ABSTRACT
Laser periocular surgery has achieved an increased popularity, particularly since the widespread use of CO2 and erbium:yttrium aluminum garnet laser and more recently with the development of nonablative laser technology. The main target of these techniques is to treat photoaging changes to obtain a rejuvenated skin. Despite the relatively safety of these procedures on experienced hands, postoperative complications affecting the periocular region, and the eye itself, may follow laser surgery. More common complications include persistent erythema, hyper- and hypopigmentation, and hypertrophic scarring. Viral, bacterial, or fungal skin infections may also jeopardize the postoperative period after periocular laser treatment. Severe burns, transitory or permanent lower lid ectropion, and even corneal injuries or ocular perforation are among the most severe hazards. The majority of these complications are related to the use of ablative technologies. A thoughtful preoperative evaluation, conscientious patient selection, comprehensive informed consent, adequate training, and a cautious and conservative approach are reinforced to minimize moderate or even severe aesthetic and functional periocular complications. Nonablative laser therapies are notably safer; however, their ability to significantly improve photoaged skin characteristics is still limited.
Keywords: Laser surgery, complication, rejuvenation, periorbital
The periocular region is commonly the target of a wide variety of laser treatments. This region plays a major aesthetic role and therefore should be conveniently addressed in treatments pursuing a facial rejuvenation of the upper and midface. Moreover, this area is particularly prone to develop photoaging changes, degenerations, and benign tumors that may be adequately treated with laser technology. Hence, different types of lasers have been used in distinct applications in the periocular region. The use of argon laser has been reported for endonasal lacrimal surgery, epilation of trichiasis lashes, treatment of benign eyelid tumors, angiomas, and telangiectasias.1,2 Various modalities of yttrium aluminum garnet (YAG) lasers were employed in lachrymal surgery and treatment of periocular angiomas.3,4 Dye lasers may also be suitable for treatment of periocular cutaneous vascular abnormalities.1 However, the most widespread lasers in periocular surgery are the new-generation carbon dioxide (CO2) and the erbium:YAG lasers, which have reached an increasing popularity.
CO2 laser was incorporated into orbital and eyelid surgery as a result of its ability to simultaneously cut tissues and produce hemostasis. These properties allowed this modality to be especially suitable for treatment of poorly circumscribed vascular orbital lesions like orbital lymphangiomas.5 Further technical advancements justified its use in cosmetic procedures. Hence, it has been incorporated by some surgeons, particularly in lower lid blepharoplasty, who claim it is faster, with less bleeding and postoperative hematoma and discomfort.6 But the most widespread use of both CO2 and erbium:YAG laser is cutaneous resurfacing. The benefits of laser resurfacing for treating rhytids, wrinkles, photoaging, acne scars, and other skin imperfections in the periocular region and the full face are well known and documented.7,8,9 This technique represented an alternative to chemical peel or dermabrasion and became the procedure of choice for this purpose until the development of new nonablative techniques.
Despite the tremendous technical refinement of laser technology and the fascination that laser technology exerts on patients and therefore its marketing power, periocular laser surgery is not exempt of complications, some of them potentially severe.10,11 The goal of this article is to review the ocular and periocular complications of laser surgery, with special attention to CO2 and erbium:YAG laser.
Although the description of the physical properties of lasers and their mechanism of action is beyond the scope of this review, a brief description of tissue interaction and ultrastructural changes due to laser may be helpful to understand some complications. As described by Thall, three basic laser-tissue interactions exist: photocoagulation, photodisruption, and photoablation.12 Each laser modality may achieve one or several of these effects. In photocoagulation, laser light is absorbed by the tissue, which generates heat that denatures proteins (coagulation). This effect is accomplished by argon laser and is mainly absorbed by vessels and melanin. Photodisruption is largely a mechanical effect; by producing a miniature lighting bolt, a tiny thunderclap is induced and mechanical shock waves cause most of the tissue damage. Due to this quality, YAG lasers, including neodymium (Nd), potassium titanyl phosphate (KTP), and holmium lasers, have been used to disrupt lachrymal bone in external or endoscopic dacryocystorhinostomy.3,13 In addition, they also may induce photocoagulation; therefore, both interstitial KTP and Nd:YAG laser have been employed to treat periocular hemangiomas.4,14 Photoablation is the most recent light-tissue interaction and probably one of the most exploited clinically (and economically). This effect is basically achieved due to a sudden rise in temperature in tissues, producing vaporization. The excimer lasers in refractive surgery and both CO2 and erbium:YAG laser used for cutaneous resurfacing provoke this result.
The CO2 and erbium laser tissue interaction deserves more attention. CO2 laser with a wavelength of 10,600 nm is strongly absorbed by water, which is the main component of soft tissues. The laser beam induces a sudden temperature rise in intracellular water far beyond the boiling point, inducing vaporization. However, a variable amount of heat is conducted to surrounding tissues, inducing coagulative necrosis and thermal damage known as “lateral thermal damage” (LTD). LTD is responsible for the majority of unwanted effects secondary to CO2 laser. However, is also responsible for desirable effects such as thermal collagen contraction and dermal damage with collagen remodeling. To minimize LTD, the principle of selective photothermolysis must be considered. This principle states that LTD is minimized if the laser pulse duration is less than the time needed for the tissue to irradiate and diminish its temperature to one half (thermal relaxation time).6 The pulsed CO2 laser, in the form of superpulsed and ultrapulsed devices, or those continuous mode systems with flash scanning devices are able to deliver short-duration pulses (shorter than the thermal relaxation time of soft tissues) at high irradiance, achieving a more precise ablation of tissue with less depth of burn.15 In laser resurfacing, the desired effects are ablation of epidermis, heat-induced collagen shrinkage, and disruption of papillary dermis to induce collagen repair and re-epithelization from the hair follicles. In blepharoplasty, the cutting and coagulation effect is preferred.
The erbium:YAG laser, with a wavelength of 2940 nm, is more efficiently absorbed by water and collagen than the CO2 laser, inducing less thermal damage. However, due to less induction of heat, erbium:YAG lacks hemostatic effects and induces less collagen shrinkage.16
Histologically the more evident effect of CO2 laser is an area of coagulative necrosis surrounding or underlying the area of tissue vaporization.17 In a research study performed by one of the authors, the area of coagulative necrosis produced by continuous mode measured in eyelid histological samples was not significant greater than that produced by the ultrapulsed mode.18
Prolonged erythema, hyper- and hypopigmentation, and hypertrophic or keloidlike scarring are among the most common complications following skin-resurfacing procedures. Although several factors may influence the healing process after laser surgery, excessive inflammation due to an intense laser-induced thermal damage is probably the major etiologic factor. Excessive LTD may induce persistent vasodilation, profuse transfer of melanin from the hair follicle melanocytes to the regenerated epithelial cells, and abundant deposition of new collagen leading to hypertrophic or keloid scar formation.
Erythema is the clinical manifestation of vasodilation in the underlying dermis. Noticeable erythema normally follows laser resurfacing and persists for 6 to 12 weeks with CO2 laser, and 4.24 ± 1.5 weeks with erbium:YAG according to Bass.9 Other authors reported an average erythema duration of 4.5 months after CO2 resurfacing.19 In the late 1990s, a laser resurfacing and laser blepharoplasty survey was carried out among members of the American Society for Aesthetic Plastic Surgery (ASAPS) and the American Society of Plastic and Reconstructive Surgery (ASPRS). A summary of the Laser Task Force Survey published by Apfelberg stated that prolonged erythema, defined as longer than 10 weeks, was the most common side effect of CO2 laser resurfacing, after persistent rhytids or dissatisfaction with the initial result, and was present in 8.8% of cases. Moreover, excessive erythema (Fig. 1) occurred in 5.8% of cases.20 Although several factors including contact or irritant dermatitis, atopy, and superficial infections (either fungal, bacterial, or viral) may lead to prolonged erythema, excess thermal damage and depth of tissue ablation are probably the most common causes of this complication.19,21 In addition, prolonged erythema is a risk factor for excessive or hypertrophic scarring and atrophic textural changes. Potent topical steroid therapy is usually recommended to treat this problem; however, due to the risk of atrophic changes or telangiectasias development; they should be used for a brief period of time. Alster et al suggested that the application of topical vitamin C in an aqueous formulation may decrease the degree and duration of erythema after cutaneous CO2 laser resurfacing,22 whereas Fulton recommended occlusive dressing to minimize this secondary effect.23
Figure 1.
Prolonged and excessive upper and midface erythema involving the periocular region after combined CO2-erbium full-face resurfacing. Complete resolution was attained with the use of a short course of topical steroids.
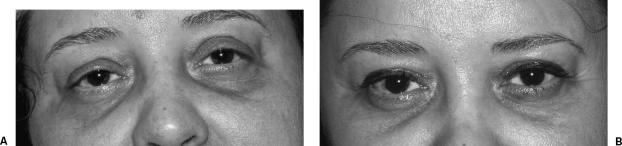
Hyper- and hypopigmentation may follow periocular laser surgery. Hyperpigmentation (Fig. 2A) is most commonly seen in darker skin types (Fitzpatrick III to VI types) and in those patients with history of postinflammatory pigment alterations.21,24 Pretreatment with bleaching agents preoperatively 2 to 8 weeks once or twice daily is recommended, particularly in those patients. More common bleaching agents include topical hydroquinone 2 to 4% or kojic acid 2% (Fig. 2B).24 The concomitant use of tretinoin and α-hydroxy acids may facilitate penetration of these compounds, further stimulate collagen regeneration, and possibly enhance the healing process. Moreover, the use of broad-spectrum sunscreen pre- and postoperatively will block ultraviolet stimulation of melanogenesis.19,21 Conversely, hypopigmentation (Fig. 3) may represent a restoration of the skin to its original pigmentation, a true loss of melanocytes due to a deep thermal damage, or, more rarely, an unmasking of vitiligo (Koebner phenomenon).21 Laws et al have reported a case of “alabaster skin” after CO2 laser resurfacing where the histological study disclosed a subepithelial fibrosis and a decrease in the amount of epidermal melanin. These authors suggested that previous cutaneous procedures such as dermabrasion or topical 5-fluorouracil may increase the risk of postlaser hypopigmentation.25 Hypopigmentation is usually a late effect, and unfortunately, almost the only good treatment is camouflage with makeup. The ASPS/ASPRS Laser Task Force Survey disclosed a rate of 6.5% of patients who develop hyperpigmentation after laser resurfacing, whereas hypopigmentation was present in only 3.2% of patients.20 Other studies disclosed a 5% rate of hyperpigmentation in the periorbital region.19
Figure 2.
(A) Hyperpigmentation affecting mainly the lower eyelids after full-face CO2-erbium resurfacing and bilateral upper lid blepharoplasty. (B) The same patient in the late postoperative phase with significant pigment reduction after the use of topical kojic acid 2%.
Figure 3.
(A) Upper eyelid bilateral xanthelasma in a heavily pigmented patient. (B) Same patient after CO2 resurfacing of the lesions displaying a moderate hypopigmentation in the treated area.
Infectious complications are most feared in the early postoperative period after periocular laser treatments due to their potential morbidity to this region and the annoyance that they carry for the patient. Bacterial, viral, and fungal infections may follow periocular laser surgery, particularly after laser resurfacing. The ASPS/ASPRS Laser Task Force Survey reported a 6.5% incidence of bacterial infections after laser resurfacing and 1.7% of herpes and other viral infections.20
Primary herpes simplex virus (HSV) outbreak, in patients without a history of such viral infection, or recurrence of HSV may complicate the healing process after laser resurfacing. Nanni and Alster reported a 7.4% incidence of HSV infection in a series of 500 cases treated with CO2 laser resurfacing, 50% with previous history and 50% without.26 Herpetic lesions may appear as a cluster of small, raw, red lesions if they occur before complete epithelial regeneration and may evolve to typical lesions if early treatment is not established.24 A herpes outbreak after laser resurfacing not only complicates the postoperative management but also may lead to undesirable scarring in the region. Oral prophylaxis with acyclovir 400 mg four times a day, valacyclovir 500 mg twice a day, or famciclovir is generally use prophylactically starting 1 day before the procedure and increased to full dose (acyclovir 800 mg, five times per day, or equivalent) if an herpetic infection develops. Other uncommon viral infections include herpes zoster, verrucae, or molluscum contagiosum.24
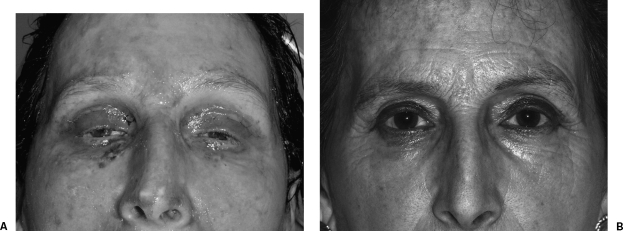
The most common bacterial skin infection is impetiginization (Fig. 4), usually manifested as painless honeylike skin crusting, due to gram-positive cocci (Staphylococcus pyogenes, or less frequently Staphylococcus aureus or epidermidis); however, more severe infectious complications may follow laser resurfacing. Pseudomonas and other gram-negative infections may induce fever, increased tenderness, and/or redness of the treated area and may lead to more severe local and even systemic disease.24 Jordan et al reported a case of necrotizing fasciitis after four-lid laser blepharoplasty and forehead resurfacing.27 Systemic involvement of localized infection after laser periocular surgery is rare, but at least two cases of toxic shock syndrome after resurfacing have been communicated.21 Oral prophylactic antibiotic therapy is recommended by the majority of laser surgeons, and cephalosporins, macrolides, or quinolones are usually initiated the same day of surgery. The use of topical antibiotic ointment is discouraged due to the extremely high risk of contact dermatitis when they are applied to raw resurfaced areas. Interestingly, occlusive dressing after resurfacing has been pointed out as a risk factor for postlaser bacterial or fungal infection.26
Figure 4.
(A) Impetiginization affecting lower lid, frontal, cheek, and nasal region after full-face resurfacing and bilateral upper lid blepharoplasty. (B) Resolution of the cutaneous infection with a mild residual periocular hyperpigmentation mainly affecting the right eye.
Superficial yeast infection may arise, especially in women with a past history of vaginal candida infection.21 The superficial moist and de-epithelialized skin surface may be prone to colonization prior to re-epithelization. The clinical manifestation may be quite variable including erythematous areas, whitish plaques, pustules, and milia-like lesions.24 The diagnosis may be confirmed by Gram stain, potassium hydroxide (KOH) preparation, or culture of the exudates found on the skin. Oral fluconazole or ketoconazole may be use prophylactically and postoperatively if symptoms are suggestive of such complication.26 Topical soaks with dilute vinegar solution help to create a local environment undesirable to the fungus.
Hypertrophic scarring is a potentially disastrous consequence of laser resurfacing, an elective aesthetic procedure, and has been reported to occur in 0.9% of patients.20 Excessive thermal damage due to poor technique (inappropriate number of passes, excessive overlap between pulses, or great depth of vaporization/ablation), infection, poor wound care, or patient-related factors, particularly keloid tendency, are among the most common etiologic factors.21 The periorbital region, particularly the medial lower lid, is a high-risk zone to develop hypertrophic scars after laser resurfacing.24,26 An adequate number of passes with the appropriate laser parameters and good wound care, avoiding irritating, picking, or use of unsuitable topical agents at the treated area, are the best guidelines to prevent posttreatment scar problems.21,26 Postlaser scarring should be treated as soon as is detected. Topical steroids and/or intralesional depot steroids (triamcinolone), alone or in combination with silicone gel or sheeting, are the best treatment modalities for this complication.21,28 The addition of dye laser treatment has also shown to be beneficial.29
Severe burns have not been commonly described; however, Grossman et al in a series of 20 consecutive patients seen in a 17-month period referred two cases of full-thickness burns (one affecting the full face) and two cases of microstomia secondary to contracture from perioral scarring after CO2 laser resurfacing. In the same series they found several thermal injuries in the periocular area including four cases of hypertrophic scarring, three cases of atrophic skin changes in the medial lower lid, one case of prolonged erythema, and one case of lower lid hypopigmentation.28
Temporary ectropion after laser lower lid blepharoplasty has been reported in 6% of patients and permanent ectropion in 0.4% and 0.1% after lower lid resurfacing and lower lid blepharoplasty, respectively.20 Risk factors include prior or simultaneous lower lid blepharoplasty or face-lift and lateral canthal tendon laxity.19,26 An adequate evaluation of the lateral canthal tendon tension and a conservative treatment of the lower lid are recommended to avoid postlaser lower lid ectropion that usually must be corrected surgically.19
There is no published report of intraocular or corneal injury after laser resurfacing; however, the ASAPS/ASPRS Laser Task Force Survey Summary disclosed a 0.3% rate of corneal injury after lower lid laser blepharoplasty.20 Cases of ocular perforation in laser blepharoplasty have also been anecdotally reported according with Goldbaum and Woog.6 The use of adequate nonreflecting eye protective shields is mandatory to prevent this hazard.
After an extensive experience with both CO2 and erbium laser or a combination of these two modalities, and despite the clinical improvement achieved, most of the enthusiasm for these treatments has been tempered by the long recovery time associated with a prolonged downtime and the unwanted secondary effects or even complications described. A shift toward laser modalities with faster recovery time and less potential complications has been experienced in the last decade. The majority of the unwanted effects described herein have been related to the ablation of the epidermis and the subsequent healing process; however, some of the beneficial effects of laser surgery do not necessarily need a previous epidermal ablation. Hence if a process of collagen remodeling and shrinkage is achieved without epidermal disruption, a theoretical cosmetic improvement of the photoaged dermis would be attained. Following this hypothesis, a new area of laser technology has been developed: so-called nonablative resurfacing or subsurface remodeling.30 Different nonablative laser modalities are available nowadays; however, despite the fact that some of them still lack an adequate follow-up, it seems that their clinical results are usually not quite as good as the more aggressive ablative techniques.31,32
In conclusion, periocular laser surgery using mainly CO2 and erbium:YAG laser is a well-established treatment modality suitable for a safe performance of lower lid blepharoplasty surgery and periocular resurfacing with rejuvenation purposes. However, potential severe complications in the periocular area may follow these aesthetic procedures. An appropriate selection of patients, adequate preoperative and prophylactic treatment, proper training and familiarity of the surgeon with the technique, and cautious, conservative approach are strongly recommended to minimize hazardous outcomes after periocular ablative laser surgery. New nonablative laser technology has been extensively developed and may represent in the future an effective and safer option for periocular laser rejuvenation.
REFERENCES
- Gonnering R S. In: Stewart WB, editor. Surgery of the Eyelid, Orbit, and Lacrimal Surgery. Vol 1. San Francisco, CA: American Academy of Ophthalmology; 1993. Physical modalities and their applications. pp. 79–81.
- Wohlrab T M, Rohrbach J M, Erb C, Schlote T, Knorr M, Thiel H J. Argon laser therapy of benign tumors of the eyelid. Am J Ophthalmol. 1998;125:693–697. doi: 10.1016/s0002-9394(98)00004-x. [DOI] [PubMed] [Google Scholar]
- Hehar S S, Jones N S, Saquid S A, Downes R N. Endoscopic holmium:YAG laser dacryocystorhinostomy-safe and effective as a day-case procedure. J Laryngol Otol. 1997;111:1056–1059. doi: 10.1017/s0022215100139325. [DOI] [PubMed] [Google Scholar]
- Clymer M A, Fortune D S, Reinisch L, Toriumi D M, Werkhaven J A, Ries W R. Interstitial Nd:YAG photocoagulation for vascular malformations and hemangiomas in childhood. Arch Otolaryngol Head Neck Surg. 1998;124:431–436. doi: 10.1001/archotol.124.4.431. [DOI] [PubMed] [Google Scholar]
- Meltzer M A. In: Smith BC, editor. Ophthalmic Plastic and Reconstructive Surgery. St. Louis, MO: Mosby; 1987. Uses of the carbon dioxide laser in ophthalmic plastic surgery. pp. 1178–1182.
- Goldbaum A M, Woog J J. The CO2 laser in oculoplastic surgery. Surv Ophthalmol. 1997;42:255–267. doi: 10.1016/s0039-6257(97)00097-0. [DOI] [PubMed] [Google Scholar]
- Apfelberg D B. The ultrapulse carbon dioxide laser with the computer pattern generator automatic scanner for facial cosmetic surgery and resurfacing. Ann Plast Surg. 1996;36:522–529. doi: 10.1097/00000637-199605000-00015. [DOI] [PubMed] [Google Scholar]
- Fitzpatrick R E, Goldman M P, Satur N M, Tope W D. Pulsed carbon dioxide laser resurfacing of photoaged facial skin. Arch Dermatol. 1996;132:395–402. [PubMed] [Google Scholar]
- Bass L S. Erbium:YAG laser skin resurfacing: preliminary clinical evaluation. Ann Plast Surg. 1998;40:328–334. doi: 10.1097/00000637-199804000-00002. [DOI] [PubMed] [Google Scholar]
- Goldberg R A. The carbon dioxide laser in oculoplastic surgery and sliced bread. Arch Ophthalmol. 1996;114:1131–1133. doi: 10.1001/archopht.1996.01100140333015. [DOI] [PubMed] [Google Scholar]
- Blanco G, Soparkar C N, Jordan D R, Patrinely J R. The ocular complications of periocular laser surgery. Curr Opin Ophthalmol. 1999;10:264–269. doi: 10.1097/00055735-199908000-00008. [DOI] [PubMed] [Google Scholar]
- Thall E H. In: Yanoff M, Duker JS, editor. Ophthalmology. London, UK: Mosby; 1999. Principles of lasers. pp. 2.5.1–2.5.6.
- Rosen N, Barak A, Rosner M. Transcanalicular laser-assisted dacryocystorhinostomy. Ophthalmic Surg Lasers. 1997;28:723–726. [PubMed] [Google Scholar]
- Achauer B M, Chang C J, VanderKam V M, Boyko A. Intralesional photocoagulation of periorbital hemangiomas. Plast Reconstr Surg. 1999;103:11–16. doi: 10.1097/00006534-199901000-00003. [DOI] [PubMed] [Google Scholar]
- Grossman A R, Majidian A M, Grossman P H. Thermal injuries as a result of CO2 laser resurfacing. Plast Reconstr Surg. 1998;102:1247–1252. doi: 10.1097/00006534-199809040-00054. [DOI] [PubMed] [Google Scholar]
- Ziering C L. Cutaneous laser resurfacing with the erbium YAG laser and the char-free carbon dioxide laser. A clinical comparison of 100 patients. International Journal of Aesthetic and Restorative Surgery. 1997;5:29–37. [Google Scholar]
- Collawn S S, Boissy R E, Vasconez L O. Skin ultrastructure after CO2 laser resurfacing. Plast Reconstr Surg. 1998;102:509–515. doi: 10.1097/00006534-199808000-00036. [DOI] [PubMed] [Google Scholar]
- Blanco G, Tucker N A, Arthus B, Peruzhar B, Burnier M N., Jr Tissue damage in CO2 laser blepharoplasty: comparison between ultrapulse vs. continuous wave modes. Invest Ophthalmol Vis Sci. 1998;39(suppl):1013. [Google Scholar]
- Nanni C A, Alster T S. Complications of cutaneous laser surgery. A review. Dermatol Surg. 1998;24:209–219. doi: 10.1111/j.1524-4725.1998.tb04139.x. [DOI] [PubMed] [Google Scholar]
- Apfelberg D B. Summary of the 1997 ASAPS/ASPRS Laser Task Force Survey on Laser Resurfacing and Laser Blepharoplasty. Plast Reconstr Surg. 1998;101:511–518. doi: 10.1097/00006534-199802000-00043. [DOI] [PubMed] [Google Scholar]
- Linsmeier-Kilmer S. Laser resurfacing complications. How to treat them and how to avoid them. International Journal of Aesthetic and Restorative Surgery. 1997;5:41–45. [Google Scholar]
- Alster T S, West T B. Effect of topical vitamin c on postoperative carbon dioxide laser resurfacing erythema. Dermatol Surg. 1998;24:331–334. doi: 10.1111/j.1524-4725.1998.tb04163.x. [DOI] [PubMed] [Google Scholar]
- Fulton J E. Complications of laser resurfacing. methods of prevention and management. Dermatol Surg. 1998;24:91–99. [PubMed] [Google Scholar]
- Khan J A. Millisecond CO2 laser skin resurfacing. Int Ophthalmol Clin. 1997;37:29–67. doi: 10.1097/00004397-199703730-00005. [DOI] [PubMed] [Google Scholar]
- Laws R A, Finley E M, McCollough M L, Grabski W J. Alabaster skin after carbon dioxide laser resurfacing with histologic correlation. Dermatol Surg. 1998;24:633–636. doi: 10.1111/j.1524-4725.1998.tb04220.x. [DOI] [PubMed] [Google Scholar]
- Nanni C A, Alster T S. Complications of carbon dioxide laser resurfacing. An evaluation of 500 patients. Dermatol Surg. 1998;24:315–320. doi: 10.1111/j.1524-4725.1998.tb04161.x. [DOI] [PubMed] [Google Scholar]
- Jordan D R, Mawn L, Marshall D H. Necrotizing fasciitis caused by group A streptococcus infection after laser blepharoplasty. Am J Ophthalmol. 1998;125:265–266. doi: 10.1016/s0002-9394(99)80108-1. [DOI] [PubMed] [Google Scholar]
- Grossman A R, Majidian A M, Grossman P H. Thermal injuries as a result of CO2 laser resurfacing. Plast Reconstr Surg. 1998;102:1247–1252. doi: 10.1097/00006534-199809040-00054. [DOI] [PubMed] [Google Scholar]
- Weinstein C, Ramirez O, Pozner J. Postoperative care following carbon dioxide laser resurfacing. Avoiding pitfalls. Dermatol Surg. 1998;24:51–56. doi: 10.1111/j.1524-4725.1998.tb04051.x. [DOI] [PubMed] [Google Scholar]
- Goldberg D J. Nonablative resurfacing. Clin Plast Surg. 2000;27:287–292. [PubMed] [Google Scholar]
- Shook B A, Hruza G J. Periorbital ablative and nonablative resurfacing. Facial Plast Surg Clin North Am. 2005;13:571–582. doi: 10.1016/j.fsc.2005.06.007. [DOI] [PubMed] [Google Scholar]
- Goldberg D J. Lasers for facial rejuvenation. Am J Clin Dermatol. 2003;4:225–234. doi: 10.2165/00128071-200304040-00002. [DOI] [PubMed] [Google Scholar]