ABSTRACT
With the increase in popularity of aesthetic surgery, patients with previous face-lifts are increasingly encountered in clinical practice. Whereas the literature is replete with face-lift techniques and management of the primary rhytidectomy patient, there is a relative paucity of information concerning secondary facial rejuvenation procedures. This article is intended to bridge that gap and stimulate further discussion about this clinical situation.
Keywords: Revision rhytidectomy, lateral sweep, revision face-lift, pixie ear deformity, face-lift sequelae
There has been a marked increase in the number of face-lifts over the past 10 years. The American Society for Aesthetic Plastic Surgery statistics estimate that there were ∼100,000 face-lifts performed in the United States in 1999; by contrast, in 2008, this number had jumped to over 130,000, an increase of over 30%.1 Increasingly, as (particularly younger) patients undergo face-lifting procedures, it is reasonable to anticipate a greater number of patients seeking secondary facial rejuvenation. A brief review of the literature illustrates the lack of material published on the subject of secondary rhytidectomy. A MEDLINE search of “rhytidectomy” returns 2132 references, whereas “revision rhytidectomy” yields only 29 results.2
There are several questions that need to be answered in the care of the revision face-lift. What is the nature of the prior dissection plane and should it be re-utilized or should a different plane be employed? Should the neck be reopened? How are deformities and cosmetic issues from the first surgery corrected and prevented after the second procedure?
The clinical situations commonly encountered in revision rhytidectomy are reviewed and treatment options discussed. For the sake of clarity, only face-lift surgery will be reviewed; secondary brow lifts and neck lifts are beyond the scope of this discussion.
PATIENT EVALUATION
As with any patient presenting for facial rejuvenation, a standard preoperative analysis of the face should be performed. A “top-down” approach has been systematized and well described.3 A history of previous rhytidectomy clearly adds a level of complexity to this assessment. Incisional and soft tissue deformities from the primary rhytidectomy should be identified and discussed with the patient, as these should be addressed for optimal secondary outcome. Any preexisting deficits in sensation and facial animation must be thoroughly searched for and documented.
During the preoperative consultation, the specific features the patient wishes to address should be individually discussed. It is important to distinguish and classify the global environment in which revision surgery is being performed. Is a once good result now less than desirable due to the natural aging process or significant weight fluctuation? Is the result of the original surgery still acceptable but other issues of facial aging now cause an aged appearance? Was the original surgical result sub-par because of random or preventable complications that now require repair?
Often, a disharmonious appearance, with adequate correction in some areas while other regions remain tired and aged-appearing, is the primary concern. The nasolabial folds are notorious for persistence despite corrective efforts.4 It is crucial as a professional to resist the temptation to criticize the prior surgeon's efforts, as several factors, including the patient's preoperatively stated desires, may have limited the initial surgery only to lead to the patient's postoperative regret. Previous operations may have been thoroughly planned, executed with great artistry and resulted in excellent results. However, rhytidectomy does not arrest the microbiological aging process or stop the effects of gravity. While the platysma corset may have remained tight and the subcutaneous fat adequately treated, the submandibular glands and anterior digastric muscles may now be ptotic, peeking through the overlying soft tissue carpet.5 In general, the face-lift surgeon is wise not only to examine the parts of the face but also to compare their relative appearance and plan accordingly. Furthermore, the genesis of the problem should be assessed: Is the patient suffering from re-ptosis of previously lifted tissues, worsening of a disharmonious result, volumetric deflation,6 or some combination of the above?
At the initial surgery, the sideburn and temporal and occipital hairlines may have been distorted either by an overly aggressive resection or by poor hairline scar site selection.7 Loss of earlobe definition and blunting of the tragus are two aesthetic problems with the ear that can be seen with improper design of the incision and/or too much tension on the ear at the initial closure.8 Additionally, the pixie ear deformity, characterized by caudal earlobe migration and axis distortion, may develop as a result of excessive wound closure tension or scar contracture.9
There are several soft tissue distortions possible after face-lift surgery: skin pleating10; lateral sweeps11; smile block (Lambros V, personal communication, October 2008); “joker's lines”12; hollow orbits11,13; commissural distortion; and flattening of facial contours.14 Hamra has discussed the negative long-term effects of a face-lift flap pulled in a completely lateral vector. This causes pleating in a lateral direction, which can be unsightly. Additionally, when the upper portion of the cheek is undercorrected with this vector of pull, as it continues to age, it may sag over the corrected lower portion of the face, causing the stigmata of the lateral sweep. Stuzin and Lambros have recently pointed out the appearance of the “joker's line,” or the cross-cheek depression. This is a sequela of the face-lift in a patient who has submalar hollowing preoperatively; this hollowing is exaggerated by the translation of the face-lift flap, leading to a dysesthetic appearance in which the commissure appears to extend onto the cheek. Commissural distortion, with a horizontal lengthening of the mouth, when combined with the cross-cheek depression, can lead to an appearance that is quite unsightly. Noting these deformities preoperatively can enable the surgeon to adequately address these problems in the revision face-lift.
Finally, with the advent of laser resurfacing as an adjunctive or stand-alone procedure, it is important to assess the color of the patients face relative to their neck. Hypopigmentation is not uncommon, and redraping darker, sun-beaten skin above the jawline will leave an unsightly demarcation on the face.15
A comprehensive preoperative discussion with the patient is absolutely mandatory. What is and (more importantly) what is not possible to correct must be frankly and specifically outlined to the patient. It is important to emphasize to the patient the limitations imposed on the revision procedure by the prior surgery.
GENERAL MANAGEMENT
Four potential presentations for the secondary face-lift can be described: (1) a poorly performed primary procedure with limited results; (2) a poorly selected face-lift procedure with limited results; (3) a poorly executed or well-executed primary face-lift with postoperative sequelae; or (4) a well-selected and executed primary face-lift procedure with good results lost over time as a result of continued aging. It is important to review preoperative and postoperative photographs and the operative report of the primary face-lift, and an assessment should be made as to whether the proper technique was used. If results of a properly performed primary procedure are limited, a more aggressive technique should be used in the secondary procedure. If limited improvement occurred after a properly selected but poorly performed technique, it is not unreasonable to proceed with a more thoroughly performed but similar procedure secondarily. If initial results were good but failed to persist, alternative forms of facial aging (e.g., soft tissue or bony volume loss) should be sought, and procedures ancillary to the revision face-lift should be considered. Patient expectations should be assessed and actively managed, as patients will bring to this secondary procedure preconceived notions of wound care, postoperative course, and surgical results.
Surgery in any region that has undergone previous operation is always more complicated than venturing into uncut tissue. Scar decreases the facility of dissection, both by distorting planes and by increasing the rigidity of the tissues. Improved postoperative vascularity of the rhytidectomy flap has never been demonstrated; however, if the same flap is dissected, it should be theoretically “delayed” with improved perfusion.16 Additionally, tension on the flap should improve the nature of its vascularity.17 Conversely, chronoaging of the skin in the time between the initial and revision surgeries, as well as the process of the prior surgery and wound healing, may have left the skin considerably less elastic than before the first procedure.
A comprehensive medical evaluation is essential, as a patient who had an uncomplicated course after a long surgery in her forties may not be as healthy 15 years later. It is important to ascertain whether the patient has begun taking any new medications or herbal supplements over the time since the first surgery. Guyuron et al demonstrated through patient survey data that a significant number of patients will have started a new medication between their first and second face-lift procedures.5 Moreover, a significant number of patients will have developed a new medical condition during this time period. Whereas patients may have stopped tobacco use at the time of the first surgery, Guyuron notes that 60% of patients who smoked before their first procedure will continue to smoke after their secondary rhytidectomy. This makes it imperative that a thorough preoperative medical evaluation is obtained. In the senior author's practice, the nature and extent of the planned procedure are discussed with the patient's primary care physician, and documented recommendations for perioperative medical management are requested.
INCISIONS
In general, the secondary face-lift is performed using the prior incisions and excising the existing scars. Exceptions to this rule include:
Any well-healed and inconspicuous portion of the scar from the initial procedure that is not necessary for flap elevation and superficial muscular aponeurotic system (SMAS) manipulation is not touched.
In women with pretragal scars and sufficient skin laxity, a retrotragal incision is used and the pretragal scar excised along with redundant skin.
Standard incisions are used in cases of obviously malpositioned scars that can be mobilized sufficiently to allow excision and closure in more appropriate locations.
Attention should be paid to the quality of wound healing from the prior surgery, and although poor scarring may have been due to poor technique in the initial surgery, it behooves the surgeon to anticipate scarring after revision rhytidectomy no better than those from the primary procedure.
THE PLANE! THE PLANE!
Every effort should be made to obtain the initial operative report in an effort to understand what was done in the previous surgery so that intraoperative findings can be anticipated and potential pitfalls avoided. Several issues should be specifically addressed:
How far was the skin flap elevated?
To what extent was the SMAS elevated/manipulated?
Was any liposuction performed?
What was done to the platysma?
Was there any inordinate bleeding or anatomic anomalies?
As previously stated, it is believed by some that the secondary face-lift flap should be more resistant to vascular embarrassment due to the delay phenomenon. Despite this, there is a theoretical disadvantage to using the same dissection plane. Scar tissue is less elastic18 and flap excursion may be diminished,19 although this idea has been challenged.5 Additionally, the connective tissue fibers in the flap are oriented parallel to the direction of the previous vector,20 and theoretically this may lead to earlier relapse after secondary surgery, as the weaker fibers are subjected to new tension and stress.21 Moreover, it is possible that the facial nerve branches might be tethered more superficially and hence more exposed and vulnerable during a secondary surgery if dissection is performed in the same plane. Finally, prior injury to some peripheral branches of the facial nerve (especially involving the zygomatic and buccal innervation to orbicularis oculi and the lip elevator muscles22,23) may not be readily apparent because of cross-innervation between these two branches. However, previous injury to some of these branches may have reduced their redundancy, and any additional injury during a sub-SMAS dissection may produce a clinically apparent lower lid or midfacial hypotonicity. In the senior author's experience, gentle blunt dissection with vertically oriented Reynolds scissors and limited sharp dissection can reliably re-elevate the SMAS without causing nerve injury.
MANAGING THE NECK
Similar to the decision regarding the management of prior incisions, treatment of the neck should be based on preoperative findings. If the neck shows good form, no intervention here is necessary. A poorly healed submental scar should be excised, at a minimum. If submental fat is excessive, liposuction or direct lipectomy is necessary. Platysmal banding, if present, is treated by corset platysmaplasty, which can also (partially) treat cobra neck deformity. Jowling, new or insufficiently treated by the initial procedure, may be due to submaxillary gland ptosis, and in addition to corset platysmaplasty oblique mattress sutures to tighten the paramedian platysma should be considered. It is important to carefully redrape the cervical skin when complete, as the reduced skin elasticity may require more extensive skin elevation than expected.
REVERSING SOFT TISSUE DEFORMITIES
Hamra observed that lateral sweep results from excessive tension and a lateral vector when using a SMAS flap for facial rejuvenation.11 It is his estimation that over time as the flap loses tension, descent occurs along this lateral vector, leading to disharmony over time. The use of a more superior vector during the secondary rhytidectomy has been shown to reverse this deformity.
Lambros and Stuzin pointed out how the secondary rhytidectomy patient might present with something they call the “cross-cheek depression” or “joker's lines,” which appears as a shadow from the oral commissure to the ear.12 They believe that this distortion is seen in patients who are morphologically prone because of strong malar prominence and a submalar hollow. These patients preoperatively have a mild version of this deformity, and it is likely unmasked by the correction of aging. Although a strong cheek ogee and submalar hollow are youthful and pleasing, this shadow can be very disharmonious. Correction of this deformity is achieved by soft tissue augmentation of the shadow to restore some submalar fullness.24
Smile block is a recently described entity in which the patient appears to have a hypodynamic cheek mound or facial fat that does not move appropriately with animation. It is unclear whether this is due to plication sutures placed too anteriorly, tethering the SMAS and zygomaticus major muscle, or blocking of facial fat and fascia by sutures and scar tissue.25 Similar to the “joker line,” treatment of smile block is achieved with soft tissue augmentation around the area that appears “blocked,” creating a more smooth appearance.26
CORRECTION OF HAIRLINE DISTORTION
A posttrichial temporal incision with aggressive superolateral flap advancement can distort or obliterate the sideburn and temporal hair tuft (Fig. 1). Though hairstyling can camouflage this deformity, a pretrichial incision could have prevented it. Secondary rhytidectomy must avoid exacerbating this situation by utilizing a pretrichial incision, and postoperative microfollicular hair transplantation should be incorporated into the treatment plan to maximally reconstruct a proper hairline. Widened and visible temporal scars can also be treated with hair transplantation when scar excision is not feasible.
Figure 1.
Visible occipital and temporal scars 15 years after rhytidectomy by a noted surgeon that required specific hairstyling for camouflage. Note the distorted appearance caused by posterosuperior transposition of temporal hair and loss of sideburn.
Occipital hairline deformities (Fig. 2) include widened scars in hair-bearing skin, visible hairline scars, or hairline step-offs. These can be corrected by scar excision, appropriate flap advancement/rotation to restore the normal visual continuity of the hairline, and meticulous layered closure. Focal hair transplantation postoperatively should be reserved for persistent deformities.
Figure 2.
(A) Obvious step-off of the occipital hairline after rhytidectomy caused by poor alignment of the transposed face-lift flap. (B) Hypertrophic scar with sublobular portion.
CORRECTION OF EAR DEFORMITIES
Ear deformities are not uncommon after rhytidectomy. It has been shown by retrospective reviews of plastic surgery practices that auricular displacement occurs in 64% of rhytidectomy patients postoperatively.27 It is likely that excess tension on the ear during healing leads to the caudal and sometimes anterior malposition of the ear.28 These problems are exacerbated by the fact that redraping of the facial soft tissues in a more youthful position causes a disharmonious contrast between the corrected face and the ptotic ear position. Pixie ear deformity describes the loss of ear lobule definition, with the helical curve blending directly into the cheek.29,30 Many methods have been devised to correct it: simple wedge excision and lobule re-creation31; triangular excision with wedge closure 32,33; lobular suturepexy with no tissue excision.34 Prevention of these ear deformities has also been discussed: McKinney et al advised cephalad overrotation of the lobule during inset at the closure of the incisions35; Barton recommends dividing the excess SMAS flap and replacing it behind the ear to brace the ear in addition to further definition of the jawline.36 In the authors' experience, this transposition of a portion of the SMAS flap posteriorly with anchorage to the mastoid periosteum can provide significant superior flap support during healing. Additionally, a semipermanent suture placed between the inferior portion of the SMAS incision and the deep aspect of the conchal cartilage can assist in defining the lobular notch. To this can be added cephalad overrotation of the earlobe during skin closure, as described by McKinney et al (Fig. 3).
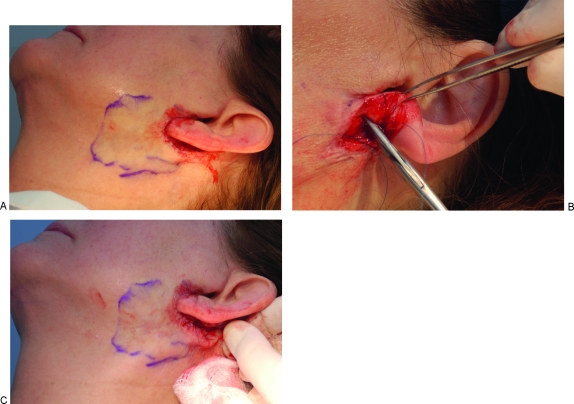
Figure 3.
(A) For correction of a pixie ear deformity, a perilobular incision is made and a small flap (limits shown by markings) is elevated inferiorly and posteriorly. (B) A suture is passed from the SMAS/scar inferiorly and anchored to the perichondrium of the inferior portion of the conchal bowl superiorly. (C) Tightening of this suture advances the flap superiorly, providing stability as well as generating sufficient redundancy to allow overrotation of the earlobe during closure.
In some cases where a retrotragal incision is used, the tragus can become anteriorly rotated, especially in patients with soft and pliable tragal cartilage, leading to an unsightly exposure of the external auditory meatus and canal. Additionally, the tragus can become bulky and blunted. Retrotragal incisions should not be used in any patient with a pliable or anteriorly rotated tragus. The lateral cheek skin redraped over the tragus at the end of the case is always thicker than the natural tragal skin and should be carefully defatted prior to closure to avoid a “plump” tragus. Finally, prior to tragal skin closure, an absorbable “tacking” suture should be placed between the dermis and soft tissue just anterior to the tragal root to better define a pretragal sulcus that visually distinguishes the lateral cheek from the tragus.
CONCLUSION
Patients may seek revision rhytidectomy as a result of operator failure, technique failure, or simply because of the inexorable progression of aging. Revision face-lift can be performed but may present additional problems and challenges compared with primary face-lifts. It is critical preoperatively to help the patient determine appropriate and achievable goals and expectations. Correction of face-lift stigmata with modest rejuvenative changes may be a more appropriate goal than aggressive skin redraping with persistent surgical deformities. An approach of “Underpromise, Overdeliver” is certainly appropriate for the typical revision rhytidectomy. However, with thoughtful planning, excellent and reliable results are obtainable.
REFERENCES
- American Society for Aesthetic Plastic Surgery 2007 Annual Statistics. Available at: http://www.surgery.org/download/2008stats.pdf. Accessed 10/14/09. Available at: http://www.surgery.org/download/2008stats.pdf
- MEDLINE. Available at: www.pubmed.gov. Accessed February 26, 2009. Available at: www.pubmed.gov
- Rohrich R J, Ghavami A, Lemmon J A, Brown S A. The individualized component face lift: developing a systematic approach to facial rejuvenation. Plast Reconstr Surg. 2009;123:1050–1063. doi: 10.1097/PRS.0b013e31819c91b0. [DOI] [PubMed] [Google Scholar]
- Millard D R, Jr, Yuan R T, Devine J W., Jr A challenge to the undefeated nasolabial folds. Plast Reconstr Surg. 1987;80:37–46. doi: 10.1097/00006534-198707000-00006. [DOI] [PubMed] [Google Scholar]
- Guyuron B, Bokhari F, Thomas T. Secondary rhytidectomy. Plast Reconstr Surg. 1997;100:1281–1284. doi: 10.1097/00006534-199710000-00033. [DOI] [PubMed] [Google Scholar]
- Lambros V. Models of facial aging and implications for treatment. Clin Plast Surg. 2008;35:319–327. discussion 317. doi: 10.1016/j.cps.2008.02.012. [DOI] [PubMed] [Google Scholar]
- Connell B F. Eyebrow, face, and neck lifts for males. Clin Plast Surg. 1978;5:15–28. [PubMed] [Google Scholar]
- Knize D M. Periauricular face lift incisions and the auricular anchor. Plast Reconstr Surg. 1999;104:1508–1520. discussion 1521–1523. [PubMed] [Google Scholar]
- Hoefflin S M. Simple repair of a pixie earlobe. Plast Reconstr Surg. 2001;107:1623–1624. [PubMed] [Google Scholar]
- Little J W. Hiding the posterior scar in rhytidectomy: the omega incision. Plast Reconstr Surg. 1999;104:259–272. discussion 273–276. [PubMed] [Google Scholar]
- Hamra S T. Frequent face lift sequelae: hollow eyes and the lateral sweep: cause and repair. Plast Reconstr Surg. 1998;102:1658–1666. doi: 10.1097/00006534-199810000-00052. [DOI] [PubMed] [Google Scholar]
- Lambros V, Stuzin J M. The cross-cheek depression: surgical cause and effect in the development of the “joker line” and its treatment. Plast Reconstr Surg. 2008;122:1543–1552. doi: 10.1097/PRS.0b013e31818894d3. [DOI] [PubMed] [Google Scholar]
- Hamra S T. Correcting the unfavorable outcomes following facelift surgery. Clin Plast Surg. 2001;28:621–638. [PubMed] [Google Scholar]
- Mendelson B C. Surgery of the superficial musculoaponeurotic system: principles of release, vectors, and fixation. Plast Reconstr Surg. 2001;107:1545–1552. discussion 1553–1555, 1556–1557, 1558–1561. [PubMed] [Google Scholar]
- Schwartz R J, Burns A J, Rohrich R J, Barton F E, Jr, Byrd H S. Long-term assessment of CO2 facial laser resurfacing: aesthetic results and complications. Plast Reconstr Surg. 1999;103:592–601. doi: 10.1097/00006534-199902000-00037. [DOI] [PubMed] [Google Scholar]
- Taylor G I, Corlett R J, Caddy C M, Zelt R G. An anatomic review of the delay phenomenon: II. Clinical applications. Plast Reconstr Surg. 1992;89:408–416. discussion 417–418. [PubMed] [Google Scholar]
- Guyuron B. Secondary rhytidectomy. Plast Reconstr Surg. 2004;114:797–800. doi: 10.1097/01.prs.0000131239.60718.85. [DOI] [PubMed] [Google Scholar]
- Cerda E. Mechanics of scars. J Biomech. 2005;38:1598–1603. doi: 10.1016/j.jbiomech.2004.07.026. [DOI] [PubMed] [Google Scholar]
- Mentz H A, III, Ruiz-Razura A, Patronella C K, Newall G. Facelift: measurement of superficial muscular aponeurotic system advancement with and without zygomaticus major muscle release. Aesthetic Plast Surg. 2005;29:353–362. doi: 10.1007/s00266-005-0005-4. [DOI] [PubMed] [Google Scholar]
- Har-Shai Y, Bodner S R, Egozy-Golan D, et al. Mechanical properties and microstructure of the superficial musculoaponeurotic system. Plast Reconstr Surg. 1996;98:59–70. discussion 71–73. doi: 10.1097/00006534-199607000-00009. [DOI] [PubMed] [Google Scholar]
- Kissmeyer A, With C. Clinical and histological studies on the pathological changes in the elastic tissues of the skin. Br J Dermatol. 1922;34:175–194. [Google Scholar]
- Hwang K, Lee D K, Lee E J, Chung I H, Lee S I. Innervation of the lower eyelid in relation to blepharoplasty and midface lift: clinical observation and cadaveric study. Ann Plast Surg. 2001;47:1–5. discussion 5–7. doi: 10.1097/00000637-200107000-00001. [DOI] [PubMed] [Google Scholar]
- Lowe J B, III, Cohen M, Hunter D A, Mackinnon S E. Analysis of the nerve branches to the orbicularis oculi muscle of the lower eyelid in fresh cadavers. Plast Reconstr Surg. 2005;116:1743–1749. discussion 1750–1751. doi: 10.1097/01.prs.0000186532.29557.96. [DOI] [PubMed] [Google Scholar]
- Lambros V. Overcorrection/undercorrection and the iatrogenic deformity of the neck following rhytidectomy. Las Vegas, NV: Presented at: Annual Meeting of the American Society of Aesthetic Plastic Surgeons; May 2009.
- Hatef D A, Hollier L H, Bullocks J M, Stal S. Smile block after rhytidectomy: a dynamic investigation into its cause. Las Vegas, NV: Presented at: Annual Meeting of the American Society of Aesthetic Plastic Surgeons; May 2009.
- Lambros V. Personal communication. Las Vegas, NV: Presented at: Annual Meeting of the American Society of Aesthetic Plastic Surgeons; May 2009.
- Brink R R. Auricular displacement with rhytidectomy. Plast Reconstr Surg. 2001;108:743–752. doi: 10.1097/00006534-200109010-00022. [DOI] [PubMed] [Google Scholar]
- McKinney P, Giese S, Placik O. Management of the ear in rhytidectomy. Plast Reconstr Surg. 1993;92:858–866. [PubMed] [Google Scholar]
- McGregor M W, Greenberg R L. In: Goldwyn RM, editor. The Unfavorable Result in Plastic Surgery. Boston, MA: Little, Brown; 1972. Rhytidectomy. pp. 173–179.
- Baker T J, Gordon H L. Complications of rhytidectomy. Plast Reconstr Surg. 1967;40:31–39. doi: 10.1097/00006534-196707000-00004. [DOI] [PubMed] [Google Scholar]
- Rich J D, Gottlieb V, Shesol B F. A simple method for correction of the pixie earlobe. Plast Reconstr Surg. 1982;69:136–138. [PubMed] [Google Scholar]
- Khoo B C. The pixie earlobe: a method of correction. Plast Reconstr Surg. 1985;76:636–638. [PubMed] [Google Scholar]
- Mowlavi A, Meldrum D G, Wilhelmi B J, Russell R C, Zook E G. The “pixie” ear deformity following face lift surgery revisited. Plast Reconstr Surg. 2005;115:1165–1171. doi: 10.1097/01.prs.0000156140.38695.5e. [DOI] [PubMed] [Google Scholar]
- Hoefflin S M. Simple repair of a pixie earlobe. Plast Reconstr Surg. 2001;107:1623–1624. [PubMed] [Google Scholar]
- McKinney P, Giese S, Placik O. Management of the ear in rhytidectomy. Plast Reconstr Surg. 1993;92:858–866. [PubMed] [Google Scholar]
- Barton F E., Jr Personal communication. Dallas, TX: Presented at: University of Texas Southwestern Department of Plastic Surgery Weekly Conference; March 2008.