Abstract
The study analyzed the effects of self-recording and behavioral skills training on guarding responses of 3 staff members while they assisted 3 students with multiple disabilities to ambulate. The intervention increased the percentage of correct posture and guarding responses and the distance that students ambulated. These effects generalized when staff taught new students.
Keywords: ambulation, behavioral skills training, generalization, self-recording
The training of correct guarding by nonspecialist staff who work with ambulating children is important because these children may be at risk for injury. Behavioral skills training (BST) has been used to train nonspecialist staff (Rosales, Stone, & Rehfeldt, 2009; Sarokoff & Sturmey, 2004) and may be useful for training staff who work with ambulating children. Therefore, the current study evaluated the effects of BST and self-recording on staff posture and guarding and the distance that students ambulated.
METHOD
Participants and Settings
Three staff members (Staff 1, 2, 3) and 3 students with physical disabilities (Jaquel, Cole, Steve) participated. Staff members (21 to 24 years old) were teaching aides in special education classrooms who had worked with students with physical disabilities for 1 to 3 years. Jaquel was a 7-year-old boy with spina bifida myelomeningocele with flaccid muscles of both lower extremities. He traveled in wheelchair or crawled and did not stand or ambulate independently. He used a hip-knee-ankle-foot orthosis with reciprocating gait orthosis. Cole was an 8-year-old boy with cerebral palsy with muscle weakness, joint laxity, visual impairments, and problems with postural control. He did not stand or ambulate independently, but crawled, drove a powered wheelchair, or used a posterior rolling walker with staff assistance. Steve was an 8-year-old boy with spastic diplegia, cerebral palsy, developmental delays with spasticity, and contractures of both knee flexors and ankle plantar flexors. He did not independently stand or ambulate and typically crawled. The study took place in the physical therapy gym and hallway of a special education school located in a medical center.
Response Measurement and Interobserver Agreement
There were six staff posture and guarding responses individualized to each student: (a) The staff member sat on a rolling stool; (b) the staff member sat directly in front of Jacquel or to the right side of Cole and Steve (Jaquel's staff member rolled backwards on his or her stool while remaining in front of him at all times); (c) the staff member's lower back was aligned erect with the upper back and was vertical; (d) the staff member's left hand was on the right side of Jaquel's pelvis and hip orthosis or Cole's and Steve's backs; (e) the staff member's right hand held the left side of Jaquel's trunk, the right side of Cole's walker, or Steve's right hand; and (f) the staff member provided behavior-descriptive praise within 3 s of the student's completion of ambulation.
The second dependent measure was the distance students ambulated without loss of balance, which was defined from a predetermined starting point in the physical therapy gym or hallway to the end of ambulation. Loss of balance was defined as five instances of trips, falls, or when the student's body shifted away from his base of support and a fall or trip was likely. Staff prevented actual falls throughout the study. Sessions were terminated if the child lost his balance or if he ambulated the target distance of 18.3 m. During all conditions, the experimenter recorded staff performance as correct or incorrect, using a checklist of the six responses described above. Distance was measured by counting the number tiles (0.305 m each).
Interobserver agreement data were collected for 57% of baseline and BST sessions. Agreement was calculated for guarding responses by dividing the number of agreements by the number of possible correct responses and converting this ratio to a percentage. Agreement was 100% for both staff behavior and distance ambulated.
Procedure and Experimental Design
Vocal instruction only (baseline)
Participants were assigned to training dyads consisting of 1 staff and 1 student. The experimenter instructed staff to take the student either from his classroom doorway to a specified location or vice versa, stated the six required response components for correct posture and guarding, and said, “Safely walk him to the [location], please.” The experimenter said nothing else during baseline.
Behavioral skills training (BST)
The experimenter gave a self-recording checklist to the staff member before each session, explained the required six response components, instructed him or her to walk the student safely to a specified location, instructed him or her to complete the self-recording checklist immediately after the completion of student ambulation and asked if he or she had any questions. Immediately after self-recording, the experimenter provided performance feedback, including positive statements on correct response components and corrective statements on errors. The staff member and the experimenter reviewed correspondence and noncorrespondence between their respective checklists, and the experimenter explained the physical therapy implications of better performance. If the staff member performed fewer than six correct response components, the experimenter modeled the correct response with the student for one trial and instructed the staff member to rehearse that correct response for one trial. During modeling and rehearsal, a trial was defined as the experimenter or the staff member guarding the student for at least 3 m. During modeling, the experimenter described the incorrectly implemented components and instructed the staff member to observe as he demonstrated those correct responses. Thereafter, the experimenter instructed the staff member to guard the student during ambulation for one trial. The experimenter then provided vocal or physical prompts for correct responses as he or she guarded the student. Immediately after completion of the behavioral rehearsal trial, the experimenter provided descriptive feedback based on the preceding trial. Modeling and rehearsal were terminated when the staff member completed two consecutive trials with all six responses emitted correctly. If he or she performed fewer than six correct responses during the first two trials, he or she participated in five further trials that included opportunities for instructions, self-recording, feedback, modeling, and rehearsal. Sessions were terminated when the student completed the required distance or lost his balance.
A multiple baseline design across three staff–student dyads was used to evaluate the effects of the BST program.
Generalization Probes, Follow-Up, and Social Validity
Generalization and follow-up were identical to baseline and were conducted every third or fourth training trial throughout baseline and treatment phases by having the staff member implement the posture and guarding procedures with other students (e.g., Staff 1 guarded Cole). Follow-up took place 4 months after intervention. Staff completed two- and four-item questionnaires before and after intervention, using a 5-point Likert scale, that concerned staff familiarity of correct guarding procedures, the role of physical therapists, the pleasantness of the interactions during training, and whether he or she would recommend this training.
RESULTS AND DISCUSSION
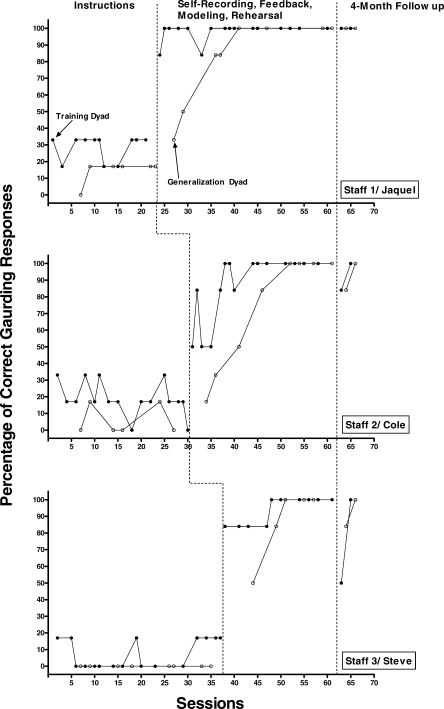
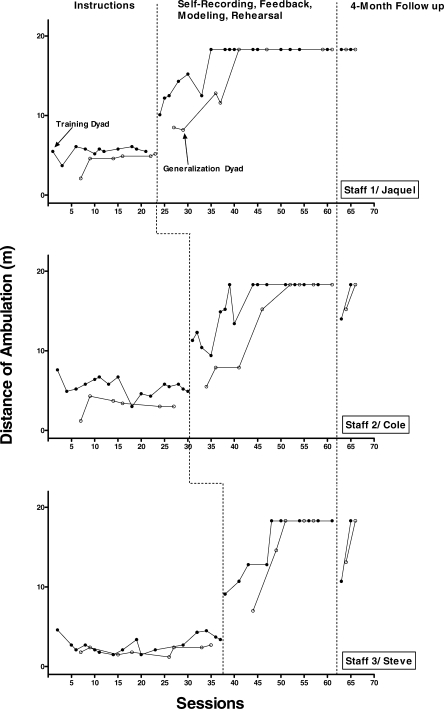
The mean percentages of correct staff responses completed were 29%, 19%, and 7% for baseline and 14%, 6%, and 0% for generalization for Staff 1, 2, and 3, respectively (Figure 1). Following intervention, the mean percentages of staff responses were 98%, 87%, and 94% during training and 95%, 73%, and 87%, during generalization sessions for Staff 1, 2, and 3, respectively. Mean percentages of correct responses at 4-month follow-up for Staff 1, 2, and 3 were 100%, 92%, and 84%, respectively. The mean baseline distances ambulated were 5.5 m, 5.5 m, and 2.8 m, and were 4.4 m, 3.1 m, and 2.0 m during generalization for Jaquel, Cole, and Steve, respectively (Figure 2). When the BST intervention was implemented, the mean distances were 16.2 m, 15.5 m, and 15.5 m during training and 14.3 m, 13.7 m, and 15.5 m during generalization sessions for Jaquel, Cole, and Steve, respectively. Mean follow-up distances for Jaquel, Cole, and Steve were 18.3 m, 16.5 m, and 15.1 m, respectively.
Figure 1.
Percentage of correct posture and guarding responses during vocal instructions only, self-recording, feedback, modeling, rehearsal, and 4-month follow-up for Staff 1, 2, and 3.
Figure 2.
Distance of ambulation (in meters) during vocal instructions only, self-recording, feedback, modeling, rehearsal, and 4-month follow-up for Jaquel, Cole, and Steve.
In response to the statements “I am familiar with the requirements for increasing safety and independence of students as they ambulate” and “I am familiar and understand the role of consultation with physical therapy providers in regards to safe and correct guarding of children as they ambulate,” mean staff ratings were 2.76 before training and 5 after training. Mean staff ratings were 5 to “I had pleasant interactions with the physical therapy provider that consulted in regards to increasing safety and independence of students as they ambulate” and “I would recommend these trainings and consultations to other staff.”
These findings extend earlier studies (Alvosius & Sulzer-Azaroff, 1986; Sarokoff & Sturmey, 2004) demonstrating that nonspecialist staff can acquire skills through BST and self-recording. Social validity measures suggested that training was acceptable to staff. Future research could extend the current findings and analyze whether self-recording with or without BST generates similar effects.
Acknowledgments
We thank the staff members and students of Children's Learning Center at United Cerebral Palsy of Nassau for their participation. We also thank Susan Vener and Andrea Gold for consulting on early procedures, Claire Poulson for consulting on social validity measures, and John Ward-Horner for assistance in graphing the data.
REFERENCES
- Alavosius M.P, Sulzer-Azaroff B. The effects of performance feedback on the safety of client lifting and transfer. Journal of Applied Behavior Analysis. 1986;19:261–267. doi: 10.1901/jaba.1986.19-261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosales R, Stone K, Rehfeldt R.A. The effects of behavioral skills training on implementation of the picture exchange communication system. Journal of Applied Behavior Analysis. 2009;42:541–549. doi: 10.1901/jaba.2009.42-541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarokoff R.A, Sturmey P. The effects of behavioral skills training on staff implementation of discrete-trial teaching. Journal of Applied Behavior Analysis. 2004;37:535–538. doi: 10.1901/jaba.2004.37-535. [DOI] [PMC free article] [PubMed] [Google Scholar]