Abstract
The vertical approach to breast reduction surgery has achieved increasing popularity. The learning curve can be a problem for surgeons starting to incorporate vertical techniques into their practices; the medial pedicle approach is outlined in detail. Designing and creating the medial pedicle is straightforward and rotating it into position is easy. An elegant curve to the lower pole of the reduced breast can thus be created. Current concepts related to the skin brassiere, breast sutures, and the longevity of results are reviewed. It is important for the surgeon to understand that the skin resection pattern and the pedicle design are separate issues when discussing breast reduction surgery.
Keywords: Vertical breast reduction, medial pedicle
Every approach to breast reduction surgery has its advantages and disadvantages. What works for one surgeon will not work as well for another surgeon. What works for one patient will not work as well for another patient. But all plastic surgeons need to become proficient in various options so that they can adopt different techniques to different circumstances.
PERSONAL EVOLUTION
In my practice, I have changed to the medial pedicle vertical reduction mammaplasty technique for the majority of my breast reduction patients.1,2,3 I still perform a variation of the inverted T reduction4,5,6 for the very large patients (with or without a free nipple graft). I also will perform liposuction-only for some patients.7,8,9,10
For the first 10 years of my practice, I used the inverted T inferior pedicle technique and was comfortable with it. I had been trained with the lateral Dufourmentel11 approach, the vertical bipedicle of McKissock,12 the horizontal bipedicle of Strombeck,13 and the medial pedicle of Biesenberger14 as well as the superior pedicle of Weiner.15 The inferior pedicle inverted T was reliable and consistent. But the inframammary scar was often unsightly; the medial and lateral dog-ears were sometimes a problem; the shape could be boxy initially and bottomed out with time.
Madeleine Lejour16,17,18,19 convinced me to try the vertical approach and I reluctantly stepped out of my comfort zone. I initially liked the superior pedicle as she described, but I encountered difficulty as I increased my indications to larger breast reductions. I had trouble insetting the pedicle and I suffered along with the patient when I had my first nipple necrosis.
I can look back now and realize that my attempt to preserve a full-thickness superior pedicle ended up in constriction of the blood supply. Now that I understand that the superior pedicle blood supply is very superficial, I know that it is actually more likely to survive when it is thinned. But I didn't realize that when I started with the vertical approach. I converted initially to a lateral pedicle (much like Skoog20 described) to preserve sensation. It was certainly a much easier pedicle to inset, and I could leave it full thickness to preserve as much sensation and breast-feeding potential as possible.
Although I was impressed with the improved shape of the vertical approach, I wasn't totally happy with the lateral pedicle. The patients were pleased with the “perky” shape—a description they had rarely ever used when I had performed the inverted T breast reduction. Unfortunately, I could not remove enough lateral breast tissue in many cases because this tissue formed the base of the lateral pedicle. I tried a medial pedicle on several patients (also described by Skoog20 and Strombeck13) on one side and a lateral pedicle on the other. I was surprised at how good the sensation was and I was pleased with the improved shape. The medial pedicle is easy to inset and it allows access to the thick lateral breast tissue. Asplund and Davies21 used a medial dermal pedicle, but I found that a full-thickness pedicle is more likely to include sensation and breast ducts, but the actual pedicle base rotates into position, giving an elegant curve to the lower pole of the breast.
I switched to the vertical technique because of the improved scarring.22,23,24,25 I persisted with the technique because of the improved shape. As time went on, I realized that not only was the medial pedicle easier to perform, the breast shape was better with the medial pedicle because the breast could be coned into an ideal shape as the base of the pedicle rotates along with the nipple-areolar complex. The inferior border of the medial pedicle becomes the medial pillar. This allows shaping that is not as easily achieved with the superior pedicle.
ADVANTAGES AND DISADVANTAGES
I have now performed over 1200 vertical breast reductions using the superior, lateral, and medial pedicles. There is no question that in my practice, the medial pedicle has equivalent sensation, is easier to perform, and allows me to give the patient a better shape. Now that I have seen 10-year results with this technique, the improved longevity of the shape can be added to the improved scarring and the improved initial shape (projection and coning) as reasons to continue with the vertical approach.
There are, however, limitations to the medial pedicle vertical technique. It is not applicable to larger breast reductions. It can be harder to perform in reductions over 1500 g per breast. I do still use the vertical approach in these cases to achieve the better coning and increased projection, but I will add a short horizontal scar. I will also discuss with the patient the possibility of using free nipple grafts if the pedicle is going to be quite long. There are two reasons for this: I don't think that the medial pedicle is quite as robust as the inferior pedicle, and leaving too much tissue in the pedicle will prevent adequate parenchymal resection and will lead to pseudoptosis.
As plastic surgeons, we accept that a certain number of patients will require a revision. A revision rate of 5% is not unusual for many aesthetic procedures (such as rhinoplasty). There are, however, patients who would like a revision but we are unable to help because we do not have much to offer. This is often the case in the inverted T approach where patients ask for a scar revision or some form of correction of the lateral and medial dog-ears. In my hands, the vertical approach has resulted in a revision rate of ∼5%. This is usually for puckers, asymmetry, or underresection.
CONCEPTS
Skin Pattern Versus Parenchymal Resection Pattern
We often talk about the inverted T or Wise pattern26 approach as if it assumes the use of an inferior pedicle. We need to be careful when discussing breast reduction to treat the skin resection pattern (inverted T, lateral, vertical, circumareolar) as separate from the nipple-areolar pedicle (superior, inferior, lateral, medial, central, or free nipple grafts). There are many available combinations, and an open mind is essential when making choices for a patient has had previous breast surgery.
Skin Brassiere Versus Parenchymal Shaping
There has been a long-running controversy about the effectiveness of using the skin to hold the breast shape. Although there is some coning attempted with the inferior pedicle inverted T approach, there is no question that the procedure relies mainly on the skin brassiere to hold the shape. We know that skin and dermis stretch with time (and variably with genetics)—is this why the inverted T tends to bottom out with time? Does the 5- cm rule for the vertical length prevent bottoming out or does it flatten the breast and push it down below the original inframammary fold?
What Role Does the Nature of the Parenchymal Resection Play?
As I watched the inframammary fold rise somewhat with the medial pedicle vertical breast reduction and as I watched the inframammary fold descend with the inferior pedicle inverted T technique, I cannot help but wonder whether the nature of the parenchymal resection is key in improving the longevity of the shape in the vertical approach.
When we use the inferior pedicle, we remove the superior, superolateral, and superomedial breast tissue. In the medial pedicle, we remove the inferior, inferolateral, and inferomedial breast tissue. Does the inverted T inferior pedicle procedure drop out more than the medial pedicle vertical procedure because we are removing what we want to leave and leaving what we want to remove? Are we giving gravity too much to work on?
Breast Sutures: Do They Work to Pectoralis Fascia?
Pectoralis fascia is slippery; any time that I have tried to suture the breast up to chest wall has only provided a temporary increase in upper pole fullness. When I followed my patients for long enough, the improved upper pole fullness did not last. On the other hand, I do think that Ruth Graf's pectoralis sling27,28,29 can provide some increased upper pole fullness over the long term. Other methods may work as well, but it is important to follow patients for at least a year to be able to draw any conclusions.
Breast Sutures: Do They Work?
Do breast sutures hold? Or do they just cause constriction and fat necrosis? In my experience, breast sutures will hold to some degree. Constriction of the tissue is not necessary as long as small bites in the fibrous tissue are used to bring fibrous tissue on each side together. Suturing fat to fat will be ineffective. If I leave an indentation laterally from a suture that is pulled too much, it tends to persist. I believe that breast-to-breast sutures hold, but breast-to-pectoralis fascia sutures do not appear to be as successful.
ANATOMY
Arterial
Corduff and Taylor30 have shown that the blood supply enters the breast at a superficial level. The branches from the internal mammary (thoracic) artery, the lateral thoracic artery, and (less so) the thoracoacromial system pass through the subcutaneous tissue into the breast and then descend into the parenchyma. There is one branch from the internal mammary artery, which comes most commonly from the second or third intercostal space and angles obliquely downward toward the nipple. It is present at the breast meridian about 1 cm deep to the skin. It is this vessel that supplies a superior or superomedial pedicle.
Branches from the lateral thoracic system are more variable in their level but they also become more superficial as they proceed medially. It is these branches that supply a laterally based pedicle.
There is, however, one vascular leash that is not superficial but instead penetrates the breast parenchyma from the pectoralis muscle. There is a strong perforator that comes from the internal thoracic system that penetrates the pectoralis muscle about the level of the fifth or sixth intercostal space medially. It is a large vessel, which is usually just medial to the breast meridian and 2 to 4 cm above the inframammary fold. It is this vessel that supplies an inferior or central pedicle.
Venous
Although there are veins that accompany the arterial perforator from the pectoralis muscle that supplies the inferior pedicle, most of the arteries do not have an accompanying vein (personal communication, Ian Taylor). The venous plexus is superficial and concentrated around the areola. It is for this reason that circumferentially incising the areola will cause significant damage to the venous system.
Any design (such as a long superior pedicle) that necessitates folding of the pedicle is likely to compromise venous return. Arterial inflow might be strong enough to overcome folding but venous return could suffer from the compression. Marking the veins preoperatively and trying to include some in the design of the pedicle may offer some increased security.
Nerve
There is no question that the lateral cutaneous branch of the fourth intercostal nerve is the most common nerve supplying sensation to the nipple. What is poorly understood, however, is the anatomy of that innervation. One branch of the nerve does go superficially, but it has been shown that there is a significant branch that runs along the pectoralis fascia and then takes an almost 90 degree turn at the level of the breast meridian and runs vertically from the posterior aspect of the breast toward the nipple.31 It is for this reason that any full-thickness pedicle (where tissue is left over the pectoralis fascia) is likely to preserve sensation to the nipple-areolar complex.
The lateral cutaneous branch of the fourth intercostal nerve is not the only nerve to supply sensation. It has also been clearly shown that the anterior cutaneous branches take a superficial course and then terminate at the medial aspect of the areola. A medially based pedicle would therefore not need to be full thickness to preserve sensation.
There are also supraclavicular branches that supply some sensation. These are small nerves and are far less important.
DESIGN AND MARKING
Nipple Position
The key to a good result is correct determination of nipple position. New nipple position must be correlated to the patient's inframammary fold, not to some arbitrary measurement. Although the fold rises 1 to 2 cm with this approach, it is a mistake to place the nipple too high in a patient with a very low inframammary fold. The nipple can be placed slightly higher in a patient who has a lot of upper pole fullness, but placing the nipple on the concave slope of the breast will result in a nipple that will point upward postoperatively.
Because of the effect of these vectors, the new nipple position must be placed lower on the larger breast. If this is not taken into account, the nipple will end up higher on the larger breast.
The new nipple position should be designed at the meridian of the breast (or preferably the meridian of the chest wall if adequate lateral breast tissue can be removed). It can be tempting to draw the meridian through the existing nipple position, but this can be misleading because the nipple may be either too medial or too lateral.
I place a measuring tape under the patient's breasts and mark where the fold is in the midline of the chest (much as Gil Gradinger32,33 described). The new nipple position must be 2 cm lower than that which is used for the Wise pattern. Lowering the design is essential to accommodate the increased projection that results from this technique (Fig. 1).
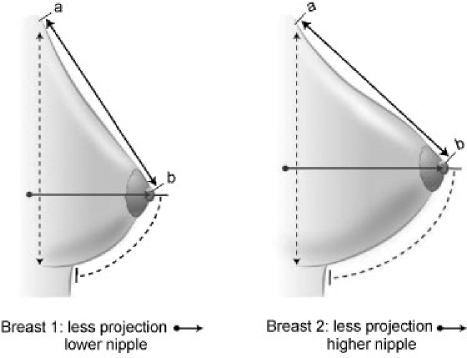
Figure 1.
This is an exaggerated drawing to show how the new nipple position appears to be higher with the vertical skin pattern techniques. The line ab is the same in both drawings, but the nipple appears higher because of the increased projection that is achieved with the coning of the breast parenchyma. The new nipple position must be marked at least 2 cm below what a surgeon would normally have marked with the Wise pattern to accommodate both the increased projection and the effect that is achieved from closure of the vertical ellipse.
It must also be recognized that the vectors are different. When we use an inverted T, we are taking a horizontal ellipse and pulling the skin inferiorly. On the other hand, when we use a vertical skin pattern, the excision is vertical and the tissue is coned (Fig. 2). Does the horizontal excision tend to pull the new nipple position inferiorly?
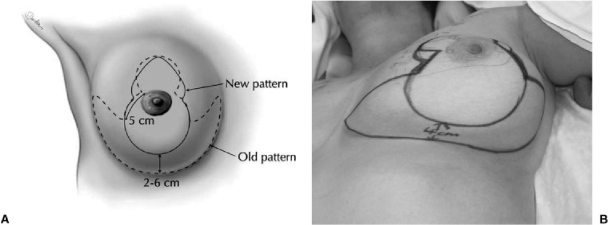
Figure 2.
Design of the vertical skin resection pattern compared with the inverted T skin resection pattern. (A) The Wise pattern is outlined in dotted lines whereas the vertical pattern is outlined in solid lines. (B) Similar comparison as seen drawn on a patient.
Areolar Opening
The opening for the areola can be designed at the marking stage or delayed until the resection is finished, as long as the new nipple position is determined first. I use a freehand design that results in a circle when it is closed (the circumference measures ∼16 to 18 cm). The opening can be made a bit larger, but a circumference of 16 cm matches an areolar diameter of 5 cm. If the circumference is longer than ∼20 cm then either scar widening or enlargement of areolar diameter will result.
Skin Resection Pattern
Because this is not a skin-shaping procedure, the actual design of the pattern is not as important in the vertical approach as it is with the inverted T. The key is not to remove too much skin. Dr. Lejour has a good method of rotating the breast upward and inward to mark the breast meridian and then upward and outward to mark the opposite breast meridian. These lines would correspond to the vertical lines in an inverted T. Instead of following the Wise pattern and extending the lines laterally and medially, these lines are just joined in a “U” shape, staying well above the inframammary fold.
Because this “U” shape is closed as an ellipse, the vertical line is lengthened. It is therefore very important to leave at least 2 to 6 cm (300 g to 900 g) of skin above the inframammary fold. It is also important to recognize that the inframammary fold rises, and if the skin resection is carried close to the fold, the scar will extend down onto the chest wall.
It is also important to design the skin excision as a “U” and not a “V.” It is tempting to do the latter to avoid the pucker, but there will be excess skin remaining. This will then need to be excised and closed as a purse-string or short horizontal scar. When a “U” is used, the pucker that sticks out at the lower end of the vertical scar will tuck in and follow the curve of the new breast.
Design of the Medial Pedicle
The pedicle is medially based and full thickness down to the chest meridian. The base of the pedicle is designed so that one-half of the base is in the areolar opening and one-half is along the vertical skin resection line. Following this half-and-half rule makes the pedicle easier to inset. It creates a good medial pillar (which originally was the inferior border of the pedicle). Leaving too much of the base inferiorly will result in too much inferior fullness. It may be wise to mark the superficial veins at this stage so that the pedicle can be designed to include some obvious venous drainage.
How long does the base of the pedicle need to be? I tend to leave about a one-to-one ratio for pedicle width to pedicle length, but it may well be safe to leave a narrower base. If some tissue is kept superiorly (making the pedicle more superomedial), it may be that some more arterial supply and venous drainage may be included. There will also be some extra tissue to form a platform for the nipple-areolar complex so that it does not become depressed postoperatively. One must realize, however, that pushing tissue up into the upper pole in this way will not result in more upper pole fullness; it will drop down and will actually result in more pseudoptosis. Too much tissue superiorly will also make it more difficult to inset the pedicle.
When is it wise to switch to full-thickness grafts? It will depend on the circumstances—the length of the pedicle and the patient's (informed) desires. An overly long pedicle (greater than 12 to 14 cm) may not only be risking loss of blood supply but may also be too bulky, leading to increased lower pole fullness and pseudoptosis.
OPERATIVE TECHNIQUE
Infiltration
If the patient is overweight, then I will use ∼500 mL of tumescent-type infiltration per side, but mainly in the lateral chest wall and preaxillary fat. Otherwise I will use a spinal needle and infiltrate ∼40 mL a side of xylocaine 0.5% with adrenalin 1/400,000 per side. I used to infiltrate into the incision lines, but I was frustrated with the resultant subcutaneous hematomas.
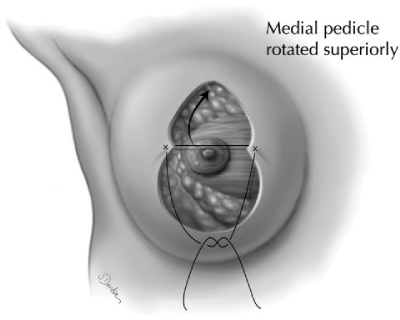
Creation of the Pedicle
The pedicle is de-epithelialized (Fig. 3) leaving a margin around the areolar edge (Schwartzmann34 maneuver). The pedicle is carried down to the chest wall using either a scalpel or cutting cautery. The pedicle is beveled superiorly to leave a platform for the nipple-areolar complex. Although it is tempting to include a significant amount of tissue superiorly to either include more vessels in the pedicle or to try to increase upper pole fullness, this platform should be conservative. If it is too large, the pedicle may be more difficult to inset and it will not help with upper pole fullness. The medial pedicle is floppy and, like the inferior pedicle, it can easily be inadvertently undermined.
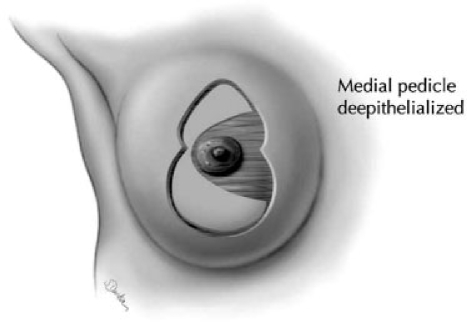
Figure 3.
The design of the vertical skin pattern with the medially based pedicle. The orientation of the base of the pedicle can be altered, but I have found that the pedicle is consistently easier to inset when half of the base is in the areolar opening and half of the base is in the vertical opening. If the base is completely in the areolar opening, it can have the same problems as the superior pedicle with difficulty insetting. If the base is completely in the vertical opening, it can cause difficulties in rotation and it may mean that there is too much inferior fullness, which can lead to pseudoptosis.
The pedicle is often more superomedial than just medially based. Some subcutaneous tissue is left superiorly rather than carrying the superior border of the pedicle all the way down to the chest wall.
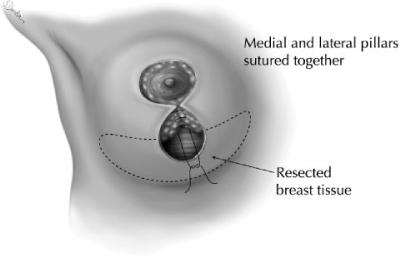
Parenchymal Resection
The breast tissue and skin is removed en bloc (Fig. 4). The breast tissue resection is beveled out extensively laterally and less so medially. The tissue is then undermined down to the inframammary fold. It is important to leave some fatty tissue on the undersurface of the skin inferiorly (about 1 cm) but if the subcutaneous tissue is not removed inferiorly, a pucker will remain. The thick tissue at the level of the inframammary fold needs to be excised directly (it does not suction well). Because the inframammary fold rises (especially laterally) the tissue at and just lateral to the meridian must be excised. Postoperative puckers are more of a problem with excess subcutaneous tissue rather than excess skin.
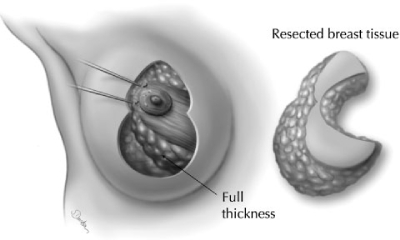
Figure 4.
The medial pedicle is a full-thickness pedicle carried down to the breast meridian. The base width measures ∼6 to 10 cm (approximately a one-to-one ratio of length to base width). Although tissue needs to be removed superiorly to allow easy inset of the pedicle, it can be beveled out to help maintain blood supply and also to provide some support behind the nipple-areolar complex. Any attempt, however, to push tissue up to achieve more upper pole fullness will fail and lower pole excess will result instead.
The tissue resection is carried down to chest wall, but pectoralis fascia is not exposed. Not only is this unnecessary, but it results in increased bleeding and probably also results in an increased risk of loss of sensation.
It is important not to remove breast tissue superiorly unless the patient has too much upper pole fullness. Tissue just lateral to the meridian can and should be excised, and some tissue should be left in the superomedial part of the parenchymal resection. This leaves some more potential blood supply to the pedicle, but it also provides some fullness to prevent the areola from becoming depressed. On the other hand, it is wrong to leave too much tissue in the areolar opening—trying to push tissue up into the upper pole will not work. It always descends. Instead of getting more upper pole fullness, the breast will end up with more lower pole fullness and pseudoptosis.
Although the skin is not removed following the Wise pattern, the breast parenchyma is. The pillars should be ∼7 cm in height, depending on the ultimate size of the breast. The lower portion of the breast tissue is beveled out under the skin laterally and medially and then undermined down to the inframammary fold.
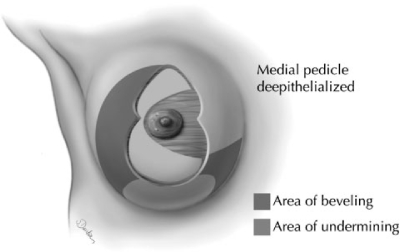
Insetting of the Pedicle
The pedicle rotates easily into position (Fig. 5). The areola may rotate up to 90 degrees, but the actual rotation is not important. What is important is to rotate it into position so that there is no kinking or compression. The inferior border of the medial pedicle now becomes the medial pillar.
Figure 5.
The areolar opening is closed with a buried 3–0 Monocryl suture. The dermis at the base of the pedicle does not need to be undermined for this closure. Once the areolar opening is closed inferiorly, the pedicle is easily rotated into position. Note that the base of the pedicle itself is also rotated and the inferior border of the medial pedicle now becomes the medial pillar.
The base of the areola is closed with an interrupted 3–0 Monocryl (Ethicon, Markham, Ontario, Canada) and the pedicle is then rotated into position. The pillars are closed before final insetting.
Closure of the Pillars
The pillars should be ∼7 to 8 cm in height (Fig. 6). They do not extend the full length of the vertical opening. If the surgeon can visualize the parenchymal resection as following the Wise pattern, the pillars will usually start about half way up the vertical opening. I usually put in only a few 3–0 Monocryl sutures into the fibrous part of the breast tissue to close the pillars.
Figure 6.
The pillar closure starts about halfway up the vertical skin opening. The Wise pattern is followed for the parenchymal resection (but not the skin resection) and the pillars should only measure ∼7 cm in vertical height. The rotation of the medial pedicle along with its base rounds out the inferior aspect of the breast (which can occur with the superior pedicle). The inferior border of the medial pedicle now becomes the medial pillar. The pillars are closed with only a few interrupted 3–0 PDS (Ethicon, Markham, Ontario, Canada) or Monocryl (Ethicon, Markham, Ontario, Canada) in the parenchyma. Care must be taken to suture solid fibrous tissue rather than using large constricting sutures in the fat.
The inferior border of the pedicle now becomes the medial pillar, and suturing begins inferiorly when the pillars are brought together. The pillar must be completely rotated into position with the first suture to close the pillars being placed close to the base of the pedicle, not part of the way along the inferior border. This suture can be fairly superficial; it is not necessary to put the deep tissues under tension.
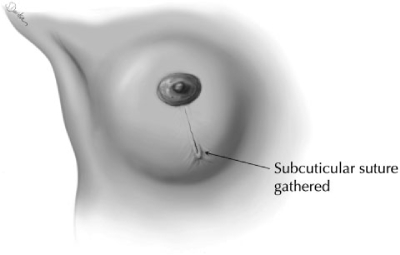
Closure of the Vertical Incision
The deep dermis is closed with interrupted buried 3–0 Monocryl. There is no need to suture the skin up to the breast tissue. There is no need to suture the pucker down to the chest wall. It is better to let the skin adapt to the new shape. Otherwise, the pucker will not be sutured into the correct position and it will take months to settle out.
The final skin closure is achieved with a subcuticular 3–0 Monocryl suture that is only lightly gathered at the inferior end (Fig. 7). It is important not to take deep bites and not to gather the skin too tightly, otherwise delayed healing will result from constriction of blood supply to the skin edges. This could also be a problem if too much skin was removed and if the edges end up being pulled too tightly.
Figure 7.
Interrupted buried 3–0 Monocryl sutures are used in the deep dermis. The skin is closed with a subcuticular 3–0 Monocryl. I am using less gathering now with this suture. Not only does it take the pucker longer to settle, the vertical skin stretches out with time in spite of the gathering. If the skin has poor elasticity, then some gathering may be indicated but only at the inferior aspect of the vertical incision. Excess gathering causes a teardrop-shaped areola in the initial postoperative stages and it could constrict the blood supply to the skin, causing wound-healing problems at the skin edges. Care must be taken not to take deep constricting bites of dermis when this suture is gathered.
Gathered skin will stretch out to some degree. The skin overlying the breast tissue itself does not need to be gathered. Only the very inferior skin that lies over the emptied area of parenchyma should be gathered, and then only very slightly. I used to gather the skin to a greater degree, but it took longer for the pucker to disappear. When the vertical incision is measured postoperatively, it gradually stretches to close to its original length. If the vertical incision measures 10 cm, I will usually gather it to no more than 8 to 9 cm. If the vertical incision measures 8 cm, I will gather it to no more than 6 to 7 cm.
Liposuction for Final Tailoring
I don't use liposuction for volume resection, but I do use it for final tailoring of the breast shape along the inframammary fold. I will use it if needed at the end of the procedure for symmetry and I will use it to reduce fullness in the preaxillary area and along the lateral chest wall (Fig. 8).
Figure 8.
This drawing shows the outline of the parenchymal resection. Very little tissue is removed superiorly unless the patient has significant upper pole fullness preoperatively. The tissue resection follows a Wise pattern. It is beveled out laterally and medially but undermined inferiorly. Because the inframammary fold rises with this technique, care must be taken to remove excess subcutaneous tissue in the region between the old and the new inframammary folds, especially just lateral to the breast meridian. Postoperative puckers are less a problem of skin excess than a problem of subcutaneous tissue excess. About a centimeter of fat must be left attached to the dermis to prevent scar contracture.
Closure of the Areola
The areola is closed with interrupted deep 3–0 Monocryl at four separate points. Then the skin is closed with a subcuticular running 3–0 Monocryl.
Drains and Antibiotics
I rarely use drains. The two hematomas (out of 1200) that necessitated reoperation would not have been helped with drains. I use perioperative antibiotics in all patients (intraoperative cephazolin and then 5 days of postoperative cephalexin). I not only had a higher infection rate before I routinely used antibiotics, I also had a significantly greater problem with wound healing at the skin edges. I suspect that seromas do occur, but I do not aspirate them. One patient developed an infected seroma, which settled well with antibiotics.
Tape, Bandages, and Compression
I use either paper tape or Steristrips (3M, St. Paul, MN) to cover the incisions. Some tape over the empty area of the breast inferiorly may help to prevent the lower pole from swelling. But I apply gauze loosely and I only use the surgical brassiere to hold the bandages in place, not for compression.
Postoperative Care
It is important to have a preoperatively informed patient. They can be your best allies. The pucker can take weeks to months to settle out and I warn patients that I will not do a revision until a full year has passed; everyone worries about the puckers, but only a very few need revision.
DISCUSSION
The medial pedicle simplifies the approach to vertical breast reduction surgery. Not only is the pedicle easier to inset, but also it adds rotation and coning to the breast tissue, resulting in a shape that has good projection.
It is my belief that this is a parenchymal resection and reshaping operation and not a skin brassiere procedure. The skin adapts to the new breast shape in the vertical approach, whereas the skin tries (often poorly) to hold the shape in the inverted T approach.
The medial pedicle also helps to obviate the effects of gravity over time by removing the heavy inferior breast tissue and leaving behind the superior breast tissue (Fig. 9).
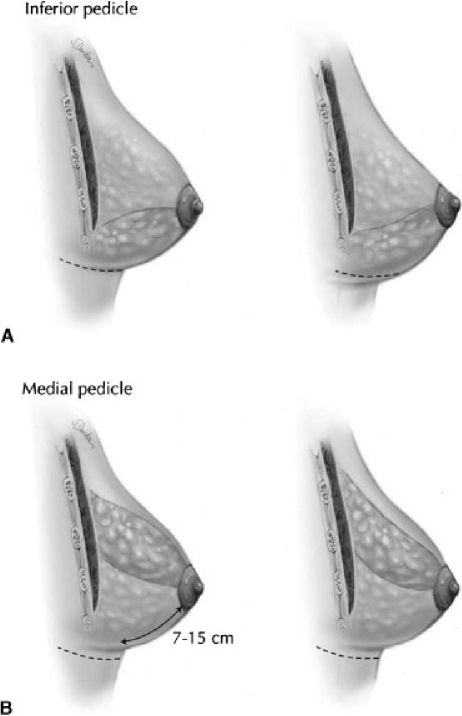
Figure 9.
The inferior pedicle stresses the skin brassiere by leaving tissue for gravity to affect. (A) Bottoming out is likely to occur with the inferior pedicle whether an inverted T or vertical skin resection pattern is used. (B) I believe that a superior, superomedial, or superolateral pedicle is less likely to cause pseudoptosis with time because the breast tissue can be coned better and the weight of the breast is not being carried by the skin.
Although I believe that breast parenchymal sutures hold to some degree, I do not believe that we yet have a solution to a breast that sits low on the chest wall. We need to design the new nipple position according to the position and level of the patient's inframammary fold, not some other ideal. Nor do we have a good solution to a lack of upper pole fullness. Pushing breast tissue up into the upper pole and trying to hold it there with sutures to the pectoralis fascia is doomed to failure as it inevitably drops out. Putting the inferior tissue up under a pectoralis sling has some merit in that it can sometimes add a small amount of fullness.
SUMMARY
The medial pedicle vertical reduction mammaplasty is a simplified approach to breast reduction that results in better scarring and better shape in both the short term and the long term (Figs. 10, 11, and 12). It is faster to perform and there is less blood loss. The recovery for the patient is easier and their satisfaction is high.
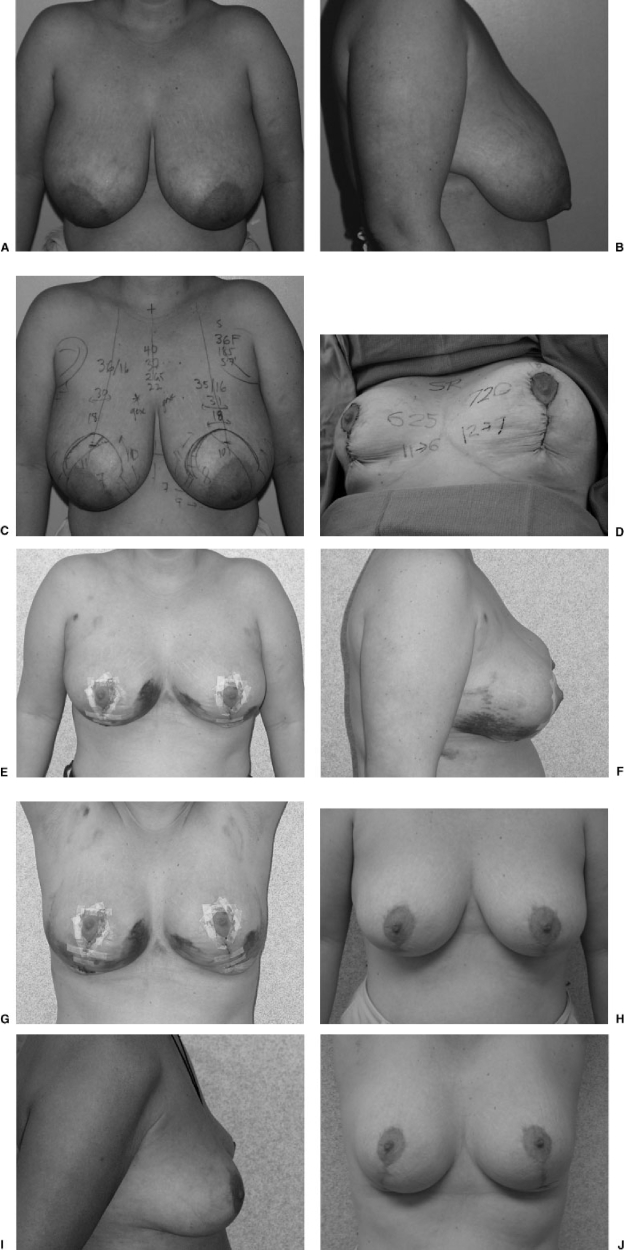
Figure 10.
(A) Preoperative frontal view of moderate-sized breast reduction (34-year-old patient who wore a 36F brassiere, 185 lb, 5′7″). (B) Preoperative lateral view. (C) Preoperative view with markings (many of these measurements are performed for statistical analysis only). The most important markings are noting the level of the inframammary fold (and therefore the new nipple position vertically), the breast and chest wall meridian (and therefore the new nipple position horizontally), as well as the areolar opening, the skin resection pattern, and the medial pedicle design. (D) Intraoperative view at completion of the vertical approach using the medial pedicle. From the right breast, 625 g were removed; 720 g were removed from the left breast. She also had 400 mL of fat removed from the lateral chest wall and preaxillary areas with some contouring of the lower portion of the breasts. Surgery time was 90 minutes. I now gather this incision far less than shown in this photograph. (E) Frontal view at 10 days postoperatively. (F) Lateral view at 10 days postoperatively. (G) Arms up view at 10 days. The results do not necessarily take a long time to settle postoperatively. (H) Frontal view at 15 months postoperatively. (I) Lateral view at 15 months postoperatively. (J) Arms up view at 15 months postoperatively.
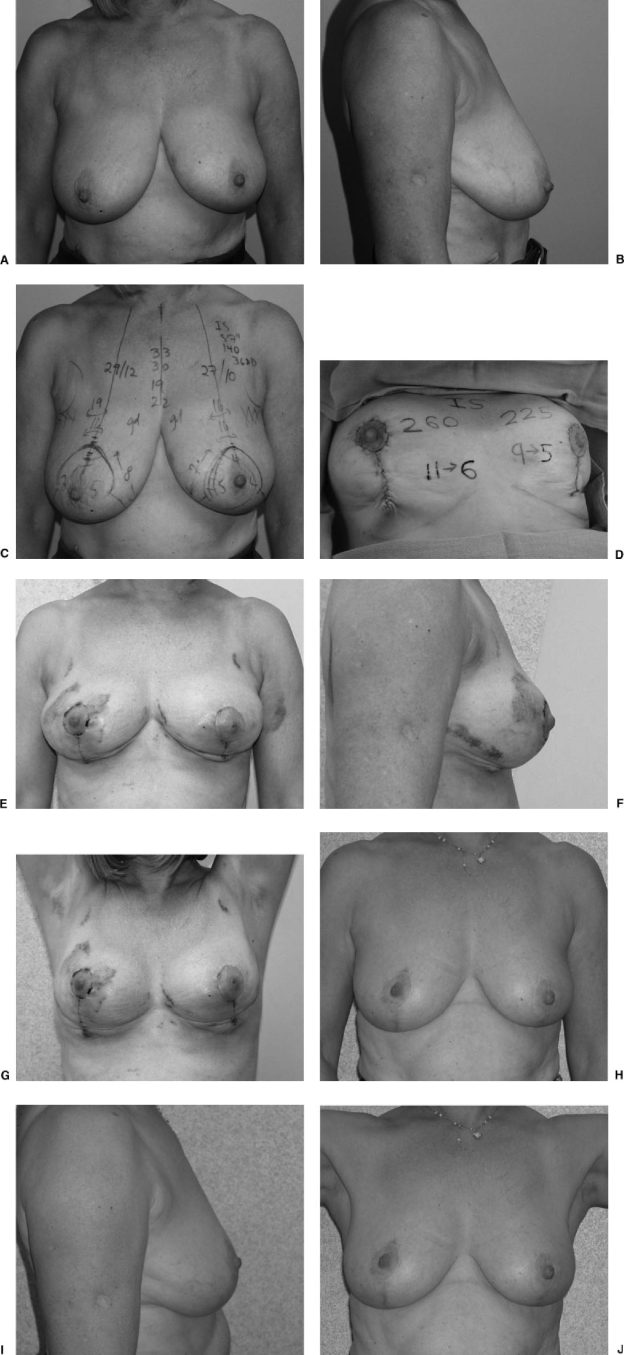
Figure 11.
(A) Preoperative frontal view of small breast reduction (56-year-old patient who wore a 36DD brassiere, 140 lb, 5′7″). (B) Preoperative lateral view. (C) Preoperative view with markings. (D) Intraoperative view at completion of the vertical approach using the medial pedicle. From the right breast, 260 g were removed; 225 g were removed from the left breast. An additional 200 mL of fat was removed from the lateral chest wall and preaxillary areas with some contouring of the lower portion of the breasts. Surgery time was 90 minutes. I now gather this incision far less than shown in this photograph. (E) Frontal view at 2 weeks postoperatively. (F) Lateral view at 2 weeks postoperatively. (G) Arms up view at 2 weeks. The results show some puckering and irregularities. A preoperatively informed patient accepts this and realizes that some time may be needed before it settles. (H) Frontal view at 2 years postoperatively. Note that the nipple is higher on the larger side; it should have been designed at a lower position. (I) Lateral view at 2 years postoperatively. (J) Arms up view at 2 years postoperatively.
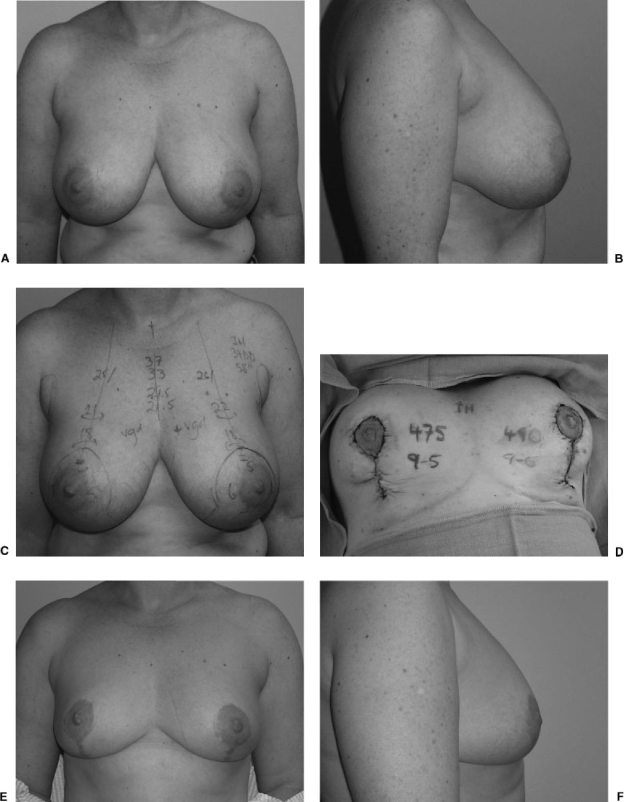
Figure 12.
(A) Preoperative view of average-sized breast reduction (47-year-old patient who wore a 34DD brassiere, 169 lb, 5′6″). (B) Preoperative lateral view. (C) Preoperative markings. (D) Intraoperative view at completion of the vertical approach using the medial pedicle. From the right side, 475 g were removed; 490 g were removed from the left side. She had an additional 260 mL of fat removed from the lateral chest wall and preaxillary areas with some contouring of the lower portion of the breasts. Surgery time was 100 minutes. I now gather this incision far less than shown in this photograph. (E) Frontal view at 2.5 years postoperatively. (F) Lateral view at 2.5 years postoperatively.
REFERENCES
- Hall-Findlay E J. A simplified vertical reduction mammaplasty: shortening the learning curve. Plast Reconstr Surg. 1999;104:748–759. [PubMed] [Google Scholar]
- Hall-Findlay E J. Vertical breast reduction with a medially based pedicle. Operative strategies. Aesthetic Surgery Journal. 2002;22(2):185–195. doi: 10.1067/maj.2002.123052. [DOI] [PubMed] [Google Scholar]
- Hall-Findlay E J. Pedicles in vertical breast reduction and mastopexy. Clin Plast Surg. 2002;29:379–391. doi: 10.1016/s0094-1298(02)00008-1. [DOI] [PubMed] [Google Scholar]
- Robbins T H. A reduction mammaplasty with the areola-nipple based on an inferior pedicle. Plast Reconstr Surg. 1977;59:64–67. doi: 10.1097/00006534-197701000-00011. [DOI] [PubMed] [Google Scholar]
- Courtiss E H, Goldwyn R M. Reduction mammaplasty by the inferior pedicle technique. An alternative to free nipple and areola grafting for severe macromastia or extreme ptosis. Plast Reconstr Surg. 1977;59:500–507. [PubMed] [Google Scholar]
- Georgiade N G, Serafin D, Morris R, Georgiade G. Reduction mammaplasty utilizing an inferior pedicle nipple-areolar flap. Ann Plast Surg. 1979;3:211–218. doi: 10.1097/00000637-197909000-00003. [DOI] [PubMed] [Google Scholar]
- Courtiss E H. Reduction mammaplasty by suction alone. Plast Reconstr Surg. 1993;92:1276–1284. [PubMed] [Google Scholar]
- Matarasso A, Courtiss E H. Suction mammaplasty: the use of suction lipectomy to reduce large breasts. Plast Reconstr Surg. 1991;87:709–717. [PubMed] [Google Scholar]
- Gray L N. Liposuction breast reduction. Aesthetic Plast Surg. 1998;22:159–162. doi: 10.1007/s002669900184. [DOI] [PubMed] [Google Scholar]
- Gray L N. Update on experience with liposuction breast reduction. Plast Reconstr Surg. 2001;108:1006–1010. doi: 10.1097/00006534-200109150-00031. [DOI] [PubMed] [Google Scholar]
- Dufourmentel C, Mouly R. Plastie mammaire par la methode oblique. Ann Chir Plast. 1961;6:45. [PubMed] [Google Scholar]
- McKissock P K. Reduction mammaplasty with a vertical dermal flap. Plast Reconstr Surg. 1972;49:245–252. doi: 10.1097/00006534-197203000-00001. [DOI] [PubMed] [Google Scholar]
- Strombeck J O. Mammaplasty: report of a new technique based on the two-pedicle procedure. Br J Plast Surg. 1960;13:79–90. doi: 10.1016/s0007-1226(60)80014-8. [DOI] [PubMed] [Google Scholar]
- Biesenberger H. Eine neue methode der mammaplastik. Zentralbl Chir. 1928;55:2382. [Google Scholar]
- Wiener D L, Aiache A E, Silver L, Tittiranonda T. A single dermal pedicle for nipple transposition in subcutaneous mastectomy, reduction mammaplasty or mastopexy. Plast Reconstr Surg. 1973;51:115. doi: 10.1097/00006534-197302000-00001. [DOI] [PubMed] [Google Scholar]
- Lejour M, Abboud M, Declety A, Kertesz P. Reduction des cicatrices de plastie mammaire: de l'ancre courte a la verticale. Ann Chir Plast Esthet. 1990;35:369–378. [PubMed] [Google Scholar]
- Lejour M. Vertical Mammaplasty and Liposuction of the Breast. St Louis: Quality Medical Publishing; 1993.
- Lejour M. Vertical mammaplasty and liposuction of the breast. Plast Reconstr Surg. 1994;94:100–114. doi: 10.1097/00006534-199407000-00010. [DOI] [PubMed] [Google Scholar]
- Lejour M, Abboud M. Vertical mammaplasty without inframammary scar and with breast liposuction. Perspectives in Plastic Surgery. 1996;4:67–90. [Google Scholar]
- Skoog T. A technique of breast reduction—transposition of the nipple on a cutaneous vascular pedicle. Acta Chir Scand. 1963;126:453–465. [PubMed] [Google Scholar]
- Asplund O, Davies D M. Vertical scar breast reduction with medial flap or glandular transposition of the nipple-areola. Br J Plast Surg. 1996;49:507–514. doi: 10.1016/s0007-1226(96)90126-5. [DOI] [PubMed] [Google Scholar]
- Lassus C. A technique for breast reduction. Int Surg. 1970;53:69–72. [PubMed] [Google Scholar]
- Marchac D, de Olarte G. Reduction mammaplasty and correction of ptosis with a short inframammary scar. Plast Reconstr Surg. 1982;69:45–55. [PubMed] [Google Scholar]
- Lassus C. Breast reduction: evolution of a technique. A single vertical scar. Aesthetic Plast Surg. 1987;11:107–112. doi: 10.1007/BF01575495. [DOI] [PubMed] [Google Scholar]
- Lassus C. A 30-year experience with vertical mammaplasty. Plast Reconstr Surg. 1996;97:373–380. doi: 10.1097/00006534-199602000-00015. [DOI] [PubMed] [Google Scholar]
- Wise R J. A preliminary report on a method of planning the mammaplasty. Plast Reconstr Surg. 1956;17:367–375. doi: 10.1097/00006534-195605000-00004. [DOI] [PubMed] [Google Scholar]
- Graf R, Auersvald A, Bernardes A, Biggs T M. Reduction mammaplasty and mastopexy with shorter scar and better shape. Aesthetic Surg J. 2000;20:99–106. [Google Scholar]
- Graf R, Biggs T M, Steely R L. Breast shape: a technique for better upper pole fullness. Aesthetic Plast Surg. 2000;24:348–352. doi: 10.1007/s002660010057. [DOI] [PubMed] [Google Scholar]
- Graf R, Biggs T M. In search of better shape in mastopexy and reduction mammaplasty. Plast Reconstr Surg. 2002;110:309–317. doi: 10.1097/00006534-200207000-00053. [DOI] [PubMed] [Google Scholar]
- Corduff N, Taylor G I. Subglandular breast reduction: the evolution of a minimal scar approach to breast reduction. Plast Reconstr Surg. 2004;113:175–184. doi: 10.1097/01.PRS.0000095945.27892.48. [DOI] [PubMed] [Google Scholar]
- Schlenz I, Kuzbari R, Gruber H, Holle J. The sensitivity of the nipple-areola complex: an anatomic study. Plast Reconstr Surg. 2000;105:905–909. doi: 10.1097/00006534-200003000-00012. [DOI] [PubMed] [Google Scholar]
- Gradinger G P. Reduction mammaplasty utilizing nipple-areola transplantation. Clin Plast Surg. 1988;15:641–654. [PubMed] [Google Scholar]
- Gradinger G P. Discussion: maximizing breast projection after free-nipple-graft reduction mammaplasty. Plast Reconstr Surg. 2001;107:961–964. [PubMed] [Google Scholar]
- Schwartzmann E. Avoidance of nipple necrosis by preservation of corium in one-stage plastic surgery of the breast. Rev Chir Struct. 1937:206–209. [Google Scholar]