ABSTRACT
Facial aesthetic surgeons are sometimes challenged by the predicament of diagnosing and managing patients with chronic eyelid edema. Herein we provide a brief review of some of the more common causes of pre- and postoperative eyelid edema, many of which have important systemic implications, and offer management suggestions.
Keywords: Periorbital, eyelid, edema
Chronic eyelid swelling is often the herald of significant systemic or periorbital disease, and for the facial aesthetic surgeon, patients with eyelid edema can pose a particularly difficult problem. First, the cosmetic surgeon is frequently the first physician to be confronted by someone with rapid changes in the eyelids, as patients often believe such changes are somehow the result of “sudden” aging. Second, over the years, many faces develop a full appearance around the eyes due to the very thin, redundant eyelid skin as well as attenuation of the orbital septum with resultant pseudoherniation of the orbital fat. This frequent eyelid appearance, unfortunately, is closely mimicked by some common forms of eyelid and orbital swelling (Fig. 1). Finally, most commonly, periocular edema unrecognized and uncontrolled preoperatively is likely to be exacerbated by surgery and then viewed as a postoperative complication. This situation is especially problematic if the swelling spreads to the conjunctiva, producing prolonged chemosis with attendant ocular irritation from dell formation (corneal desiccation, thinning, and ulceration) and significant visual disturbance, turning an aesthetic disaster into a functional one as well.
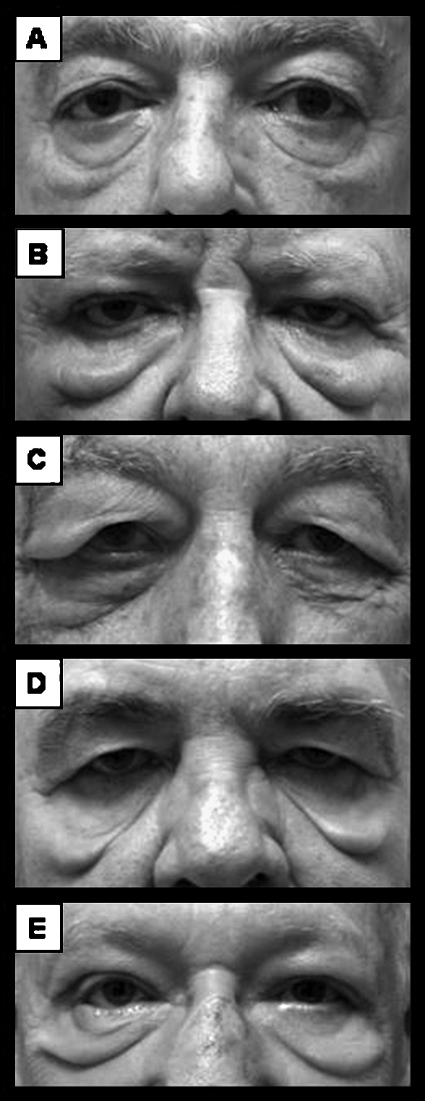
Figure 1.
(A) Normal periocular aging changes. (B) Eyelid edema from chronic renal failure following three attempts at lower eyelid blepharoplasty and correction of lower eyelid retraction before referral. (C–E) Chronic eyelid edema secondary to systemic medical disease.
Eyelid edema, generally speaking, is a nonspecific sign with etiologies spanning the fields of immunology, dermatology, endocrinology, cardiology, gastroenterology, infectious disease, neurology, otolaryngology, and ophthalmology, and a comprehensive diagnostic algorithm encompassing all these causes is well beyond the space limitations of this article. However, luckily, there are some easily recognized causes common to developed countries. Thus, we present a simplified framework for the diagnosis and management of many of the more frequently encountered and more easily recognized forms of preoperative and postoperative eyelid edema seen in the United States, primarily emphasizing those forms that involve both eyes and are generally chronic in duration, lasting weeks to months and beyond.
RECOGNIZING EYELID EDEMA
The first challenge is to recognize periocular inflammation and edema. Obvious cases have erythematous skin, conjunctival swelling (chemosis), or frankly translucent eyelid skin (Fig. 2A). More subtle clues, however, might include a history of relatively rapid “aging” of the eyelids over weeks or months. Physician beware! An alteration in eyelid appearance that has not slowly progressed over years demands careful scrutiny and evaluation. Daily or frequent use of ophthalmic decongestants (over-the-counter drops intended to “get the red out”) may conceal overt signs of localized swelling, and the ocular surface vascular hyperemia targeted by these drops may be the herald of chronic, local inflammation. “Bags” or “dark circles” under the eyes that are much, much worse in the morning after prolonged reclined posture or following considerable salt consumption the night before indicate increased periocular blood flow and vascular permeability, both signs of inflammation. A “glassy” or “watery” appearance of the eyes is often due to subtle chemosis, which is unlikely to have developed in isolation. Downward turned eyelashes in the upper eyelid may be an indication of chronic eyelid inflammation with tarsal weakening, as commonly occurs in several disorders including floppy eyelid syndrome and sleep apnea (Fig. 2B). Finally, pay careful attention to the eyelid rhytids. Vertically oriented rhytids in the eyelids are never due to relaxed skin tension lines. Instead, these most commonly reflect atopic dermatitis or systemic allergy (Figs. 2C,D). Although a less specific sign, a profound relative lack of rhytids in the eyelids compared with the rest of the face may indicate eyelid swelling.
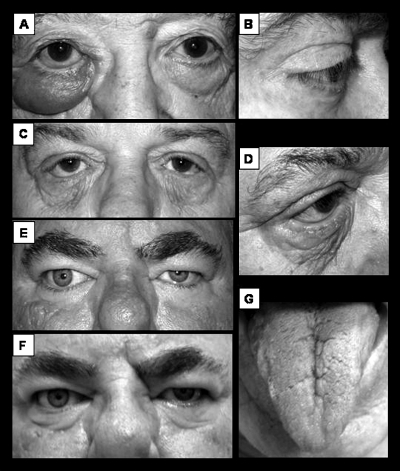
Figure 2.
(A) Unilateral eyelid swelling with erythematous and translucent skin as well as conjunctival swelling (chemosis). (B) Eyelash ptosis of floppy eyelid syndrome with subtle preseptal eyelid edema in both upper and lower eyelids. (C, D) Atopic dermatitis with eyelid skin erythema, thickening, and lost elasticity leading to eyelid retraction. Note the characteristic vertically oriented rhytids. (E) Rosacea-associated posterior lid margin disease blepharitis with mild chemosis and attendant eyelid edema. Flash photography demonstrates a light reflex from chemosis at the eyelid margin in the left eye. (F) Nonflash photograph of same patient in (E) showing shadowing from the lower eyelid edema. (G) Deeply fissured tongue seen in Melkersson Rosenthal syndrome.
EYELID EDEMA IN THE PREOPERATIVE SETTING
In this section, we present forms of eyelid edema that may be easily recognized in the preoperative setting.
Medications
Many medications—topical, oral, and parenteral—are well recognized to create eyelid swelling through generalized fluid retention, angioedema, urticaria, or topical blepharoconjunctivitis. A list of the more common offenders may be found in Table 1, but some deserve special mention, including corticosteroids, acetaminophen, aspirin, other frequently used prescription and nonprescription nonsteroidal anti-inflammatory medications, and hormonal supplements. Many of these are almost ubiquitously used, whereas others may be employed specifically to alleviate periocular inflammation from another cause, only to compound and further confuse the problem. In suspected cases, a 2-week moratorium on all medications should be attempted, if medically possible. Potential offenders should then be added back one at a time. Mild engorgement of other mucous membranes (including genitalia) suggests angioedema, whereas greater involvement of the lower eyelid or erythema streaking down the cheek below the eye is more suggestive of topical blepharoconjunctivitis from eyedrops.
Table 1.
Medications Known to Cause Eyelid Edema
| Acetaminophen* |
| Acetylcholinesterase inhibitors*,† |
| Acylovir* |
| Albuterol* |
| Aldosterone* |
| Alprazolam* |
| Amiodarone* |
| Ampicillin* |
| Amide and ester anesthetics‡ |
| Aproclonidine‡ |
| Aspirin*,† |
| Atropine‡ |
| Bacitracin* |
| Bleomycin* |
| Brimonidine‡ |
| Busulfan* |
| Butabarbital* |
| Carbamazepine* |
| Carbimazole* |
| Cephalosporins* |
| Contact lens solutions (especially those containing the preservative benzalkonium chloride)‡ |
| Dexamethasone* |
| Digitalis* |
| Dorzolamide‡ |
| Erythromycin* |
| Estrogens† |
| Fluoroquinolones* |
| Hydrocortisone* |
| Ibuprofen*,† |
| Indomethacin*,† |
| Insulin* |
| Iodine‡ |
| Penicillin‡,* |
| Phenylbutazone*,† |
| Pilocarpine‡ |
| Prednisone* |
| Progesterone† |
| Quinidine,* quinine* |
| Ranitidine (and other H2 receptor blockers)* |
| Rifampin* |
| Sulindac*,† |
| Sympatholytics*,† |
| Temazepam* |
| Tetracyclines* |
| Thiabendazole* |
| Triamcinolone* |
| Triazolam* |
| Vaccinations (including diphtheria, tetanus, pertussis vaccine, measles, mumps, rubella vaccine, poliovirus vaccine, rubella vaccine, rabies vaccine, rabies immune globulin, tetanus toxoid, and tetanus immune globulin),* vancomycin* |
| Vasodilators*,† |
| Verapamil* |
Known to cause urticaria/angioedema with eyelid swelling.
Known to cause eyelid swelling due to generalized fluid retention.
Known to cause allergic contact blepharoconjunctivitis with eyelid swelling.
Allergies
Allergic conditions affecting the periocular area include seasonal and perennial allergies as well as vernal keratoconjunctivitis, atopy or contact dermatitis, and drug-induced allergic blepharoconjunctivitis (discussed above). All are hypersensitivity reactions that can result in puffy swollen eyelids, chemosis, ocular surface hyperemia (injection), tearing, and a scaly eczematous rash in the pattern of exposure. The classical signs of allergic reaction, itching and vertical eyelid rhytids, are diagnostic if present but may also be absent (Figs. 2C, D).
Environmental allergies, including vernal keratoconjunctivitis, are usually easily identified through history and other systemic manifestations, such as rhinorrhea, sneezing, postnasal drip, and so on. Atopic contact dermatitis, a type IV hypersensitivity reaction, requires previous sensitization to the offending allergen, which can be cosmetics, eyedrops, or occupational allergens. Most common offending cosmetics include hair dyes (paraphenylenediamine, synthetic fragrances, acrylics, parabens, resorcinol, ammonia, and henna), nail polishes (toluene sulfonamide, sulfonamide-formaldehyde, and quaternium-15), nail enhancements (methacrylates), sunscreens (para-aminobenzoic acid, cinnamates, benzophenones, salicylates, and anthranilates), mascaras (shellac), and eye shadows (numerous allergenic metals).1,2,3,4 Eyedrops, contact lens solution, and ophthalmic ointments may also contain allergenic preservatives such as brimonidine tartrate and benzalkonium chloride.
Urticarial, immunoglobulin E–mediated reactions typically produce hives and an apparent thickening of the skin through swelling of the papillary dermis. Although this reaction is typically thought of as acute and fulminate, repeated chronic, low-grade allergen exposure may lead to prolonged skin thickening, especially in areas of trauma and in the very thin skin of the eyelid. Such triggers commonly include foods (egg, milk, peanut, soy, wheat, additives, and preservatives) and insect bites (ants are the insect most responsible for repeated exposures over time). Importantly, paraneoplastic syndromes and autoimmune diseases (systemic lupus erythematosis, cryoglobulinemia, paraproteinemia, etc.) can also cause urticaria. Physical urticaria can be caused by pressure (swimming goggles) and heat (daily warm compresses for ocular meibomitis treatment).1 Angioedema, an urticaria-like allergic condition involving deep dermis and subcuticular tissue and in some cases the mucosa of the respiratory and digestive tracts, is even more likely to present acutely. However, episodic, recurrent forms (discussed below) exist, and the resultant damage over time to the eyelids may be misinterpreted as simple dermatochalasis.
The treatment of allergic conditions rests primarily on separating the patient from allergen contact, if possible. A meticulous patient diary and allergists can be very helpful in identifying the offending trigger.
Ocular Rosacea
Acne rosacea and close relative, sebaceous hyperplasia, are common, chronic dermatoses affecting individuals of all ages, although the onset of symptoms is usually between the ages of 30 and 60 years with the severity of the disorder progressing over time and most commonly involving the cheeks, nose, forehead, and chin.2 Although these disorders may be more frequent among those of Celtic ancestry, individuals of all races can be afflicted.
Rosacea is a chronic inflammatory disorder of debated etiology. H. pylori infection, S. epidermidis overcolonization, and vascular dilation and incompetence have all been hypothesized in isolation and in combination.3,4,5 Several rosacea subtypes are described, including erythematotelangiectatic, inflammatory papulopustular, phymatous, and ocular.6 Regardless of the nomenclature, all forms produce some degree of posterior eyelid margin blepharitis or meibomitis. The result is a thickening of the secretions of the meibomian glands that reside in the eyelid margins with decreased normal flow of oil into the tear film. This has multiple consequences. First, the meibomian glands become inflamed, compressing the emptying ductules, further decreasing flow from the glands and perpetuating the problem. Over years, chronic eyelid inflammation leads to scarring and permanent occlusion of the meibomian glands. When this happens, the oil component of the tear film essential for decreasing the rate of tear evaporation is then absent and the patient's eye dries. The chronic eyelid inflammation may also contribute significantly to decreasing the aqueous portion of the tear film as well. Thus, in addition to patients having poor-quality tear, there may be decreased tear volume as well. Dry eye is not only visually disabling, but it can also be extremely painful and threaten the very survival of the eye. Some patients may also go on to develop toxic tear syndrome, a problem where the thick, poorly diluted, partially oxidized lipids that actually do make it into the tear film are highly inflammatory and irritating to the eye. Paradoxically, this problem is often exacerbated by punctual occlusion, closing off of the tear drains, commonly performed for patients with dry eye, as the irritating lipids then are unable to drain away and merely further concentrate as the aqueous component of the tear film evaporates.
Early, the meibomitis may present as ocular dryness with a gritty or burning feeling, morning crusting, light sensitivity, periodic blurry or “smeary” vision, and even paradoxical reflex tearing. Ophthalmic symptoms, like the underlying disease, worsen with time. Erythema and thickening of the eyelid margin, conjunctival hyperemia and chemosis, and eyelid margin telangiectatic vessels are all visible with the naked eye (Figs. 2E,F). Slit-lamp examination is more sensitive and can be used to grade the severity of disease as well as treatment progress.
The treatment of rosacea, and the attendant ocular and cutaneous symptoms, is generally prolonged and can be quite complex, involving a myriad of hygiene techniques as well as carefully balanced topical and systemic therapies. Although the management is beyond the scope of this article and is probably best left to both dermatology and ophthalmology, patients recognized with this disorder preoperatively should be started on therapy, as eyelid surgery always worsens the ophthalmic disease.
Thyroid Eye Disease
Although thyroid eye disease (TED) is covered exhaustively elsewhere in this issue, this common problem deserves additional emphasis, not only because TED commonly causes eyelid, conjunctival, and orbital edema (Fig. 3A), nor because the stable, quiescent phase can mimic eyelid edema, nor because many patients who seek cosmetic eyelid surgery have previously undiagnosed TED and represent an opportunity for life-altering medical intervention (Fig. 3B), nor even because if the disease is active and unrecognized, surgery on a changing anatomic situation begs for unpredictable results. Perhaps the most important reason to always be suspicions of TED in eyelids that have rapidly changed appearance is that our primary dictum is to “first do no harm.” TED is an inflammatory disorder of autoimmune etiology. Trauma, or the iatrogenic trauma of regional surgery, during the active phase of TED is strongly believed by many to exacerbate the clinical course. Florid TED can be profoundly disfiguring, psychologically crippling, and even blinding, all terrible consequences of a missed diagnosis prior to cosmetic eyelid surgery.
Figure 3.
(A) Thyroid ophthalmopathy with three eyelid edema, chemosis, and upper eyelid retraction. (B) More subtle, previously undiagnosed thyroid ophthalmopathy and eyelid edema in a patient presenting for elective blepharoplasty. (C–E) Blepharochalasis syndrome with chronic eyelid changes of skin thinning narrowed horizontal fissures and loss of lateral canthal tendon fixation. (F) Chronic left upper eyelid edema and resultant blepharoptosis in a patient with previously undiagnosed inflammatory bowel disease-associated orbital inflammation. (G) Same patient as in (F) following blepharoplasty, blepharoptosis repair, and preseptal orbicularis myectomy.
Melkersson Rosenthal Syndrome
Melkersson Rosenthal (MR) syndrome is a relatively rare, gender-unbiased, noncaseating granulomatous condition, which may arise any time from adolescence through the ninth decade of life. The characteristic clinical triad of facial palsy, facial edema, and lingua plicata (“furrowed” or “scrotal” tongue) is unfortunately quite variable both in the full triumvirate expression and in the presentation of each.7
Perhaps the most constant feature is the facial palsy of MR syndrome, which by itself may be clinically indistinguishable from Bell's palsy. The neuropathy may be partial or complete and most often spontaneously fully recovers, although permanent residual weakness has been reported. The palsy is usually unilateral but can be bilateral. Recurrent episodes are common on either the ipsilateral or contralateral side.
The facial edema is classically perioral; however eyelid edema may also be present or be the sole representation of facial swelling. The eyelid edema is painless, nonpitting, and most frequently bilateral but may also be unilateral. The edema is initially intermittent but may progress to being constant. Either situation can cause eyelid tissue laxity with destruction of elastic fibers.
Lingua plicata (Fig. 2G), present in 40% of cases, is always congenital. The tongue appears slightly larger and red with definite, deep furrows and grooves on the surface but is otherwise a benign finding.
Due to a highly variable presentation and oligosymptomatic forms, the diagnosis of MR syndrome can be challenging. An autosomal-dominant pattern of inheritance has been proposed, but the incomplete expressivity generally makes tracing the disease through families difficult. Furthermore, the eyelid histopathology is characteristic but not necessarily specific. The tissue edema, noncaseating epithelioid granulomatous lymphangitis, multinucleated Langhans'-type giant cells, perivascular mononuclear inflammatory infiltrate, and eventual fibrosis can all be seen in the eyelid edema associated with Crohn's inflammatory bowel disease, sarcoidosis, spirochete infections, and even severe rosacea.8
Treatment of MR syndrome is aimed at symptomatic relief. Intralesional corticosteroids, tetracycline, methotrexate, and clofazimine have all been used to alleviate the facial swelling with variable and temporary results. Surgery with blepharoptosis repair, superior lateral canthal tightening, blepharoplasty, and partial myectomy (see below) probably remains the best option.
Floppy Eyelid Syndrome
Floppy eyelid syndrome, an acquired problem primarily affecting the upper eyelids, is characterized by floppy tarsi, easily everted eyelids, eyelash ptosis or frank marginal entropion, and chronic papillary conjunctivitis. In addition, there is often some degree of eyelid thickening and edema, S-shaped blepharoptosis, and meibomian gland dysfunction. The eyelid skin may be wrinkly and paper-thin from repeated inflammation. Patients may complain of severe ocular irritation upon awakening if they are belly sleepers and their eyelids flip inside out, allowing the bedding to rub against their eye during sleep. Floppy eyelid syndrome is typically described in middle-aged, obese men but may be seen in both sexes and across a wide range of ages. Associations have been made with sleep apnea, diabetes, hypertension, spontaneous optic disc edema, and sudden optic neuropathy and blindness. Surgical treatment is complex and generally is aimed at addressing the excess eyelid skin, blepharoptosis, eyelash ptosis or entropion, and overall horizontal eyelid laxity.
C1-Esterase Inhibitor Deficiency-Type Angioedema
Hereditary angioneurotic edema, a relatively rare condition, is a genetic deficiency of C1 esterase inhibitor (C1-INH) activity that manifests with recurrent bouts of inflammation that may be visibly isolated to the eyelids. Attacks, which involve circumscribed, nonpitting, subepithelial swelling lasting mere days, may start as early as early childhood and may worsen at puberty. There may be associated angioedema of the intestines, resulting in abdominal pain and diarrhea. Urinary retention and central nervous system involvement are often present. There are two variants. Type I, the more common form, is a true deficiency of C1-INH protein. Type II may have normal or increased levels of C1-INH, but the protein is dysfunctional. There are also two types of acquired C1-INH deficiency: type I, associated with lymphoproliferative disorders, and type II in which autoantibodies against C1-INH develop. This latter condition is associated with other autoimmune disorders such as systemic lupus erythematosis, rheumatoid arthritis, and Sjögren's syndrome. Diagnosis requires determination of C1-INH level, C4 level, and C1-INH activity.
Blepharochalasis
Blepharochalasis, thought by some to be an angioedema variant, is a relatively rare disorder, typically bilateral, slightly more common in women, and characterized by recurrent bouts of painless, nonpitting periorbital edema starting in adolescence but decreasing in frequency over time.9 Episodes may be provoked by physical or emotional stress. Rarely, the disorder may be unilateral or be associated with perioral swelling. Adult-onset variants also exist. Recurrent inflammatory bouts result in characteristic papery-thin atrophy of the upper eyelid skin, lateral canthal angle rounding due to tendon laxity, and levator dehiscence-type blepharoptosis. The weakened orbital septum often results in lacrimal gland prolapse and orbital fat pseudoherniation, which produce a bulging appearance (Figs. 3C–E). These eyelids are hypervascular and may develop hyperpigmentation. Histopathology typically reveals an atrophic dermis with perivascular inflammatory cellular infiltrates, decreased elastic and collagen fibers, and immunoglobulin A deposits in the dermis and the dermoepidermal junction.
The treatment of blepharochalasis is surgically complex, and inattention to all of the eyelid deformities will frequently lead to greater disfigurement and worse eyelid function. Surgery may also precipitate an inflammatory event with corticosteroids having a limited impact.
Whole Body Edema
Whole body edema may present first or most notably with eyelid swelling. Disorders such as cardiac disease, renal disease, hepatic disease, low protein states, lymphatic obstruction, and hypothyroidism should all be considered. The hallmark of whole body edema is eyelid swelling that worsens first thing in the morning after prolonged dependent posture with gradual improvement throughout the day. Importantly, because the eyelid swelling may be related to how one sleeps, dramatic asymmetry may confound the presentation. Right heart failure tends to cause more pitting edema, whereas hepatic disease may give more truncal swelling.
EYELID EDEMA IN THE POSTOPERATIVE SETTING
Persistent eyelid edema in the postoperative period may be conveniently divided into three types: (1) edema present preoperatively but undiagnosed; (2) preexisting conditions exacerbated by surgery and tipped over into eyelid edema; and (3) problems directly related to surgical intervention. The first type has been amply covered above but should always be suspected in the postoperative setting. The second type, perhaps the most common cause of prolonged postoperative eyelid and conjunctival edema, refers mostly to situations of meibomian gland dysfunction, as discussed above under rosacea, and management by eye care providers familiar with these problems is strongly suggested. Remember, though, that in pure tear film problems, there is adequate closure of the eyelids. The third group, pure iatrogenic causes of postoperative eyelid edema, is discussed below.
Cold Urticaria
Cold urticaria, a form of physical urticaria, may be primary (idiopathic) or secondary to underlying hematologic or infectious diseases, such as cryoglobulinemia, chronic lymphocytic leukemia, lymphosarcoma, syphilis, rubeola, varicella, hepatitis, infectious mononucleosis, and mycoplasma. Cold urticaria is characterized by the development of hives and angioedema that may be localized (appearing just as eyelid edema following postoperative cold compresses) or generalized and involve the respiratory tract (hoarseness, dyspnea, and wheezing), gastrointestinal tract (duodenal ulcers and abdominal pain), and the cardiovascular system (hypotension, tachycardia, and arrhythmias). Like someone with an allergic reaction to corticosteroids, patients with cold urticaria and persistent postoperative eyelid edema may be managed for prolonged periods with precisely the therapy that worsens their condition.10 In suspected cases, a cold stimulation test may be necessary to make the diagnosis, and terminating exposure to cold stimuli (including chilled intravenous therapy) is essential for resolution of the problem.
Lymphedema
Lymphedema, localized swelling from accumulation of extracellular fluid that normally drains via the lymphatic system, can be grossly disfiguring and extraordinarily difficult to manage. Lymphedema may affect not only the eyelid skin but also the posterior lamella, or the palpebral conjunctiva, and contiguous spread of fluid may lead to frank, persistent chemosis. Postoperative lymphedema generally results from disruption or destruction of the lymphatics. Eventually, if not managed, eyelid lymphedema may result in tissue fibrosis with permanent barriers created to impede the normal handling of extracellular fluid.
Periocular lymphedema is most common after a full-thickness, vertical laceration (or incision) along the lateral aspect of the eyelid or following upper and lower eyelid blepharoplasty where the incisions come within a millimeter or two of one another, or actually meet.11 Most commonly, lymphedema is transient and resolves spontaneously in weeks to months as new lymphatics develop. However, occasionally lymphedema may persist and require treatment. Some argue strongly for lymphatic massage, whereas others support injections and surgical intervention as detailed below.
Eyelid-Dependent Keratoconjunctivitis Sicca
Keratoconjunctivitis sicca, or dry eye, can be both extremely painful and sight-threatening. Thus, this cause of eyelid edema should not be missed. As the surface of the eye dries, the conjunctiva may paradoxically swell, and the chemosis can spill over into the palpebral conjunctiva, ultimately creating eyelid edema. As long as the eye continues to dry, the eyelids will remain swollen. If the first division of the trigeminal nerve is functioning, patients typically complain of ocular irritation, and this is an important clue to the cause in the absence of a slit-lamp examination. There are many causes of dry eye, of course, but we limit our discussion to those situations caused by postsurgical disturbances of eyelid function.
Global orbicularis muscle dysfunction may be related to local anesthetic myotoxicity, yet this does not frequently cause profound blink paralysis. On the other hand, damage to or removal of just a few millimeters of the pretarsal orbicularis, as commonly occurs in the hands of the unwary physician during transcutaneous lower eyelid blepharoplasty, can result in significant loss of eyelid blink function and dry eye. Correcting orbicularis dysfunction can be challenging, because the muscle can't be replaced and compensating measures must be undertaken, which may alter the appearance of the eye.
Shortages of the anterior (skin) or middle lamellae (retractors) of the eyelids most commonly result from overly aggressive surgery, although preexisting eyelid retraction left unaddressed can have a similar result. All of these problems are easily identified by trying to move the eyelid in the desired position (i.e., trying to move a retracted lower eyelid upward) with a finger and feeling a tethered, tight, or overly heavy reluctance to movement. The ultimate solution here is to replace lost tissue, either through regional recruitment with solid fixation or free grafting.
In short, anything that decreases the ability of the eyelids to blink closed in a frequent and complete fashion will diminish ocular lubrication. One commonly overlooked eyelid problem after surgery is lateral canthal rounding or downward displacement, both of which may lead to regional ocular surface drying but without the patient's awareness of ocular irritation, because the highly sensate cornea is still well protected.
MANAGING EYELID EDEMA
The first step to managing chronic eyelid edema is recognizing the problem and if possible, the etiology. Although preoperative disorders should be resolved prior to operating on eyelids, surgery can also be curative. In experienced hands, a complete preseptal myectomy that carefully preserves the pretarsal and orbital portions of the muscle removes the lymphatics and obliterates the potential space where fluid accumulates (Figs. 3F, G). Corticosteroids may be useful in treating posterior eyelid margin blepharitis, but most other causes of eyelid edema do not have a persistent inflammatory source and are thus not ameliorated by this approach. Similarly, oral antibiotic use in a situation that is not clearly infected is helpful only for suspected mycobacterium infiltration and is overly aggressive treatment for posterior eyelid margin blepharitis. Diuretics may prove beneficial but should only be used if the underlying cause is known and being addressed. For lymphedema, lymphatic massage by a legitimate expert can be helpful, as can hyaluronidase injections, but these are short-term solutions while waiting for new lymphatic vessel growth.
SUMMARY
Patients with eyelid edema frequently present first to their aesthetic surgeon with a problem that is sometimes difficult to recognize as aging eyelids may look quite similar. Missing the diagnosis preoperatively, however, can lead to postoperative disasters. Herein, we have presented some common and more easily recognized causes of eyelid edema, emphasizing diagnosis and management.
REFERENCES
- Greaves M W, Salvoe R A. ABC of allergies: allergy and the skin. I–Urticaria. BMJ. 1998;316:1147–1150. doi: 10.1136/bmj.316.7138.1147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stone D U, Chodosh J. Ocular rosacea: an update on pathogenesis and therapy. Curr Opin Ophthalmol. 2004;15:499–502. [PubMed] [Google Scholar]
- Diaz C, O'Callaghan C J, Khan A, Ilchyshyn A. Rosacea: a cutaneous marker of Helicobacter pylori infection? Acta Derm Venereol. 2003;83:282–286. doi: 10.1080/00015550310016544. [DOI] [PubMed] [Google Scholar]
- Millikan L E. Rosacea as an inflammatory disorder: a unifying theory? Cutis. 2004;73(suppl 1):5–8. [PubMed] [Google Scholar]
- Dahl M V, Ross A J, Schlievert P M. Temperature regulates bacterial protein production: possible role in rosacea. J Am Acad Dermatol. 2004;50:266–272. doi: 10.1016/j.jaad.2003.05.005. [DOI] [PubMed] [Google Scholar]
- Dahl M V. Rosacea subtypes: a treatment algorithm. Cutis. 2004;74(3 Suppl):21–27. 32–34. [PubMed] [Google Scholar]
- Cockerham K P, Hidayat A A, Cockerham G C, et al. Melkersson-Rosenthal syndrome: new clinicopathologic findings in 4 cases. Arch Ophthalmol. 2000;118:227–232. doi: 10.1001/archopht.118.2.227. [DOI] [PubMed] [Google Scholar]
- Shapiro M, Peters S, Spinelli H M. Melkersson-Rosenthal syndrome in the periocular area: a review of the literature and case report. Ann Plast Surg. 2003;50:644–648. doi: 10.1097/01.SAP.0000069068.03742.48. [DOI] [PubMed] [Google Scholar]
- Dozsa A, Karolyi Z S, Degrell P. Bilateral blepharochalasis. J Eur Acad Dermatol Venereol. 2005;19:725–728. doi: 10.1111/j.1468-3083.2005.01252.x. [DOI] [PubMed] [Google Scholar]
- Burroughs J R, Patrinely J R, Nugent J S, et al. Cold urticaria: an under recognized cause of postsurgical periorbital swelling. Ophthal Plast Reconstr Surg. 2005;21:327–330. doi: 10.1097/01.iop.0000176272.40058.4f. [DOI] [PubMed] [Google Scholar]
- Soparkar C S, Patrinely J R. Palpebral surgical approaches for orbital fracture repair. Semin Plast Surg. 2002;16:273–282. [Google Scholar]