ABSTRACT
Thighplasty after massive weight loss is daunting. The deformity is complex and difficult to treat. The therapeutic index is narrow. A range of only centimeters of medial thigh skin resection width can mean the difference between residual skin laxity and unsightly descended scars. Wound closure is awkward. The scar from vertical extension excisions is exposed. Delayed healing is common. Prolonged edema and thrombophlebitis loom. Disappointed with prevalent lower body and thigh recontouring procedures, I evolved a comprehensive approach, which includes the “L thighplasty.” The “L” relates to the shape of the excision and resulting scar with the long limb along the medial thigh and the short limb between the thigh and labia majora and mons pubis. The planning, technique and selected results are presented.
Keywords: Medial thighplasty, weight loss surgery, lower body lift
Medial thighplasty is aesthetic reshaping of the thigh following removal of excess medial skin and fat.1,2,3,4,5 The new contour should be attractive, the scars inconspicuous, and complications minor. Medial thighplasty may be solely an upper thigh crescent excision adjacent to the labia majora (scrotum),2,5 extended with a wide band excision tapering at the knee for distal deformity,3,4,6 or something in between. The extent of the operation depends on the deformity and the patient's expectations and acceptance of risk. The essential facets to improve thigh contour are excision of medial thigh skin, lipoplasty, efficient use of prone and supine operative positions, accurate presurgical marking of a unique excision design using multiple patient positions, and single-stage integration of the medial lift into the lower body operative correction.
Contrary to some experts,3,4,5,7,8,9 I find medial thighplasty complementary to lower body lift and abdominoplasty.6,10,11,12 The combined procedures are synergistic, capitalizing on the biomechanics of skin tension. For the most favorable cases, I offer single-stage total body lift surgery.8 With unacceptable distal thigh redundancy, I recommend the L vertical thighplasty. The additional work involved with an extended thigh lift usually precludes a simultaneous upper body lift.
CLINICAL PRESENTATION
Obesity causes considerable excess subcutaneous fat in the thighs and hips. Women circumferentially enlarge their thighs, except for the distal lateral portion. Men mostly fill their anterior and medial portions and not along the lateral thigh. Rapid massive weight loss through caloric deficit catabolizes these fat stores and to a lesser extent some of the supporting connective tissue. Gastric bypass reduces the pepsinogen enzyme contact with ingested protein, thereby reducing essential amino acid digestion.
The thigh weight loss deformity varies by genetic predisposition, extent of loss, and residual obesity. For the obese female who has lost most of her excess weight, there is a characteristic presentation (Figs. 1, 2). Except for the lower lateral thigh, the skin is diffusely loose and flaccid. The upper lateral thighs bulge into what is commonly referred to as saddlebags, abruptly stopping at the midthigh. The buttocks skin atrophies, leaving inferior accordion-like pleats of skin. Looseness of the upper posterior thigh is less dramatic. The medial thighs invariable sag with cascading rolls of skin, progressively diminishing toward the knees. The anterior thighs have stacked waves of skin. The appearance with the severest weight loss resembles melted candle wax (Figs. 3–5). Incomplete weight loss leaves bulging thighs (Figs. 6, 7).
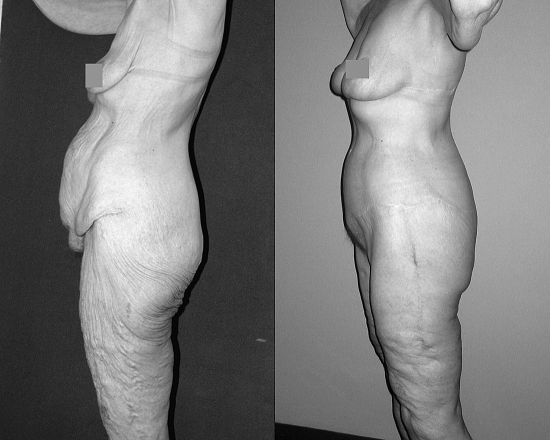
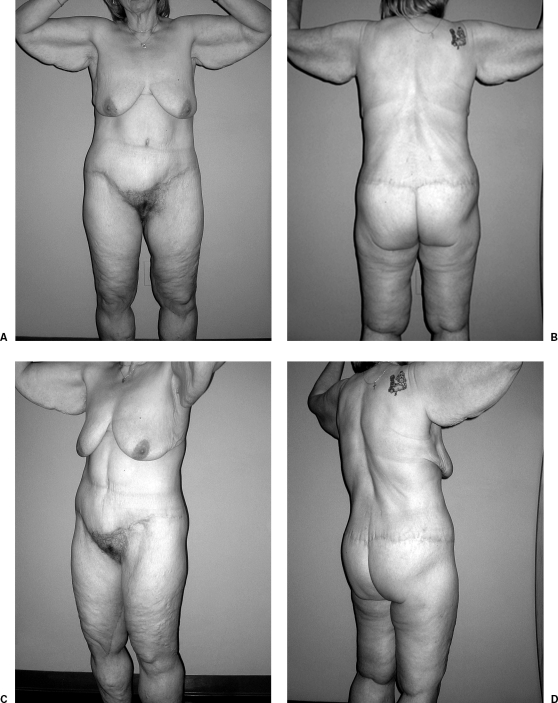
Figure 1.
The thighs of a 49-year-old, 5 feet, 7 inch, 157-pound woman after she lost 230 pounds subsequent to a gastric restrictive procedure. Her rolls of redundant skin are worst in the medial and least in the upper anterior and lower lateral thigh. The middle anterior thighs have stacked layers of skin resembling melted candle wax. Loose skin hangs from the hips to the midlateral thigh. The buttocks have inferior accordion-like pleats. The L thighplasty markings have been drawn and are better visualized when she elevates her abdominal pannus and upper medial thighs.
Figure 2.
Posterior and lateral views of the patient in Fig. 1.
Figure 3.
A 58-year-old, 5 foot, 7 inch woman weighing 130 pounds after losing 188 pounds has dramatic loose skin circumferentially around her thighs. Extreme wrinkling of the anterior thighs, resembling melted wax, is seen on these standing views. The 1-year results after a two-stage total body lift with L thighplasties and brachioplasties are seen.
Figure 4.
Before and after views of the patient in Fig. 3.
Figure 5.
Figure 6.
A 60-year-old, 5 foot, 7 inch, 200-pound women has persistent oversized and sagging thighs after gastric bypass and 150 pounds of weight loss. Fat excess billows out everywhere but most prominently along the medial thighs, hips, and saddlebags. The markings for her operation have just been completed. The pluses indicate anticipated relative amounts for liposuction.
Figure 7.
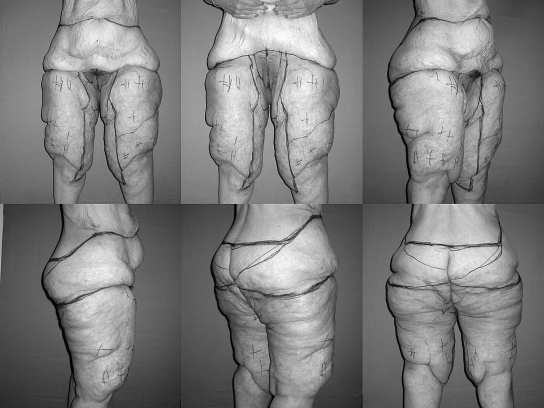
This composite figure shows the essential steps in marking the L thighplasty. (Upper left) By appropriate cephalad traction on the abdominal pannus, the lower incision line of the abdominoplasty is drawn. (Upper right) The leg is moderately abducted as the loose inner thigh skin is pushed toward the knee to mark the upper incision line between the labia majora and thigh. (Middle left) The point of maximal resection along the midmedial thigh is determined with the thigh flexed and adducted. After pushing loose skin beneath the pubic ramus, the midmedial thigh inferior resection line is marked. (Middle right) With the leg again abducted, the crescent-shaped inferior incision line from this inferior resection mark is extended anterior to the outer mons pubis line and posterior to the buttock thigh junction line. Later, while the patient is standing and the lifted buttock position simulated, the dog ear triangular inferior gluteal thigh resection is made. (Lower left) The patient remains supine during planning of the long limb of the vertical band extension to the knee. With medial drag on the anterior thigh skin, the anterior excision line is drawn along the midmedial line. Then the width of maximal resection at the midthigh is gathered as shown and this point is marked. (Lower right) From this midthigh mark, a widening posterior incision line is drawn from below the knee to the ischial tuberosity. Finally, the angle between this vertical limb and the upper crescent excision is narrowed by edging the superior portion of the anterior line further posterior. The patient then stands to adjust the markings.
Weight loss patients usually desire thighplasty. Hating their appearance, they hide under tent-like skirts and baggy pants. Panniculectomy further exposes the unsightliness. Repugnant odors emanate. Some are tormented by red chafed skin under folds. Sagging inner thighs coupled with an overhanging abdominal apron and mons pubis rob self-esteem. These patients shun intimacy. They invariably welcome an upper medial thighplasty but may need encouragement to accept the medical vertical extension scar.
After full evaluation of the medial thigh problem, it is placed in the context of the remaining thigh and lower body deformity. During the examination the lower body lift can be simulated by having the patient pull up on her lower abdomen, buttocks, and saddlebags. The lateral thigh should be tight and the residual thigh redundancy mainly anterior and medial.
While the patient is standing, overall thigh skin drape, excess, bulges, and tension are observed. Exceptional residual obesity is treated by liposuction or further weight loss. The examination continues with the patient suspending the abdominal apron. This aids visualization and simulates anticipated tension on the upper thigh. When medial thighs touch, liposuction should be considered. The pattern of sagging is observed. Loose skin of the inner thigh tends to be greatest proximally. The relationship of skin to underlying adipose is noted. Thin tissues need no or little discontinuous undermining. Bulging fat suggests the need for liposuction.
After simulating the anticipated crescent excision by firmly pulling up the sagging skin of the upper thigh to the labia majora, one examines the remaining inner thigh. If the patient still objects to her distal thigh laxity, explain that her upper lift will be inadequate. If the distal thigh is acceptable, the vertical band extension is unnecessary. One should grasp the distal excess and shake it to be sure the patient understands what will be left behind if a vertical lift is not done.
In oversized thighs, primary healing is unlikely. Fat necrosis, skin separations, and troublesome suture-related abscess occur. For the borderline overweight thigh, I gently remove fat by Vaser® LipoSelectionSM (Sound Surgical Technologies, Boulder, CO). Along with their Ventex™ aspiration system, the supportive subcutaneous tissue and vascularity are maximally maintained, encouraging faster healing and better skin retraction. I acknowledge that I was a member of the original scientific advisory board of Sound Surgical Technologies with unexercised stock options.
OPERATIVE PROCEDURE
Inconspicuous, predictable scar location is essential. Scar position is related to the extent, location, and closure tension of the skin excision. The magnitude of skin removal is determined through tissue gathering maneuvers preferably of the most redundant sites. Gender-specific contour is enhanced by selective retention of subcutaneous tissue. Regimented planning gives confidence to judge the position and width of each skin resection, ensuring accurate scar location. Then the adjacent dependent region can be planned. For example, the drawing for the crescent medial thighplasty begins only after the design for abdominoplasty is complete. Likewise, the medial thigh vertical excision extension follows the design of the upper crescent. Figure 1 simulates the changes effected by sequential operations.
Traditionally, incision location is customarily sighted while the patient is standing. However, the magnitude of the hanging pannus, buttocks, and thigh skin in the patient with massive weight loss is awkward. Hence, a sequence of recumbent body and limb positioning for orderly, unrestricted, and painless tissue gathering and incision drawing was developed. Markings start with the abdominoplasty and lower body lift. Once that belt-like excision is planned, the markings commence for the medial thighplasty.6
The upper crescent medial thighplasty markings are made in the same way whether or not a vertical band extension is performed (Fig. 7). The patient is supine with the leg flexed (raised) and slightly abducted. With the loose inner thigh skin pushed toward the knee, the upper incision line is drawn between the labia majora and thigh. This line is a continuation of a perpendicular dropped from the transverse lower abdominoplasty incision. Posterior to the labia, the upper line continues beyond the ischial tuberosity. The point of maximal resection along the midmedial thigh is determined with the thigh flexed and adducted. Pushing all loose skin beneath the pubic ramus, the inferior resection line is marked at the level of the labia majora. With the thigh skin again abducted, a crescent-shaped inferior incision line is extended from this inferior resection mark anterior to the outer mons pubis line and posterior to the buttock thigh junction line. This outer mons pubis line is a second perpendicular line made several centimeters lateral to the first lateral mons pubis line. The width of this resection of paramedian pubic skin is just enough to efface the mons pubis. While the patient is standing and the lifted buttock position simulated, the dog ear triangular gluteal thigh resection is estimated and marked.
Next, the medial vertical band extension to the knee is planned (Fig. 7). With the leg on the bed, the anterior excision line from medial knee up the thigh to the apex of the crescent excision line is drawn. A posterior medial meridian is estimated by medial drag on the anterior thigh skin. The maximal resection at the midthigh is then gathered, and this point is marked. From this midthigh mark, a widening posterior incision line is drawn from below the knee to the ischial tuberosity. The angle between this vertical limb and the upper crescent excision is narrowed by edging the superior portion of the anterior line posterior. This moves the scar posterior to form an L shape. For symmetry, the lines are again inked and then the thighs are rubbed together to imprint on to the opposite thigh. Nevertheless, the appropriate extent of the opposite side excision is confirmed by tissue gathering. The patient then stands as seen in Figure 1 to adjust the markings.
The thighplasty begins with the lower body lift. The surgeon stands to the right side of the prone patient, facing the buttocks, to excise the broad band of skin and adipose and close the posterior wound. The midlateral wide torso resection is closed tightly to efface the saddlebag deformity. To close the gap under the least tension, the leg is abducted on a wide arm board. Large, deeply placed absorbable sutures secure the lateral thigh deep dermis to the fascia lata of the thigh. The excision is closed with very large permanent braided sutures in the subcutaneous fascia, followed by intradermal long-lasting monofilament absorbable sutures.
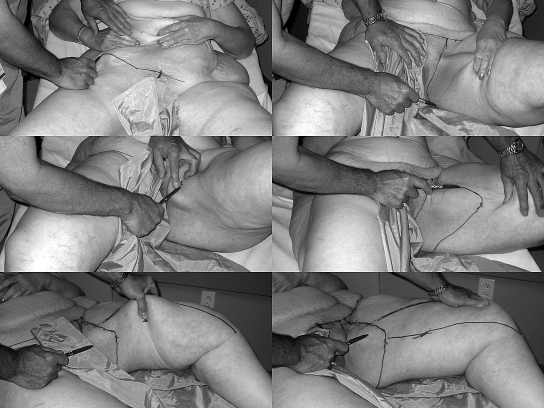
While assistants close the lower body lift, the surgeon removes the anticipated infragluteal dog ears of the medial thighplasties under the buttock folds. In the unusual situation in which the posterior thigh is very loose, this excision can be beyond 8 cm. The infragluteal dog ear excision is best made after the buttock lift is completed. The width of triangular excision is adjusted inferiorly as needed. The skin resection of this dog ear is thin to avoid injury to buttock sensory inferior cluneal nerves and nutrient vasculature to the distal thigh. If a wide vertical band excision is planned, the posterior limbs are incised through deep subcutaneous fascia. The terminal incision may fishtail anterior to the knee or posterior toward the popliteal fossa. Prior to turning the patient supine, the posterior vertical thigh incision is temporarily approximated with staples (Fig. 8).
Figure 8.
A view of the prone patient from the foot of the operating room table at the completion of the lower body lift, closure of the infragluteal dog ear extensions, and incision of the posterior band of the vertical thighplasty. The prone position aids in team surgery and symmetrical results. Prior to turning the patient supine, the vertical incision is closed with staples.
The patient is wrapped into a surgeon's gown, turned supine, and frog legged. The abdominoplasty is resumed with the inferior incision from the anterior superior iliac spine across the groins through the mons pubis and completed across the other side. Broad suprafascial dissection continues to the umbilicus. The umbilicus is cut out as an inverted triangle. The dissection continues as a narrow midline band to the xyphoid. After removal of excess from the superior abdominoplasty flap, the operating room table is flexed. Towel clips approximate the abdominal flap along the groins and mons pubis.
As assistants suture closed the abdominoplasty, the surgeon resumes the medial thighplasty. The longitudinal anterior incision is made through skin to muscular fascia. Several centimeters of undermining develop a subcutaneous edge for suture closure. Skin and underlying adipose are raised from knee to the labia majora superficial to the fascia lata. Distal thigh lymphatics should be preserved. The vertical extension is approximated with towel clamps and closed from knee to upper inner thigh in two long-lasting absorbable monofilament sutures (Fig. 9).
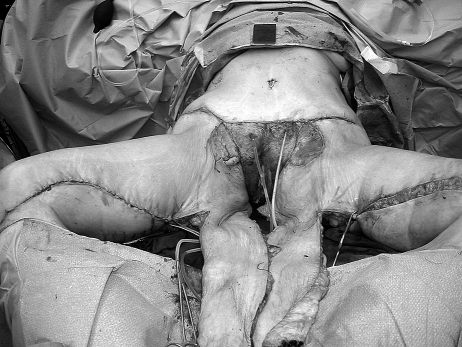
Figure 9.
The patient has been turned supine and the abdominoplasty completed. The planned vertical band excision was rechecked, excised to subcutaneous fascia, and closed in two layers of continuous absorbable suture. The horizontal crescent can now be excised after reevaluation.
The final step of the L vertical medial thighplasty is resection of the transverse proximal crescent. The width of that resection is now adjusted. Adduction of the thigh helps gauge this resection. The resection tapers along the mons pubis to reach the abdominoplasty closure. The paramons vertical resections start 6 to 7 cm from the midline, and each is about 4 cm in width. The paramedian mons pubis skin resections are only skin deep to avoid injury to groin lymphatics. A large multiprong rake retractor elevates the lateral edge of the incised labia and blunt-tipped scissors expose Colles fascia along the lateral pubic bone. The round ligament or spermatic cord may need to be pushed out of the way. One should avoid cutting any structures as the genitofemoral nerve also travels this path.
With the helping hand finger palpating the pubis as a guide, three heavy braided permanent sutures are placed into Colles fascia (even pubic tuberosity periosteum) deep to the labia majora. I prefer 0 Braillon with a taper pop-off needle (US Surgical, Danbury, CT). Then each stitch generously bites the anterior thigh subcutaneous fascia. The thigh is adducted to tie the three deep braided sutures under mild tension. Then the mons plasty is sutured closed in two more layers superiorly and the medial thigh to labial junction to the ischial tuberosity inferiorly The completed thigh suture line resembles an L with the long limb down the thigh and the short limb along the labia and mons pubis (Fig. 10). The serif tail lies along the buttock thigh fold (the closed dog ear). The skin should be tight throughout but with no tension on the labii majora. Two anterior abdominal suction drains are placed through pubic stab wound incisions and extended laterally over the flanks. A supportive below-knee elastic garment is worn without gauze dressings.
Figure 10.
The just closed suture line resembles an L with the long limb running from the medial knee to the ischial tuberosity and the short limb extending from there along the labial majora lateral to the mons pubis.
POSTOPERATIVE CARE
Throughout the procedure and during the 2- to 4-day hospitalization, automatic alternating pressure lower leg stockings function. Lower torso drains are removed when daily output is less than 50 mL each, which is in about 10 days.
The patient will gain about 10 pounds of weight because of large-volume fluid administration and postsurgical total body fluid retention. This makes patients look and feel poorly. If the natural diuresis is delayed beyond 3 days, oral diuretics are started. To expedite edema resolution and improve skin quality, we prefer to start Endermologie' (LPG, Miami, FL) within 2 weeks. Home use of an automatic pressure device such as a Lymphapress can be helpful.
The suture lines are covered with Steri-Strips or dermal glue for added security and to minimize topical care. When gauze dressings are used, they need to be changed several times a day. All suture lines are inspected daily for skin vitality and separation. Routinely, the inner thigh to labial closure is moist and, despite best efforts for a secure closure, small gaps are common. Meticulous wound care with bland soap cleansing and dry dressings reduces irritation and malodor. Antifungal creams may be needed.
I favor postoperative compression garments and currently use the black, lace-bordered long leg wraps by Inamed (Santa Barbara, CA). The crotch opening exacerbates uppermost medial thigh and pubic swelling.
COMPLICATIONS AND THEIR MANAGEMENT
Premature removal of drains leads to seromas. Seromas are tense or bolatable asymmetrical swellings. Large-bore needle aspirations are both diagnostic and therapeutic. Local compression with a Reston sponge and elastic wrap is tried for several days. If serum accumulates, aspiration is repeated or preferably a percutaneous drainage catheter is inserted, sutured in place, and connected to a suction bulb. Seven to 10 days later it is removed. Once a scarred seroma cavity is formed, compete resolution may require injection of sclerosing agents or surgical excision with quilting suture closure.
Several weeks after surgery, a firm deep slightly tender mass may be palpable above the medial knee. Upon aspiration this invariably yields straw-colored watery fluid, which refills to firmness within a day, suggestive of a lymphocele. Prolonged closed suction drainage usually resolves the problem. When a small tense mass persists, it is left alone as it tends to resolve by sclerosis. An abscess developed in four patients that required intraoperative drainage and outpatient wound care with antibiotic. Healing of one wound was expedited with vacuum-assisted care.
Inadequate care and excessive activity can lead to troublesome thigh swelling. Skin edge necrosis is followed by suture line dehiscence. Because of the tightness of the closure and persistent swelling, a conservative wound care approach is taken. Débridement is performed to pain tolerance and bleeding. Then topical débriding agents are left to do the rest, allowing secondary closure.
Descent of the labial thigh scars and distortion of the labii are feared long-term complications. With the introduction of the Colles fascia stitch, I believe that problem uncommon.5 Nevertheless, overresection of medial thigh skin cannot be overcome by those sutures. Skin grafts are the most expedient means to correct the labial deformity but may be rejected as unsightly by the patient. Theoretically, tissue expansion, although awkward in this location, should yield more skin. If there is residual transverse laxity of thigh skin, a limited vertical band excision can raise the scar and take distorting tension off the labii majora.
Weight loss patients with unstable chronic illnesses and cardiovascular disease, postphlebitic syndrome, or lymphedema are not candidates for this surgery. Neither are patients with unresolved depression or unrealistic expectations. Figure 11 shows the 6-month postoperative result of the patient in Figures 1 and 2.
Figure 11.
Except for the distal thigh, the postoperative views show the deformities in Figures 1 and 2 to be corrected by a single complex 10-hour operation, just described. The scars are level, symmetrical, and narrow. There are long but inconspicuous scars running down the medial posterior thighs, between the labia and thigh, and in a belt-like manner around the lower torso. The buttock curvature is full due to the adipose flap reconstruction. There is some residual looseness below the buttocks and about the knees, which will be corrected secondarily.
CONCLUSION
Body contouring surgery after massive weight loss is reconstructive surgery with aesthetic goals. The upper inner thighplasty does not improve circumferential excess of the middle to lower thighs. Vertical inner thigh band extensions have been described but for the most part with no technical detail. My L thighplasty differs from Renault's extended thighplasty.2 She describes a vertical extension from a circular excision around the lower buttocks and across the groins.2 Those scars are unacceptable. The mons pubis ptosis is undertreated. I agree that the designs of her extended thighplasty and abdominoplasty cause conflicting skin tensions and therefore must be staged.
The recently designed L thighplasty with a vertical extension improves the distal two thirds of oversized thighs. The long limb excision reduces circumferential excess to tighten the anterior medial and posterior thigh. The short limb suspends the upper thigh and improves the mons pubis. If this lengthy resection is not done on heavy thighs, leaving the weight contributes to descent of the medial thigh scar and to recurrence of the saddlebag deformity.
For the crescent medial thighplasty, a properly positioned labia-thigh scar is an acceptable trade-off for objectionable loose inner skin. In the L thighplasty, the vertical scar is better accepted if it lies posterior to the median line of the thigh and extends toward the ischial tuberosity. Most of these scars mature into fine lines and are not visible on exposed thighs during walking. The aesthetic shortcoming is residual loose skin about the knee despite attempts at tight oblique closures. Secondary low transverse excisions address this problem.
Concomitant abdominoplasty and lower body lift with the L medial thighplasty does improve severe lower torso and thigh laxity with reasonable scars and minor complications. Accurate presurgical marking in an L pattern and efficient use of multiple positions are essential. The prone and supine operative positions expedite efficient, symmetrical surgery. Chronic leg edema is preempted by postoperative leg compression. Heavy thighs may benefit from preliminary lipoplasty.
I started combining the lower body and medial thighplasty because there is so much that needs to be corrected in these patients with massive weight loss. The recognized expert on the modern lower body lift and upper medial thighplasty, Ted Lockwood, originally combined these procedures.5 However, by 2001 he preferred to stage the transverse medial thighplasty after the lower body lift.7,8 He argued that medial thigh laxity is improved by the abdominoplasty and lower body lift.5 A staged upper medial thigh lift is performed later, if necessary.
We agree that the lower body lift raises the lateral thighs and buttocks through a circumferential wide belt-like excision of skin and discontinuous undermining of the lateral thighs. A byproduct of the high lateral tension abdominoplasty is some suspension of the proximal anterior and medial thigh. We both close the lateral portion of the lower body lift under high tension and temporarily reduce the tension by full abduction of the thigh (my patients are prone with the leg abducted on an arm board and Lockwood's are lateral with the leg abducted on pillows). Upon completion of the lateral closure, the legs are adducted, which transmits tautness along the entire lateral thigh.
My closure of the crescent portion of the medial thighplasty is completed with the leg adducted, forcing the vector of body lift pull completely cephalad. This is the optimal time for the medial thighplasty because cephalad pull of the lower body lift and abdominoplasty is at its greatest.6
The combined lower body lift, abdominoplasty, and L thighplasty is a complex elective correction of a difficult clinical problem. Through experience, organization, and team surgery, the results have been good, the complications minor, and patients' satisfaction high.
ACKNOWLEDGMENT
This article has been adapted from my manuscript for chapter 8, “Approach to the medial thighplasty,” in Body Contouring after Massive Weight Loss, edited by A. Matarrasso and P. Rubin, Elsevier, Germany, 2006.
REFERENCES
- Lewis J R. The thigh lift. J Int Coll Surg. 1957;27:330–334. [PubMed] [Google Scholar]
- Schultz R C, Feinberg L A. Medial thigh lift. Ann Plast Surg. 1979;2:404–410. doi: 10.1097/00000637-197905000-00007. [DOI] [PubMed] [Google Scholar]
- Regnault P, Daniel R K. In: Regnault P, editor. Aesthetic Plastic Surgery: Principles and Techniques. Philadelphia, PA: Lippincott Williams & Wilkins; 1984. Lower extremity. pp. 655–678.
- Regnault P, Daniel R K. In: Regnault P, editor. Aesthetic Plastic Surgery: Principles and Techniques. Philadelphia, PA: Lippincott Williams & Wilkins; 1984. Massive weight loss. pp. 705–720.
- Lockwood T. Fascial anchoring technique in medial thigh lifts. Plast Reconstr Surg. 1988;82:299–304. doi: 10.1097/00006534-198808000-00015. [DOI] [PubMed] [Google Scholar]
- Hurwitz D J. Medial thighplasty. Aesthetic Surg J. 2005;25:180–191. doi: 10.1016/j.asj.2005.01.013. [DOI] [PubMed] [Google Scholar]
- Lockwood T. Lower-body lift. Aesthetic Surg J. 2001;21:355–370. doi: 10.1067/maj.2001.118028. [DOI] [PubMed] [Google Scholar]
- Lockwood T E. Maximizing aesthetics in lateral-tension abdominoplasty and body lifts. Clin Plast Surg. 2004;31:523–537. doi: 10.1016/j.cps.2004.04.001. [DOI] [PubMed] [Google Scholar]
- Aly A S, Cram A E, Chao M, Pang J, McKeon M. Belt lipectomy for circumferential truncal excess: the University of Iowa experience. Plast Reconstr Surg. 2003;111:398–413. doi: 10.1097/01.PRS.0000037873.49035.2A. [DOI] [PubMed] [Google Scholar]
- Hurwitz D J, Zewert T. Body contouring surgery in the bariatric surgical patient. Oper Tech Plast Surg Reconstr Surg. 2002;8:87–95. [Google Scholar]
- Hurwitz D J. Single stage total body lift after massive weight loss. Ann Plast Surg. 2004;52:435–441. doi: 10.1097/01.sap.0000123361.14654.a5. [DOI] [PubMed] [Google Scholar]
- Hurwitz D J, Rubin J P, Risen M, Sejjadian A, Serieka S. Correcting the saddlebag deformity in the massive weight loss patient. Plast Reconstr Surg. 2004;114:1313–1325. doi: 10.1097/01.prs.0000135862.83833.5f. [DOI] [PubMed] [Google Scholar]