ABSTRACT
There is a broad spectrum of complications that can occur following cosmetic eyelid surgery. The experienced eyelid surgeon should be able to avoid most serious complications through proper patient selection, a comprehensive preoperative assessment and surgical plan, meticulous surgical technique, and appropriate postoperative care. The aesthetic eyelid surgeon must counsel a patient contemplating blepharoplasty surgery regarding typical expectations including edema, eyelid numbness, dry eyes, and mild blurred vision. Patients must also be aware of the risks and the signs of serious complications such as infection, hematoma, or severe vision loss. Oculofacial surgeons must be capable of managing these adverse outcomes. The management of these urgent complications as well as other significant postoperative problems including diplopia, lagophthalmos, eyelid malposition, severe chemosis and edema, crease abnormalities, and wound dehiscence is outlined in this review.
Keywords: Blepharoplasty, complications, cosmetic eyelid surgery, hematoma, vision loss
Blepharoplasty is one of the most successful and gratifying operations in facial plastic surgery. Although blepharoplasty surgery has a high probability of success, surgeons must avoid complacency in their surgical technique. Patients are often unaware of the complexities of eyelid surgery, so thorough patient education and inclusion in management decisions is essential. Even the most skilled aesthetic eyelid surgeon will encounter surgical complications at some point during his or her career. The experienced surgeon recognizes that many complications can be minimized with thoughtful presurgical planning and careful, meticulous surgical technique. Nonetheless, complications can occur with the best techniques in the best of hands.
PATIENT SELECTION
Proper patient selection is a critical first step in achieving optimal surgical results. In evaluating patients who are considering periocular aesthetic procedures, various psychiatric, emotional, and physical issues must be assessed to determine whether the patient is an appropriate candidate for oculofacial surgery. Silkiss1 has provided an excellent blueprint for improving surgeon and patient communication to help improve surgical outcomes in the cosmetic surgery patient.
A patient's motives and expectations must be thoroughly evaluated to ensure that they are legitimate and realistic. In essence, surgeons must ask themselves, “Is this patient here for the right reasons and do they have an easily correctable problem utilizing procedures that I am comfortable performing?” It is frequently necessary to use patient photographs and hand mirrors to clearly demonstrate which features a patient would like to correct. It may not be clear to the patient that blepharoplasty surgery is not the ideal method to correct diffuse skin pigmentation, periorbital wrinkles, or large malar fluid bags.2 In addition, the patient's concerns may be entirely different than what the surgeon views as the most obvious cosmetic abnormality.
A patient with unreasonable expectations, unclear motives, obvious psychopathology, severe anxiety, or dissatisfaction with previous surgery may ultimately be an unhappy patient even if a reasonable surgical outcome is achieved.3 Body dysmorphic syndrome, dysmorphophobia, or narcissistic behavior must be identified prior to consideration of surgery.4,5,6
Alternatively, a rational, emotionally stable patient with reasonable motives and expectations, who understands there are risks with all surgeries, including cosmetic procedures, is likely to be a good candidate for aesthetic surgery.7 Although it is often the intent of the surgeon to perform symmetric, bilateral surgery, patients often perceive asymmetry in bruising, swelling, and discomfort during the early postoperative period.8 Patients must understand that healing is often unpredictable and uncontrollable and that scarring is part of surgery, with secondary revisions or touch-ups occasionally necessary within a few weeks or a few months after surgery.
Patients with dry eye syndrome should be well informed that blepharoplasty surgery may worsen their symptoms for several days or weeks. Reflex epiphora can be expected in the dry eye patient or patient with mild postoperative lagophthalmos. Contact lens wearers should be aware that spectacles will be recommended postoperatively for 1 to 3 weeks. Postoperative eyelid numbness is not considered a complication and typically resolves over 2 to 4 months. Unfortunately, even with careful patient selection and surgical planning, some patients may be dissatisfied with their results. Establishing a good patient-surgeon bond preoperatively is essential to managing any real or perceived surgical complications that may occur.
PREOPERATIVE EXAMINATION
The preoperative assessment of the eye and periocular region is thoroughly covered in the article by Burroughs and colleagues elsewhere in this issue, so only a few important points will be highlighted in this section. To limit the risk of postoperative complications, certain historical information should be identified. Thyroid eye disease is frequently associated with increased eyelid vascularity and orbital congestion, which may increase the risk of periocular hemorrhage. Poorly controlled systemic hypertension or underlying coagulopathies may cause difficulties in intraoperative hemostasis and increase the risk of postoperative hematoma formation. Similarly, medications with anticoagulant and cardiovascular effects, including aspirin, nonsteroidal anti-inflammatories, platelet inhibitors (Plavix® [Bristol-Meyers Squibb, New York, NY]), low molecular weight heparin products (Lovenox® [Aventis Pharmaceuticals, Inc., Bridgewater, NJ]), factor Xa inhibitors (Artixtra® [Organon Sanofi-Sunthelablo LLC, Roseland, NJ]), warfarin (Coumadin® [Bristol-Meyers Squibb, New York, NY]), large doses of vitamin E, gingko bilboa extract, garlic, ginseng, kava, ephedra, and other herbal agents should be discontinued prior to surgery.9,10 Red wine, which contains resveratol, has been shown to promote bleeding and should not be ingested for 2 weeks before surgery.11
Systemic diseases, such as thyroid dysfunction and renal disease, that may contribute to altered eyelid positions and eyelid edema should be investigated.12 A history of hives, anaphylaxis, or swelling after contact with cold objects should be elicited.13
A preoperative ophthalmologic assessment should document best corrected visual acuity. Dry eyes, narrow anterior chamber angles, facial nerve dysfunction, blepharitis, periorbital eczema, rosacea, blepharospasm, reduced visual acuity, limited visual field, and other ocular disorders should be identified. Postoperative vision changes are common following blepharoptosis repair but also occur after blepharoplasty surgery. Postoperative dry eye is the most common cause of temporary postoperative vision changes. Preexisting dry eyes, diminished blink reflex, upper or lower eyelid malposition, and lagophthalmos are the most common causes of postoperative discomfort and blurred vision from ocular surface exposure. Tear film changes generally improve by 4 to 6 weeks after the operation. Recent studies have observed measurable corneal astigmatic changes several months after upper eyelid ptosis repair and blepharoplasty.14,15,16 Patients should be advised preoperatively that eyelid repositioning may induce or alter astigmatism, leading to temporary or long-term changes in spectacle or contact lens correction, and that new prescriptions may be needed postoperatively. Eyelid surgeons should be aware that transient vision loss, internal ophthalmoplegia, and exotropia can occur due to diffusion of locally injected anesthetic agents causing disruption of nerved transduction in the optic nerve, ciliary ganglion, and medial rectus muscle.17
Identifying eyelid and facial characteristics that are unique to each patient seeking aesthetic surgery is a critical element of preoperative surgical planning and essential in achieving a successful surgical result and minimizing the risk of a disappointed patient and postoperative complications. Previous surgical scars and approaches must be discussed, and the potential impact of prior surgeries on the planned procedures should be reviewed. Blepharoptosis, eyebrow ptosis, eyelid retraction, and/or eyelid, eyebrow, or orbital asymmetries must be identified preoperatively. The surgical plan must also account for the amount and location of excess skin, orbicularis hypertrophy, orbital fat pseudoherniation, malar bags or festoons, and the degree of malar soft tissue descent. The degree and type (medial, lateral) of upper and lower eyelid laxity may impact whether horizontal eyelid shortening procedures are performed at the time of periorbital rejuvenation. Racial and ethnic facial characteristics including skin type and underlying bone structure may also have a role in surgical planning and in establishing realistic expectations for the surgery.18,19,20
All patients contemplating cosmetic oculofacial surgery should have standardized photographs performed of the eyelids and upper face. Clinical photographs provide clear documentation of a patient's preoperative eyelid and facial abnormalities. Blepharoplasty patients should be photographed in primary gaze in both the frontal plane and in oblique views. Occasionally, photographs of patients in up and down gaze may be useful. Photographs can help the surgeon explain to the patient some of their unique clinical features and provide a useful tool in describing the planned surgical techniques. Postoperative photographs can be compared with preoperative photographs to illustrate to the patient their improvement. It is quite remarkable how often patients fail to recognize substantial change in their appearance until they view comparative photographs. Photographs are also an essential part of the medical record and are helpful in resolving medicolegal disputes.
DEEP ORBITAL HEMORRHAGE AND SEVERE VISION LOSS
Deep orbital hemorrhage with vision loss is a rare complication of eyelid surgery. Following cosmetic blepharoplasty, the incidence of orbital hemorrhage after surgery has been estimated to be 1:2000 (0.05%), with orbital hemorrhage resulting in permanent visual loss in 1:10,000 (0.01%).21 Orbital hemorrhage usually occurs within the first 24 hours following surgery but can appear up to a week after surgery. Therefore, it is recommended that operating surgeons should remain readily available to their patients for at least 24 hours after surgery in the event of excessive postoperative bleeding.
Incision of the orbital septum and manipulation of orbital fat are likely prerequisites for blindness resulting from postoperative orbital hemorrhage. Hemorrhage within the orbit may result from traction on orbital fat, resection of orbital fat with unidentified intraoperative bleeding, or posterior extension of wound hemorrhage that often results from delayed bleeding in patients with poorly controlled systemic hypertension. Vision loss may ensue from microvascular compression that leads to ischemic optic neuropathy.22,23,24,25 It has also been postulated that a tense orbit may exceed the mean arterial pressure of the ophthalmic artery or central retinal artery resulting in central retinal artery occlusion.26,27,28,29,30,31,32 With prompt treatment vision loss can be reversible after retrobulbar hemorrhage.27,28,33,34 Rarely, severe proptosis with exposure keratopathy can also occur.
The risk of postoperative orbital hemorrhage can be limited through strict and meticulous attention to intraoperative hemostasis. Insulated fine needle electrocautery (such as a protected tungsten ultrasharp tip device, e.g. Colorado MicroDissection Needle® [Stryker Corp., Portage, MI]), radiosurgery, and carbon dioxide lasers may help seal small blood vessels during dissection and limit the amount of deep orbital traction required by conventional clamping and cutting techniques.35,36,37,38,39,40,41,42 Historical concerns regarding the channeling effect with retrograde transmission of electrical impulses along orbital nerves and vessels have not been realized with current electrosurgical hardware. We are not aware of any reported cases of optic nerve injury secondary to modern monopolar cautery and have not experienced any complications with judicious use during anterior orbital fat dissection and removal. Standard biterminal, bipolar cauterization using a smooth, nonstick, Adson-type forceps limits the area of cauterization, may minimize thermal damage, and is an excellent means to maintain complete hemostasis throughout the procedure. Blood pressure should be closely monitored and controlled while in the operating room and following surgery.
The addition of epinephrine to local anesthetic solutions is generally believed to prolong the duration of action of the anesthetic agent and reduce intraoperative bleeding. Some investigators believe, however, that epinephrine results in vasospasm and rebound congestion after its vasoconstrictive effect wears off.22,30,43,44 Others have also alluded to the possible role of epinephrine in postoperative orbital hemorrhage and have suggested reconsidering the use of epinephrine.45,46 We routinely use epinephrine-containing local anesthetics in periocular surgery and have found that reduced intraoperative bleeding when accompanied by meticulous cauterization and maintenance of a dry operative field outweighs the theoretical risk of rebound hemorrhage.
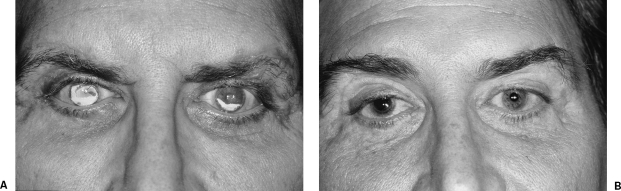
Acute orbital hemorrhage is a medical and surgical emergency. Prompt recognition of severe postoperative bleeding is critical to allow for timely intervention and the prevention of permanent visual sequelae. Postoperative patches and bandages should be avoided to permit early detection of postoperative bleeding. Surgical recovery area staff should be educated regarding the signs of orbital hemorrhage. Often a tense, purplish periorbital hematoma and brisk incisional bleeding is apparent (Fig. 1). Evidence of proptosis, ocular dystopia, severe pain, decreased visual acuity, and abnormal pupillary reactivity (a relative afferent pupillary defect) should alert recovery room personnel to immediately contact the operating surgeon.
Figure 1.
(A) A 60-year-old woman with upper eyelid ptosis and dermatochalasis. (B) Hematoma of left of upper eyelid 6 hours following bilateral upper eyelid blepharoplasty and ptosis repair. (C) Final postoperative appearance following evacuation of hematoma and subsequent ptosis revision surgery.
Simple, postoperative instructions should be outlined and reviewed for the patient and/or their caregivers. A malpractice insurance company review of blindness after blepharoplasty identified activities (constipated bowel movement, sudden coughing fit, bending over and reaching down to tie shoes, and so on) that cause a sudden rise in blood pressure after arriving home from outpatient surgery as major risk factors for early postoperative hemorrhage.47 Head elevation and maintenance of the supine position during sleep, frequent application of ice packs during the first 3 to 4 days after surgery, and limitations on bending over and heavy lifting during the first postoperative week may limit the risk of postoperative hemorrhage.21 Patients should be reminded to continue with all of their antihypertensive medications.
Following discharge from the surgical facility, patients should be given clear instructions to test their vision by completely covering each eye separately and while using their reading spectacles attempt to read small magazine or newspaper print. Patients should expect that their vision may be minimally blurred by debris or ointment in the tear film and possibly by their diminished postoperative blink reflex. Forceful blinking and the installation of artificial tears may help clear the tear film. Any precipitous change in vision should prompt the patient or their family to immediately contact the operating surgeon.
In the event of elevated intraocular pressure (greater than 35 to 40 mm Hg) presumably due to a deep orbital hemorrhage, topical ocular hypotensives (such as β-blockers or carbonic anhydrase inhibitors) should be given and an urgent ophthalmologic consultation requested. More aggressive systemic medical intervention including intravenous acetazolamide (500 mg), mannitol 20% (1 to 2 g/kg over 30 to 60 minutes), and corticosteroids (Solu-medrol 100 mg) may be given with the close involvement of an internist or other colleague qualified to assist in the management of the significant fluid shifts caused by these osmotic agents.31,32,48,49
If progressive vision loss is noted, release of the developing orbital compartment syndrome must be attempted at the bedside. Opening of the wound permits evacuation of the hematoma and active bleeding points can typically be identified and cauterized. Frequently, active bleeding has subsided from tamponading within the closed orbital compartment. The wound may be left open or closed loosely. Prompt wound decompression alone can restore vision.30,44,50 If the hematoma cannot be completely evacuated or the orbital pressure remains elevated, then the standard bedside surgical approach is a lateral canthotomy with lysis of the inferior (and/or superior) crus of the lateral canthal tendon.26,32,49,51,52 If this does not provide for an adequate decompression, then further surgical intervention should be performed in the operating room.
Rapid restoration of optic nerve and ocular blood flow is critical to prevent permanent anoxic damage. It is believed that irreversible optic nerve and retinal ischemic damage may be prevented if appropriate intervention is performed within 1 to 2 hours.53,54 If progressive proptosis, vision loss, or elevated intraocular pressure persists despite medical management, a canthotomy/cantholysis, wound exploration, then an emergent computed tomography scan should be arranged to identify a retrobulbar hematoma and direct the surgical approach. If present, a posterior orbital hemorrhage may require orbital decompression surgery.55 A lower eyelid, transconjunctival approach permits exposure of the orbital floor and creation of a medial floor osteotomy.
INFECTION
Another surgical complication feared by patient and surgeon alike is a postoperative wound infection. Fortunately, postoperative eyelid infections are uncommon due to the extensive vascularization of the periorbital region. The infection rate after blepharoplasty has been estimated to be 0.2%.56
Necrotizing fasciitis resulting from Staphylococcus aureus or group A B-hemolytic Streptococcus has also been reported following blepharoplasty surgery.57,58,59,60,61 These severe infections initially may be difficult to distinguish from other causes of preseptal inflammation. However, necrotizing fasciitis progresses rapidly as the infection spreads along relatively avascular fascial planes. Tense edema, local anesthesia and/or pain, violaceous bullae filled with serosanguinous fluid, overlying necrotic tissue, and a sharp demarcation between the infected area and adjacent uninvolved tissue are characteristic features of infections caused by these virulent organisms.
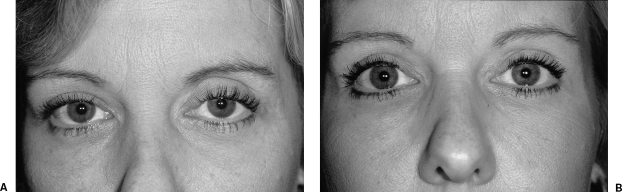
Other cases of bacterial infections of the orbit as well as dacryocystitis have also been reported.62,63 These infections should be managed according to the clinical findings. Obtaining cultures is often difficult, and empiric therapy for suspected infections should be strongly considered in any patient with unexplained erythema and pain (Fig. 2). As with other presentations of periorbital infection, broad-spectrum antibiotic therapy and drainage, if possible, often results in successful treatment of suspected postoperative infections. Patients with necrotizing disease may require debridement of involved tissues; however, extensive tissue removal is associated with extensive eyelid and facial morbidity and may not adequately treat the infection.64 Early and aggressive intravenous antibiotic therapy, such as piperacillin/tazobactam, is critical in treating necrotizing fasciitis. The role of hyperbaric oxygen therapy in preserving ischemic tissue has not been clearly established.61,64
Figure 2.
A 73-year-old woman with right upper eyelid induration, erythema, and edema 2 days following bilateral upper eyelid blepharoplasty and ptosis repair. Cultures of mucopurulent drainage grew methicillin-resistant Staphylococcus aureus.
Methicillin-resistant S. aureus (MRSA) has long been recognized as a cause of severe nosocomial infections. Over the past 5 years, there has been a marked increase in the incidence of MRSA infections among prison inmates, athletic teams, military recruits, children in day care, and other patients with no history of hospitalization. At the time of this publication there have been few reports in the ophthalmic literature of community-associated MRSA (CAMRSA) involving the ocular adnexa65; however, many oculofacial surgeons in the United States are encountering an increasing incidence of CAMRSA infections in their practices (authors' experience and personal communications; Fig. 2).
Hospital-acquired and community-acquired MRSA infections are both resistant to methicillin and other B-lactam antibiotics (such as oxacillin and nafcillin). Whereas hospital strains are resistant to all antibiotics except vancomycin (a glycopeptide) and linezolid, CAMRSA may be sensitive to trimethoprim-sulfamethoxazole, doxycycline, rifampin, and clindamycin. Unfortunately, inducible clindamycin resistance may result in treatment failures despite sensitivity on standard susceptibility testing methods.
Newer-generation carbapenems, such as meropenem and ertapenem, are characterized by broad activity against Gram-positive and Gram-negative aerobes and anaerobes and are resistant to hydrolysis by many β-lactamases. Oxazolidinones, streptogramin combinations, and cyclic lipopeptides are currently being studied for treatment of severe soft tissue infections caused by MRSA and vancomycin-resistant enterococci.66 Linezolid (Zyvox®, Pfizer, New York, NY), an oxazolidinone derivative, has a similar spectrum of coverage to that of vancomycin but can be administered orally unlike vancomycin, which requires long term parenteral administration. Daptomycin (Cubicin®, Cubist Pharmaceuticals, Lexington, MA) is a cyclic lipopeptide that has also received U.S. Food and Drug Administration approval for treatment of severe soft tissue infections.
Atypical mycobacterial infections are an increasingly recognized cause of posttraumatic and postoperative wound infections.67 Nontuberculous mycobacterial infections have been well described following blepharoplasty.68,69,70,71 Tender, nodular swelling with or without draining abscesses are often identified in these infections 1 to several months after surgery. Clinical suspicion, debridement, and confirmatory cultures are important. Oral clarithromycin administered over several months is often an effective treatment.
SEVERE EDEMA
A certain amount of postoperative edema occurs in all surgeries. Postoperative swelling often worsens during the initial 24 to 48 hours following surgery. The degree of swelling is often directly related to surgical factors such as ecchymosis, excessive cauterization, extensive tissue manipulation or excision, and dissection in the lateral canthal area resulting in lymphatic disruption. Patients may also influence their postoperative course through the use of cool compresses, head elevation, and limitations on activity. The most common causes of progressive postoperative periorbital inflammation include infection, toxoallergic blepharoconjunctivitis, and rarely primary acquired cold urticaria (PACU).
Almost all topical medications are capable of causing a toxoallergic response. Patients experiencing severe itching, cutaneous erythema, and conjunctival injection more than would be expected from their stage in healing should be suspected of having an allergic reaction and the topical agent discontinued immediately. Neomycin is a frequent offending medication; however, any drug including bacitracin and erythromycin may cause toxoallergic inflammation. Ocular use of nonophthalmic topical antibiotics inadvertently given to the patient by the nursing staff can also cause significant periocular reactions. Patients will often continue topical antibiotics past the typically recommended 1 week of use. These patients are at greater risk for dermatoblepharitis. Patients increasing their use of preservative containing lubricating eye drops may also develop a toxoallergic blepharoconjunctivitis. Nonpreserved artificial tears should be recommended for all patients requiring intense postoperative ocular lubrication. Cool compresses, topical corticosteroid medications, antihistamine eye drops, and diphenhydramine oral (Benadryl® [Pfizer, Morris Plains, NJ]) may be helpful to more rapidly alleviate the discomfort associated with toxoallergic reactions.
Cold urticaria is generally a primary and self-limited disease that occurs in young adults.72,73 PACU is an increasingly recognized cause of progressive postoperative edema following oculofacial surgery.13 Secondary acquired cold urticaria (SACU) is less common but can be life-threatening. The most common cause of secondary disease is cryoglobulinemia, either primary or related to a malignancy.74 Mononucleosis, syphilis, and leukemia, among others, are less common causes of SACU.
Patients treated for presumed infection with progressive edema, pruritus, and discomfort despite antibiotic therapy and cessation of topical ointments and drops should be suspected of having PACU. A basic systemic workup should be arranged including complete blood count with differential, erythrocyte sedimentation rate, serum protein electrophoresis, cryoglobulin and cryofibrinogen testing, rheumatoid factor, and antinuclear antibodies. A cold stimulation test is necessary to confirm the diagnosis and subtype of PACU. Patient education and cold avoidance are the primary means of treatment. Nonsedating antihistamines may help control cold-induced symptoms. An allergist can help guide workup and management of this condition. Patients with previously established disease can still undergo surgery if appropriate safety precautions are followed in the operating suite and postanesthesia recovery unit.
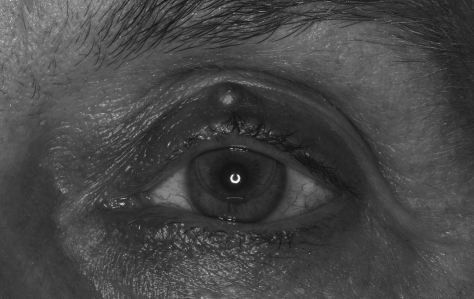
PTOSIS
Blepharoptosis is a common occurrence following upper blepharoplasty surgery. Acquired ptosis often accompanies dermatochalasis and may not be recognized prior to blepharoplasty surgery. Preoperative assessment of the blepharoplasty patient must document the palpebral fissure height, the upper eyelid margin to corneal light reflex distance, and levator muscle function. Clinically significant ptosis must be identified and treated prior to or at the time of blepharoplasty surgery (Fig. 3). The method of repair is determined by the type and degree of ptosis, as well as surgeon preference.
Figure 3.
(A) A 59-year-old man with brow ptosis and severe dermatochalasis. (B) Mild left upper eyelid ptosis evident following uncomplicated brow ptosis repair and upper eyelid blepharoplasty.
Upper eyelid ptosis frequently occurs after upper eyelid procedures due to eyelid edema, diminished levator or Mueller muscle function, or hematoma formation.48,75,76 In most of these cases, the upper eyelid position improves once the edema and ecchymosis resolve and the elevator muscles resume their preoperative function. Prolonged lymphedema or slowly resolving hematoma formation may result in levator muscle or aponeurotic changes that do not completely improve. Similarly, inadvertent disinsertion of the levator aponeurosis during blepharoplasty surgery may result from aggressive resection of the pretarsal orbicularis muscle or preaponeurotic fat. Cases of persistent postoperative ptosis are generally observed for at least 3 to 6 months as spontaneous improvement can occur for several months.77 If clinically significant ptosis remains once all of the eyelid edema has resolved, then levator muscle advancement repair may be indicated.
LAGOPHTHALMOS
An incomplete blink and lagophthalmos frequently occur after upper eyelid ptosis correction and occur less often following upper and lower blepharoplasty surgery. Pretarsal orbicularis muscle dysfunction or denervation or even myotoxicity from local anesthetics may contribute to poor eyelid closure. In most cases mild postoperative lagophthalmos resolves several days or a few weeks after eyelid surgery. Excessive upper or lower eyelid skin resection may cause prolonged lagophthalmos (Fig. 4). Poor eyelid closure may lead to exacerbation of dry eyes and result in exposure keratoconjunctivitis. Aggressive postoperative ocular lubrication is critical in all patients with lagophthalmos. Nonpreserved artificial tears and gels may need to be instilled up to every 30 minutes. Lubricating eye ointments should be applied liberally prior to bedtime. Dissolvable punctal plugs may be helpful for symptomatic relief up to 2 months, whereas silicone punctal plugs are useful for long-term punctal occlusion. In more severe cases, a moisture chamber may need to be constructed over the involved eye during sleep (as described for management of conjunctival chemosis).78,79 Inadequate tear film supplementation can result in disruption of the corneal epithelium and increase the risk for microbial keratitis, stromal thinning or scarring, and permanent visual disturbance.
Figure 4.
(A) Bilateral calcific band keratopathy due to lagophthalmos and chronic corneal exposure. (B) Upper and lower eyelid full-thickness skin grafting required to improve eyelid closure and allow for keratoplasty and visual rehabilitation.
It is worth emphasizing again the importance of preoperative surgical planning in avoiding overcorrection of eyelid skin removal. Unrecognized or uncorrected brow ptosis may give the patient and the inexperienced eyelid surgeon the incorrect impression of significant dermatochalasis. Aggressive upper eyelid skin removal may actually worsen the brow ptosis and lead to a stare or surprised appearance on brow elevation. When surgically marking the blepharoplasty patient, it is important to hold the ptotic brow in an elevated position. A smooth forceps is useful to pinch the redundant eyelid skin. Ideally, subtle movement of the eyelid margin and not overt lagophthalmos should be visible when the skin is pinched.
Transcutaneous lower eyelid blepharoplasty should be reserved for patients with significant excess lower eyelid skin redundancy. The amount of skin removal is determined intraoperatively after creation of the lower eyelid skin-muscle flap. With the eyes in the up gaze position and the mouth open, the skin-muscle flap is draped over the subciliary wound and the amount of skin that can be safely removed is carefully determined. More aggressive skin excision may be performed laterally, whereas medial skin resection should be minimal. In both upper and lower eyelid transcutaneous blepharoplasties, conservative skin resection is recommended as it is much simpler to remove additional skin at a later time than to correct vertical shortening of the eyelid.
If excessive skin resection is a concern during the operation, then the surgeon can wrap the removed skin in saline gauze, refrigerate, and replace as a skin graft if needed in 1 to 2 weeks. This contingency is rarely implemented by experienced blepharoplasty surgeons. More commonly, correction of anterior lamella shortening of the upper or lower eyelid is done in a delayed fashion and may require cheek elevation, canthoplasty, or even full-thickness skin grafting. If adequate upper eyelid donor skin is not available after blepharoplasty surgery, the retroauricular and preauricular areas provide the next best donor sites for full-thickness skin grafting. The supraclavicular region and inner arm are also useful donor areas if rhytidectomy incisions preclude the use of periauricular skin or if additional skin is needed.
A 4–0 silk traction suture is passed the through the margin of the operative eyelid and the eyelid placed on stretch. In upper eyelid repair, an incision is made in the eyelid crease area, and subcutaneous undermining is performed superiorly. The skin graft is then nicely hidden by the supratarsal fold. In lower eyelid repair, an incision is made in the previous subciliary incision site, and a skin flap is raised down to the inferior orbital rim. Areas of cicatrix formation are lysed until the skin moves freely and the size of the lower eyelid defect can be assessed. The slightly oversized, thinned skin graft is secured within the defect using several interrupted 6–0 plain or mild gut sutures. A lateral canthoplasty is indicated to maintain lower eyelid tone and position.
Postoperative lagophthalmos may also occur following contracture of the middle lamellar tissues of the upper (orbital septum, levator aponeurosis) or lower (orbital septum, lower eyelid retractors) eyelid. Limitation of eyelid excursion due to deep traction bands is usually evident on observation of eyelid movement and palpation of the involved eyelid. Intermittent eyelid massage, temporary Frost sutures, and occasionally corticosteroid injections can be beneficial during the first few months after surgery; however, eyelid malpositions that have not adequately resolved by 6 months after surgery may require surgical intervention.80,81,82
Inadvertent inclusion of the orbital septum during levator aponeurosis advancement, eyelid crease formation, or wound closure is probably the most common cause of postoperative middle lamellar cicatrix formation in the upper eyelid. In these cases, lagophthalmos may occur even if there is adequate overlying skin. Lysis of adhesions between the preseptal orbicularis muscle and the orbital septum and levator aponeurosis should be performed. Levator aponeurosis recession is required in more severe cases of upper eyelid retraction. Recession of the aponeurosis should be performed in a graded fashion with careful dissection performed in the avascular plane separating the aponeurosis from the underlying Müller's muscle. Ideally, minimal patient sedation is utilized during aponeurotic surgery so that upper eyelid height and contour can be assessed intraoperatively.
Lower eyelid retraction due to middle lamellar cicatrix formation can be a particularly challenging problem to correct. A variety of different surgical approaches have been described to treat postblepharoplasty lower eyelid retraction.80,81,83,84,85,86 With the eyelid placed on stretch, as described above, a subciliary incision is performed and a shelved dissection plane created, leaving the pretarsal orbicularis muscle intact and continuing the dissection in a suborbicular fashion toward the inferior orbital rim. Deep cicatricial bands are released until the skin-muscle flap moves freely. Recession of the lower eyelid retractors is carefully performed by dissecting the fibrotic retractor complex from the underlying conjunctiva until the eyelid is released. Semirigid spacer placement is generally not required in all but the most severe cases. A limited lateral tarsal strip canthoplasty procedure should also be performed if lower eyelid laxity is present. Limiting the length of the vertical cantholysis helps to ensure that the lateral retinacular tissues below the tarsus are not disturbed, which may aid in anatomic reattachment of the tarsal strip84 and may limit postoperative lymphedema. In severe cases of lower eyelid anterior and/or middle lamellar tissue shortage, additional eyelid support can be accomplished by vertical recruitment of premalar tissue utilizing aggressive suborbicularis oculi fat elevation.
Following skin graft repair or middle lamellar cicatrix release, a double-armed 4–0 silk traction (Frost) suture should be passed over a cotton or rubber bolster, through the eyelid margin, and secured to the forehead (lower eyelid suture) or cheek (upper eyelid suture) and left in place up to 1 to 3 weeks following eyelid reconstruction.87 All the wounds are dressed with ophthalmic antibiotic ointment. A TELFA® nonadherent dressing (The Kendall Company, Mansfield, MA) and two eye patches are placed over the eyelid skin grafts for moderate postoperative compression. The patch may be removed in 3 days.
CONJUNCTIVAL CHEMOSIS
Persistent conjunctival chemosis following blepharoplasty surgery can be disturbing to the patient and a challenge to the surgeon.88 Prominent postoperative edema and chemosis may be more common in poorly treated rosacea patients, in hypervascular patients who excessively blush with laughter or facial expression, and with extensive surgical dissection of the lateral canthus and periorbital areas. Chemosis may cause epiphora, corneal and conjunctival drying, corneal dellen, blurred vision, and ocular discomfort. Mild cases often quickly improve with continuous ocular lubrication such as frequent nonpreserved artificial tears and lubricating eye ointments. If topical antibiotic drops or ointment are suspected of causing an allergic reaction, then these should be discontinued. Topical and systemic corticosteroids may be helpful when early evidence of chemosis is detected. Gentle massage and reposition of prolapsing conjunctiva may hasten improvement. Severe conjunctival prolapse may require creation of a moisture chamber using a transparent plastic wrap or cellophane (Saran wrap), OpSite™ (Smith and Nephew, London, UK) Tegaderm™ (3M, St. Paul, MN), or similar transparent, occlusive dressing secured to the orbital rim with a petrolatum-based ointment. Adjunctive lubricating ointment should be applied to the exposed conjunctiva beneath the occlusive dressing.78,79
Chronic, unresolving chemosis may result in breakdown of the forniceal attachments of the conjunctiva.89 If conservative measures have failed, then refixation of the fornix may be required. A few or several double-armed absorbable sutures such as 5–0 chromic gut are passed through the prolapsing conjunctiva and involved fornix and secured externally over the eyelid skin. Alternatively, a modified conjunctivoplasty with gentle cauterization may adequately reposit prolapsed conjunctiva.
EYELID CREASE ASYMMETRY
Preoperative identification of the existing eyelid crease and precise measurements and marking of the planned upper blepharoplasty incision site are critical to minimize the risk of postoperative eyelid crease asymmetries. If adequate skin redundancy is present, reexcision of anterior lamellar tissue including the unwanted eyelid crease may be an option. More frequently, an incision is placed where the crease is desired, and undermining of the unwanted eyelid crease is performed. A new eyelid crease is created during interrupted skin closure by incorporating superficial fibers of the levator aponeurosis just above the superior edge of the tarsal plate. After tightening these sutures, the eyelid margin position is observed to ensure that ectropion does not result. This technique works nicely for elevation of a crease that is too low. Excessively high creases are more challenging (Fig. 5). It is sometimes easier to raise the crease of the contralateral eyelid to help improve symmetry.
Figure 5.
(A) A 37-year-old woman with asymmetric upper eyelid crease height following blepharoplasty. (B) Improved crease symmetry following insertion of Alloderm® graft and refixation of left upper eyelid crease.
DIPLOPIA
Diplopia is a feared but avoidable complication of blepharoplasty surgery. Injuries to the inferior oblique muscle, and less commonly to the inferior rectus muscle, are the most serious causes of postoperative double vision following lower eyelid blepharoplasty.90,91,92,93,94,95 Rarely, medial rectus dysfunction can occur with deep resection of the medial fat pad in the upper eyelid. Injuries to the superior oblique tendon and muscle have also been reported.95,96,97,98
Transient extraocular muscle dysfunction may result from traumatic intramuscular hemorrhage or edema. Another proposed mechanism of temporary diplopia is myotoxicity associated with local anesthetics.76 Conservative treatment and observation for spontaneous improvement is indicated in these patients. Patients also occasionally complain of monocular diplopia due to disruption of the tear film. This mild diplopia improves with blinking and resolves after a few days after surgery.
Permanent strabismus can occur following direct or indirect muscle or nerve injury. The importance of gentle lower eyelid fat resection performed under direct visualization cannot be overemphasized. The surgeon must seek to isolate the respective fat pads prior to removal or repositioning. The inferior oblique muscle is the most commonly encountered extraocular muscle in blepharoplasty surgery. The inferior oblique muscle should be located and not disturbed in any fashion during the orbital fat dissection.92,99 Meticulous cautery of the fat to maintain a dry field throughout the lower eyelid blepharoplasty is critical and allows the surgeon to maintain awareness of the proximity of the inferior oblique muscle. Particular care should be exercised in patients undergoing secondary blepharoplasty procedures.90,92
Significant postoperative diplopia should be closely observed postoperatively. If complete resolution of the double vision does not occur after 8 weeks, then referral to a strabismologist is indicated. Monthly orthoptic measurements in all fields of gaze and Hess-Lancaster screening examinations should be performed to detect improvements in ocular motility. Fresnel-type stick-on or permanent prisms ground into spectacles may be useful for temporary treatment of patients with disabling diplopia in primary gaze or the reading position. Surgical exploration and/or extraocular muscle surgery by a strabismologist may be necessary for patients with incomitant deviations that have not improved several months after eyelid surgery.
WOUND DEHISCENCE
Dehiscence of a postoperative wound may occur due to inadvertent trauma, poor wound healing, excessive tension on wound closure, early suture removal, and infection. It often occurs in patients who inadvertently rub their eyes while sleeping or in those patients who excessively raise their eyebrows, squeeze their eyelids, or animate their face. Dehiscences usually occur laterally in both upper and lower eyelid surgery. Postoperative Steri-Strips™ (3M, St. Paul, MN) may only offer limited protection but serve to help remind patients not to touch or rub the operative site(s). Absorbable sutures, particularly fast-absorbing plain gut sutures in the upper eyelid, are more likely to allow for wound disruption; however, wound dehiscence can also occur with nonabsorbable suture placement. Nonabsorbable suture removal is recommended 5 to 7 days after surgery.
Repair of upper eyelid skin wound dehiscence should be performed with nonabsorbable sutures passed in interrupted fashion using the next largest caliber of suture material (i.e., 6–0 polypropylene rather than 7–0 polypropylene). Use of buried absorbable sutures such as 6–0 polyglactin 910 may help reapproximate the orbicularis muscle and minimize tension on the skin closure. Lower eyelid skin wounds are also managed with interrupted wound closure. Wounds open longer than 24 hours should have their edges sharply freshened prior to closure.
Deeper wound repair following lower eyelid blepharoplasty may require refixation of a dehisced lateral canthoplasty. Resuturing of a lateral tarsal strip should seek to minimize tension on the lower eyelid. Supplemental plication sutures passed through pretarsal orbicularis muscle and suspended to the periorbita of the lateral orbital rim may reinforce closure of the lateral canthal area. Steri-Strip™ (3M, St. Paul, MN) adhesive closure strips should be placed across the reoperated areas and patients reminded to avoid to touching the affected areas. A hard eye shield (Foxx shield) may diminish the risk of nocturnal inadvertent wound disruption.
MEDIAL CANTHAL WEBBING
Attention to a few important surgical guidelines regarding medial upper eyelid wound closure will help prevent webbing in the medial canthus. Aggressive excision of medial eyelid skin including some nasal skin, spectacle deformation of the medial canthus, and a preexisting tarsal fold increase the risk of web formation. Prior to closure, a strip of orbicularis muscle under the superior and inferior medial wound edges should be carefully excised. It is helpful to leave the medial 4 to 6 mm of the wound open and to place the second running suture bite close to the knot. Closure in this manner should allow the medial wound edges to gently appose so that the upper and lower skin edges are of equal length.
Spectacle wearers should be advised to rest their glasses lower on their nose to avoid tension on the medical canthus. Gentle postoperative massage may be useful for mild webbing. More extensive medial canthal deformities may require Z-plasty or W-plasty transposition flaps or Y-V advancement procedures.100 Excision of the scar tissue and muscle under the abnormal skin web as described for treatment of the Asian epicanthal fold may allow the overlying skin to adhere to the deeper tissues.101,102
HYPERPIGMENTATION
Hyperpigmentation following incisional eyelid surgery may result from slowly resolving ecchymosis and red blood cell degradation products (hemosiderin) causing staining of the overlying skin. This pigmentation is usually self-limited. Careful hemostasis and evacuation of postoperative hematomas may diminish the likelihood of hyperpigmentation. Postinflammatory pigmentary changes may also lead to darkening of the skin. Melanin deposition may be increased in the epidermis. Postoperative sun exposure is a rare cause of hyperpigmentation, but sunglasses with ultraviolet protection are useful during surgical recovery.48 Fitzpatrick skin types III to V may be predisposed to postoperative hyperpigmentation.
Mild to moderate postinflammatory changes may respond to several weeks of topical hydroquinone 4% United States Pharmacopia cream applied at bedtime. Hydrocortisone 2.5% also helps reduce inflammatory hyperpigmentation.
INCISION AND SCAR ABNORMALITIES
Numbness involving the upper eyelid skin and eyelashes is a common, expected outcome after upper eyelid crease incisions in blepharoplasty or blepharoptosis repair. Vertically oriented sensory nerve fibers from the supraorbital, supratrochlear, and lacrimal nerves travel in the preorbicular plane, suborbicular fascial plane, and within the orbicularis muscle.103 These distal branches of the ophthalmic division of the trigeminal nerve are transected during supratarsal eyelid crease incision for blepharoplasty and ptosis repair.104 Recovery from new nerve growth and collateral sprouting may take several weeks or months.105
Most significant eyelid scar abnormalities can be avoided by appropriate incision placement, minimal tissue manipulation, and appropriate suture selection, tension, and removal. Excessive thermal damage from electrocautery or defocusing of the laser can result in hypertrophic scarring. Asian patients and those with a history of keloid formation may be at increased risk of hypertrophic scar formation. True keloid formation in the eyelids is exceedingly rare. Local corticosteroid injections should be considered with caution due to the risk of dermal atrophy and skin depigmentation.
Incisions that extend laterally to the lateral rim and beyond may not be easily concealed. Visible scars in the lateral canthal region may improve with massage in the first few months after surgery. A steroid-containing ointment, such as fluorometholone 0.1% or hydrocortisone 0.5% or 1%, can help soften firm scars and lessen erythema. Unsightly scars may require reexcision with debulking of the adjacent subcutaneous tissue. Meticulous closure with good wound eversion should be performed with nonabsorbable sutures.
Sequestered epithelial remnants may form small whitish-yellow inclusion cysts along the suture line. These may atrophy in 2 to 3 months or are simply managed without anesthesia by uncapping of the cyst and marsupialization with an 18-gauge needle.
A larger, tender, erythematous nodule along the incision line may represent encapsulation around a suture sometimes referred to as a suture granuloma106 (Fig. 6). These often appear 4 to 6 weeks after placement of buried catgut, polyglactin, or other slowly absorbable suture. Warm compresses and topical corticosteroids may help resolve suture granulomas. If these nodules do not improve with observation and conservative management, then incision with expression of the inflammatory contents and removal of the offending suture, if visible, is recommended.
Figure 6.
Erythematous nodule along the incision line representing encapsulation around a suture (suture granuloma).
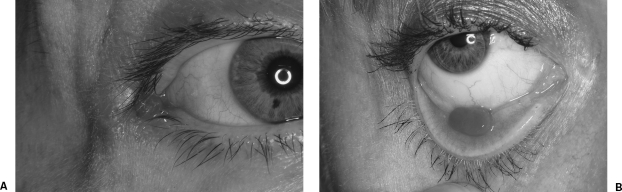
Pyogenic granulomas can occur along transconjunctival incision sites.107 These crimson-colored, fleshy, highly vascular lesions are, paradoxically, neither pyogenic nor granulomatous (Fig. 7). Rather, impaired wound closure or chronic irritation may permit the development of exuberant granulation tissue.108 Pyogenic granulomas may improve with topical corticosteroid ointment. Larger lesions may require excision in the office with topical anesthetic eye drops. Gentle cautery at the base of the excised lesion minimizes the risk of recurrence.
Figure 7.
(A) Lateral canthal pyogenic granuloma following canthoplasty. (B)Lower eyelid pyogenic granuloma following transconjunctival blepharoplasty.
SUMMARY
Aesthetic eyelid surgery is a wonderful and powerful option in facial rejuvenation. Surgeons and patients alike must be cautious of the apparent simplicity of blepharoplasty surgery. The busy oculofacial surgeon will encounter blepharoplasty complications and must be aware of the ophthalmic and potentially sight-threatening sequelae. A thorough understanding of eyelid surgery complications and their management is critical for all surgeons who perform periorbital rejuvenation procedures.
REFERENCES
- Silkiss R Z. Eight-fold path to happiness for the cosmetic surgery patient. Ophthal Plast Reconstr Surg. 2006;22:157–160. doi: 10.1097/01.iop.0000214509.24446.32. [DOI] [PubMed] [Google Scholar]
- Holt J E, Holt G R. Blepharoplasty: indications and preoperative assessment. Arch Otolaryngol. 1985;111:394–397. doi: 10.1001/archotol.1985.00800080080010. [DOI] [PubMed] [Google Scholar]
- Adams J, Murray R. The general approach to the difficult patient. Emerg Med Clin North Am. 1998;16:689–700. doi: 10.1016/s0733-8627(05)70028-6. [DOI] [PubMed] [Google Scholar]
- Jordan D R, Mawn L A. Dysmorphophobia. Can J Ophthalmol. 2003;38:223–224. doi: 10.1016/s0008-4182(03)80064-9. [DOI] [PubMed] [Google Scholar]
- Mackley C L. Body dysmorphic disorder. Dermatol Surg. 2005;31:553–558. doi: 10.1111/j.1524-4725.2005.31160. [DOI] [PubMed] [Google Scholar]
- McCullough M E, Emmons R A, Kilpatrick S D, Mooney C N. Narcissists as ‘victims’: the role of narcissism in the perception of transgressions. Pers Soc Psychol Bull. 2003;29:885–893. doi: 10.1177/0146167203029007007. [DOI] [PubMed] [Google Scholar]
- Lewis C M, Lavell S, Simpson M F. Patient selection and patient satisfaction. Clin Plast Surg. 1983;10:321–332. [PubMed] [Google Scholar]
- Hatton M P, Kelley J M, Rubin P AD. Symmetry in healing after bilateral eyelid surgery. Ophthal Plast Reconstr Surg. 2006;22:266–268. doi: 10.1097/01.iop.0000225747.29778.3b. [DOI] [PubMed] [Google Scholar]
- Bartley G B, Warndahl R A. Surgical bleeding associated with aspirin and nonsteroidal anti-inflammatory agents. Mayo Clin Proc. 1992;67:402–403. doi: 10.1016/s0025-6196(12)61566-3. [DOI] [PubMed] [Google Scholar]
- Ang-Lee M K, Moss J, Yuan C. Herbal medicines and perioperative care. JAMA. 2001;286:208–216. doi: 10.1001/jama.286.2.208. [DOI] [PubMed] [Google Scholar]
- Wolfort F G, Pan D, Gee J. Alcohol and preoperative management. Plast Reconstr Surg. 1996;98:1306–1309. doi: 10.1097/00006534-199612000-00033. [DOI] [PubMed] [Google Scholar]
- Knopf H. Refractive distractions from drugs and disease. Ophthalmol Clin North Am. 1993;6:599–605. [Google Scholar]
- Burroughs J R, Patrinely J R, Nugent J S, Soparkar C NS, Anderson R L, Pennington J H. Cold urticaria: an underrecognized cause of postsurgical periorbital swelling. Ophthal Plast Reconstr Surg. 2005;21:327–330. doi: 10.1097/01.iop.0000176272.40058.4f. [DOI] [PubMed] [Google Scholar]
- Holck D E, Dutton J J, Wehrly S R. Changes in astigmatism after ptosis surgery measured by corneal topography. Ophthal Plast Reconstr Surg. 1998;14:151–158. doi: 10.1097/00002341-199805000-00001. [DOI] [PubMed] [Google Scholar]
- Brown M S, Siegel I M, Lisman R D. Prospective analysis of changes in corneal topography after upper eyelid surgery. Ophthal Plast Reconstr Surg. 1999;15:378–383. doi: 10.1097/00002341-199911000-00002. [DOI] [PubMed] [Google Scholar]
- Shao W, Byrne P, Harrison A, Nelson E, Hilger P. Persistent blurred vision after blepharoplasty and ptosis repair. Arch Facial Plast Surg. 2004;6:155–157. doi: 10.1001/archfaci.6.3.155. [DOI] [PubMed] [Google Scholar]
- Oliva M S, Ahmadi A J, Mudumbai R, Hargiss J L, Sires B S. Transient impaired vision, external ophthalmoplegia, and internal ophthalmoplegia after blepharoplasty under local anesthesia. Am J Ophthalmol. 2003;135:410–412. doi: 10.1016/s0002-9394(02)01939-6. [DOI] [PubMed] [Google Scholar]
- Wiggs E O. Blepharoplasty complications. Trans Am Acad Ophthalmol Otolaryngol. 1976;81:603–606. [PubMed] [Google Scholar]
- Beekhuis G J. Blepharoplasty. Otolaryngol Clin North Am. 1980;13:225–236. [PubMed] [Google Scholar]
- Shorr N, Cohen M S. Cosmetic blepharoplasty. Ophthalmol Clin North Am. 1991;4:17–33. [Google Scholar]
- Hass A N, Penne R B, Stefanyszyn M A, Flanagan J C. Incidence of postblepharoplasty orbital hemorrhage and associated visual loss. Ophthal Plast Reconstr Surg. 2004;20:426–432. doi: 10.1097/01.iop.0000143711.48389.c5. [DOI] [PubMed] [Google Scholar]
- Anderson R L, Edwards J J. Bilateral visual loss after blepharoplasty. Ann Plast Surg. 1980;5:288–292. doi: 10.1097/00000637-198010000-00007. [DOI] [PubMed] [Google Scholar]
- Goldberg R A, Marmor M F, Shorr N, Christenbury J D. Blindness following blepharoplasty: two case reports, and a discussion of management. Ophthalmic Surg. 1990;21:85–89. [PubMed] [Google Scholar]
- Good C D, Cassidy L M, Moseley I F, Sanders M D. Posterior optic nerve infarction after lower lid blepharoplasty. J Neuroophthalmol. 1999;19:176–179. [PubMed] [Google Scholar]
- Yachouh J, Arnaud D, Psomas C, Arnaud S, Goudot P. Amaurosis after lower eyelid laser blepharoplasty. Ophthal Plast Reconstr Surg. 2006;22:214–235. doi: 10.1097/01.iop.0000214531.58587.57. [DOI] [PubMed] [Google Scholar]
- Hartley J H, Jr, Lester J C, Schatten W E. Acute retrobulbar hemorrhage during elective blepharoplasty: its pathophysiology and management. Plast Reconstr Surg. 1973;52:8–12. doi: 10.1097/00006534-197307000-00002. [DOI] [PubMed] [Google Scholar]
- Hueston J T, Heinze J B. Successful early relief of blindness occurring after blepharoplasty: case report. Plast Reconstr Surg. 1974;53:588–592. doi: 10.1097/00006534-197405000-00026. [DOI] [PubMed] [Google Scholar]
- Hueston J T, Heinze J B. A second case of relief of blindness following blepharoplasty: case report. Plast Reconstr Surg. 1977;59:430–431. doi: 10.1097/00006534-197703000-00027. [DOI] [PubMed] [Google Scholar]
- Kraushar M F, Seelenfreund M H, Freilich D B. Central retinal artery closure during orbital hemorrhage from retrobulbar injection. Trans Am Acad Ophthalmol Otolaryngol. 1974;78:65–70. [PubMed] [Google Scholar]
- Putterman A M. Temporary blindness after cosmetic blepharoplasty. Am J Ophthalmol. 1975;80:1081–1083. doi: 10.1016/0002-9394(75)90339-6. [DOI] [PubMed] [Google Scholar]
- Heinze J B, Hueston J T. Blindness after blepharoplasty: mechanism and early reversal. Plast Reconstr Surg. 1978;61:347–354. doi: 10.1097/00006534-197803000-00007. [DOI] [PubMed] [Google Scholar]
- Kelly P W, May D R. Central retinal artery occlusion following cosmetic blepharoplasty. Br J Ophthalmol. 1980;64:918–922. doi: 10.1136/bjo.64.12.918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fry H J. Reversible visual loss after proptosis from retrobulbar hemorrhage. Plast Reconstr Surg. 1969;44:480–483. [PubMed] [Google Scholar]
- Huang T T, Horowitz B, Lewis S R. Retrobulbar hemorrhage. Plast Reconstr Surg. 1977;59:39–44. doi: 10.1097/00006534-197701000-00007. [DOI] [PubMed] [Google Scholar]
- Colton J J, Beekhuis G J. Use of electrosurgery in blepharoplasty. Arch Otolaryngol. 1985;111:441–442. doi: 10.1001/archotol.1985.00800090055007. [DOI] [PubMed] [Google Scholar]
- Tobin H A. Electrosurgical blepharoplasty: a technique that questions conventional concepts of fat compartmentalization. Ann Plast Surg. 1985;14:59–63. doi: 10.1097/00000637-198501000-00011. [DOI] [PubMed] [Google Scholar]
- David L M, Sanders G. CO2 laser blepharoplasty: a comparison to cold steel and electrocautery. J Dermatol Surg Oncol. 1987;13:110–114. doi: 10.1111/j.1524-4725.1987.tb00507.x. [DOI] [PubMed] [Google Scholar]
- Sherman D D, Dortzbach R K. Monopolar electrocautery dissection in ophthalmic plastic surgery. Ophthal Plast Reconstr Surg. 1993;9:143–147. doi: 10.1097/00002341-199306000-00012. [DOI] [PubMed] [Google Scholar]
- Popp J C. Complications of blepharoplasty and their management. J Dermatol Surg Oncol. 1992;18:1122–1126. doi: 10.1111/j.1524-4725.1992.tb02792.x. [DOI] [PubMed] [Google Scholar]
- Seckel B R, Kovanda C J, Cetrulo C L, Jr, Passmore A K, Meneses P G, White T. Laser blepharoplasty with transconjunctival orbicularis muscle/septum tightening and periocular skin resurfacing: a safe and advantageous technique. Plast Reconstr Surg. 2000;106:1127–1141. doi: 10.1097/00006534-200010000-00024. [DOI] [PubMed] [Google Scholar]
- Münker R. Laser blepharoplasty and periorbital laser skin resurfacing. Facial Plast Surg. 2001;17:209–217. doi: 10.1055/s-2001-17971. [DOI] [PubMed] [Google Scholar]
- Older J J. The value of radiosurgery in oculoplastics. Ophthal Plast Reconstr Surg. 2002;18:214–218. doi: 10.1097/00002341-200205000-00012. [DOI] [PubMed] [Google Scholar]
- Lemoine A N., Jr Acute retrobulbar hemorrhage during elective blepharoplasty. Plast Reconstr Surg. 1973;52:12–13. doi: 10.1097/00006534-197307000-00002. (commentary) [DOI] [PubMed] [Google Scholar]
- Rafaty F M. Transient total blindness during cosmetic blepharoplasty: a case report and discussion. Ann Plast Surg. 1979;3:373–375. doi: 10.1097/00000637-197910000-00016. [DOI] [PubMed] [Google Scholar]
- Callahan M A. Prevention of blindness after blepharoplasty. Ophthalmology. 1983;90:1047–1051. doi: 10.1016/s0161-6420(83)80045-1. [DOI] [PubMed] [Google Scholar]
- Mahaffey P J, Wallace A F. Blindness following cosmetic blepharoplasty—a review. Br J Plast Surg. 1986;39:213–221. doi: 10.1016/0007-1226(86)90085-8. [DOI] [PubMed] [Google Scholar]
- Gorney M. Claims prevention for the aesthetic surgeon: preparing for the less-than-perfect outcome. Facial Plast Surg. 2002;18:135–142. doi: 10.1055/s-2002-32204. [DOI] [PubMed] [Google Scholar]
- Adams B JS, Fuerstein S S. Complications of blepharoplasty. Ear Nose Throat J. 1986;65:11–28. [PubMed] [Google Scholar]
- Castillo G D. Management of blindness in the practice of cosmetic surgery. Otolaryngol Head Neck Surg. 1989;100:559–562. doi: 10.1177/019459988910000606. [DOI] [PubMed] [Google Scholar]
- Lloyd W C, III, Leone C R., Jr Transient bilateral blindness following blepharoplasty. Ophthal Plast Reconstr Surg. 1985;1:29–34. doi: 10.1097/00002341-198501000-00005. [DOI] [PubMed] [Google Scholar]
- Stasior O G. Blindness associated with cosmetic blepharoplasty. Clin Plast Surg. 1981;8:793–795. [PubMed] [Google Scholar]
- Waller R R. Is blindness a realistic complication in blepharoplasty procedures. Ophthalmology. 1978;85:730–735. doi: 10.1016/s0161-6420(78)35621-9. [DOI] [PubMed] [Google Scholar]
- Hayreh S S, Weingeist T A. Experimental occlusion of the central artery of the retina I. Ophthalmoscopic and fluorescein fundus angiographic studies. Br J Ophthalmol. 1980;64:896–912. doi: 10.1136/bjo.64.12.896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoon Y H, Marmor M F. Dextromethorphan enhances ERG recovery after retinal ischemia. Arch Ophthalmol. 1989;107:409–411. doi: 10.1001/archopht.1989.01070010419037. [DOI] [PubMed] [Google Scholar]
- Sacks S H, Lawson W, Edelstein D, Green R P. Surgical treatment of blindness secondary to intraorbital hemorrhage. Arch Otolaryngol Head Neck Surg. 1988;114:801–803. doi: 10.1001/archotol.1988.01860190105034. [DOI] [PubMed] [Google Scholar]
- Carter S R, Stewart J M, Khan J, et al. Infection after blepharoplasty with and without carbon dioxide laser resurfacing. Ophthalmology. 2003;110:1430–1432. doi: 10.1016/S0161-6420(03)00447-0. [DOI] [PubMed] [Google Scholar]
- Morgan S C. Orbital cellulitis and blindness following a blepharoplasty. Plast Reconstr Surg. 1979;64:823–826. doi: 10.1097/00006534-197912000-00022. [DOI] [PubMed] [Google Scholar]
- Jordan D R, Mawn L, Marshall D H. Necrotizing fasciitis caused by group A Streptococcus infection after laser blepharoplasty. Am J Ophthalmol. 1998;125:265–266. doi: 10.1016/s0002-9394(99)80108-1. [DOI] [PubMed] [Google Scholar]
- Suner I J, Meldrum M L, Johnson T E, Tse D T. Necrotizing fasciitis after cosmetic blepharoplasty. Am J Ophthalmol. 1999;128:367–368. doi: 10.1016/s0002-9394(99)00134-8. [DOI] [PubMed] [Google Scholar]
- Chen S H, Wang C H, Chen H C, Weng G C, Lin P Y, Wei F C. Upper eyelid mycobacterial infection following Oriental blepharoplasty in a pulmonary tuberculosis patient. Aesthetic Plast Surg. 2001;25:295–298. doi: 10.1007/s002660010141. [DOI] [PubMed] [Google Scholar]
- Goldberg R A, Li T G. Postoperative infection with group A beta-hemolytic Streptococcus after blepharoplasty. Am J Ophthalmol. 2002;134:908–910. doi: 10.1016/s0002-9394(02)01848-2. [DOI] [PubMed] [Google Scholar]
- Allen M V, Cohen K L, Grimson B S. Orbital cellulitis secondary to dacryocystitis following blepharoplasty. Ann Ophthalmol. 1985;17:498–499. [PubMed] [Google Scholar]
- Rees T D, Craig S M, Fisher Y. Orbital abscess following blepharoplasty. Plast Reconstr Surg. 1984;73:126–127. doi: 10.1097/00006534-198401000-00031. [DOI] [PubMed] [Google Scholar]
- Kronish J W, McLeish W M. Eyelid necrosis and periorbital necrotizing fasciitis. Ophthalmology. 1991;98:92–98. doi: 10.1016/s0161-6420(91)32334-0. [DOI] [PubMed] [Google Scholar]
- Rutar T, Chambers H F, Crawford J B, et al. Ophthalmic manifestations of infections caused by the USA300 clone of community-associated methicillin-resistant Staphylococcus aureus. Ophthalmology. 2006;113:1455–1462. doi: 10.1016/j.ophtha.2006.03.031. [DOI] [PubMed] [Google Scholar]
- Raghavan M, Linden P K. Newer treatment options for skin and soft tissue infections. Drugs. 2004;64:1621–1642. doi: 10.2165/00003495-200464150-00002. [DOI] [PubMed] [Google Scholar]
- Klapper S R, Patrinely J R, Kaplan S L, Font R L. Atypical mycobacterial infection of the orbit. Ophthalmology. 1995;102:1536–1541. doi: 10.1016/s0161-6420(95)30834-2. [DOI] [PubMed] [Google Scholar]
- Moorthy R S, Rao N A. Atypical mycobacterial wound infection after blepharoplasty. Br J Ophthalmol. 1995;79:93. doi: 10.1136/bjo.79.1.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kevitch R, Guyuron B. Mycobacterial infection following blepharoplasty. Aesthetic Plast Surg. 1991;15:229–232. doi: 10.1007/BF02273863. [DOI] [PubMed] [Google Scholar]
- Gonzalez-Fernandez F, Kaltreider S A. Orbital lipogranulomatous inflammation harboring Mycobacterium abscessus. Ophthal Plast Reconstr Surg. 2001;17:374–380. doi: 10.1097/00002341-200109000-00013. [DOI] [PubMed] [Google Scholar]
- Chang W J, Tse D T, Rosa R H, Jr, Miller D. Periocular atypical mycobacterial infections. Ophthalmology. 1999;106:86–90. doi: 10.1016/S0161-6420(99)90010-6. [DOI] [PubMed] [Google Scholar]
- Wanderer A A. The spectrum of cold urticaria. Immunol Allergy Clin North Am. 1995;15:701–723. [Google Scholar]
- Lee C W, Sheffer A L. Primary acquired cold urticaria. Allergy Asthma Proc. 2003;24:9–12. [PubMed] [Google Scholar]
- Wanderer A A, Grandel K E, Wasserman S I, Farr R S. Clinical characteristics of cold-induced systemic reactions in acquired cold urticaria syndromes: recommendations for prevention of this complication and a proposal for a diagnostic classification of cold urticaria. J Allergy Clin Immunol. 1986;78:417–423. doi: 10.1016/0091-6749(86)90027-8. [DOI] [PubMed] [Google Scholar]
- Baylis H I, Sutcliffe T, Fett D R. Levator injury during blepharoplasty. Arch Ophthalmol. 1984;102:570–571. doi: 10.1001/archopht.1984.01040030448023. [DOI] [PubMed] [Google Scholar]
- Rainin E A, Carlson B M. Postoperative diplopia and ptosis: a clinical hypothesis based on the myotoxicity of local anesthetics. Arch Ophthalmol. 1985;103:1337–1339. doi: 10.1001/archopht.1985.01050090089038. [DOI] [PubMed] [Google Scholar]
- Hornblass A. Ptosis and pseudoptosis and blepharoplasty. Clin Plast Surg. 1981;8:811–830. [PubMed] [Google Scholar]
- Airiani S, Braunstein R E, Kazim M, Schrier A, Auran J D, Srinivasan B D. Tegaderm transparent dressing (3M) for the treatment of chronic exposure keratopathy. Ophthalmic Plast Reconstr Surg. 2003;19:75–76. doi: 10.1097/00002341-200301000-00010. [DOI] [PubMed] [Google Scholar]
- Chavez M, Putterman A M, Pak J. Tegaderm transparent dressing (3M) for the treatment of chronic exposure keratopathy “Letter”. Ophthal Plast Reconstr Surg. 2006;22:236. doi: 10.1097/01.iop.0000217707.74251.cb. [DOI] [PubMed] [Google Scholar]
- McGraw M D, Adamson P A. Postblepharoplasty ectropion: prevention and management. Arch Otolaryngol Head Neck Surg. 1991;117:852–856. doi: 10.1001/archotol.1991.01870200046006. [DOI] [PubMed] [Google Scholar]
- Carraway J H, Mellow C G. The prevention and treatment of lower lid ectropion following blepharoplasty. Plast Reconstr Surg. 1990;85:971–981. doi: 10.1097/00006534-199006000-00025. [DOI] [PubMed] [Google Scholar]
- Wilkins R B, Byrd W A. Complications of blepharoplasty. Ophthal Plast Reconstr Surg. 1985;1:195–198. doi: 10.1097/00002341-198501030-00007. [DOI] [PubMed] [Google Scholar]
- Shorr N, Fallor M K. “Madame Butterfly” procedure: combined cheek and lateral canthal suspension procedure for post-blepharoplasty, “round eye,” and lower eyelid retraction. Ophthal Plast Reconstr Surg. 1985;1:229–235. [PubMed] [Google Scholar]
- Patipa M. The evaluation and management of lower eyelid retraction following cosmetic surgery. Plast Reconstr Surg. 2000;106:438–453. doi: 10.1097/00006534-200008000-00033. [DOI] [PubMed] [Google Scholar]
- Patel B CK, Patipa M, Anderson R L, McLeish W. Management of postblepharoplasty lower eyelid retraction with hard palate grafts and lateral tarsal strip. Plast Reconstr Surg. 1997;99:1251–1260. doi: 10.1097/00006534-199704001-00007. [DOI] [PubMed] [Google Scholar]
- McCord C D, Jr, Ellis D S. The correction of lower lid malposition following lower lid blepharoplasty. Plast Reconstr Surg. 1993;92:1068–1072. doi: 10.1097/00006534-199311000-00011. [DOI] [PubMed] [Google Scholar]
- Lisman R D, Hyde K, Smith B. Complications of blepharoplasty. Clin Plast Surg. 1988;15:309–335. [PubMed] [Google Scholar]
- Levine M R, Davies R, Ross J. Chemosis following blepharoplasty: an unusual complication. Ophthalmic Surg. 1994;25:593–596. [PubMed] [Google Scholar]
- Enzer Y R, Shorr N. Medical and surgical management of chemosis after blepharoplasty. Ophthal Plast Reconstr Surg. 1994;10:57–63. doi: 10.1097/00002341-199403000-00012. [DOI] [PubMed] [Google Scholar]
- Alfonso E, Levada A J, Flynn J T. Inferior rectus paresis after secondary blepharoplasty. Br J Ophthalmol. 1984;68:535–537. doi: 10.1136/bjo.68.8.535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayworth R S, Lisman R D, Muchnick R S, Smith B. Diplopia following blepharoplasty. Ann Ophthalmol. 1984;16:448–451. [PubMed] [Google Scholar]
- Harley R D, Nelson L B, Flanagan J C, Calhoun J H. Ocular motility disturbances following cosmetic blepharoplasty. Arch Ophthalmol. 1986;104:542–544. doi: 10.1001/archopht.1986.01050160098021. [DOI] [PubMed] [Google Scholar]
- Baylis H I, Long J A, Groth M J. Transconjunctival lower eyelid blepharoplasty: technique and complications. Ophthalmology. 1989;96:1027–1032. doi: 10.1016/s0161-6420(89)32787-4. [DOI] [PubMed] [Google Scholar]
- Ghabrial R, Lisman R D, Kane M A, Milite J, Richards R. Diplopia following transconjunctival blepharoplasty. Plast Reconstr Surg. 1998;102:1219–1225. doi: 10.1097/00006534-199809040-00049. [DOI] [PubMed] [Google Scholar]
- Syniuta L A, Goldberg R A, Thacker N M, Rosenbaum A L. Acquired strabismus following cosmetic blepharoplasty. Plast Reconstr Surg. 2003;111:2053–2059. doi: 10.1097/01.PRS.0000056840.61348.35. [DOI] [PubMed] [Google Scholar]
- Levine M R, Boynton J, Tenzel R R, Miller G R. Complications of blepharoplasty. Ophthalmic Surg. 1975;6:53–57. [PubMed] [Google Scholar]
- Wesley R E, Pollard Z F, McCord C D., Jr Superior oblique paresis after blepharoplasty. Plast Reconstr Surg. 1980;66:283–286. doi: 10.1097/00006534-198008000-00020. [DOI] [PubMed] [Google Scholar]
- Neely K A, Ernest J T, Mottier M. Combined superior oblique paresis and Brown's syndrome after blepharoplasty. Am J Ophthalmol. 1990;109:347–349. doi: 10.1016/s0002-9394(14)74565-9. (letter) [DOI] [PubMed] [Google Scholar]
- Jordan D R, Anderson R L, Thiese S M. Avoiding inferior oblique injury during lower blepharoplasty. Arch Ophthalmol. 1989;107:1382–1383. doi: 10.1001/archopht.1989.01070020452053. [DOI] [PubMed] [Google Scholar]
- Patrinely J R, Marines H M, Anderson R L. Skin flaps in periorbital reconstruction. Surv Ophthalmol. 1987;31:249–261. doi: 10.1016/0039-6257(87)90024-5. [DOI] [PubMed] [Google Scholar]
- Jordan D R, Anderson R L. Epicanthal folds: a deep tissue approach. Arch Ophthalmol. 1989;107:1532–1535. doi: 10.1001/archopht.1989.01070020606050. [DOI] [PubMed] [Google Scholar]
- Yen M T, Jordan D R, Anderson R L. No-scar Asian epicanthoplasty. Ophthal Plast Reconstr Surg. 2002;18:40–44. doi: 10.1097/00002341-200201000-00006. [DOI] [PubMed] [Google Scholar]
- Scott K R, Tse D T, Kronish J W. Vertically oriented upper eyelid nerves: a clinical, anatomical and immunohistochemical study. Ophthalmology. 1992;99:222–226. doi: 10.1016/s0161-6420(92)31989-x. [DOI] [PubMed] [Google Scholar]
- Black E H, Gladstone G J, Nesi F A. Eyelid sensation after supratarsal lid crease incision. Ophthal Plast Reconstr Surg. 2002;18:45–49. doi: 10.1097/00002341-200201000-00007. [DOI] [PubMed] [Google Scholar]
- Aszmann O C, Muse V, Dellon A L. Evidence in support of collateral sprouting after sensory nerve resection. Ann Plast Surg. 1996;37:520–525. doi: 10.1097/00000637-199611000-00011. [DOI] [PubMed] [Google Scholar]
- Aiache A E, Messler G. Perisuture capsular contraction. Plast Reconstr Surg. 2001;107:1613–1614. [PubMed] [Google Scholar]
- Soll S M, Lisman R D, Charles N C, Palu R N. Pyogenic granuloma after transconjunctival blepharoplasty: a case report. Ophthal Plast Reconstr Surg. 1993;9:298–301. doi: 10.1097/00002341-199312000-00013. [DOI] [PubMed] [Google Scholar]
- Fryer R H, Reinke K R. Pyogenic granuloma: a complication of transconjunctival incisions. Plast Reconstr Surg. 2000;105:1565–1566. doi: 10.1097/00006534-200004040-00056. [DOI] [PubMed] [Google Scholar]