ABSTRACT
The relatively new concept and technique of microvascular joint transplantation for the correction of the congenitally deformed wrist is presented with a series of 24 operated radial club hands. The results from the 19 upper extremities with a mean follow-up of 11 years show that the new technique will not diminish the longitudinal growth of the ulna. The ulna length in the series is now 15.4 cm in mean and will develop further and presumably better than that reported in the previous long-term studies after centralization. The superiority in wrist active mobility compared with those of some previous long-term studies is reported with total active motion of 83 degrees in mean. The radial deviation deformity has become increased by 12 degrees in mean in the long-term follow-up compared with the results reported previously by the same author in the series of the first nine patients in 1998. The balance in the growth between the supporting metatarsal joint and the distal ulna has remained satisfactory, and the resting radial deviation angle is 28 degrees in mean (range, 0 to 45 degrees) in the cases with successful joint transfer. A subluxation tendency in six of the transplanted joints is a new finding, and its prevention needs careful attention during the reconstruction. With respect to timing, the joint alignment and transplantation procedure is best performed between the ages of 2.5 and 4 years according to the current experience of the author. A pollicization is usually added after the wrist alignment procedure. This technique will give the child a period of ~10 years without any new need for surgical treatment, and usually no splinting is needed during that period. However, an additional corrective osteotomy may be needed at early puberty depending on the growth properties of the joint graft and original ulna and because of ulnar bowing. The reported technique with preoperative and postoperative measures takes a period of about one-half year, and the whole procedure is considered quite demanding as far as an adequate preoperative soft tissue distraction and the microvascular joint transplantation are concerned. It is recommended that the treatment be performed in dedicated microsurgical centers with adequate pediatric tissue transfer experience.
Keywords: Congenital hand deformity, radial aplasia, toe-to-hand transplantation, joint transplantation, microsurgery
The congenital absence of the radius, or radial club hand, is a relatively rare congenital upper-extremity abnormality typically appearing with hypoplasia or lack of the radius and also a lack of a functional thumb in most cases. Radial club hands do vary from a mild degree of hypoplasia to complete absence of the radius, and sometimes defects at the proximal humerus and associated musculature may be found. There are often severe combined syndromes, and multiple organ systems or anatomic structures may be affected. The treatment of radial club hand has traditionally been a variant of centralization,1,2 and it has recently been combined with a preoperative soft tissue distraction3,4 to enhance the operative procedures. During the past 30 years, a few attempts at reconstruction have been made using a vascularized fibula to replace the missing radius. With the aid of advanced microsurgical techniques, which were developed together with toe-to-hand transplantation surgery for congenital finger defects,5 a vascularized second-toe metatarsophalangeal (MTP-II) joint transplantation6 was introduced by the author in 1992 as a treatment option for stabilizing the radially deviating hand. The current article aims to summarize the experiences from this new treatment alternative and give the guidelines of our current technique. Also, an attempt is made to correlate the results with the severity of the defect, which is really very variable. This may give a base for further modified classification of the severity of the radial club hand.
PATIENTS AND METHODS
The operative treatment principle used, stabilization of the hand into corrected position with a vascularized MTP-II joint graft, was developed in 1987, when the first patient in the series was operated on. The use of preoperative distraction was started with the second patient, and the results and a detailed technique7 was published in 1998 with 5.5 years of follow-up of the first nine patients.8 Until now, we have continued to use the same technique and tried to improve the details of our treatment. The understanding of the disease itself and the limits and benefits of the technique used have increased during the 20-year period. The current material consists of 24 operatively treated radial club hands in 22 patients and the follow-up study with 19 treated hands in 18 patients, with a minimum follow-up of more than 4 years and with mean 11 years of follow-up. There have been two patients with Thrombocytenia Absent Radius syndrome (TAR) and two patients with a special (RAPALIDINO) syndrome characterized by absence of Radius, patellae, and short body height. Additional features include diarrhea tendency in childhood and normal intelligence.9 Two of the patients have a Goldenhar syndrome. A (VATER) syndrome characterized by vertebral defects, analatresia, tracheoesophageal fistula and esophageal atresia and radial dysplasia has been diagnosed in five patients. A useful thumb has originally been present in 4 hands, a pollicization has been performed in 12 hands, and 8 of the hands are still without a thumb for various reasons. According to Bayne and Klug classification,10 which is based only on bone defect at radius, we had 21 type-4 hands and 3 type-3 hands when the treatment was begun. This classification does not correlate with the function or quality of different hands. It would be more useful to observe the mobility or contractures of the finger joints, radial wrist and forearm tissue tightness, and the specific lack of extensor or radial musculature, which also may vary quite extensively. In addition to criticism, it was noticed that many previously totally absent radius bones became partially visible at the proximal third area at the time of the follow-up. This change was visible clearly in three forearms, and a tiny portion of radial head was visible in four additional cases. Therefore a proposal to classify the patients into different difficulty categories has been done with respect to bone defect, defective finger function, wrist deformity, and other musculoskeletal defects and malfunctions of the affected extremity (Table 1). Depending on the severity of the disease, also the success with the different attempts at early primary conservative management of the wrist deformity has been variable, and this may have influenced to the possibilities of the full correction of the deformity.
Table 1.
The Patients and Their Severity Grades in the Series
| Patients (9 Girls, 13 Boys) |
Affected Hand |
Severity Grade |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Hand No./Sex | Diagnosed Syndrome | Bone (Bayne Type) | Fingers |
Wrist Tightness (Radial Deviation) | Hand (Grades 1 to 8) | Wrist (Grades 1 to 4) | Other (Grades 0 to 3) | RCH Severity Score (Maximum Score 15) |
Opposite Hand | |||
| MCP Joint Stiffness (Flexion Defect) |
PIP Joint Camptodactyly (Extension Lag) |
Severe |
Moderate |
Mild |
||||||||
| > 10 | 6 to 9 | > 5 | ||||||||||
| Patients | ||||||||||||
| now = Bayne type changed at follow-up. | ||||||||||||
| Affected Hand and evaluation criteria: | ||||||||||||
| MCP:+for each finger with a flexion ability < 45 degrees. | ||||||||||||
| PIP:+for each finger with a camptodactyly and extension lag > 20 degrees. | ||||||||||||
| Tightness of the wrist when pulled gently into extension:+for each starting 30 degrees of radial deviation, or+(0–30 degrees),++(30–60 degrees),+++(60–90 degrees),++++ (> 90 degrees radial deviation). | ||||||||||||
| release = release of tight structures done at the start of distraction. | ||||||||||||
| post c = status post centralization. | ||||||||||||
| dx, dexter (right); sin, sinister (left); MCP, metacarpophalangeal; PIP, proximal interphalangeal. | ||||||||||||
| Severity Grade | ||||||||||||
| 1 point for each: elbow flexion defect or weak; elbow extension defect > 20 degrees; shoulder abduction defect; shoulder flexion defect. | ||||||||||||
| Other: O = severity of the functional defect at elbow or shoulder. | ||||||||||||
| n = the number of hands belonging to each group. | ||||||||||||
| 1/M | 4 | +++ | ++ | ++++ release | 5 | 4 | 1 | 10 | RCH type 4 (nontreated) | |||
| 2/M | VATER | 4 (now 3) | + | ++ | ++ | 3 | 2 | 1 | 6 | Thumb hypoplasia grade 2 | ||
| 3/M | TAR | 4 | ++++ | ++ | ++++ release | 6 | 4 | 2 | 12 | RCH type 4 (centralized) | ||
| 4/M | VATER | 4 (now 3* ) | + | ++ | ++ | 3 | 2 | 0 | 5 | Unstable, original duplicate thumb | ||
| 5/F | 4 (now 3*) | ++ | - | ++ | 2 | 2 | 0 | 4 | Thumb hypoplasia grade 1 | |||
| 6/F dx* | TAR | 4 | ++ | - | +++ | 2 | 3 | 1 | 6 | RCH type 4 = hand no. 8 | ||
| 7/M | 4 (now 3) | ++ | + | ++ | 3 | 2 | 1 | 6 | Thumb hypoplasia grade 3A | |||
| 8/F sin* | TAR | 4 | ++ | - | +++ | 2 | 3 | 2 | 7 | RCH type 4 = hand no. 6 | ||
| 9/F | RAPALIDINO | 4 | +++ | ++ | +++ | 5 | 3 | 2 | 10 | RCH type 4 (nontreated) | ||
| 10/F | 4 (now 3*) | +++ | ++ | +++ | 5 | 3 | 1 | 9 | Thumb hypoplasia grade 3a | |||
| 11/M | 4 | ++ | - | ++post c | 2 | 2 | 0 | 4 | RCH type 4 (post c) no thumb (pollicization) | |||
| 12/M | VATER | 3 | + | - | +++release | 1 | 3 | 0 | 4 | Thumb hypoplasia grade 1 | ||
| 13/M | VATER | 4 | + | - | ++ | 1 | 2 | 0 | 3 | Thumb hypoplasia grade 1 | ||
| 14/F | Goldenhar | 4 | ++ | ++ | ++ | 4 | 2 | 0 | 6 | Thumb hypoplasia grade 2 | ||
| 15/M | Goldenhar | 4 (now 3) | ++ | ++ | ++ | 4 | 2 | 1 | 7 | Thumb hypoplasia grade 1 | ||
| 16/F | 4 (now 3*) | ++ | - | + | 2 | 1 | 0 | 3 | Thumb hypoplasia grade 3b | |||
| 17/M | VATER | 4 | ++++ | +++ | ++++ release | 7 | 4 | 2 | 13 | RCH type 4 (nontreated) | ||
| 18/F | RAPALIDINO | 4 | +++ | - | +++release | 3 | 3 | 1 | 7 | RCH type 2 (nontreated) | ||
| 19/F | 3 | ++ | - | ++ | 2 | 2 | 0 | 4 | Thumb missing | |||
| 20/M dx** | 4 | +++ | +++ | +++ | 6 | 3 | 2 | 11 | RCH type 4 = hand no. 22 | |||
| 21/M | 3 | + | - | ++ | 1 | 2 | 0 | 3 | Normal | |||
| 22/M sin** | 4 | +++ | +++ | +++release | 6 | 3 | 2 | 11 | RCH type 4 = hand no. 20 | |||
| 23/M | 4 | ++ | - | + | 2 | 1 | 0 | 3 | Thumb hypoplasia grade 1 | |||
| 24/F | 4 | ++ | ++ | +++ | 4 | 3 | 0 | 7 | Thumb hypoplasia grade 1 | |||
| n = 6 | 9 | 9 | ||||||||||
Hand 6 = the right and hand 8 = the left of a patient treated bilaterally.
Hand 20 = the right and hand 22 = the left of another patient treated bilaterally.
= very small proximal bone remnant (indicates that the Bayne type has changed but the visible proximal radius is a very small bone piece, less than 1 cm).
OPERATIONS
Historically, the idea of stabilizing the radially deviating hand with a bone graft and forming a Y-form distal ulna was presented in 1928 by Albee11 using simple tibial bone grafts, and in 1945 Starr12 did use preoperative 6 weeks skeletal traction for hand alignment correction followed by a nonvascularized fibula graft. During the microsurgery era, there have been some reports of using vascularized fibula graft13,14 in similar fashion. Experimental studies by Nettelblad15 and later by Bowen16 confirm that epiphyseal growth may be possible after microvascular transfer of the growing bone. However, a conventional centralization4 or its variant has continued to be the main operative procedure by most present-day authors despite the reported partly unsatisfactory results.17,18,19 The current method using a microvascular MTP-II joint for correcting the wrist deformity was first used by the author in 1987. The detailed technique7 was published in 1998, and the results of preliminary series8 were introduced during the same year. The aim is first to use a gradual soft tissue distraction for proper hand alignment and then after the correction to insert a microvascular MTP-II joint graft for permanent support and with the ability to grow. This means that the radial half of the wrist joint is reconstructed with a complete MTP-II joint aiming at improved wrist motion compared with the mobility that is possible after centralization. The physis in the metatarsal joint remains growing, and the alignment of the hand during the growth period is dependent on the balanced growth rate of the Y-fork, which is formed by the hypertrophied metatarsal bone and the distal ulna. The experiences achieved in the treatment of 24 radial club hands are presented with technical refinements and with the contemporary and partly long-term results from the “experimental series.” This treatment concept will demand a meticulous microsurgical approach and a donation of one toe with metatarsal bone from the foot.
Indications and Timing
In a newborn baby with the radial club hand, a careful splinting is always a primary treatment, and it should be started from day 1 after the birth and continued meticulously trying to improve the hand alignment and wrist mobility. In addition, the early treatment should be associated with regular gentle manipulative measures by the parents. The radial deviation will become quickly more difficult to treat when these measures have not been started early or the started splinting is discontinued. The current method to treat a radial club hand is considered suitable for the Bayne grade 3 and 4 defects. In grade 2, when the radius is only hypoplastic, the deformity is usually not progressive. Often such a short radius may be treated with conservative observation and with meticulous and continuous splinting. In some severe cases, the radial deviation of the wrist may need correction with a bone lengthening of the hypoplastic radius. In types 3 and 4, there is no support of the radius at all, and the hand will deform and deviate to radial direction very severely (Fig. 1) and operative treatment in most cases is considered necessary. The presented method is also useful after attempted centralization with moderate or severe recurrence.
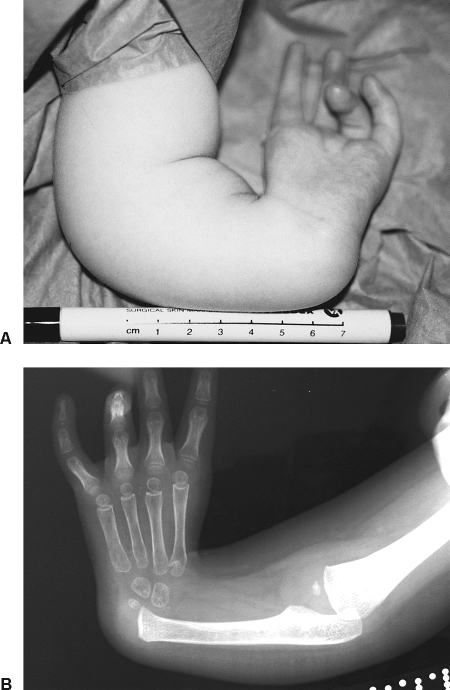
Figure 1.
(A) Preoperative view of the hand of a girl at the age of 3 years 5 months (hand no. 14). (B) Preoperative radiograph of the same patient before distraction.
The timing for operative treatment of the radial club hand has traditionally been at about 1 year of age in conventional centralization or radialization. These more or less aggressive surgical procedures near the distal ulna epiphysis may have drawbacks and they may be harmful to the longitudinal forearm growth. The radial club hand treatment should be aimed to allow maximal forearm length by natural ulna growth. The timing for difficult reconstructive surgery can be postponed and may be more successful in a 2- to 3-year-old child. At that age, especially after adequate splinting, the necessary hand alignment can be achieved using modern soft tissue distraction techniques combined only in most severe cases with a suitable release of the tight radial structures. At this age, the hand bones are stronger for distraction purposes, and the microvascular part of the operation is clearly easier. Also, necessary tendinous stabilization of the new joint may be performed with better precision. The pollicization, which clearly improves the overall function, can usually be done after wrist correction, when the starting pinching pattern is situated between index and middle fingers. When the starting pinching pattern is between small and ring fingers, the pollicization should be done early and even before the wrist correction. When there is a pattern to use the index finger as a thumb, the recommended age for microvascular joint transplantation is between 2.5 and 4 years.
Soft Tissue Distraction and Optional Release
When the alignment of the wrist can be achieved relatively easily, there is no need for the release at first stage. A preoperative x-ray with a trial to align the wrist with pulling from the fingers will give guidelines about its necessity. Also, a clear clinical tightness may dictate its need. However, it is rarely needed in conservatively well-treated cases. Unnecessary scar from the dissection at the radial aspect of the wrist may also add difficulties during the main procedure later on. If the release is considered necessary, it is done trough a transverse incision cutting all parts of the scarred remnants of the radial wrist extensors and flexors together with the release of capsular tightness. All tendons moving the fingers must be left intact. This must be a delicate and atraumatic procedure keeping in mind the necessary vessels and nerves for the later actual joint transplantation.
The soft tissue distraction, to align the hand with the forearm, needs careful planning, a strong lightweight lengthening device, frequent controls, and proper education of the parents. We have used the unilateral Hammer distraction device (Swemac Orthopaedics AB, Linköping, Sweden) (Fig. 2) from the beginning of the series and adopted a technique to place it on the dorsoulnar aspect of the wrist and forearm. The children will adapt very well with the distractor, and use of the hand during normal playing activities has not been much disturbed even during the long-time use of the external fixator. This fixator position will allow full access to the operative field during the second phase of the reconstructive procedure without the need to remove it because the external fixator is considered necessary during the healing period. When the fixator device is assembled, the final pro-supination position of the hand will be determined. The pins for the metacarpals need to be provided with slow or dense thread, and the length of the penetrating tip part should be ~10 mm. Usually, two of three distal pins become inserted into the second metacarpal bone and one of the pins into the third metacarpal bone because the base of the second metacarpal bone must be left untouched for later bone osteosynthesis. These bones are the most stable part of the hand. The second metacarpal will become discarded from its diaphyseal part during the later pollicization, and the possible pin infections do less harm to the rest of the hand bones and extensor tendons using these pin positions. When the procedure is done after pollicization, then the third and fourth metacarpals are used for distal fixation. The proximal pins are usually easy to apply on the dorsoulnar aspect of the proximal ulna. The thread part of the pins must be clearly longer for proximal ulna or minimum of 15 mm, and they will be placed just distal from the elbow joint area. The longitudinal bar must be parallel with the ulna, and in a severely deviating hand situation, the lengthening bar should deviate ~10 to 15 degrees to the ulnar direction. The amount of necessary soft tissue distraction is ~25 mm in mean after primary manual correction during the external fixation distractor assembly. This means a 45- to 50-day distraction period before the second part of the reconstruction can be performed. The soft tissue distraction is always a time-consuming procedure. Not more than 0.5 mm per day can be recommended. There is clear evidence that the physeal detachment and the ischemia of the forearm muscles will occur with higher distraction speeds.20,21,22 The parents must understand, perform, and monitor (according to detailed written schedule) the lengthening procedure, and radiologic controls for its progress are necessary after about every 10 mm of distraction. The aim is to get the best possible alignment of the hand and to create the necessary place between the base of the second metacarpal and the radiologically visible distal ulna. The MTP joint transplant used will need ~45 to 50 mm of space between the base of the second metacarpal and the distal radiologically visible ulna bone (Fig. 3) at the age of 3 years.23,24
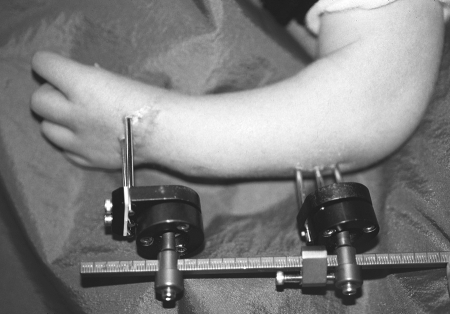
Figure 2.
Soft tissue distraction in progress (hand no. 14) . The Hammer distraction device is lightweight and it weighs ~120 g with 6 pins. The ball joints allow easy assembling.
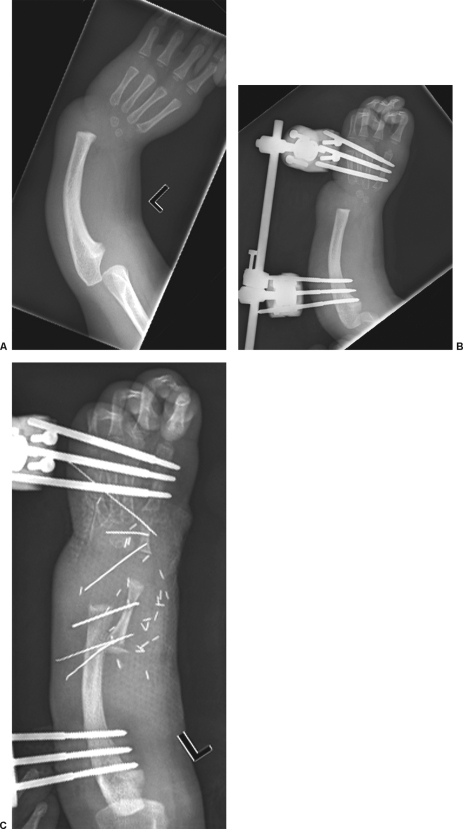
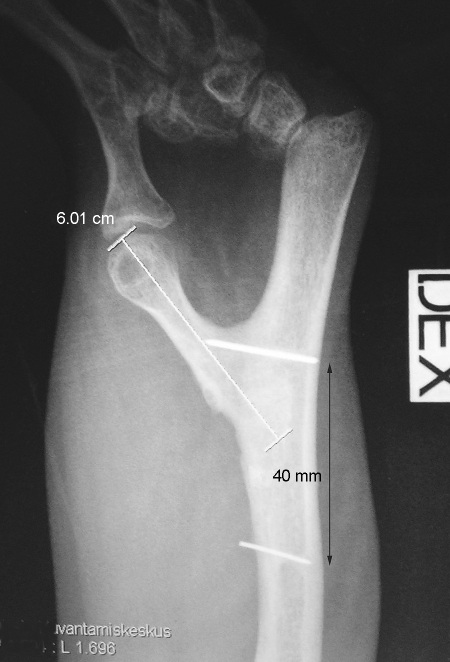
Figure 3.
Radiographs of a recently operated hand (no. 23). (A) The patient is a 2.5-year-old boy. The principle of the treatment is first to do a slow soft tissue distraction with a pace of 0.5 mm/day. (B) When a good alignment has been achieved, (C) a microvascular MTP-II joint graft is performed to provide radial stability. The amount of distraction is 20.5 mm. The graft length is 45 mm.
Microvascular Joint Transplantation
A two-team approach is used: one team experienced in the dissection of a microvascular toe transplant and the other team experienced in the anatomy of the radial club hand with its peculiarities.25
TAKING A TOE
The ipsilateral second toe with the full length of its metatarsal bone is used. The preferred arteries with the metatarsal are II/III plantar metatarsal artery (PMTA) and I/II dorsal metatarsal artery (DMTA), which come from the plantar arch (Fig. 4) formed by the dorsalis pedis and the posterior tibial arteries. In our series, we have mainly used separately these short metatarsal arteries, but it may be practical to continue dissection proximally to the dorsalis pedis artery and to take a part of the plantar arch with both previously mentioned vessels to get a sound and longer pedicle. This is needed when an end-to-side anastomosis with a single ulnar forearm artery is necessary. Otherwise a vein graft may be needed. The vein system is taken as in a conventional toe-to-hand transfer. The transplant is taken with all extensor and flexor tendons including the dorsal nerves serving the skin at the dorsal aspect of the MTP-II joint. The further preparation of the joint graft includes amputation of the distal and middle phalanges. At this point, the distal flexor tendon insertions will become detached, and the long flexor tendon is therefore looped around the strong tendon sheet of the proximal phalanx. It is sutured to itself to form a new insertion for flexor side muscle attachment. The extensor tendon will remain an original attachment at the dorsum of the proximal phalanx for the dorsal joint control. The skin included to the graft is incised and opened from the fibular aspect of the transplant and then carefully filleted to form radial (tibial) side coverage during the reconstruction. All this preparation can be done leaving the toe hanging only on the arterial and venous pedicles.
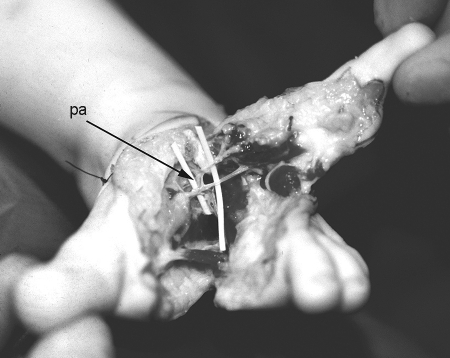
Figure 4.
The second-toe ray is completely removed. The II/III PMTA and I/II DMTA are visualized when they leave the arterial plantar arch (pa).
THE WRIST PREPARATION AND THE RELEASE OF TIGHT RADIAL STRUCTURES
The arteries are localized preoperatively with Doppler ultrasound and marked before operation. The distractor frame or ex-fix is always kept in place during the whole procedure and continued afterwards during the healing period until good bone healing occurs at both poles of the graft.
A longitudinal incision on the radial aspect of the wrist is used. Also, a transverse incision is added distally at the wrist crease both dorsally and volarly. Large triangular flaps are raised. Tight fascia is completely removed from the radial distal forearm. The necessary donor structures for microvascular transplantation are first identified. A good cephalic vein is usually available; the hypoplastic radial artery (Fig. 5) may be present under the big radial branch of the median nerve. When needed, the ulnar artery is identified, and a vessel loop is used for marking. The release of tight radial structures is done starting near the cartilaginous wrist bones, and a good rule is to detach and cut everything that is not moving the fingers. Only the essential nerves and vessel structures and the tendons (extensors and flexors) moving the fingers are preserved. The tight structures may include remnants of the brachioradialis, flexor carpi radialis (FCR) group, and extensor carpi radialis (ECR) tendons and muscles. This structure is divided into dorsal and volar parts (Fig. 5), and there should be functioning muscle elements available, which can be transferred for joint stabilization and to help control the wrist mobility. After the complete release, a 1- to 2-mm soft tissue distraction may be added to maximize the corrected hand position. The distal ulnar physis remains untouched, and its position is only identified with an injection needle. The needle is placed to determine the correct fixation point for the metatarsal graft at the radiologically visible distal ulna. Another needle is used to confirm the base of the second metacarpal. At this stage, an intraoperative x-ray control is mandatory to confirm the correct positions of these needles before further preparation. The base of the second metatarsal is freshened, and in cases when there exists a scaphoid cartilage, it can be partly carved for proximal phalanx accommodation and to ensure the best possible position of the joint. Then the distal ulna 5 to 10 mm proximally to the physeal plate is opened with an osteotome and a one-third thickness of the ulna as a 15- to 20-mm-long bone flap is turned radially to form a good platform for the metatarsal portion of the graft. Special care is taken with TAR syndrome patients with a good thumb. Preoperative magnetic resonance imaging (MRI) is recommended to figure out the presence of all cartilaginous parts of the wrist. There may be a small remaining portion of distal radius present, and that may change the positioning of the graft to a more proximal level. In hands no. 6 and no. 8, a TAR patient with bilateral situation had a tiny cartilage proximal to the scaphoid. The joint grafts were attached to this cartilage. At late follow-up, the radiograph demonstrated respectively 16-mm and 18-mm broad radius fragments. She has a good range of motion in her “original wrist joints” despite that hand no. 8 was a failure and the joint was fused at age 15.
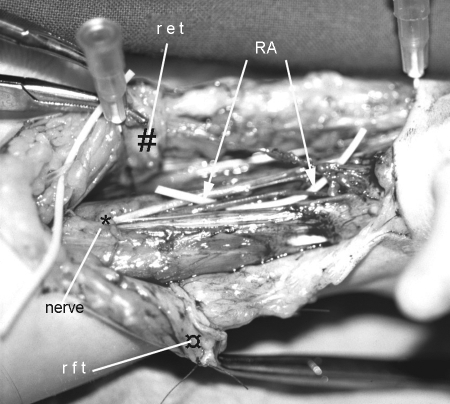
Figure 5.
Exposure of the radial aspect of the wrist under distraction. The radial branch from median nerve is a useful landmark. Hypoplastic radial artery (RA) is under the nerve branching area (*). ret (#) = released portion of tight extensor tendon remnants; rft (¤) = released portion of tight flexor tendon remnants. Two marking needles ~45 mm apart are used to locate the correct bone landmarks under fluoroscopy; right needle at second metacarpal base, left needle at the junction of distal ulna and the physis.
RECONSTRUCTION
After 30 minutes of recirculation in the prepared toe-joint transplant, it is detached from the feeding vessels, and the wrist reconstruction can be started. The graft is placed into its new location created by extensive tissue release. The alignment of the joint is crucial, and the stability of the joint is better in 15- to 20-degree flexion. A hyperextended position will endanger the later stability. The alignment of the bone parts should be as parallel as possible with the ulna, and no deviation is allowed at the joint itself. Usually, three thin (0.6 mm) K-wires are used for both bone parts to ensure the necessary position in posteroanterior view (Fig. 3C). They are drilled to the opposite side of the forearm, where they can be left visible and easily removed after a healing period. X-ray control is mandatory at that stage for proper alignment of the graft. Tendon transfers for additional joint stability are important. The previously identified remnants of the radial wrist extensors and flexors (Fig. 5) are transferred to the prepared extensor and flexor tendons of the joint transplant. This is necessary for later joint stability and for the control of the wrist mobility. In some cases, these two separate motor units may be very hypoplastic and difficult to find. The dynamic active tendon functions and a mild flexion position of the MTP joint may play an important role for the long-lasting stability at the new transplanted joint.
MICROSURGICAL CONNECTIONS
The best possible feeding artery should be used. When there is a single ulnar artery, then an end-to-side anastomosis is done with a long arterial pedicle or a reversed vein graft from the distal cephalic vein is first connected with an end-to-side anastomosis into ulnar artery and the other end is connected into the II/III PMTA. When hypoplastic radial artery is used, it should be cut very distally. Because of a gradual distraction, there seems to be added tension in the artery wall, and when this elastic structure is cut, it will become pulled back to a more proximal position, and difficulties with an increased suture line tension may arise from this reason. A microvascular anastomosis is done between the proximal cut end of hypoplastic radial artery and II/III PMTA. The I/II DMTA can be more easily connected to the distal cut end of hypoplastic radial artery or additionally connected to a branch of the ulnar artery or an end-to-side anastomosis is performed directly with the ulnar artery. The vein of the joint graft is connected to the cephalic vein of the forearm. One third of the radial branch of the median nerve is used for neurotization of the dorsal graft nerves. The wound closure is done gently using the toe-fillet flap, which covers the joint area from the radial side. A small area of split skin graft may additionally be needed. The pulpa area of the toe-skin is usually discarded, and the dorsal type skin is preferred. If needed, this red-colored pulpar skin can also be used for skin coverage and removed later at the time of pollicization.
AFTER-CARE
The child is kept in intensive care observation until the circulation is stabilized and the healing of the tissues has started. A personal nurse is considered mandatory during the first week for prevention of unnecessary complications. The donor foot is immobilized with a plaster cast for 4 weeks, but walking with the plaster cast is encouraged after 1 week postoperatively. A long-term prophylactic antibacterial treatment and careful pin-tract care are essential for success with the long-term use of ex-fix. The dynamization of the fixator is never recommended in small children because the pins are already very loose after the long period of treatment, and the fixator will drop off if the tension is diminished. The ex-fix is removed after bone healing, usually after 9 weeks, and then the new wrist is protected with a long-arm plaster cast for an additional month. The protection of the joint is continued with a splint made by an occupational therapist during 2 more months, and free-hand use is allowed only after 5 months from the reconstructive joint transplantation.
COMPLICATIONS (TABLE 2)
Table 2.
Operative Treatment and Early After-Care, Complications, and Secondary Operations
| Hand no./Sex (9 Girls, 13 Boys) | Preoperative Distraction |
Age at Operation 2 (Months) | Postoperative Treatment |
Complications | Primary Vascular Reoperation | Secondary Operations | Age at Pollicization (Months) | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age at Start (Months) | Ulna Length (mm) | Distraction | Ex-fix | Plaster | Splint | |||||||
| Speed (mm/Day in mean) | Distance (mm) (Mean, 27 mm) | (Weeks) | (Weeks) | (Weeks) | ||||||||
| dx = dexter (right) | ||||||||||||
| sin = sinister (left) | ||||||||||||
| PP = proximal phalanx | ||||||||||||
| MC = metacarpal II | ||||||||||||
| thumb+ =thumb existing (no need for pollicization) | ||||||||||||
| 1/M | 68 | 103 | - | - | 68 | 5 | 3 | 4 | - | - | Joint transport at age 10 | - |
| 2/M | 12 | 66 | 0.9 | 18 | 13 | 11 | 3 | 4 | Delayed healing joint wound, split skin graft | - | 48 | |
| 3/M | 166 | 150 | 0.9 | 50 | 168 | 9 | 2 | 4 | Arterial spasm at end-to-side junction | + | Thumb+ | |
| 4/M | 20 | 66 | 1 | 28 | 21 | 5 | 2 | 3 | Fracture MTP joint 2 months postoperatively; MT head necrosis | - | Joint transport at age 11 | 48 |
| 5/F | 13 | 63 | 0.9 | 40 | 14.5 | 8 | 4 | 3 | - | - | Bowed ulna osteotomy at age 16 | 36 |
| 6/F dx* | 21 | 63 | 0.8 | 24 | 22 | 6 | 5 | 4 | - | - | Thumb+ | |
| 7/M | 18 | 65 | 0.8 | 26 | 20 | 9 | 5 | 4 | Pseudarthrosis PP/MC, radial instability | - | 60 | |
| 8/F sin* | 34 | 85 | 0.8 | 26 | 35 | 10 | 4 | 6 | Arterial failure, MTP joint fragmentation | + | Bone graft stabilization at age 16 | Thumb+ |
| 9/F | 50 | 85 | 0.7 | 35 | 52 | 8 | 4 | 8 | Arterial failure and skin flap loss | + | - | |
| 10/F | 25 | 80 | 0.9 | 32 | 27 | 9 | 5 | 8 | Pseudarthrosis PP/MC | - | Joint transport at age 4 | Thumb+ |
| 11/M | 73 | 84 | 1 | 21 | 75 | 12 | 5 | 8 | - | - | - | |
| 12/M | 28 | 80 | 0.6 | 32 | 30 | 7 | 5 | 8 | - | - | 46 | |
| 13/M | 15 | 66 | 0.5 | 20 | 16 | 7 | 6 | 6 | Ex-fix dropped off and reassembled | - | Bowed ulna osteotomy at age 11 | 30 |
| 14/F | 39 | 73 | 0.5 | 21 | 42 | 11 | 4 | 8 | Delayed bone healing MT/ulna | - | 52 | |
| 15/M | 21 | 75 | 0.3 | 20 | 23 | 8 | 5 | 8 | Delayed bone healing MT/ulna | - | Thumb hypoplasia grade 2 | |
| 16/F | 25 | 72 | 0.5 | 25 | 27 | 11 | 5 | 8 | Fracture MT shaft | + | - | |
| 17/M | 32 | 88 | 0.5 | 29 | 33 | 14 | 5 | 8 | Arterial failure, MT head necrosis | + | - | |
| 18/F | 58 | 80 | 0.5 | 18 | 60 | 8 | 5 | 8 | - | - | 79 | |
| 19/F | 43 | 88 | 0.5 | 22 | 45 | 9 | 5 | 8 | - | - | 30 | |
| 20/M dx** | 26 | 100 | 0.6 | 30 | 28 | 5 | 5 | 8 | Severe pin-site infection, early fixator removal | - | 39 | |
| 21/M | 25 | 90 | 0.5 | 22 | 27 | 8 | 5 | 8 | - | - | 36 | |
| 22/M sin** | 50 | 120 | 0.5 | 26 | 51 | 9 | 5 | 8 | - | - | 25 | |
| 23/M | 29 | 80 | 0.5 | 20 | 30 | 10 | 5 | 9 | - | - | - | |
| 24/F | 28 | 70 | 0.5 | 30 | 29 | 9 | 4 | 10 | - | - | - | |
Hand 6 = the right and hand 8 = the left of a patient treated bilaterally.
Hand 20 = the right and hand 22 = the left of another patient treated bilaterally.
Difficulties during the soft tissue distraction are not uncommon. The preoperative distraction carries a risk of all possible complications that are related to usual external-fixator use, with pin-site infections being the most common. They may secondarily produce extensor tendon adhesions and add to metacarpophalangeal (MCP) joint stiffness. Accidents with the fixator may also happen when children play and use the hand. A good rule is to teach that nobody is allowed to touch the fingers of the hand that is under distraction. When handling the arm in ex-fix, the control of the extremity should be done by holding the device firmly from the proximal end, where the fixator pins are very stabile at the proximal ulna compared with the fixator pins at the hand metacarpals. After microvascular joint transplantation, vascular problems are possible in the beginning due to a spasm tendency from hypovolemia and long-lasting general anesthesia.26 We have experienced 3 times an arterial failure. In two failure cases (hands no. 8 and no. 17), all the bones remained and the wounds did heal secondarily, but the joints did suffer. In one case (hand no. 8), the graft became fragmented; in the other (hand no. 17), the metatarsal bone did not grow at all. In the third case (hand no. 9), only the monitoring skin was lost but the joint did survive. In two other patients (hands no. 3 and no. 16), an arterial spasm did lead to exploration, which was helpful without new anastomosis. Failures in the joint-graft alignment have been related to faults in distraction device function or to too-early removal of the external fixator without complete bone healing. There has twice been a fracture in the metatarsal part of the bone graft after the removal of the fixator, even if a plaster cast has been used regularly for an additional month after ex-fix removal. One of these fractures in earlier series (hand no. 4) did destroy the MTP joint with the growth plate, although the ex-fix was immediately reapplied. Complications in bone healing have also taken place in two hands (no. 7 and no. 10) at the distal graft connection to the second metacarpal. This will compromise the wrist stability, while an extra joint will allow the wrist to deviate, while the joint graft bends into Z-deformity like a tilting scaphoid bone during radial deviation. Long-term complications include a subluxation of the transplanted joint, which apparently is due to bad primary alignment or due to the lack of stabilizing forces by the poor or lacking radial forearm muscles. The dorsal scar at the foot donor site may be a problem if the incisions are not properly planned to avoid the need for skin grafting. Only a minimal slice of the skin from the foot should be taken, and a primary skin closure should always be possible.
RESULTS (TABLE 3)
Table 3.
The Long-term Results
| Hand No./Sex | Age (Years) | Body Height (cm) | Follow-up Time (Years) | Ulna Length (cm) | RUL (%) | Hand- Forearm Angle (Degrees) | Ulna Bowing (Degrees) | Wrist TAM (Degrees) | MTP Joint Configuration | Y-fork Balance MT ULNA (mm) | Donor Foot | Overall Result | Hand-Forearm Angle in 2007 Compared with That in 1998; Increased by (Degrees) | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| RUL (relative ulna length) in mean: cases 9, 11, and 17 omitted from calculation (special short stature or previous operation). | ||||||||||||||
| TAR = a TAR–syndrome patient. | ||||||||||||||
| 1/M | 25 | 178 | 19.5 | 19 | 66 | 45 | 0 | 70 | Okay | Joint transport | Okay | Poor | 10 | |
| 2/M | 18 | 167 | 17 | 20 | 71 | 20 | 40 | 80 | Mild subluxation | 36 | 50 | Okay | Satisfactory | 10 |
| 3/M | 30 | 179 | 16.5 | 18 | 62 | 20 | 0 | 30 | Okay | 37 | 63 | Okay | Poor | 5 |
| 4/M | 17 | 170 | 16 | 19 | 70 | 35 | 50 | 65 | Subluxed | Joint transport | Okay | Poor | 10 | |
| 5/F | 16 | 167 | 15 | 17 | 65 | 30 | 30 | 75 | Mild subluxation | 37 | 47 | Pain Occasional | Good | 20 |
| 6/F dx* | 16 | 149 | 14.5 | 15 | 60 | 35 | 0 | 90 | Okaya | TAR | Okay | Satisfactory | 10 | |
| 7/M | 15 | 150 | 13.5 | 16 | 74 | 25b | 0 | 80 | Okayb | 33 | 44 | Okay | Satisfactory | 20 |
| 8/F sin* | 16 | 149 | 13 | 14 | 56 | 25c | 15 | 90 | Fusedc | TAR | Okay | Good | -5c | |
| 9/F | 16.5 | 120 | 12 | 14 | 51 | 35 | 15 | 70 | Mild subluxation | 37 | 47 | Okay | Satisfactory | 0 |
| 10/F | 13 | 160 | 10.5 | 17 | 68 | 40 | 20 | 50 | Subluxed | Joint transport | Hallux valgus | Poor | ||
| 11/M | 15.5 | 160 | 9 | 14.5 | 45 | 15 | 20 | 75 | Okay | 48 | 40 | Scar to I | Good | |
| 12/M | 11 | 148 | 9 | 16 | 68 | 20 | 20 | 110 | Okay | 54 | 53 | Okay | Good | |
| 13/M | 9.5 | 125 | 8.5 | 13.5 | 65 | 40 | 20 | 85 | Okay | 30 | 30 | Okay | Satisfactory | |
| 14/F | 11 | 134 | 8 | 14 | 67 | 10 | 10 | 115 | Okay | 43 | 41 | Okay | Good | |
| 15/M | 9.5 | 130 | 7.5 | 14 | 67 | 30 | 30 | 90 | Okay | 35 | 31 | Okay | Satisfactory | |
| 16/F | 8.5 | 133 | 6.5 | 13.5 | 67 | 20 | 10 | 115 | Mild subluxation | 40 | 36 | Okay | Good | |
| 17/M | 8.5 | 130 | 5.5 | 15 | 78 | 65 | 0 | 80 | MT head necrosis | 27 | 40 | Okay | Poor | |
| 18/F | 10 | 108 | 5 | 10 | 49 | 0 | 30 | 110 | Okay | 40 | 35 | Scar to III | Good | |
| 19/F | 7.5 | 122 | 4 | 12 | 69 | 20 | 15 | 100 | Okay | 40 | 38 | Okay | Good | |
| Average | 14.4 | 146 | 11 | 15.4 | 67 | 28 | 17 | 83 | 36 | 42 | ||||
Hand 6 = the right and hand 8 = the left of a patient treated bilaterally.
TAR patient and the MTP joint is in proximal location. The motion comes partly from the original wrist joint.
Continuously a pseudarthrosis at the junction of proximal phalanx and the base of second metatarsal allowing an abnormal mobility to radial deviation.
The mobility at the wrist is excellent at the original wrist joint. In this TAR patient, a vascular failure did lead to joint fragmentation, but there has appeared a distal small portion of the radius. This distal radius part with the fragments of the joint graft is now fused to the MT bone. That induced a correction of the hand forearm angle with 30 degrees.
The experience in the treatment of 24 radial club hands during the period of about 20 years (June 1987 to March 2007) using the vascularized MTP joint transplantation for stabilization after wrist alignment is presented. The current results are from 19 radial club hands, where the follow-up has been more than 4 years and the follow-up times have been 11 years in mean. Three patients in the series have reached maturity. The youngest patient in this group is at the age of 7.5 years. Additionally, we have treated five radial club hands with a shorter follow-up.
Primary survival of the joint graft occurred in 22 of 24 hands. Two vascular failures occurred, and additionally one monitoring filleted toe skin was lost (case no. 9) but the joint survived. One metatarsal head was accidentally fractured in the early postoperative period. Two graft failures did lead into metatarsal (MT)-head necrosis, and one badly fractured metatarsal head did not grow at all and was also considered a necrotic MT head. There has occurred a clear hypertrophy and a variable longitudinal growth in 16 of these 19 MTP joint grafts during the long-term follow-up. For unknown reason, the proximal phalanx growth seems to be more reliable than is the metatarsal longitudinal growth. The same finding has previously been presented by the author in the toe-to-hand transplantation series for congenital finger defects.5 The ulna growth has followed the natural growth, which is specific to the radial club hand.23,27 The mean length of involved ulnas is 15.4 cm in these 19 patients. Only a minor enhancement in ulnar longitudinal growth may be due to the preoperative distraction period. Maximal ulna length in the series is 20 cm. The relative ulna length (RUL) compared with normal opposite extremity or normal 50% percentile was 67% in mean. Three patients were withdrawn from the calculation due to the special short body height and a tendency to dwarfism in two RAPALIDINO patients (no. 9 and no. 18), and one patient (no. 11) had a failed centralization before the joint transplantation, which has clearly worsened the longitudinal growth of the ulna. The correction of the severe radial deviation deformity was successful in most cases after the joint transplantation. An initially good alignment (Fig. 6) has gradually worsened with 12 degrees in mean in the long-term follow-up of the earlier series of the initial nine patients. Radial deviation (radial forearm angle) at wrist is now between 10 and 45 degrees (mean, 28 degrees). The growth balance at distal Y-formed ulna is good in eight hands (Table 3 and Fig. 7.). All these patients belong in the latter half of the series (hands no. 11 to 19). Out of 16 primarily successful cases, the MTP-II joint graft at the wrist has tolerated well the stress forces in 11 cases. There appears a mild (four joints) or clear (two joints) subluxation tendency in the grafted joints. However, none of the patients have reported any pain at the reconstruction area. The wrist mobility has been uniformly good with a total active motion (TAM) range from 30 to 115 degrees (mean 83 degrees), but extension of the wrist has remained weak in many hands apparently due to the severe congenital muscular defects. The extension occurs actively to neutral position in 11 cases and more extension into dorsiflexion is actively possible in 6 hands with the range from 5 to 30 degrees (mean, 17 degrees). Also, in 8 hands there is an extension lag below neutral within the range 10 to 50 degrees (mean, 17 degrees). A true pro-supination is completely lacking in all cases because the stabilizing bone unit is fixed to the ulna and all the hands are in slightly pronated position. The proximal shaft of the ulna has stayed straight in five cases. However, it was bowed over 40 degrees in two older patients. Twelve other forearms had a milder bowing tendency within a range of 10 to 30 degrees. The ulna bow usually at midshaft was in mean 17 degrees. After the successful wrist reconstruction, the next 10 years in the child's life seems to be without problems, and the deforming force by radial structures was not a prominent feature any longer. However, at adolescence the growth spurt of the distal ulnar epiphysis will change the balance at the Y-fork of the distal ulna especially when the metatarsal growth at the transplanted MTP joint is not appropriate. A fusion of the distal ulna physis may become indicated at the age of 11 to 13 years to prevent recurrent deviation. Also, additional bowing at the ulna more proximally may be an indication for further treatment attempts with correction osteotomy. Two osteotomies (hands no. 5 and no. 13) have been done for this reason. In all hands but not the first case, the sequence of treatment has been as described. In hand no.1 there was no distraction done preoperatively. It was done some years later combined with a “joint transport.” Joint transport means that the external fixator is reapplied and the MT-bone is detached from the ulna. Then with a new distraction period, the wrist alignment can be corrected and the MTP joint carried more distally and fixed again to a more distal area or simply letting it heal with elongated position with spontaneous bone formation as in the bone-lengthening procedure. This has also been done in hand no. 10 after delayed healing at the distal graft connection and after the growth arrest due to the fracture problem in hand no. 4 (Fig. 8).
Figure 6.
(A) Clinical view of the overcorrected radial club hand (hand no. 14) before pollicization at age 4 years. (B) A radiologic view of the same hand 11 months after joint transfer.
Figure 7.
Radiograph of a Y-formed distal ulna in hand no. 14. The situation 8 years postoperatively shows a good balance with “radial Y-fork limb” or metatarsal length of 43 mm and distal ulna length of 41 mm.
Figure 8.
An example of “joint transport” in hand no. 4. Because of the severe fracture complication, this boy had no growth in the metatarsal part, and as a secondary salvage procedure at the age of 11 years, the joint was detached from the ulna, and the distraction procedure was repeated until a good hand alignment was achieved.
Comments on Distal forearm Y-fork Balance
The alignment of the hand and the axis of the wrist joint is dependent on growth balance between the limbs of the Y-fork at the distal ulna. The radial limb is the transplanted metatarsus and the ulnar limb is the distal ulna after the created branching point (Fig. 7). Theoretically, the longitudinal growth of the second metatarsal bone from age 3 (bone length 3 to 4 cm) to age 17 (bone length 6 to 10 cm) at the foot may be between 3 and 7 cm among normal individuals. The expected value of metatarsal growth is available if an x-ray is taken of the father's (mother's) and patient's foot at the same time. However, the growth properties of the metatarsal graft after the transplantation are influenced by the operative technique, transplantation procedure, ischemia time, circulatory disturbances postoperatively, loading alterations, and other partly unknown factors. At the same time, the distal ulna epiphysis has certain abnormal growth properties in all radial club hand patients. After successful reconstruction, the longest ulnar limb at the Y-fork has been 63 mm in length at long-term follow-up (range, 30 to 63 mm; mean, 42 mm). Radial limb at the Y-fork has been within the range 24 mm to 54 mm (mean, 36 mm) at follow-up. There are some well-growing metatarsal parts (hand no.15) with too transverse alignment, which is adding to the hand forearm angle unnecessarily. The balance at the distal forearm Y-fork growth can only be expected when the metatarsal bone longitudinal growth remains unaffected or will grow almost normally. This means that in addition to the joint graft alignment problems, a failure or retardation in growth on the metatarsal side will dictate the recurrent radial deviation.
Comments on Hand Function
The hand function in long-term follow-up seems to be influenced mainly by the original stiffness or quality of the fingers at the affected hand. In severe cases, when the fingers have marked camptodactyly and stiff MCP joints, hand function remains clearly inferior, and possibilities for a good thumb function after pollicization are also limited. Also, an associated syndactyly may additionally compromise the hand function. There exist no normal intrinsic muscles in some of the diseased hands. Also, there has been one patient with second-toe metatarsal transplant without any interosseal muscles (patient no. 17). A pollicization, when it is possible to perform successfully, will improve the hand function and is usually recommended in all cases with good finger function. The limitation of wrist function is dependent on original muscular defects of the forearm. Elbow function seems to become slightly improved by the added tension after soft tissue distraction.
Comments on the Donor Site
At long-term follow-up, there has been very minimal complaint if any about the donor site. Even the scar has been almost invisible and without any effect to toe or foot function. The rule is to leave enough skin for primary closure to prevent scar problems at donor site. Donor-site problems are rare and minor including two scar contractures; one limiting the great toe flexion (patient no. 11), and another pulling the third toe into a mild hammer-toe position (patient no. 18). Also, one moderate hallux valgus deformity was noticed in patient no. 10, but she had a hallux valgus tendency on the opposite foot as well. The donor foot after second ray removal has been without pain in all but one 16-year-old girl, who has been very active in sports and dancing (patient no. 5). This has been a temporary symptom related to heavy gymnastic activity. The patients have been usually satisfied with their donor feet after second ray removal at late follow-up (Fig. 9).
Figure 9.
The feet of a female patient (hand no. 14) at the age of 11 years 4 months. The second metatarsal joint from other foot has been used for temporomandibular joint reconstruction due to a mandible anomaly.
Overall Results (Fig. 10)
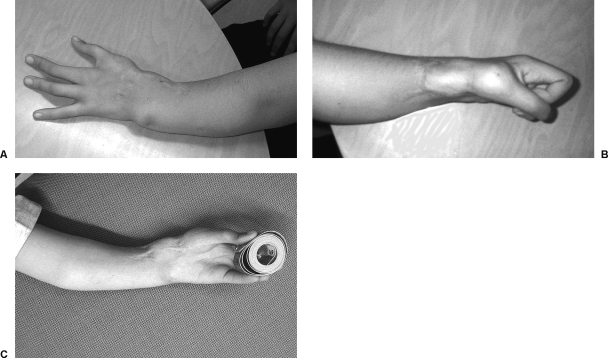
Figure 10.
The treated radial club hand (hand no. 14) 8 years postoperatively. Patient age is 11 years 4 months. (A) There is a mild bow in the ulna midshaft and a 10-degree hand-forearm angle. (B) Making a fist is limited by the original stiffness of the III MCP joint. (C) Volar view of the treated extremity showing the pollicized index.
In the early period after transplantation, a joint graft will add to the broadness of the wrist area especially when the alignment is overcorrected. The distal forearm on the proximal side of the joint graft remains narrow because the shaft of the radius is lacking. These two facts correlate with the cosmetic appearance. The results during the next 8 to 10 years after joint transplantation with successfully aligned wrists are quite acceptable. At the late follow-up, there was an increased bow at the proximal ulna in some cases, and a slow recurrence of the radial deviation may give an appearance of radially bowed extremity because these two deformities are combined. The wrist function remains good (TAM is 83 degrees in mean), and the worst thing is the great length discrepancy when speaking of unilateral cases. The ulna length discrepancy was from 55 to 100 mm (mean, 77 mm) in the group of 10 unilateral patients. In this series, there was no advantage of performing the treatment at the age of 1 year like patients no. 2, no. 5, and no. 13. The best results have been obtained in the age group when the treatment was started between 24 and 48 months. Functionally, the results in long-term follow-up did correlate best with the preoperative RCH-severity score. In the group of poor results, there were four hands with preoperative grading as severe. One poor result was due to the comminuted joint fracture 2 months after the reconstruction.
Good functional results could be achieved in grades mild and moderate. Generally, the results seem to be better in the latter part of the series probably due to the learning curve, but also in this group the growth spurt at adolescence has not yet influenced the final Y-branch balance. Also, the joint configuration or the subluxation tendency has not become apparent or there has been better success in its prevention. Despite complete failure after joint transplantation of the hand of a TAR patient (no. 8) was considered as good after secondary procedures completed at the age of 15 years. The usefulness of the operation can be seen in good and effective wrist mobility and in the ability to reach higher with the treated extremity over the nontreated one, especially in four bilateral cases with one nontreated hand. The reach to the higher object is 6 to 20 cm (mean, 11 cm) better in these 4 extremities. In the severe bilateral situation (patient no. 3), even if both hands are now straight, there is no possibility to take care of personal hygiene due to other related stiffness problems at elbows and shoulders. The first operated patient would have been in the same situation without this treatment, which did give a possibility to flex the wrist. Only two operated hands (no. 9 and no. 17) have become dominant hands in two patients who also have an opposite nontreated radial club hand. The result in case 11 (Fig. 11), which was operated after bilaterally failed centralization, shows that when the growth of ulna has become disturbed, the metatarsal will compete even in a better way than in nonoperated cases. After 9 years of follow-up, the Y-fork balance is very good at the age of 15.5 years.
Figure 11.
In this patient both hands were primarily centralized, but the radial deviation did recur. The right wrist (hand no. 11) was reconstructed with a MTP joint graft at the age of 6 years. A pollicization was done only to the left hand. (A) Early postoperative view 6 months after a joint transfer for the right wrist. (B) View at the age of 15.5 years and after 9 years of follow-up. A mild bowing of the forearm during the follow-up is seen. The ulna length is 14.5 cm bilaterally. The shortness is due to the previous centralization attempts.
DISCUSSION
The presented clinical material and the technique using preoperative soft tissue distraction followed by a metatarsal joint graft for wrist reconstruction and stabilization represents an almost experimental type of surgery from its historical part. The operative method was developed when the author was investigating the patients from the old series28,29 of professor Heikel and after observations that the ulna growth was clearly affected by all conventional centralizations of his time. Also, the use of a vascularized joint transplantation was a natural development after the experiences with the series5 of the toe transplantations for congenital finger defects. The gradual improvement and understanding of the effects of operative details may already have influenced the later series after 1998, and uniformity in management schedule has been achieved only with the aid of improved knowledge from the first published series 8, when the same patients (hand nos 1 to 9) have been further followed up. The conventional treatment with centralization or radialization has a reputation to be unreliable as far as longitudinal ulna growth and stability of the hand alignment is concerned. Also, there will remain a marked limitation of wrist mobility. These problems have been reported in most long-term follow-up studies.19,28,30,31,32 The only certain means of achieving a straight hand alignment may be the complete fusion of the wrist area as stated by Heikel in 1959 in his classic conclusions 28. The attempts at improving the management technique in the past have included the use of the microvascular fibula graft.13,14 These results in the past were not completely satisfactory. The growth using a microvascular fibula might currently be the best solution for the longitudinal forearm development because these techniques have recently become apparently improved.33,34 However, the reported complications (Innocenti M, personal communication) at donor site may be a contraindication for the use of proximal fibula at early age with this congenital indication, when the lower limb is developing. There is a risk for peroneal palsy or some permanent weakness in foot or toe extension and a risk of valgus deformity at the ankle. Sometimes, a great-toe flexor dysfunction can be found after the removal of muscle insertion area. Also, the severity of the hand abnormality or associated syndromes may be so great that there is simply no indication to risk for additional morbidity because the extremely poor hand function will anyway remain a major concern in most severe grades (13 and over). When selecting the treatment method and evaluating the results, a more specific classification of the radial club hands in Bayne type 3 and 4 categories should be used. A severity grade should always be assessed before treatment attempts according to the defects of the fingers, hand, wrist, and forearm and also according to available proximal elbow and shoulder joint functions (Table 1). A severe syndrome situation will also influence the assessment of the radial club hand patient. The hand deformity may appear as the least important among multiple other problems. A radial-deficient upper extremity in the complete absence of the radius remains a challenge. There is no a single operation to solve all the components of this problem. The soft tissue distraction is not easily performed without complications in a small child. The device to be attached to the small hand bones must be reliable and easily operated by the parents. The soft tissue distraction program must be planned according to the individual circumstances. A written schedule with exact orders with an appropriate time table is mandatory for the parents, who do their best in repeating the planned program in the right order. Most parents do manage this part very well and usually without severe pin-track infections or other complications. Regular pin-site cleaning with the removal of crusts is the basis of long-lasting management period with the ex-fix. A prophylactic antibacterial medication has been considered helpful in similar fashion as the prevention of the urinary tract infections in small children. The x-ray controls are necessary in the proper timing of the joint transplantation operation. The joint transplantation with a successful epiphyseal growth is a demanding task and requires experience in adult and child toe-transfers by the surgical team as well as by the pediatric anesthesiologists,26 who take the biggest risk of the long procedure. That is why this type of surgery should be done in dedicated centers of microsurgical reconstruction for the pediatric patient population. When conducting his team, the responsible surgeon should have an orchestra with specialized hand surgeons for each part of the operation to guarantee high quality at every step. The responsibility is continued in the after-care of this complex procedure, and the first five days are mandatorily under intensive care observation.
The factors that do encourage the use of this type of joint transplantation method for the radial club hand stabilization are as follows. The longitudinal forearm growth is not endangered due to the operation because the distal ulna head with the physis is not touched or dissected during the procedure. The relative ulna length (RUL) has been 67% in this series. The ulna length has been clearly longer (average, 15.4 cm) in the current series than in the long-term series after centralization studied by Goldfarb et al.32 They reported that average ulna length was only 12 cm despite the fact that their study was done in mean 20 years postoperatively with most patients at adulthood. Also, the relative ulna length in their series was only 54%. In our series, the ulna growth has remained at the level that is considered specific to the radial club hand. When the joint transplantation is successfully performed, there are chances first for clear hypertrophy and second for normal epiphyseal growth in the transplanted metatarsal bone supporting the hand in the right alignment during the growth period (Fig. 7). Additionally, the MTP joint graft used allows a good and stable range of motion for the wrist. It is excellent to flexion but there is a limitation and weakness in extension function due to the original defects of the radial forearm musculature.
There are also factors against using this type reconstruction. The learning of the procedure and all the long-term care needed is difficult and requires regular experience in microsurgical toe-transfer or at least a lot of experience in other microsurgical reconstruction like replantation or composite flap transplantation surgery. The prevention of possible MTP joint subluxation needs to be studied further. All efforts should be made during reconstruction to get the best possible alignment of the joint and to create a sound dynamic stability to prevent this problem. In the current series, the donor-site morbidity is acceptable (Fig. 9) and can be prevented with adequate planning. The long-term foot problems are minimal when using the second metatarsal ray in a carefully planned way for the reconstruction of the radial half of the wrist joint. Only the feet with primary pes metatarsus primus varus are in danger to develop a hallux valgus deformity as they are even without any operations. In the presented small series, with a mean follow-up time of 11 years, one third of the extremities show a good hand alignment with acceptable wrist motion. The Y-formed ulna created with a microsurgical MTP joint graft seems to be a good solution to support the hand in good alignment for the period from 3 years until 11 years, and it allows good wrist extension-flexion mobility. In a majority of the cases, the MTP joint has tolerated well the stress forces, and the growth has continued in an acceptable way in the successful cases. The longest follow-up is now 20 years in a patient operated in 1987 with still-good joint configuration (Fig. 12). However, there seems to be a tendency to subluxation in six of the joint grafts at late follow-up. This may be due to the fact that in the earlier series, the active tendon stabilization was not carefully respected or it was not possible to do perfectly due to anatomic defects. Also, the alignment of the joint graft may have been less optimal. Partly, this subluxation may be induced by abnormal biomechanics when the deviational stress forces do load this simple and relatively small joint structure. This fact should be clearly taken in account during reconstructive procedures using any joint transfers, which remain under heavy load with a large range of motion. The worst results from the joint transplantation have been due to the vascular failures in two cases with fragmentation of metatarsal head in one (hand no. 8) and necrosis of the MT head in the other (hand no. 17). After failure hand no. 8 had a bad alignment of the wrist, but it was solved with a conventional bone graft at the age of 15 years, and the wrist alignment was corrected from 55 degrees radial deviation to 25 degrees finally. Because of the TAR syndrome, there appeared to be also some distal remnant of the radius, and her wrist function is now among the best. The experience with this TAR patient does mean that a centralization is contraindicated in such a situation, and all efforts to stabilize the possibly existing distal radius fragment should be done with a growing bone graft. When a joint graft is used that can be fused at adolescence, the mobility will remain at the original wrist joint. Also, a fracture complication in one patient (hand no. 4) has induced a metatarsal head necrosis. The positive results in the later 10-year part of the series is promising and may lead to better long-term results as understanding of the problems during the complex treatment period increases.
Figure 12.
The first patient (hand no. 1) in the series had a MTP joint transfer in 1987 at the age of 5 years. His only distraction procedure was done at the age of 10 years with a “joint transport.” The metatarsal bone was fixed 40 mm more distally. The situation in the radiograph, 20 years postoperatively, shows that the MTP joint still has a good configuration although a bone cyst is visible at the metatarsal head.
CONCLUSION
Soft tissue distraction is a good means of aligning the radially deviated hand into acceptable position. It should be done cautiously with a speed not exceeding 0.5 mm/day. Suitable timing for starting the procedure is between the age 2.5 and 4 years.
The ulna growth continues after joint transplantation according to a growth rate that is specific to the radial club hand. The ulna length will be between 14 and 20 cm at adulthood. It averaged 67% of the normal ulna length in this series.
After a successful vascularized MTP joint transfer, the wrist remains stable and the alignment stays acceptable for the next 8 to 10 years when the reconstruction is done at the age of 3 years.
The distal ulna will grow faster than the transplanted metatarsal during the growth spurt at adolescence leading to a slow partial recurrence of radial deviation. Among 19 patients followed 11 years in mean, the hand forearm angle averaged 28 degrees. It was increased by 12 degrees in mean in the initial 9 patients operated before 1998. Also, a tendency to a variable degree of subluxation at the MTP joint graft was noticed in 6 of 19 cases. The radial deviation was increased in these cases due to the weakened stability.
The active extension-flexion mobility of the reconstructed wrists was uniformly good with a mean range of 83%. There was always a marked weakness in hand extension force due to the congenital muscular defects, and the weakness in grip strength was also clear for the same reason.
The final overall hand function is mainly dependent on the original severity grade of the individual congenital defect of the whole extremity.
There may be a need for corrective osteotomy due to bowing at the middle ulna.
A preoperative MRI study is necessary especially in TAR patients. A possibly existing remnant of the distal radius cartilage in TAR syndrome should be preserved. This finding may be a contraindication for a conventional centralization procedure. MRI study would be helpful in all RCH cases in the assessment of the nonvisible cartilage parts, but it will require an extra anesthesia, and we have not done it without special reasons.
The radial club hand will remain very often poorly understood and probably even more often poorly managed without complete guidance about conservative therapy immediately after birth. At this stage, the chances of conservative measures are greatest, and this option should always be used and maintained with careful continuous splinting and responsible follow-up. Hopefully, the severe deformity and the longitudinal growth defect at forearm of these children can be managed in the future by better means. The effects of preoperative distraction will be better understood. At present, a soft tissue distraction that is too fast may be harmful for the muscle tissue and its later function. Possibly, the chances of the physeal distraction may be used in a more positive way in the future to achieve longer forearms. Because the limb-length discrepancy often remains the major concern in treatment of the radial club hand, bone-lengthening methods may also be needed. These lengthening procedures are extremely time consuming and at risk of many complications. Only a few patients have been treated with full correction of limb-length discrepancy.17,18 In these referenced series, the indication to bone lengthening seems to have been a growth impairment or cessation after too early and possibly “aggressive” surgery near the distal ulna growth plate. The bone-lengthening procedure may have to be repeated when done too early during the growth period. To avoid unnecessary need for bone lengthening, the operative procedures used to treat the radial club hand in early childhood should not endanger the longitudinal growth in any circumstances. The aim should be to save or enhance the ability to grow in these short extremities. The recent development of techniques in performing the proximal epiphyseal transplantation33,34 of the fibula after malignant forearm bone tumor cases seems to be promising and may perhaps be helpful, when properly used, in achieving a more normal forearm growth in radial club hand patients.
REFERENCES
- Buck-Gramcko D. Radialization as a new treatment for radial club hand. J Hand Surg. 1985;10A:964–968. doi: 10.1016/s0363-5023(85)80013-7. [DOI] [PubMed] [Google Scholar]
- Urban M A, Osterman A L. Management of radial dysplasia. Hand Clin. 1990;6:589–605. [PubMed] [Google Scholar]
- Sabharwal S, Finuoli A L, Ghobadi F. Pre-centralization soft tissue distraction for Bayne type IV congenital radial deficiency in children. J Pediatr Orthop. 2005;25:377–381. doi: 10.1097/01.bpo.0000152907.31293.00. [DOI] [PubMed] [Google Scholar]
- Goldfarb C A, Murtha Y M, Gordon J E, Manske P R. Soft-tissue distraction with a ring external fixator before centralization for radial longitudinal deficiency. J Hand Surg. 2006;31A:952–959. doi: 10.1016/j.jhsa.2006.03.019. [DOI] [PubMed] [Google Scholar]
- Vilkki S K. Advances in microsurgical reconstruction of the congenitally adactylous hand. Clin Orthop Relat Res. 1995;314:45–58. [PubMed] [Google Scholar]
- Vilkki S K. In Canadell J, Ferial F, Lazo-Zbikowski J, editor. Proceedings of the 14th International Hoffman External Fixation Conference. EUROGRAF, Pampolona, Spain: 1992. Distraction lengthening and microvascular bone transplantation in the treatment of radial club hand. pp. pp. 249–251.
- Vilkki S K. Vascularized joint transfer for radial club hand techniques in hand and upper extremity surgery. Tech Hand Up Extrem Surg. 1998;2:126–137. doi: 10.1097/00130911-199806000-00007. [DOI] [PubMed] [Google Scholar]
- Vilkki S K. Distraction and microvascular epiphysis transfer for radial club hand. J Hand Surg. 1998;23B:445–452. doi: 10.1016/s0266-7681(98)80120-4. [DOI] [PubMed] [Google Scholar]
- Kaariainen H, Ryoppy S, Norio R. RAPADILINO syndrome with radial and patellar aplasia/hypoplasia as main manifestations. Am J Med Genet. 1989;33:346–351. doi: 10.1002/ajmg.1320330312. [DOI] [PubMed] [Google Scholar]
- Bayne L G, Klug M S. Long-term review of the surgical treatment of radial deficiencies. J Hand Surg. 1987;12A:169–179. doi: 10.1016/s0363-5023(87)80267-8. [DOI] [PubMed] [Google Scholar]
- Albee F H. Formation of radius congenitally absent. Conditions seven years after implantation of bone graft. Ann Surg. 1928;87:105–110. [PMC free article] [PubMed] [Google Scholar]
- Starr D E. Congenital absence of the radius. A method of surgical correction. J Bone Joint Surg. 1945;27A:572–577. [Google Scholar]
- Pho R WH, Patterson M H, Kumar V P. Free vascularized epiphyseal transplantation in upper extremity reconstruction. J Hand Surg. 1988;13B:440–447. doi: 10.1016/0266-7681_88_90175-1. [DOI] [PubMed] [Google Scholar]
- Tsai T M, Ludvig L, Tonkin M. Vascularised fibular epiphyseal transfer. A clinical study. Clin Orthop Relat Res. 1986;210:228–234. [PubMed] [Google Scholar]
- Nettelblad H. Microvascular Growth Plate Transplantation [master's thesis] Linköping, Sweden: Linköping Medical University; 1984.
- Bowen C VA, Ethridge C P, O`Brien B M, Frykman G K, Gumley G J. Experimental microvascular free growth plate transfers. Parts I and II. J Bone Joint Surg. 1988;70B:305–314. doi: 10.1302/0301-620X.70B2.3346312. [DOI] [PubMed] [Google Scholar]
- Kawabata H, Shibata T, Masatomi T, Yasui N. Residual deformity in congenital radial club hands after previous centralisation of the wrist. Ulnar lengthening and correction by the Ilizarov method. J Bone Joint Surg. 1998;80B:762–765. doi: 10.1302/0301-620x.80b5.8839. [DOI] [PubMed] [Google Scholar]
- Pickford M A, Scheker L R. Distraction lengthening of the ulna in radial club hand using the Ilizarov technique. J Hand Surg. 1998;23B:186–191. doi: 10.1016/s0266-7681(98)80172-1. [DOI] [PubMed] [Google Scholar]
- Damore E, Kozin S H, Thoder J J, Porter S. The recurrence of deformity after surgical centralization for radial club hand. J Hand Surg. 2000;25A:745–751. doi: 10.1053/jhsu.2000.6460. [DOI] [PubMed] [Google Scholar]
- Catagni M A, Szabo R M, Cattaneo R. Preliminary experience with Ilizarov method in late reconstruction of radial hemimelia. J Hand Surg. 1993;18A:316–321. doi: 10.1016/0363-5023(93)90367-C. [DOI] [PubMed] [Google Scholar]
- De Pablos J, Canadell J. Experimental physeal distraction in immature sheep. Clin Orthop Relat Res. 1990;250:73–80. [PubMed] [Google Scholar]
- Alberty A. The effects of physeal distraction and compression on the growth plate. An experimental study on rabbits [master's thesis] Helsinki, Finland: University of Helsinki; 1993.
- Vilkki S K. In: Duparc, Alnot, Soucacos P, editor. Surgical Techniques in Orthopaedics and Traumatology. Paris, Elsevier: 2001. Radial club hand: distraction and joint transplantation. pp. Chapter: 55-370-C-10, 1–5.
- Vilkki Simo K. In: Wei FC, Chuang DCC, Chen H, editor. Reconstructive Microsurgery. Proceedings of the Inaugural Congress of the World Society for Reconstructive Microsurgery, Taipei, Taiwan. Bologna: Monduzzi Editore; 2001. Radial club hand. Guidelines for wrist distraction technique before microvascular epiphyseal joint transfer. pp. 199–200.
- Skerik S K, Flatt A E. The anatomy of congenital radial dysplasia. Clin Orthop Relat Res. 1969;66:125–143. [PubMed] [Google Scholar]
- Inberg P, Kassila M, Vilkki S, Neuvonen P. Anesthesia for microvascular surgery in children. A combination of general anesthesia and axillary plexus block. Acta Anaesthesiol Scand. 1995;39:518–522. doi: 10.1111/j.1399-6576.1995.tb04111.x. [DOI] [PubMed] [Google Scholar]
- Sestero A M, Van Heest A, Agel J. Ulnar growth patterns in radial longitudinal deficiency. J Hand Surg. 2006;31A:960–967. doi: 10.1016/j.jhsa.2006.03.016. [DOI] [PubMed] [Google Scholar]
- Heikel H VA. Aplasia and hypoplasia of the radius: studies on 64 cases and on epiphyseal transplantation in rabbits with the imitated defect. Acta Orthop Scand. 1959;Suppl 39:1–155. [PubMed] [Google Scholar]
- Vilkki Simo K. Aplasia radii and the material of Henrik Heikel: the results of the long-term follow-up after 35-years. Finnish Journal of Orthopaedics and Traumatology. 1997;20:205–208. [in Finnish] [Google Scholar]
- Lamb D W. Radial club hand. J Bone Joint Surg. 1977;59A:1–13. [PubMed] [Google Scholar]
- Bora F W, Jr, Osterman A L, Kaneda R R, Esterhai J. Radial club hand deformity. Long term follow-up. J Bone Joint Surg. 1981;63A:741–745. [PubMed] [Google Scholar]
- Goldfarb C A, Klepps S J, Dailey L A, Manske P R. Functional outcome after centralization for radius dysplasia. J Hand Surg. 2002;27A:118–124. doi: 10.1053/jhsu.2002.30078. [DOI] [PubMed] [Google Scholar]
- Innocenti M, Delcroix L, Romano G F, Capanna R. Vascularized epiphyseal transplant. Orthop Clin North Am. 2007;38:95–101. doi: 10.1016/j.ocl.2006.10.003. [DOI] [PubMed] [Google Scholar]
- Innocenti M, Delcroix L, Manfrini M, Ceruso M, Capanna R. Vascularized proximal fibular epiphyseal transfer for distal radial reconstruction. J Bone Joint Surg. 2004;86A:1504–1511. doi: 10.2106/00004623-200407000-00021. [DOI] [PubMed] [Google Scholar]