vulnerable populations: A community oriented perspective. Family and Community Health. 1997;19:1–18. [Google Scholar]
- Aday L. At risk in America: The health and health care needs of vulnerable populations in the United States. San Francisco, CA: Jossey-Bass Publishers; 2001. [Google Scholar]
- Aday L, Fleming G, Anderson R. Access to medical care in the US: who has it, who doesn’t? Chicago, IL: Pluribus Press; 1984. [Google Scholar]
- American Psychiatric Association APA (APA: 2000) Diagnostic and Statistical Manual of Mental Disorders, Text Revision (4th Revision: DSM-IV-R) Washington, DC: American Psychiatric Press; [Google Scholar]
- Andersen R. Revisiting the behavioral model and access to medical care: Does it matter? Journal of Health and Social Behavior. 1995;36:1–10. [PubMed] [Google Scholar]
- Andersen R, Newman J. Societal and individual determinants of medical care utilization in the United States. Milbank Memorial Fund Quarterly. 1973;51:95–124. [PubMed] [Google Scholar]
- Berkman LF. The role of social relations in health promotion. Psychosomatic Medicine. 1995;57:245–254. doi: 10.1097/00006842-199505000-00006. [DOI] [PubMed] [Google Scholar]
- Berkman LF, Glass T. Social integration, social networks, social support, and health. In: Berkman LF, Kawachi I, editors. Social Epidemiology. New York: Oxford; 2000. pp. 137–173. [Google Scholar]
- Booth RE, Kwiatkowski CF, Weissman G. Health related service utilization and HIV risk behaviors among HIV infection drug users and crack smokers. Drug and Alcohol Dependence. 1999;55:69–78. doi: 10.1016/s0376-8716(98)00179-3. [DOI] [PubMed] [Google Scholar]
- Burnam MA. Use of mental health and substance abuse treatment services among adults with HIV in the United States. Archives of General Psychiatry. 2001;58:729–736. doi: 10.1001/archpsyc.58.8.729. [DOI] [PubMed] [Google Scholar]
- Chitwood D, McBride D, Metsch L, Comerford M, McCoy C. A comparison of the need for health care and use of health care by injection-drug users, other chronic drug users, and non-drug users. American Behavioral Scientist. 1998;41:1107–1122. [Google Scholar]
- Chitwood D, McBride D, French M, Comerford M. Health need and utilization: A preliminary comparison of injection drug users, other illicit drug users, and nonusers. Substance Use and Misuse. 1999;34:727–746. doi: 10.3109/10826089909037240. [DOI] [PubMed] [Google Scholar]
- Chitwood D, Comerford M, McCoy V. Satisfaction with access to health care among injection drug users, other drug users, and non-users. Journal of Behavioral Health Services & Research. 2002;29:189–197. doi: 10.1007/BF02287705. [DOI] [PubMed] [Google Scholar]
- Choe JY, Teplin LA, Abram KM. Perpetration of violence, violent victimization, and severe mental illness: balancing public health concerns. Psychiatric Services. 2008;59:153–164. doi: 10.1176/appi.ps.59.2.153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins KS, Schoen C, Joseph S, Duchon L, Simantov E, Yellowitz M. Health concerns across a woman’s life span: 1998 survey of women’s health. New York: The Commonwealth Fund; 1999. [Google Scholar]
- Compton SN, Swanson JW, Wagner HR, Swartz MS, Burns BJ, Elbogen EB. Involuntary outpatient commitment and homelessness in persons with severe mental illness. Mental Health Services Research. 2003;5:27–38. doi: 10.1023/a:1021755408267. [DOI] [PubMed] [Google Scholar]
- Curran GM, Sullivan G, Williams K, Han X, Collins K, Keys J, Kotral K. Emergency department use of persons with co-morbid psychiatric and substance abuse disorders. The Practice of Emergency Medicine. 2003;41:659–667. doi: 10.1067/mem.2003.154. [DOI] [PubMed] [Google Scholar]
- Gelberg L, Leake B. Substance abuse among impoverished medical patients: The effect of housing status and other factors. Medical Care. 1993;31:757–766. doi: 10.1097/00005650-199309000-00001. [DOI] [PubMed] [Google Scholar]
- Gelberg L, Gallagher T, Andersen R, Koegel P. Competing priorities as a barrier to medical care among homeless adults in Los Angeles. American Journal of Public Health. 1997;87:217–220. doi: 10.2105/ajph.87.2.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gelberg L, Andersen R, Leake B. The behavioral model for vulnerable populations: Application to medical care use and outcomes for homeless people. Health Services Research. 2000;36:1273–1301. [PMC free article] [PubMed] [Google Scholar]
- Green BL, Goodman LA, Krupnick JL, Corcoran CB, Petty RM, Stockton P, Stern NM. Outcomes of a single versus multiple trauma exposure in a screening sample. Journal of Traumatic Stress. 2000;13:271–286. doi: 10.1023/A:1007758711939. [DOI] [PubMed] [Google Scholar]
- Hosmer DW, Lemeshow S. Applied Logistic Regression. 2nd Edition. New York: Wiley; 2002. [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age of onset distribution of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005a;62:593–768. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Walters EE. Prevalence, severity and comorbidity of twelve –month DSM-IV disorders in the National Comorbidity Survey Replication (NCS-R) Archives of General Psychiatry. 2005b;62:617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Demler O, Frank RG, Olfson M, Pincus H, Walters EE, Wang P, Wells KB, Zaslavsky AM. Prevalence and treatment of mental disorders, 1990 to 2003. The New England Journal of Medicine. 2005c;352:2515–2523. doi: 10.1056/NEJMsa043266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Heeringa S, Lakoma MD, Petukhova M, Rupp AE, Schoenbaum M, Wang PS, Zaslavsky AM. Individual and societal effects of mental disorders on earning in the United States: Results from the national co-morbidity survey replication. American Journal of Psychiatry. 2008;165:703–711. doi: 10.1176/appi.ajp.2008.08010126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, McGonagle KA, Zhoa S, Nelson CB, Hughes M, Eshleman S, Wittchen H, Kendler KS. Lifetime and 12- month prevalence of DSM-III-R psychiatric disorders in the United States: Results from the national co-morbidity survey. Archives of General Psychiatry. 1994;51:8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Wang PS. The descriptive epidemiology of comorbidity occurring mental disorders in the United States. Annual Reviews of Public Health. 2008;29:115–129. doi: 10.1146/annurev.publhealth.29.020907.090847. [DOI] [PubMed] [Google Scholar]
- Koegel P, Sullivan G, Burnam A, Morton S, Wenzel S. sUtilization of mental health and substance abuse services among homeless adults in Los Angeles. Medical Care. 1999;37:306–317. doi: 10.1097/00005650-199903000-00010. [DOI] [PubMed] [Google Scholar]
- Lim Y, Andersen R, Leake B, Cunningham W, Gelberg L. How accessible is medical care for homeless women? Medical Care. 2002;40:510–520. doi: 10.1097/00005650-200206000-00008. [DOI] [PubMed] [Google Scholar]
- McCoy CB, Metsch LR, Chitwood DD. Health services for chronic drug users in an era of managed care: The University of Miami community-based health services research center. Advances in Medical Sociology. 2000;7:151–174. [Google Scholar]
- McQuistion HL, Finnerty M, Hirschowitz J, Susser ES. Challenges for Psychiatry in Serving Homeless People with Psychiatric Disorders. Psychiatric Services. 2003;54:669–676. doi: 10.1176/appi.ps.54.5.669. [DOI] [PubMed] [Google Scholar]
- Menard S. Applied logistic regression analysis. 2nd edition. Thousand Oaks, CA: Sage Publications; 2002. [Google Scholar]
- Metsch L, Crandall L, Wohler-Torres B, Miles C, Chitwood D, McCoy C. Met and unmet need for dental services among active drug users in Miami, Florida. The Journal of Behavioral Health Services & Research. 2002;29:176–188. doi: 10.1007/BF02287704. [DOI] [PubMed] [Google Scholar]
- Pampel F. Logistic regression: A primer. Series: Quantitative applications in the social sciences. Thousand Oaks, CA: Sage Publications; 2000. [Google Scholar]
- Perneger T. What's wrong with Bonferroni adjustments? British Medical Journal. 1998;316:1236–1238. doi: 10.1136/bmj.316.7139.1236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ro M, Shum L. Forgotten policy: An examination of mental health in the U.S. Michigan: W.K. Kellogg Foundation; 2001. [Google Scholar]
- Robins LN, Regier DA, editors. Psychiatric disorders in America: The epidemiologic catchment area study. New York: Free Press; 1991. [Google Scholar]
- Ullman S, Brecklin L. Sexual assault history and health-related outcomes in a national sample of women. Psychology of Women Quarterly. 2003;27:46–57. [Google Scholar]
- US Congress. H.R. 6983: Paul Wellstone and Pete Domenici Mental Health Parity and Addiction Equity Act of 2008. 110th Congress. 2008 [Google Scholar]
- U.S. Department of Health and Human Services. Mental Health: A Report of the Surgeon General. Rockville, MD: U.S. Department of Health and Human Services, Substance Abuse and Mental Health Services Administration, Center for Mental Health Services, National Institutes of Health, National Institute of Mental Health; 1999. [Google Scholar]
- U.S. Department of Health and Human Services. New freedom commission on mental health. Achieve the promises: transforming mental health care in America: Final report. Rockville, MD: Publication SMA-03-3832. Rockville, MD: U.S. Department of Health and Human Services, Substance Abuse and Mental Health Services Administration, Center for Mental Health Services, National Institutes of Health, National Institute of Mental Health.; 2003. [Google Scholar]
- Wang PS, Berglund P, Olfson M, Pincus HA, Wells KB, Kessler RC. Failure and delay in treatment contact after onset of mental disorders in the national co-morbidity survey replication. Archives of General Psychiatry. 2005a;62:603–613. doi: 10.1001/archpsyc.62.6.603. [DOI] [PubMed] [Google Scholar]
- Wang PS, Lane M, Olfson M, Pincus HA, Wells KB, Kessler RC. Twelve-month use of mental health services in the United States. Archives of General Psychiatry. 2005b;62:629–640. doi: 10.1001/archpsyc.62.6.629. [DOI] [PubMed] [Google Scholar]
- Wells K, Sherbourne C, Sturum R, Young A, Burnam A. Alcohol, drug abuse, and mental health care for uninsured and insured adults. Health Services Research. 2002;37:1055–1066. doi: 10.1034/j.1600-0560.2002.65.x. [DOI] [PMC free article] [PubMed] [Google Scholar]