Coronary artery bypass surgery (CABS) patients often experience many symptoms during their early recovery over the first three months after hospital discharge. It is common for CABS patients to experience multiple symptoms simultaneously, rather than just isolated symptoms.1,2 Anxiety and depression are among the most commonly occurring symptoms that affect psychosocial recovery following CABS.3,4 The presence of these symptoms is predictive of increased morbidity and mortality within the first six months after CABS.5–7 Therefore, it is crucial to examine psychosocial recovery in order to improve patients' overall health and health related quality of life (HRQoL). However, there has been limited research that has examined the types of simultaneously occurring symptoms during recovery after CABS in relation to other patient characteristics (e.g. gender, marital status, comorbidities). Furthermore, the literature is lacking in regards to how multiple symptoms impact the recovery of elderly CABS patients. An approach to take to further examine multiple symptoms occurring simultaneously among elderly CABS patients is to examine symptoms within a cluster; as multiple symptoms can influence one another, and various cluster subgroups may impact recovery outcomes. This is important because according to the AHA (2008), over 50% of the total CABS performed in 2005 were on patients over age 65 years.8 Although the process of aging has been suggested as the reason for alterations in symptoms and recovery delays,9 there is a dearth of information available on the trajectory of symptoms experienced following CABS and any age-related impact. Therefore, the purpose of these secondary analyses were to identify and describe subgroups of elderly CABS patients based on their symptom profile and examine how psychosocial functioning differed by symptom cluster subgroups over time (at discharge, 6-weeks and 3-months after CABS).
BACKGROUND
Several concepts from the Theory of Unpleasant Symptoms were used to guide this study examining symptom clusters among elderly CABS patients at discharge.10 The main assumptions behind this theory are that several interacting symptoms (e.g., SOB and fatigue) may occur simultaneously and impact important patient outcomes (e.g., functioning). This theory also addresses factors influencing symptoms and gives consideration to them when examining symptom clusters.11 The theory components include the symptoms experienced, influential factors that contribute to and affect symptoms, and the consequences of the experience. Each symptom experienced is multidimensional and can be measured by its intensity, timing, level of distress, and quality. In the database used for these secondary analyses, symptom frequency and severity were measured. These correspond with symptom timing and intensity as measured by the Theory of Unpleasant Symptoms. The timing and intensity scores were analyzed as a mean score prior to discharge from the hospital. Influential factors are factors that influence the intensity and timing of the symptoms and are divided into physiological (related to one's health e.g., comorbidities and baseline functioning) and situational (aspects of one's social and physical environment e.g., gender and marital status). These influential factors were used in this study to profile the individuals who experience various symptom clusters. The consequences component was operationalized as outcomes for this study.
Symptoms Experienced
Following CABS, patients often report shortness of breath, fatigue, depression, trouble sleeping, incision pain, lower extremity edema (swelling), anxiety, and poor appetite in the early recovery period. These symptoms usually persist up to three months following discharge and can interfere with both physiological and psychosocial recovery outcomes; with the symptoms typically dissipating over time.1,2,12,13 Patients experiencing more symptoms reported poorer psychosocial functioning than those with fewer symptoms.14
Influential Factors
Many influential factors (e.g. age, functional capacity, self-efficacy, and gender) impact symptoms and psychosocial functioning following CABS. Older adults over age 65 compared to younger CABS usually report the presence of more symptoms.2,6,15,16 Symptoms experienced also differ by gender,9,13,17–20 level of education,18,19 number of comorbidities,21,22 baseline level of functioning,19,23 and marital status.13,19,23,24 Preoperative status and functional capacity were found to negatively impact postoperative functioning;25,26 with variability in functional outcomes being explained by self-efficacy rather than by disease severity, functional capacity, comorbidity, or preoperative functioning.27
Consequences/Outcomes
Psychosocial functioning is one type of consequence or outcome of the symptom experience. In several studies, psychosocial functioning was found to decline in the early-recovery period after CABS, and was negatively influenced by the presence of early recovery symptoms such as depression18,28 and sleep disruption.29 In a study of elderly CABS patients (N = 72), by Doering, patients with more depressive symptoms reported significantly poorer emotional recovery (p < 0.001) than those with fewer symptoms.28 Higher levels of depressive symptoms assessed prior to CABS were also found to be a strong predictor (p < 0.0001) for poorer functional recovery six months following surgery in a large study by Mallik of first-time CABS patients (N = 963) after controlling for disease severity, angina class, baseline physical subscale scores of the Medical Outcome Study (MOS) SF-36, and medical history.18 Edell-Gustafsson found that sleep disruption accounted for 44.5% of the variance in quality of life and psychosocial functioning among men (N=38) after CABS who suffered from anxiety and depressive symptoms.29
In contrast, other researchers have reported psychosocial functioning improved over time after CABS.30,31 Researchers studied the functional status of 47 CABS patients over time and found that psychosocial functioning (e.g., social and mental functioning) significantly improved (p < 0.0001) over time, at 3, 6 and 12-months after CABS.30 Similarly, Barry et al. reported significant improvements in psychosocial functioning (p < 0.01) over time among subjects (n=1072) following CABS.31
Symptom Clusters
Symptom clustering is an emerging area of study in nursing. Symptom clusters have been defined as consisting of two or more symptoms that are related to one another and occur simultaneously.32,33 Symptom cluster research has been conducted in oncology, medical-surgical, mental health, and cardiac populations using a variety of statistical methods including hierarchical cluster analysis,34,35 latent cluster analysis,36 factor analysis,11,37 and regression analysis.38,39 A few studies have examined symptom clusters in cardiac populations,34,36,37 but none have specifically analyzed symptom clusters in the CABS population. Correlations reported between symptoms experienced among patients following CABS have provided the foundation for study of symptom clusters in this population.1,6,40
In summary, psychosocial recovery is an important component of CABS patients' improvement in health and overall health related quality of life. Based on previous studies, symptoms may dissipate over time, however, the persistence of symptoms and relationship between symptoms occurring simultaneously need to be further examined. Therefore, the use of symptom clustering analysis can be beneficial to identify those patient profiles that may be at risk for delayed or impaired psychosocial functioning following CABS. The specific aims of this study were to: 1) identify and describe cluster subgroups of elderly CABS patients based on symptom intensity/timing of eight early recovery symptoms (shortness of breath, fatigue, depression, trouble sleeping, incision pain, lower extremity edema (swelling), anxiety, and poor appetite) at baseline (prior to discharge); and 2) determine if these cluster subgroups varied on demographic (age, gender, marital status, work status, and years of education) and clinical characteristics [history of congestive heart failure (CHF), hypertension, and/or diabetes, New York Heart Association Classification (NYHA), Charlson Comorbidity Index (CCI), Duke Activity Status Index (DASI), self-efficacy (Barnason Efficacy Expectation Scale [BEES]), and Hospital Anxiety and Depression Scale (HADS)] at baseline; and 3) examine how these cluster subgroups influenced psychosocial functioning [role-emotional, social, and mental subscales of the MOS SF-36] over time (at 3 and 6 weeks and 3 months after discharge).
METHODS
Design and Sample
Descriptive, secondary analyses were conducted on elderly CABS patients (N = 226) aged 65 years and older who had elective surgery and participated in a larger randomized clinical trial (RCT). Although 280 patients were enrolled in the original study, only 226 met the inclusion criteria of having complete data for the three months after hospitalization. Patients in the larger, parent study met the following criteria: (a) 65 years of age or older who underwent CABS; (b) discharged within seven days following CABS; and (c) no physical impairments that would limit physical functioning following surgery.
Variables/Measures
Measures of Symptoms for Cluster Analyses
The Cardiac Symptom Survey (CSS) was used to measure subjects' symptoms prior to hospital discharge. It consists of a 40-item scale, which measures symptom presence, symptom evaluation (or burden) and symptom response to 10 symptoms which commonly occur among post-CABS patients. The frequency and severity of symptoms (ranging from 0 or no symptom to 10 most severe/intense symptom frequency and severity) were determined with a mean timing/intensity score computed for each symptom prior to discharge. Test-retest correlations for this survey were acceptable for each symptom (0.85 to 1.0), as was internal consistency (0.85 to 0.98) over time.41 The symptoms of angina and fluttering, although addressed in the CSS, were not used in the analyses in this study as few subjects reported these symptoms.
Measures of Demographic and Clinical Characteristics
Data were gathered prior to hospital discharge on the following: age, gender, marital status, work status, education level, and type of procedure, NYHA classification, ejection fraction, cardiac history (e.g., myocardial infarction, CHF), cardiac disease risk factors (e.g., hypertension, diabetes, tobacco use). In addition, subjects' comorbidities were measured using the Charlson Comorbidity Index (CCI). The CCI is a weighted index that is summed based on the number and seriousness of comorbid diseases.42 The total score (range: 0–37) was determined prior to discharge for these analyses. The Duke Activity Status Index (DASI), which measures functional capacity, was used to measure physiological functioning. The DASI is a 12-item self-rating, disease-specific questionnaire.43 Weighted scores determined by the metabolic demand of activities are used as a proxy measure to predict peak oxygen consumption (VO2) with higher scores (range: 0 – 58) representing higher capacity. Initial correlations of 0.81 were reported between DASI total score and (VO2). The DASI has been used with a variety of cardiovascular disorders, including CABS.44–46 Means reported in the literature for DASI in cardiac populations ranged from 20 to 27.8.43,47,48
Measures of Anxiety and Depression Clinical Characteristics
The Hospital Anxiety and Depression Scale (HADS)49 was used to measure states of anxiety and depression. The scale consists of subscales for anxiety and depression (7 items each) and ranges in score of 0 to 21 for each subscale. Higher subscale scores indicate greater levels of anxiety and depression. Factor analyses have verified the 2-factor scale, and reliability has been estimated by Cronbach's alpha (range from .68 to .93 for the Hospital Anxiety and Depression Scale-Anxiety Subscale (HADS-A) and from .67 to .90 for the Hospital Anxiety and Depression Scale-Depression Subscale (HADS-D) in numerous populations).50
Measure of Self-Efficacy Clinical Characteristics
The Barnason Efficacy Expectation Scale (BEES), consisting of 15 Likert-scale items (range: 15–60), was used to determine the patient's self-efficacy related to aspects of recovery and lifestyle adjustment after CABS (physical functioning, psychosocial functioning, coronary artery disease risk factor modification and self-care management).51 Reported internal consistency reliability of the instrument was 0.93 and principal components analysis revealed a single factor (Eigenvalue = 10.59, percent variance = 70.61%).
Measures of Psychosocial Functioning
The psychosocial functioning subscales of the MOS SF- 36, a generic, multidimensional scale (range: 0–100) that measures both physical and psychosocial functioning, was used.52 Internal consistency reliability alphas have been reported in the literature from 0.67 to 0.93.53–57 In this study, the role-emotional, social, and mental subscales were used as measures of psychosocial functioning.
PROCEDURES
Institutional review board approval was obtained prior to conducting the secondary analysis. Demographics were obtained from the database created for the parent study. All data were entered into a secure online database that facilitated ease of downloading into statistical programs used for the analyses in this study.
DATA ANALYSIS
In this study, SAS 9.1 was used for data analyses, along with the R 2.8.1 statistical program being specifically used for the cluster analyses. An overall α level was set at 0.05 for all analyses. Descriptive statistics were used to describe the sample and the symptom cluster profiles. The model-based clustering method (MBCM) was performed using the R program to determine the number clusters in the CABS sample (Aim 1), as this technique has been shown to provide the most consistent results.58 The R program is a free software environment for statistical computing and graphics and it was selected because the MBCM package was originally created based on the R platform. Chi-Square and analysis of variance (ANOVA) with Bonferroni adjustments for multiple comparisons using SAS were used to determine if there were differences between clusters on baseline demographic and clinical factors (Aim 2). Repeated measures analyses of variance (RM-ANOVAs) were employed to determine how psychosocial functioning differed by symptom cluster subgroups over time (Aim 3).
FINDINGS/RESULTS
Sample Profile
A total of 226 subjects from the larger RCT parent study were included in this secondary analysis of data. The majority of the sample was married (86 %), with an average age of 71years (SD = 4.96). There were 187 (83 %) males and 39 (17.3 %) females included in the study; they had only a few comorbidities based on the CCI (M=1.13 ± 1.3). The most common risk factors among the study sample were hypercholesterolemia and hypertension both 74%. Further detail on subject characteristics by cluster groups is depicted in Tables 1 and 2.
Table 1.
Demographic and Clinical Characteristics of Study Participants by Patient Clusters (N=226)
| Variable | Category | Cluster 1 (36) | Cluster 2 (130) | Cluster 3 (60) | |||
|---|---|---|---|---|---|---|---|
| Demographic | n | (%) | n | (%) | n | (%) | |
| Marital Status | Married | 32 | 88.9 | 110 | 84.6 | 53 | 88.3 |
| Gender | Male | 33 | 91.7 | 102 | 78.5 | 52 | 86.7 |
| Currently working outside of the home | Yes | 20 | 55.6 | 51 | 39.2 | 31 | 51.7 |
| Clinical | n | (%) | n | (%) | n | (%) | |
|---|---|---|---|---|---|---|---|
| New York Heart Association (NYHA) Classification ** | I | 26 | 72.2 | 64 | 49.2 | 20 | 33.3 |
| II | 10 | 27.8 | 52 | 40 | 31 | 51.7 | |
| III | 0 | 0 | 14 | 10.8 | 8 | 13.3 | |
| IV | 0 | 0 | 0 | 0 | 1 | 1.7 | |
| Ejection Fraction | < 50% | 3 | 8.3 | 25 | 19.4 | 14 | 23.7 |
| Previous Myocardial Infarcton | Yes | 4 | 11.1 | 14 | 10.8 | 7 | 11.7 |
| Diabetes | Yes | 7 | 19.4 | 29 | 22.3 | 15 | 25 |
| Hypertension | Yes | 28 | 77.8 | 90 | 69.2 | 49 | 29.3 |
| CHF | Yes | 1 | .0 | 5 | .1 | 2 | .0 |
| High cholesterol | Yes | 27 | 75 | 92 | 70.8 | 47 | 78.3 |
| History of Tobacco Use | Yes | 17 | 47.2 | 71 | 54.6 | 27 | 45 |
| History of Smokeless Tobacco | Yes | 0 | 0 | 6 | 4.7 | 1 | 1.7 |
| Family History of Coronary Artery Disease | Yes | 23 | 63.9 | 98 | 76 | 37 | 61.7 |
p-value < 0.05
p-value < 0.01
p-value <0.0001
Table 2.
Means and Standard Deviations for Additional Variables by Symptom Burden Cluster Subgroups (N=226)
| Variable | Cluster 1 (n=36) | Cluster 2 (n=130) | Cluster 3 (n=60) | |||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | |
| Length of Hospital Stay | 5.0 | 1.2 | 5.5 | 1.2 | 5.6 | 0.9 |
| Age | 71.1 | 4.9 | 71.5 | 5.2 | 70.8 | 4.6 |
| Education | 12.5 | 2.9 | 13.4 | 2.9 | 13.2 | 2.7 |
| Charlson Comorbidity Index (CCI) | 1.1 | 1.3 | 1.0 | 1.2 | 1.4 | 1.3 |
| Hospital Anxiety & Depression Scale (HADS)*** (range 0–21) | 5.9 | 4.3 | 8.2 | 4.8 | 11.8 | 6.9 |
| BEES*** (range 15–60) | 51.7 | 6.6 | 48.6 | 8.0 | 44.9 | 7.5 |
| Duke Activity Status Index (DASI)* (range 0–58) | 26.6 | 5.9 | 24.3 | 6.2 | 22.4 | 6.8 |
p-value < 0.05
p-value < 0.01
p-value <0.0001
Identification of Cluster Subgroups
Based on the results of t-tests, eight symptoms, as measured by the Cardiac Symptom Survey, were used to classify the subgroups of patients after CABS. Results of MBCM demonstrated that there were three patient clusters and the largest BIC value was −7437.67. Table 3 depicts the mean symptom burden scores for each of the three clusters.
Table 3.
Mean Score Comparison for Pre-Discharge Symptoms by Symptom Burden Cluster Groups (N = 226)
| Pre-Discharge Symptoms | Low Symptom Burden Cluster Group (n = 36) | Low - Moderate Symptom Burden Cluster Group (n = 130) | Moderate Symptom Burden Cluster Group (n = 60) | |||
|---|---|---|---|---|---|---|
| Means | SD | Means | SD | Means | SD | |
| Shortness of Breath | 0 | 0 | 0.63 | 1.21 | 2.59 | 2.91 |
| Fatigue | 0.11 | 0.46 | 1.90 | 2.21 | 4.60 | 3.39 |
| Depression | 0 | 0 | 0.07 | 0.34 | 2.46 | 2.38 |
| Trouble Sleeping | 0.08 | 0.37 | 2.07 | 3.06 | 4.27 | 3.54 |
| Incision Pain | 0.44 | 0.67 | 1.36 | 1.60 | 2.88 | 2.49 |
| Edema (Swelling) | 0.08 | 0.35 | 2.14 | 2.70 | 2.55 | 2.96 |
| Anxiety | 0 | 0 | 0.40 | 0.96 | 3.36 | 3.04 |
| Poor Appetite | 0.83 | 1.43 | 3.05 | 3.34 | 4.48 | 3.82 |
Furthermore, by categorizing the symptom severities into categories: Low (0–2), moderate (>2), one could construct the cluster profile of each symptom cluster. Table 3 depicts the three cluster symptom burden groups as Cluster 1 low symptom burden on all 8 symptoms, Cluster 3 moderate symptom burden on all 8 symptoms, and Cluster 2 as a combination of low (shortness of breath, fatigue, depression, incision pain, anxiety) and moderate (sleep problems, lower extremity edema [swelling], and appetite problems) symptom burden.
Cluster Subgroup Characteristics
Using ANOVAs and Chi-Square tests, there were significant differences in clinical characteristics detected between clusters on physiological functioning measured by the DASI [F (2, 223) = 5.12; p = 0.007] and the NYHA classification (χ2 = 17.44; p = 0.008); self-efficacy measured by the BEES [F (2, 223) = 9.60; p < 0.0001]; and anxiety and depression measured by HADS [F (2, 219) = 15.14; p < 0.0001]. Using Bonferroni follow-up analyses, differences in DASI scores (p = 0.005) and NYHA classification (p = 0.006) were noted between the low and the moderate symptom burden cluster groups; indicating that those with higher physical functioning had minor symptoms in comparison to those with lower physical functioning who had higher symptom timing and intensity or were more challenged in the early recovery period after CABS. The low and moderate symptom burden cluster groups also differed on mean scores for self-efficacy (as measured by the BEES) and for anxiety and depression (as measured by the HADS). Likewise there were also self-efficacy, anxiety and depression differences between the combined low-moderate and the moderate symptom burden cluster groups. Data findings indicated that when self-efficacy was higher, subjects reported lower levels of anxiety and depression.
There were no statistically significant differences between the clusters for the demographic variables of age, level of education; gender, marital status, and work status. Additionally there were no statistically significant differences between the clusters for clinical characteristics of comorbidities; history of CHF; history of hypertension or history of diabetes.
Psychosocial Functioning and Cluster Subgroup
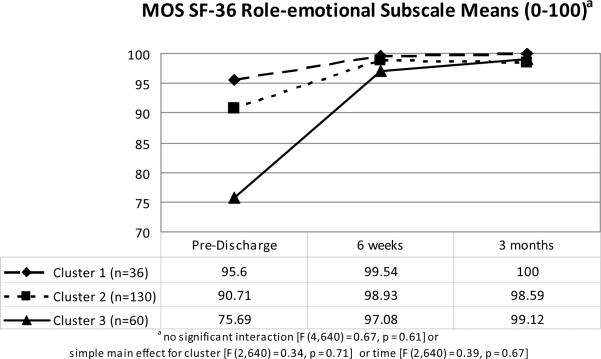
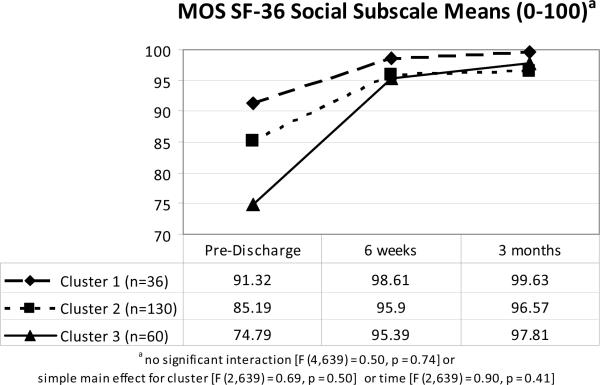
The influence of the cluster groups (low, low-moderate, and moderate symptom burden cluster groups) on psychosocial functioning examined the psychosocial functioning mean scores of the MOS SF-36 subscales (role-emotional, social and mental functioning). There were no significant interactions between (cluster) group* time for either role-emotional or social functioning; nor were there any significant main effects for (cluster) group or for time. Refer to Figures 1 and 2 for an overview of the role-emotional and social functioning mean scores by cluster group over time.
Figure 1.
Mean scores (0–100) for MOS SF-36 role-emotional subscale by cluster
Figure 2.
Mean scores (0–100) for MOS SF-36 social subscale by cluster
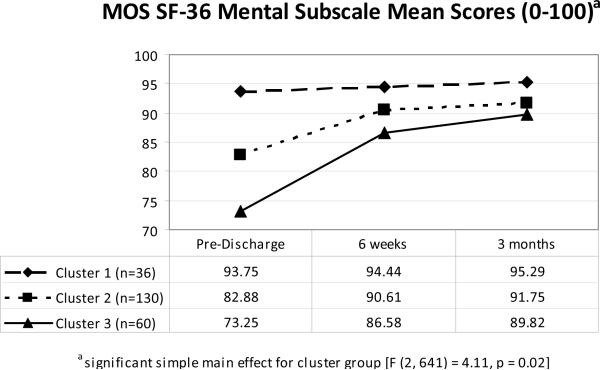
When evaluating the influence of cluster group on the mental functioning scores over time, there was no significant interaction [F (4, 641) = 0.30, p = 0.88]; however, there was a simple main effect for symptom burden cluster group [F (2, 641) = 4.11, p = 0.02] as depicted in Figure 3. Follow-up of simple main effects indicated symptom burden cluster group membership influenced mental functioning scores and improved regardless of time. There were differences between the low and the moderate symptom burden cluster groups (p = 0.01) with those who reported greater symptom timing/intensity scores having lower mental functioning scores. The mental functioning scores were significantly higher, reflecting better psychosocial functioning for those in the low symptom burden cluster group [Cluster 1, estimate 92.80 (0.91)] as compared to those in the moderate symptom burden cluster group [Cluster 3, estimate 89.39(0.71)].
Figure 3.
Mean scores (0–100) for MOS SF-36 mental subscale by cluster
DISCUSSION
This study was conducted to identify and describe subgroups of elderly CABS patients based on symptoms at time of discharge and to examine how these identified symptom cluster subgroups influenced psychosocial functioning over time. The three cluster groups that emerged in this study are congruent with current definitions of a symptom cluster as consisting of two or more symptoms related to one another and occur concurrently32,33,59 with varying mean timing/intensity scores across the clusters.
Significant differences were detected at baseline between the clusters on physiological functioning (DASI and NYHA) and self-efficacy (BEES) and anxiety and depression (HADS). In this study the low and moderate symptom burden cluster groups differed, indicating that those with lower levels of symptoms and higher physiological functioning experienced less anxiety and depression at time of hospital discharge, and greater self-efficacy for managing their recovery following CABS than those with the moderate symptom burden cluster group. Significant differences were also noted between the low- moderate and the moderate symptom burden cluster groups for the BEES and HADS with those having the low-moderate symptom burden cluster reporting lower anxiety and depression and greater self-efficacy than those with the moderate symptom burden cluster. This finding is consistent with the literature, as depression is common among patients with more symptoms, chronic illnesses, and among the elderly.6,28,60 In this study anxiety and depression was associated with more symptoms, findings which are congruent with other researcher who have reported that anxiety is known to contribute to symptom exacerbation and poor psychosocial outcomes following CABS.14,16,61
There were no significant interaction effects noted for any of the psychosocial functioning variables over time. However, there was a simple main effect by symptom burden cluster group for mental functioning indicating that regardless of time, cluster membership significantly influenced mental subscale scores. Those with higher symptom scores also had higher mental functioning scores as measured with the MOS SF-36. Overall, the adjusted mean scores for each symptom burden cluster group [Cluster 1 M=93, Cluster 2 M=91, and Cluster 3 M=89] were higher in this study than previously reported in the literature, with mean scores ranging from 65 to 69 for mental functioning.25,26,45,62,63 Based on previous research, mental functioning (reflective of depressive symptoms) has been found to significantly predict postoperative psychosocial functioning over time.31,61,64,65 This measure of psychosocial functioning subscale, along with the HADS (also highest in those with higher symptom scores), could be a useful tool to identify those patients at risk for clinicians to intervene because we know that depression and anxiety negatively influence functioning,60,28,60 other recovery outcomes such as mortality and adverse cardiac events,5,7,7 and wound healing.28
LIMITATIONS
There are several limitations that need to be acknowledged. This study was a secondary analysis with different purposes than the parent study, therefore there was no control over data collection and the variables included, and symptoms were only measured through a self-reported tool. Findings of this study have limited generalizability as the sample of this study was a homogenous, convenience sample of primarily elderly Caucasian males who had undergone CABS. The study sample had relatively few comorbidities, as reflected by the limited number of subjects who had CHF or diabetes, thus limiting the generalizability to other patient populations.
CONCLUSIONS
In the CABS population three different cluster groups were identified as low, low-moderate, and moderate symptom burden clusters; and were characterized by higher physiological functioning, greater self-efficacy, lower anxiety and depression, and greater psychosocial functioning (mental) than those in the other two clusters. The moderate symptom burden cluster group had higher symptom scores (including anxiety and depression) and lower physiological functioning and self-efficacy than did the other two clusters. Overall, these clusters may provide new insight for nurses in assessing, intervening, and studying early recovery symptoms in older adults following CABS, in order for tailored discharge planning being initiated for those patients who are at-risk for delayed psychosocial functioning (higher levels of psychosocial symptoms and lower physiological functioning).
IMPLICATIONS FOR PRACTICE AND RESEARCH
The results of this study have implications for both clinicians and researchers. First, clinicians must be informed that symptom clusters have been identified in elderly, post-CABS patients and specifically which early recovery symptoms had the highest mean timing/intensity scores by cluster groups. Although this is just a start, these symptom clusters have the potential for providing further evaluation of multiple, concurrently occurring symptoms in this population. Assessments of these symptoms could be completed prior to discharge and would enable clinicians to stratify those patients at risk for impaired recovery after CABS. Clinicians can use this data for early identification of at-risk individuals who may need assistance and in guiding discharge planning as well as management of all symptoms (as there were strong correlations of most symptoms) after dismissal. Categorizing patients with various levels of symptom burden clusters may aid the clinician to provide education on various strategies aimed at reducing symptom burden, as well as information on when to notify a physician of frequently occurring or increasing numbers of symptoms. Ideally, clinicians could more specifically tailor to what the patient needs at discharge or in the early recovery period rather than everyone receiving the same, generic information. For example, by knowing that individuals stabilize in regards to the mental functioning at six weeks following CABS, interventions designed to improve mental status must be delivered and encouraged prior to this time especially for those patients with the moderate symptom burden cluster who experienced less psychosocial improvement than those in the other symptom burden clusters. Such strategies may include teaching the patients what to do if symptoms worsen, providing patients with resources and contact people to whom questions and worries could be expressed, and to help patients identify personal coping strategies to use when feelings of anxiety and/or depression worsen. Subsequently, this information could potentially be used to support the development of protocols and guidelines for CABS patients' recovery and could impact policy for reimbursement for follow-up care by supporting services and resources for selected, high-risk groups of CABS patients.
Study findings also have implications for researchers. Cluster research is in its infancy. Overall, the results of this study provide beginning insights into symptom clusters in elderly, patients after CABS and support the need for future studies to be designed to assure adequate distribution of influential factors. Through profiling those at-risk patients, researchers can focus their attention and healthcare resources on designing and testing tailored interventions to address patients' management of the symptom clusters, rather than just a single symptom, for improving recovery outcomes including psychosocial functioning over time. Other research is needed to determine relationships among symptoms within the clusters; specifically, if there is a biological basis for these symptoms in the CABS populations as suggested by researchers studying symptom clusters in oncology populations.66,67 This work may enhance knowledge and understanding of the etiology, pathophysiology, and influential factors that underlie various symptoms in CABS populations ultimately advancing the science of symptom management. When a deeper, foundational understanding of why and how symptoms cluster is gained, a better understanding of how clusters influence psychosocial as well as physiological outcomes will also emerge for CABS and other populations. Finally, additional studies are needed to determine which symptoms constitute a “true” cluster so that to researchers can test if these clusters are replicable, using this and other statistical tests in other higher risk, more diverse post-CABS (or other cardiac) populations since this was not the intent of the original parent study.
Summary and Implications.
Low, Low - Moderate and Moderate Symptom Burden Cluster Subgroups were identified in this CABS population based on mean symptom timing/intensity scores.
Those with low mean symptom burden cluster scores and higher physiological functioning experienced less anxiety and depression while in the hospital and greater self-efficacy than those with the moderate symptom burden cluster.
A simple main effect for cluster was found in the mental subscale indicating that regardless of time, cluster group membership significantly impacted mental subscale scores.
By profiling those CABS patients at risk for delayed psychosocial recovering following CABS, researchers can focus healthcare resources on designing and testing tailored protocols to target those patients at risk for impaired psychosocial recovery.
Footnotes
This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Gallagher R, McKinley S, Dracup K. Post discharge problems in women recovering from coronary artery bypass graft surgery. Aust Crit Care. 2004;17(4):160–165. doi: 10.1016/s1036-7314(04)80021-3. [DOI] [PubMed] [Google Scholar]
- 2.Miller KH, Grindel CG. Comparison of symptoms of younger and older patients undergoing coronary artery bypass surgery. Clin Nurs Res. 2004;13(3):179–93. doi: 10.1177/1054773804265693. discussion 194–8. [DOI] [PubMed] [Google Scholar]
- 3.Duits AA, Duivenvoorden HJ, Boeke S, et al. A structural modeling analysis of anxiety and depression in patients undergoing coronary artery bypass graft surgery: A model generating approach. J Psychosom Res. 1999;46(2):187–200. doi: 10.1016/s0022-3999(98)00046-4. [DOI] [PubMed] [Google Scholar]
- 4.Gallo LC, Malek MJ, Gilbertson AD, Moore JL. Perceived cognitive function and emotional distress following coronary artery bypass surgery. J Behav Med. 2005;28(5):433–442. doi: 10.1007/s10865-005-9010-y. [DOI] [PubMed] [Google Scholar]
- 5.Blumenthal JA, Lett HS, Babyak MA, et al. Depression as a risk factor for mortality after coronary artery bypass surgery. The Lancet. 2003;362(9384):604–609. doi: 10.1016/S0140-6736(03)14190-6. [DOI] [PubMed] [Google Scholar]
- 6.Burg MM, Benedetto MC, Rosenberg R, Soufer R. Presurgical depression predicts medical morbidity 6 months after coronary artery bypass graft surgery. Psychosom Med. 2003;65(1):111–118. doi: 10.1097/01.psy.0000038940.33335.09. [DOI] [PubMed] [Google Scholar]
- 7.Connerney I, Shapiro PA, McLaughlin JS, Bagiella E, Sloan RP. Relation between depression after coronary artery bypass surgery and 12-month outcome: a prospective study. Lancet. 2001;358:1766–1771. doi: 10.1016/S0140-6736(01)06803-9. [DOI] [PubMed] [Google Scholar]
- 8.American Heart Association [Accessed 3/21, 2008];Heart Disease and Stroke Statistics Update. http://www.americanheart.org/presenter.jhtml?identifier=1928. Published 2008. Updated 2008.
- 9.Hedges C. Sleep, memory, and learning in off-pump coronary artery bypass patients. Res Nurs Health. 2005;28(6):462–473. doi: 10.1002/nur.20101. [DOI] [PubMed] [Google Scholar]
- 10.Lenz ER, Pugh LC, Milligan RA, Gift A, Suppe F. The middle-range theory of unpleasant symptoms: an update. ANS Adv Nurs Sci. 1997;19(3):14–27. doi: 10.1097/00012272-199703000-00003. [DOI] [PubMed] [Google Scholar]
- 11.Gift AG, Jablonski A, Stommel M, Given CW. Symptom clusters in elderly patients with lung cancer. Oncol Nurs Forum. 2004;31(2):202–212. doi: 10.1188/04.ONF.202-212. [DOI] [PubMed] [Google Scholar]
- 12.Zimmerman L, Barnason S, Nieveen J, Schmaderer M. Symptom management intervention in elderly coronary artery bypass graft patients. Outcomes Manag. 2004;8(1):5–12. [PubMed] [Google Scholar]
- 13.Schulz P, Zimmerman L, Barnason S, Nieveen J. Gender differences in recovery after coronary artery bypass graft surgery. Prog Cardiovasc Nurs. 2005;20:58–64. doi: 10.1111/j.0889-7204.2005.03868.x. [DOI] [PubMed] [Google Scholar]
- 14.Oxlad M, Wade TD. Longitudinal risk factors for adverse psychological functioning six months after coronary artery bypass graft surgery. J Health Psychol. 2008;13(1):79–92. doi: 10.1177/1359105307084314. [DOI] [PubMed] [Google Scholar]
- 15.Chocron S, Tatou E, Schjoth B, et al. Perceived health status in patients over 70 before and after open-heart operations. Age Ageing. 2000;29(4):329–334. doi: 10.1093/ageing/29.4.329. [DOI] [PubMed] [Google Scholar]
- 16.Gallagher R, McKinley S. Stressors and Anxiety in Patients Undergoing Coronary Artery Bypass Surgery. Am J Crit Care. 2007;16(3):248–257. [PubMed] [Google Scholar]
- 17.Moore SM. A comparison of women's and men's symptoms during home recovery after coronary artery bypass surgery. Heart & Lung: The Journal of Acute and Critical Care. 1995;24(6):495–501. doi: 10.1016/s0147-9563(95)80027-1. [DOI] [PubMed] [Google Scholar]
- 18.Mallik S, Krumholz HM, Lin ZQ, et al. Patients with depressive symptoms have lower health status benefits after coronary artery bypass surgery. Circulation. 2005;111:271–277. doi: 10.1161/01.CIR.0000152102.29293.D7. [DOI] [PubMed] [Google Scholar]
- 19.Vaccarino V, Lin ZQ, Kasl SV, et al. Gender differences in recovery after coronary artery bypass surgery. J Am Coll Cardiol. 2003;41(2):307–314. doi: 10.1016/s0735-1097(02)02698-0. [DOI] [PubMed] [Google Scholar]
- 20.Redeker NS, Ruggiero JS, Hedges C. Sleep is related to physical function and emotional well-being after cardiac surgery. Nurs Res. 2004;53(3):154–162. doi: 10.1097/00006199-200405000-00002. [DOI] [PubMed] [Google Scholar]
- 21.Jeger RV, Bonetti PO, Zellweger MJ, et al. Influence of revascularization on long-term outcome in patients > or =75 years of age with diabetes mellitus and angina pectoris. Am J Cardiol. 2005;96(2):193–198. doi: 10.1016/j.amjcard.2005.03.042. [DOI] [PubMed] [Google Scholar]
- 22.Rankin SH. Women recovering from acute myocardial infarction: Psychosocial and physical functioning outcomes for 12 months after acute myocardial infarction. Heart & Lung: The Journal of Acute and Critical Care. 2002;31(6):399–410. doi: 10.1067/mhl.2002.129447. [DOI] [PubMed] [Google Scholar]
- 23.King KM. Gender and short-term recovery from cardiac surgery. Nurs Res. 2000;49(1):29–36. doi: 10.1097/00006199-200001000-00005. [DOI] [PubMed] [Google Scholar]
- 24.Koivula M, Tarkka MT, Tarkka M, Laippala P, Paunonen-Ilmonen M. Fear and anxiety in patients at different time-points in the coronary artery bypass process. Int J Nurs Stud. 2002;39(8):811–822. doi: 10.1016/s0020-7489(02)00022-6. [DOI] [PubMed] [Google Scholar]
- 25.Pasquali SK, Alexander KP, Coombs LP, Lytle BL, Peterson ED. Effect of cardiac rehabilitation on functional outcomes after coronary revascularization. American Heart Journal. 2003;145(3):445–451. doi: 10.1067/mhj.2003.172. [DOI] [PubMed] [Google Scholar]
- 26.Barnason S, Zimmerman L, Nieveen J, Hertzog M. Impact of a telehealth intervention to augment home health care on functional and recovery outcomes of elderly patients undergoing coronary artery bypass grafting. Heart Lung. 2006;35(4):225–233. doi: 10.1016/j.hrtlng.2005.10.003. http://search.ebscohost.com/login.aspx?direct=true&db=cmedm&AN=16863894&site=ehost-live. [DOI] [PubMed] [Google Scholar]
- 27.Allen JK, Becker DM, Swank RT. FActors related to functional status after coronary artery bypass surgery. Heart & Lung. 1990;24(6):337. [PubMed] [Google Scholar]
- 28.Doering LV, Moser DK, Lemankiewicz W, Luper C, Khan S. Depression, Healing, and Recovery From Coronary Artery Bypass Surgery. Am J Crit Care. 2005;14(4):316–324. [PubMed] [Google Scholar]
- 29.Edell-Gustafsson UM, Hetta JE. Anxiety, depression and sleep in male patients undergoing coronary artery bypass surgery. Scand J Caring Sci. 1999;13(2):137–143. [PubMed] [Google Scholar]
- 30.Barnason S, Zimmerman L, Anderson A, Mohr-Burt S, Nieveen J. Functional status outcomes of patients with a coronary artery bypass graft over time. Heart Lung. 2000;29(1):33–46. doi: 10.1016/s0147-9563(00)90035-9. [DOI] [PubMed] [Google Scholar]
- 31.Barry LC, Kasl SV, Lichtman J, Vaccarino V, Krumholz HM. Social support and change in health-related quality of life 6 months after coronary artery bypass grafting. J Psychosom Res. 2006;60(2):185–193. doi: 10.1016/j.jpsychores.2005.06.080. [DOI] [PubMed] [Google Scholar]
- 32.Dodd MJ, Miaskowski C, Lee KA. Occurrence of symptom clusters. J Natl Cancer Inst Monogr. 2004;(32)(32):76–78. doi: 10.1093/jncimonographs/lgh008. [DOI] [PubMed] [Google Scholar]
- 33.Kim HJ, McGuire DB, Tulman L, Barsevick AM. Symptom clusters: concept analysis and clinical implications for cancer nursing. Cancer Nurs. 2005;28(4):270–82. doi: 10.1097/00002820-200507000-00005. quiz 283–4. [DOI] [PubMed] [Google Scholar]
- 34.Lindgren TG, Fukuoka Y, Rankin SH, Cooper BA, Carroll D, Munn YL. Cluster analysis of elderly cardiac patients' prehospital symptomatology. Nurs Res. 2008;57(1):14–23. doi: 10.1097/01.NNR.0000280654.50642.1a. [DOI] [PubMed] [Google Scholar]
- 35.Fukuoka Y, Lindgren TG, Rankin SH, Cooper BA, Carroll DL. Cluster analysis: a useful technique to identify elderly cardiac patients at risk for poor quality of life. Qual Life Res. 2007;16(10):1655–1663. doi: 10.1007/s11136-007-9272-7. [DOI] [PubMed] [Google Scholar]
- 36.Ryan CJ, DeVon HA, Horne R, et al. Symptom clusters in acute myocardial infarction: a secondary data analysis. Nurs Res. 2007;56(2):72–81. doi: 10.1097/01.NNR.0000263968.01254.d6. [DOI] [PubMed] [Google Scholar]
- 37.Ryan CJ, Zerwic JJ. Knowledge of symptom clusters among adults at risk for acute myocardial infarction. Nurs Res. 2004;53(6):363–369. doi: 10.1097/00006199-200411000-00004. [DOI] [PubMed] [Google Scholar]
- 38.Dodd MJ, Miaskowski C, Paul SM. Symptom clusters and their effect on the functional status of patients with cancer. Oncol Nurs Forum. 2001;28(3):465–470. [PubMed] [Google Scholar]
- 39.Barsevick AM, Dudley WN, Beck SL. Cancer-related fatigue, depressive symptoms, and functional status: a mediation model. Nurs Res. 2006;55(5):366–372. doi: 10.1097/00006199-200609000-00009. [DOI] [PubMed] [Google Scholar]
- 40.Gallagher R, McKinley S. Stressors and anxiety in patients undergoing coronary artery bypass surgery. Am J Crit Care. 2007;16(3):248–257. [PubMed] [Google Scholar]
- 41.Nieveen JL, Zimmerman LM, Barnason SA, Yates BC. Development and content validity testing of the Cardiac Symptom Survey in patients after coronary artery bypass grafting. Heart Lung. 2008;37(1):17–27. doi: 10.1016/j.hrtlng.2006.12.002. [DOI] [PubMed] [Google Scholar]
- 42.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 43.Hlatky MA, Boineau RE, Higginbotham MB, et al. A brief self-administered questionnaire to determine functional capacity (the Duke Activity Status Index) Am J Cardiol. 1989;64(10):651–654. doi: 10.1016/0002-9149(89)90496-7. [DOI] [PubMed] [Google Scholar]
- 44.Koch CG, Li L, Lauer M, Sabik J, Starr NJ, Blackstone EH. Effect of functional health-related quality of life on long-term survival after cardiac surgery. Circulation. 2007;115(6):692–699. doi: 10.1161/CIRCULATIONAHA.106.640573. [DOI] [PubMed] [Google Scholar]
- 45.Rumsfeld JS, Magid DJ, O'Brien M, et al. Changes in health-related quality of life following coronary artery bypass graft surgery. Ann Thorac Surg. 2001;72(6):2026–2032. doi: 10.1016/s0003-4975(01)03213-1. [DOI] [PubMed] [Google Scholar]
- 46.Stewart RD, Blair JL, Emond CE, Lahey SJ, Levitsky S, Campos CT. Gender and functional outcome after coronary artery bypass. Surgery. 1999;126(2):184–190. [PubMed] [Google Scholar]
- 47.Hedeshian MH, Namour N, Dziadik E, Stewart RD, Campos CT. Does increasing age have a negative impact on six-month functional outcome after coronary artery bypass? Surgery. 2002;132(2):239–244. doi: 10.1067/msy.2002.125388. [DOI] [PubMed] [Google Scholar]
- 48.Alonso J, Permanyer-Miralda G, Cascant P, Brotons C, Prieto L, Soler-Soler J. Measuring functional status of chronic coronary patients. Reliability, validity and responsiveness to clinical change of the reduced version of the Duke Activity Status Index (DASI) Eur Heart J. 1997;18(3):414–419. doi: 10.1093/oxfordjournals.eurheartj.a015260. [DOI] [PubMed] [Google Scholar]
- 49.Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatry Scandia. 1983;67:361. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 50.Bjelland I, Dahl AA, Haung TT, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale: An updated literature review. Journal of Psychosomatic Research, [HADS] 2002;52:69. doi: 10.1016/s0022-3999(01)00296-3. [DOI] [PubMed] [Google Scholar]
- 51.Barnason S, Zimmerman L, Atwood J, Nieveen J, Schmaderer M. Development of a self-efficacy instrument for coronary artery bypass graft patients. Journal of Nursing Measurement. 2002;10(2):123. doi: 10.1891/jnum.10.2.123.52553. [DOI] [PubMed] [Google Scholar]
- 52.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30(6):473–483. [PubMed] [Google Scholar]
- 53.Jette D, Downing J. Health status of individuals entering a cardiac rehabilitation program as measured by the medical outcomes study short-form 36-item health survey in black patients and white patients with acute chest pain. Medical care. 1994;33(3):145–160. [Google Scholar]
- 54.Johnson PA, Goldman L, Orav EJ, Garcia T, Pearson SD, Lee TH. Comparison of the Medical Outcomes Study Short-Form 36-Item Health Survey in black patients and white patients with acute chest pain. Med Care. 1995;33(2):145–160. [PubMed] [Google Scholar]
- 55.Lerner DJ, Levine S, Malspeis S, D'Agostino RB. Job strain and health-related quality of life in a national sample. Am J Public Health. 1994;84(10):1580–1585. doi: 10.2105/ajph.84.10.1580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.McHorney CA, Ware JE, Jr, Rogers W, Raczek AE, Lu JF. The validity and relative precision of MOS short- and long-form health status scales and Dartmouth COOP charts. Results from the Medical Outcomes Study. Med Care. 1992;30(5 Suppl):MS253–65. doi: 10.1097/00005650-199205001-00025. [DOI] [PubMed] [Google Scholar]
- 57.McHorney CA, Ware JE, Jr, Lu JF, Sherbourne CD. The MOS 36-item Short-Form Health Survey (SF-36): III. Tests of data quality, scaling assumptions, and reliability across diverse patient groups. Med Care. 1994;32(1):40–66. doi: 10.1097/00005650-199401000-00004. [DOI] [PubMed] [Google Scholar]
- 58.Tu C, Zimmerman L, Barnason S, Schulz P. Comparing Cluster Analysis Methods in Clinical Studies. 2009 [Google Scholar]
- 59.Given CW, Given B, Azzouz F, Kozachik S, Stommel M. Predictors of pain and fatigue in the year following diagnosis among elderly cancer patients. J Pain Symptom Manage. 2001;21(6):456–466. doi: 10.1016/s0885-3924(01)00284-6. Publisher URL: www.cinahl.com/cgibin/refsvc?jid=463&accno=2001085513; http://search.ebscohost.com/login.aspx?direct=true&db=cin20&AN=2001085513&site=ehost-live. [DOI] [PubMed] [Google Scholar]
- 60.Mallik S, Krumholz HM, Lin ZQ, et al. Patients with depressive symptoms have lower health status benefits after coronary artery bypass surgery. Circulation. 2005;111(3):271–277. doi: 10.1161/01.CIR.0000152102.29293.D7. [DOI] [PubMed] [Google Scholar]
- 61.Rymaszewska J, Kiejna A, Hadrys T. Depression and anxiety in coronary artery bypass grafting patients. Eur Psychiatry. 2003;18(4):155–160. doi: 10.1016/s0924-9338(03)00052-x. [DOI] [PubMed] [Google Scholar]
- 62.Ross AC, Ostrow L. Subjectively perceived quality of life after coronary artery bypass surgery. Am J Crit Care. 2001;10(1):11–16. [PubMed] [Google Scholar]
- 63.Hunt JO, Hendrata MV, Myles PS. Quality of life 12 months after coronary artery bypass graft surgery. Heart Lung. 2000;29(6):401–411. doi: 10.1067/mhl.2000.110578. [DOI] [PubMed] [Google Scholar]
- 64.Jarvinen O, Saarinen T, Julkunen J, Huhtala H, Tarkka MR. Changes in health-related quality of life and functional capacity following coronary artery bypass graft surgery. Eur J Cardiothorac Surg. 2003;24(5):750–756. doi: 10.1016/s1010-7940(03)00413-5. [DOI] [PubMed] [Google Scholar]
- 65.Utriyaprasit K, Moore S. Recovery symptoms and mood states in Thai CABG patients. J Transcult Nurs. 2005;16(2):97–106. doi: 10.1177/1043659604273548. [DOI] [PubMed] [Google Scholar]
- 66.Miaskowski C, Aouizerat BE. Is there a biological basis for the clustering of symptoms? Semin Oncol Nurs. 2007;23(2):99–105. doi: 10.1016/j.soncn.2007.01.008. [DOI] [PubMed] [Google Scholar]
- 67.Parker KP, Kimble LP, Dunbar SB, Clark PC. Symptom interactions as mechanisms underlying symptom pairs and clusters. J Nurs Scholarsh. 2005;37(3):209–215. doi: 10.1111/j.1547-5069.2005.00037.x. [DOI] [PubMed] [Google Scholar]