Abstract
This study evaluated the effectiveness and cost-effectiveness of two types of outpatient treatment with and without Assertive Continuing Care (ACC) for 320 adolescents with substance use disorders. Study participants were randomly assigned to one of four conditions: (a) Chestnut’s Bloomington Outpatient Treatment (CBOP) without ACC; (b) CBOP with ACC; (c) Motivational Enhancement Therapy/Cognitive Behavior Therapy-7 session model (MET/CBT7) without ACC; and (d) MET/CBT7 with ACC. All study conditions attained high rates of participant engagement and retention. Follow-up interviews were completed with over 90% of the adolescents at three, six, nine, and twelve months after treatment admission. There was a significant time by condition effect over 12 months, with CBOP having a slight advantage for average percentage of days abstinent. Unlike previous findings that ACC provided incremental effectiveness following residential treatment, there were no statistically significant findings with regard to the incremental effectiveness of ACC following outpatient treatment. Analysis of the costs of each intervention combined with its outcomes revealed that the most cost-effective condition was MET/CBT7 without ACC.
Keywords: substance abuse, adolescent outpatient treatment, continuing care, outcomes
1. Introduction
It is estimated that over two million adolescents in the U.S. have substance abuse and dependence disorders (Substance Abuse and Mental Health Services Administration, & Office of Applied Studies, 2007a). Half of substance abuse treatment admissions for persons aged 12 to 17 are referrals from the juvenile justice system (Substance Abuse and Mental Health Services Administration & Office of Applied Studies, 2007b). Moreover, studies have shown relationships among substance use and grades, truancy, and school dropout (Bray et al., 2000; Fergusson et al., 2003), as well as co-occurring mental health problems (Chan et al., 2008; Kaminer & Bukstein, 2008). Effective treatments are needed to help alleviate the multiple problems associated with adolescent substance abuse.
Almost 90% of adolescents entering treatment in the U.S. are in outpatient settings (Substance Abuse and Mental Health Services Administration & Office of Applied Studies, 2007a). Recently, a number of well-designed studies have demonstrated promising outpatient treatment approaches for adolescents (Dennis et al., 2004; Waldron & Turner, 2008; Williams & Chang, 2000). The approaches evaluated include ones based on Motivational Enhancement Therapy (MET; Monti et al., 2001), Cognitive Behavior Therapy (CBT; Waldron et al., 2001), or their combination (Dennis et al., 2004), Adolescent Community Reinforcement Approach (A-CRA; Dennis et al., 2004; Godley, Meyers et al., 2001), and a number of family interventions, including Multisystemic Therapy (Henggeler et al., 2006), Multidimensional Family Therapy (Liddle et al., 2001), and Brief Strategic Family Therapy (Szapocznik et al., 1986, 2003).
Community-based treatment providers are encouraged by researchers and their funders to use these evidence-based interventions (Gotham, 2006); however, there is debate about whether this means the adoption of a specific evidence-based treatment (EBT) or multiple empirically supported treatment practices. For example, Fixsen and colleagues (Fixsen et al., 2005) define an Evidence-Based Program as:
“Organized, multi-faceted interventions that are designed to serve consumers with complex problems. Such programs, for example, may seek to integrate social skills training, family counseling, and educational assistance, where needed, in a comprehensive yet individualized manner…” (Fixsen et al., 2005, p.82).
An example of such a multi-faceted intervention is Chestnut’s Bloomington Outpatient Program (CBOP; Godley et al., 2003), which was developed over a twenty year period based on multiple empirically supported practices derived from different, but seemingly complementary, theories of change (e.g., Rogerian, behavioral, cognitive, and mutual support). Rogerian (Rogers, 1951, 1959) practices include unconditional positive regard, acceptance, and rapport building, which are used by clinicians to help foster change through development of a strong therapeutic alliance. Behavioral skill building approaches are believed to help adolescents incorporate new skills that can increase positive consequences from their environment (Hester & Miller, 1989; Kazdin, 2000). Cognitive therapy emphasizes evaluating perceptions and thoughts and changing thinking patterns by reframing and cognitive restructuring to result in the adolescent deciding to engage in more positive/healthy actions (Ellis et al., 1988; Walen et al., 1992; Yankura & Dryden, 1990). Mutual support or 12-step approaches are thought to complement other approaches by creating a supportive environment to help achieve and maintain recovery (White, 2009). For a similar reason, the program incorporates family education and therapy groups (Risberg & Funk, 2000) to help increase the support for recovery once an adolescent completes treatment. Additionally, state licensure guidelines mandate the use of American Society of Addiction Medicine (ASAM) Patient Placement guidelines (American Society of Addiction Medicine, 2001), which require ongoing assessment of individual needs, resulting in an individualized number of treatment sessions. Though comprehensive, the cost of a program that incorporates so many different components is high, so it is important to understand not only its effectiveness, but also its cost-effectiveness.
In contrast, the five-session Motivational Enhancement Therapy and Cognitive Behavior Therapy (MET/CBT; Sampl & Kadden, 2001) is a brief intervention with a fixed number of sessions that shares some of the same theories of change as the CBOP model. This EBT was developed and evaluated in the Cannabis Youth Treatment (CYT) study (Dennis et al., 2004). The two MET sessions are based on the hypothesis that individuals will achieve greater change when motivation comes from within them rather than when others attempt to impose it (Miller & Rollnick, 1991). MET uses Prochaska and DiClemente’s (1984) five stages of change model (precontemplation, contemplation, determination, action, and maintenance) in combination with multiple techniques (e.g., highlighting discrepancies, rolling with resistance) to enhance motivation to change. The three CBT group sessions then help the adolescent develop the coping skills needed to recognize and manage common risk situations that typically lead to drug use (Monti et al., 1989). Within this model, skill deficits are viewed as a primary cause of relapse. Therefore, the group process focused on teaching and rehearsing these skills, and developers hypothesized that group members may become part of a recovery network for each other (Diamond et al., 2002). Due to its brevity and use of groups for three of the five prescribed sessions, it is not surprising that MET/CBT5 was found to be one of the most cost-effective approaches in the CYT study (Dennis et al., 2004).
In a quasi-experiment (Godley et al., 2004), outcomes for 274 adolescents were compared with those who received either Chestnut Health System’s Bloomington Outpatient Treatment (CBOP; Godley et al., 2003) or one of three research-based interventions (including MET/CBT) in the CYT study (Dennis et al., 2004). Adolescents in the CBOP cohort had significantly longer lengths of stay and received over three times as many hours of treatment. After controlling for initial differences in substance use severity, mixed effects analyses revealed that the CYT participants were significantly more likely to report decreases in their substance use, but the CBOP participants were significantly more likely to report an increase in self-help attendance and a decrease in recovery environment risk. However, given that the Cannabis Youth Treatment participants had twice as much substance use at intake as the CBOP group, it is unclear whether a quasi-experimental design was sufficient to control for these initial differences between groups, and a randomized clinical trial is needed to better understand the comparative clinical and cost-effectiveness of these interventions.
A clinical trial evaluating the two outpatient interventions also provides the opportunity to evaluate the combination of an assertive continuing care approach with these outpatient treatments. Outcome data from even the best interventions tested in randomized clinical trials reveal that it is common for many adolescents to experience periods of relapse after treatment (Dennis et al., 2004; Godley et al., 2004; Waldron et al., 2001). Thus, it was hypothesized that regardless of the length of time in outpatient treatment, participants might benefit from a subsequent period of continuing care focused more on support for recovery. Continuing care has been described as services to maintain therapeutic gains from prior treatment (Ito & Donovan, 1986). Assertive Continuing Care (ACC) has been evaluated following residential substance abuse treatment for adolescents and was found to be related to better rates of abstinence from marijuana following discharge (Godley et al., 2002, 2007). Its hypothesized mechanisms of change are that adolescents can be linked to continuing care if clinicians provide these services in the adolescent’s home and community and that in the context of the adolescent’s environment, new skills can be reinforced and support for recovery enhanced. Prior research has provided support for these hypothesized mechanisms of change since ACC improved abstinence outcomes by decreasing both environmental (arguments, fights at home, nights away from home, increased 12-step attendance) and social (association with using peers) risks (Garner et al., 2007). We know of only one recently published outcome study of continuing care for adolescents following outpatient treatment, which showed promise for an active aftercare component (Kaminer et al., 2008). No experimental studies have examined the combination of ACC with different types of adolescent outpatient treatment, although it seemed reasonable to expect that this intervention would improve effectiveness, especially when combined with a shorter outpatient treatment episode since lengths of stay over 90 days in outpatient treatment have been shown to increase treatment effectiveness (Hser et al., 2001).
This paper describes the findings from a randomized design with intent-to-treat analysis comparing the relative effectiveness and cost-effectiveness of two forms of outpatient treatment with and without ACC. Based on the prior quasi and experimental studies reviewed above, we hypothesized that MET/CBT would be more effective and cost-effective than CBOP in terms of increasing days abstinent and decreasing substance abuse problems. Additionally, we hypothesized that the groups receiving ACC would have significantly better outcomes than the groups without ACC. Lastly, we hypothesized that adding ACC to MET/CBT would be the most cost-effective option in terms of days abstinent.
2. Methods
2.1. Participants
Adolescents from rural and urban parts of Central Illinois were enrolled in the study between September 2002 and December 2007. They were referred to services by the juvenile justice system (56%), a family member (23%), another agency (11%), and other sources (10%). Based on self-report, 38% of the adolescents had private insurance, 34% had public insurance, and 28% had mixed sources of insurance, did not know, or had no insurance. Adolescents met inclusion criteria if they were 12 to 18 years old, met ASAM’s (2001) Patient Placement criteria for Level I Outpatient treatment based on a substance abuse or dependence diagnosis and six dimensional admission criteria (i.e., severity of intoxication/withdrawal, physical health, emotional/behavioral health, treatment readiness, relapse potential, and recovery environment), and attended an admission appointment.
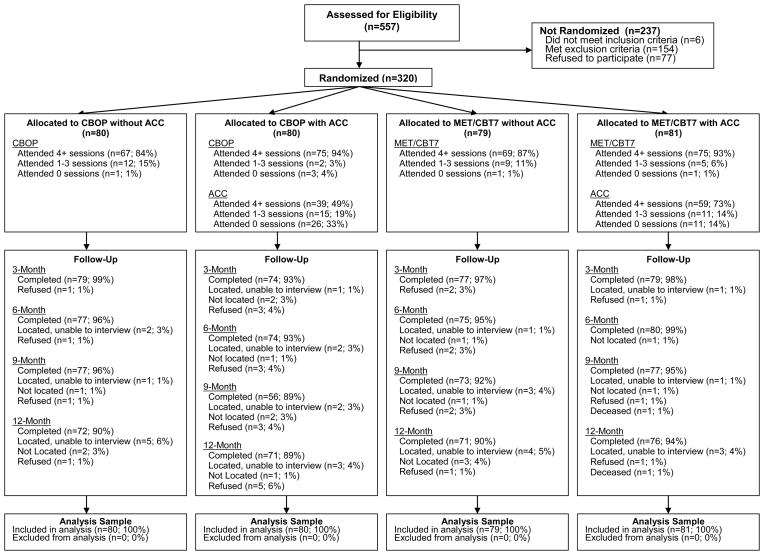
Out of 557 assessed for eligibility, 551 unique adolescents met all inclusion criteria. Out of the 551 eligible, 154 were excluded from the study for one or more of the following reasons, they: (a) were “stepped-down” from residential treatment and were therefore more severe than adolescents who entered outpatient treatment from the community (n = 102); (b) were recommended only for individual counseling, as both outpatient treatment conditions had group components (n = 21); (c) were a ward of the state (n = 27); (d) did not have a parent/guardian present during admission to outpatient treatment (n=4); (e) appeared to have insufficient mental capacity to provide informed consent (n = 2); or (f) did not speak English with sufficient ability to understand study procedures and instruments (n=1). Among the 397 adolescents passing all inclusion and exclusion criteria, 320 (81%) agreed to participate in the current study and were randomized. If adolescents chose not to participate in the study, they were offered admission to the regular outpatient treatment program (CBOP). When refusers (n = 77) were compared with those who agreed to participate, refusers were significantly older (t(335) = 2.02, p < .05; M =16.2) than study participants (M = 15.9, d = 28). See Figure 1 for additional data on participant flow through the experimental conditions.1
Figure 1.
Flow of participants through treatment and follow-up data collection waves by experiment condition.
Participation was voluntary and under the supervision of Chestnut’s Institutional Review Board on Human Subjects, and both the adolescent and a parent/guardian had to agree to study participation and sign the informed consent form after an explanation by research staff. A Federal Certificate of Confidentiality was obtained to further protect the confidentiality of participants’ data.
The average participant age was 15.9 years old (SD = 1.2). Seventy-six percent were male, 73% were Caucasian, 13% were African American, 93% were in school, and 73% were involved in the criminal justice system. Based on endorsing DSM-IV symptoms consistent with diagnoses of past year substance abuse or dependence using the GAIN-I or other information available to their therapist (e.g., collateral report), seventy-five percent met criteria for cannabis abuse or dependence, 49% met criteria for alcohol abuse or dependence, and 35% met criteria for both cannabis and alcohol disorders. Over half (56%) reported symptoms for co-occurring psychological problems (this includes depression, generalized anxiety, trauma, ADHD, and conduct disorder). The only variable for which there was a significant difference by condition was the percentage of participants with cannabis dependence disorder (see Table 1). There were no significant differences for type of reported payer.
Table 1.
Demographic and Clinical Characteristics by Condition
| CBOP |
MET/CBT7 |
||||
|---|---|---|---|---|---|
| Characteristic | No ACC (n = 80) | ACC (n = 80) | No ACC (n = 79) | ACC (n = 81) | Overall (n =320) |
| Demographic | |||||
| Female | 24% | 18% | 27% | 30% | 24% |
| African American/Black | 13% | 11% | 17% | 10% | 13% |
| Caucasian/White | 75% | 74% | 73% | 70% | 73% |
| Hispanic/Latino/other/mixed | 12% | 15% | 10% | 20% | 14% |
| Aged 13–14 | 13% | 9% | 11% | 20% | 13% |
| Aged 15–16 | 49% | 53% | 58% | 63% | 56% |
| Aged 17–18 | 39% | 39% | 30% | 17% | 31% |
| Substance use disorders | |||||
| Weekly alcohol & other drug use | 55% | 48% | 44% | 49% | 49% |
| Cannabis dependence * | 38% | 28% | 39% | 20% | 31% |
| Cannabis abuse | 38% | 46% | 38% | 56% | 44% |
| Alcohol dependence | 14% | 14% | 9% | 7% | 11% |
| Alcohol abuse | 35% | 40% | 37% | 40% | 38% |
| Other substance dependence | 4% | 3% | 4% | 1% | 3% |
| Other substance abuse | 3% | 1% | 3% | 4% | 3% |
| Past year psychological problems | |||||
| Any co-occurring problems | 58% | 59% | 54% | 54% | 56% |
| Major depressive disorder | 30% | 29% | 28% | 26% | 28% |
| Generalized anxiety | 8% | 8% | 8% | 7% | 8% |
| Traumatic distress | 13% | 24% | 19% | 21% | 19% |
| ADHD | 34% | 36% | 33% | 32% | 34% |
| Conduct disorder | 44% | 40% | 43% | 41% | 42% |
| Any prior mental health treatment | 50% | 56% | 53% | 49% | 52% |
| Dependent variables at baseline | |||||
| Percentage of days abstinent from AOD M(SD) | 69(30) | 75(29) | 78(27) | 76(28) | 74(29) |
| Percentage of days abstinent from alcohol M(SD) | 93(11) | 96(5) | 96(7) | 95(10) | 95(9) |
| Substance Problems Scale M(SD) | 3.7(3.4) | 2.6(2.7) | 3.0(3.8) | 2.8(3.0) | 3.0(3.3) |
| Percentage in recovery | 10% | 20% | 20% | 17% | 17% |
Note. CBOP = Chestnut Bloomington outpatient; MET/CBT7 = Motivational Enhancement Therapy/Cognitive Behavior Treatment-7 sessions; ACC = Assertive Continuing Care; AOD = alcohol and other drugs. Chi-square tests revealed only one significant difference by condition: cannabis dependence, χ2 (3) = 9.34.
p < .05.
2.2. Description of Treatment Conditions
2.2.1. Chestnut Bloomington Outpatient (CBOP)
As noted above, CBOP is an evidence-informed intervention that has developed over twenty years and been shaped by treatment research. The underlying theory of change is that the combination of multiple evidence-based and best-practice treatment components will increase the adolescent’s desire to change, provide the necessary skills, and create an environment supportive for this change. The intervention is based on a manual (Godley et al., 2003) and is primarily delivered through skill and therapy groups, combined with a limited number of family and individual sessions for treatment planning and progress reviews. Though it evolved from practice, CBOP has been evaluated (Godley et al., 2004), recognized by Drug Strategies’ Guide to Treating Teens (Drug Strategies, 2003), and is listed on SAMHSA’s National Registry of Evidence-Based Programs and Practices.
2.2.2. Motivational Enhancement Therapy/Cognitive Behavior Treatment (MET/CBT7)
This intervention was based on a manual developed and evaluated in the Cannabis Youth Treatment study (Dennis et al., 2004). For this study, the five-session MET/CBT model (Sampl & Kadden, 2001) was supplemented with two family sessions to address concerns raised about the lack of parent involvement in the intervention (Godley, White et al., 2001) and best-practice recommendations that parental involvement is necessary for adolescents in substance abuse treatment (Center for Substance Abuse Treatment, 1993). The first session was a family session, which provided parents with an overview of the intervention and a review of several intervention-specific materials (i.e., signs and symptoms card, adolescent and parent education packets). The next session was the first individual participant MET session that focused on building rapport, explaining treatment expectations, assessing and building motivation, and reviewing the adolescent’s Personalized Feedback Report. The latter contained information from the intake assessment that outlined the adolescent’s substance use, use-related problems, and reasons for quitting. During the third session, the therapist reviewed progress and helped the adolescent complete a functional analysis of substance use and a personal goal worksheet related to quitting substances. During sessions 4–6, the adolescent joined a closed group of six adolescents for 90-minute CBT skills groups, which focused on alcohol and drug refusal skills, enhancing social support, planning for unanticipated high-risk situations, and coping with relapse. The last session was a family session during which the therapist reviewed the adolescent’s progress to date, relapse signs, and continuing care plans. Treatment was approximately 12 weeks long because time elapsed while waiting for six youth to accumulate for the three group sessions that followed the two individual sessions.
2.2.3. Assertive Continuing Care (ACC)
ACC is a home-based continuing care approach that takes place over a 12 to 14 week period and has shown promise in a randomized clinical trial of adolescents discharged from residential treatment (Godley et al., 2002, 2007). Following an operant reinforcement and skills training model, ACC combines the Adolescent Community Reinforcement Approach (Godley, Meyers et al., 2001) and case management services (Godley et al., 2006) to help adolescents and their caregivers engage in prosocial activities, skills, and needed community services during weekly home visits.
2.3. Involvement in Juvenile Justice and Other Services
Seventy-three percent of the sample was involved in the juvenile justice system; most were in diversion services, with a smaller number on probation. No juvenile drug court was available in the service area, and adolescents’ legal requirements varied and were not manipulated as part of the study. Therapists for both outpatient conditions completed weekly forms for each adolescent’s court officer, which included attendance, level of participation in treatment, the youth’s level of recovery orientation, results of alcohol and drug screens, and general progress toward discharge or need for a higher level of treatment. Adolescents were not admitted to treatment if they were receiving substance abuse treatment elsewhere, but some adolescents participated in other mental health treatment (e.g., counseling and/or medication management).
2.4. Procedures
2.4.1. Randomization
After agreeing to participate in the research study, participants were enrolled and assigned by research staff to one of four conditions based on a randomization log, which was generated by the project manager and consisted of alternating blocks of six assignment slots to the MET/CBT7 intervention (due to closed groups) or CBOP. A coin was flipped to determine which treatment condition would be the initial outpatient condition. Within each block of a treatment assignment, there were alternating assignments to the continuing care conditions, with the first continuing care condition in each block also determined by a coin toss. Thus, each participant was simultaneously assigned to one of the outpatient treatments and one of the continuing care conditions. The randomization log was stored in a locked file cabinet in the office of research staff. Analysis of participant characteristics revealed no significant differences by condition in 19 of the 20 participant characteristics listed in Table 1 (within the limits of what would be expected by chance). The one significant difference among groups (i.e., cannabis dependence) was tested by controlling for it in the core analysis, and it did not change the outcomes. It was not possible to blind staff to condition; however, research staff with no connection to the conditions administered all follow-up interviews.
2.4.2. Assessments, Incentives, and Treatment Costs for Participants
Baseline measures that took approximately two hours were collected from each adolescent at admission and were administered by intake clinicians with master’s degrees, and follow-up measures were completed at three, six, nine, and 12 months after admission. The Accusign DOA 2 THC/COC Panel Assay using solid-phase chromatographic membrane immunoassay technology was used for the detection of cannabis and cocaine at the time of the 3 and 12 month interviews. Adolescents and their guardians were informed when urine samples would be collected at the time of informed consent and reminded when arranging interview appointments. Samples were temperature monitored, unobserved, and screened in a specially designated bathroom in the research office after the interview was completed. Adolescents were able to decline providing a sample without penalty. At each follow-up wave, adolescents were compensated $40 for completing measurement interviews, and an additional $10 for completing the interview within one week of its due date. Follow-up interviews lasted between one and one and a half hours and were administered by research staff with bachelor’s or master’s degrees. Interviews were conducted in a research office, homes, or in correctional or treatment centers. Training in the study assessments included formal training sessions, observation, feedback on audiotaped administrations until certification was achieved, and ongoing monitoring with scheduled reviews of additional audiotapes. Follow-up rates were 97%, 96%, 93%, and 91% for each respective follow-up wave and were above 90% for each condition by wave. The last follow-up interview was completed in December 2008. Outpatient treatment costs for participants were covered either by insurance, grants, public aid, or by self-pay. There were no significant differences by funder. ACC was provided at no cost.
2.4.3. Clinician Characteristics
Twelve clinicians provided treatment during the course of the study. In general, clinicians provided only one type of treatment; however, due to insurance requirements for specific credentials, one clinician treated three adolescents in each of the outpatient conditions. This individual was the clinical supervisor and had delivered the CBOP intervention for several years prior to the study, had been trained on MET/CBT7 by the author of the treatment manual, and was certified to train and supervise others in MET/CBT. Characteristics of the eight clinicians delivering the CBOP intervention were: Caucasian (87.5%); African American (12.5%); female (62.5%); with a Master’s Degree (87.5%); and with a Bachelor’s Degree (12.5%). Characteristics of the four clinicians delivering the MET/CBT7 intervention were: Caucasian (100%); female (75%); with a Master’s Degree (75%); and with a Bachelor’s Degree (25%). The one clinician delivering ACC was a Bachelor-level Caucasian female. On average, clinicians treated 28 adolescents (SD = 34.65; range 1–110).
2.4.4. Clinician Training and Fidelity Monitoring
CBOP clinicians were trained and supervised as required in the treatment manual (Godley et al., 2003). The program had several training and monitoring practices already in place, and relying on these existing fidelity monitoring approaches helped ensure the “usual treatment” did not change as a result of the experiment. The initial training process included several tasks, such as completion of reading and written assignments, development and review of treatment plans, observation of therapy groups and adolescent-family interactions, and participation in the team clinical decision making process. The supervision process included six primary components: (a) weekly clinical supervision sessions; (b) informal consultations with the supervisor as needed; (c) supervisor observation of the clinician in sessions; (d) staff meeting discussions; (e) supervisor completion and feedback of a “Clinical Competency Skills” checklist after three months of employment and annually thereafter; and (f) peer review of performance improvement data. Clinicians delivering CBOP were also required to record therapeutic activity session data.
Experts in the respective interventions trained clinicians providing MET/CBT7 and ACC in two- to three-day sessions. After training, clinicians providing these models were required to regularly audio record their sessions, and these recordings were rated by clinical supervisors with fidelity checklists, which were reviewed during weekly supervision meetings. Clinicians also entered treatment data in electronic systems designed to facilitate monitoring of modality-specific treatment fidelity. Reliability of the clinicians’ data was examined by comparing their reports to what supervisors heard while listening to audio recorded sessions. Comparisons were made across activities reported by clinicians and those observed by supervisors across MET/CBT7 and ACC sessions. There were high agreements between supervisors and clinicians, with kappa’s ranging from 0.79 to 1.00.
2.5. Measures
Participant characteristics, other treatment received, and outcomes were collected using the Global Appraisal of Individual Needs (GAIN; Dennis, Titus et al., 2003; Dennis et al., 2009), which is one of the most widely used measures in adolescent substance abuse treatment evaluation. These data were supplemented with data from staff service logs and urine tests. Below are descriptions of the study’s key outcome and process measures.
2.5.1. Clinical Outcomes
Primary outcome measures were the percentage of days abstinent from any alcohol and drugs, days abstinent from alcohol alone, substance use problems, and recovery status at the end of the study. The GAIN’s Substance Problem Scale (SPS) is based on recency ratings (e.g., past month, two to 12 months ago, more than 12 months ago, never) on 16 symptoms: seven corresponding to DSM-IV criteria for dependence, four for abuse, two for substance-induced health and psychological problems, and three on lower severity symptoms of use (e.g., hiding use, people complaining about use, weekly use). The past month SPS symptom count has excellent internal consistency (α =.9) and good test-retest reliability (r=.7; Dennis, Dawud-Noursi et al., 2003). Cronbach’s alpha for the current sample was .84. Being in recovery at the end of the study was defined as living in the community (vs. being incarcerated, or residing in inpatient treatment or other controlled environment) and reporting no past month substance use, abuse, or dependence problems at the 12-month interview. Urine samples were collected as described above in 2.4.2., and when an adolescent reported being in recovery but the urine test result suggested a false-negative self-report, data were re-coded to show the adolescent as not being in recovery.
2.5.2. Service Data
To track treatment service delivery, including hours and cumulative retention in the outpatient or continuing care interventions, clinicians delivering MET/CBT7, CBOP, and ACC completed electronic service logs. Clinicians recorded which therapy or case management procedure(s) were conducted with which participant, when, and the duration.
2.5.3. Treatment Costs and Cost-Effectiveness
The cost of each treatment is based on the Drug Abuse Treatment Cost Analysis Program (DATCAP; French et al., 1997; French, 2003; www.DATCAP.com), and the cost estimates were completed by the developer’s team. This instrument was designed to measure both the accounting and opportunity costs of substance abuse treatment programs based on standard economic principles. It includes data elements related to personnel, facilities, supplies and materials, client case flow, and amount of services received. The DATCAP also was used in evaluating the costs of the five treatments in the Cannabis Youth Treatment study (Dennis et al., 2004; French et al., 2002; French, 2003). As in the CYT study, two economic outcomes evaluated were the (a) cost per day of abstinence (CPDA) over the 12-month study follow-up period; and (b) cost per participant in recovery (CPPR) at the end of the study. The economic costs of each episode of care were estimated in 2007 dollars based on the values of goods and services that were used. Estimates were made for each of three treatment types (CBOP, MET/CBT, and ACC). Within each condition, these costs were prorated based on the hours of outpatient and ACC sessions received by a given adolescent, divided by the average hours for all individuals in the same condition. CPDA was then calculated by dividing the adolescent’s prorated costs (PC) by his or her total days of abstinence (TDA; i.e., for individual i, CPDAi = PCi/TDAi). CPPR was calculated as the individual’s prorated costs divided by the percentage of individuals for the same therapy condition (within site) that were in recovery (PR); that is, for individual i, in condition c, CPPRi = PCi/PRc.
2.6. Data Analytic Procedures
All analyses were conducted with SPSS (2007) Version 16 using an “intent to treat” approach. Thus, follow-up data were collected from all participants and data analyzed per original assignment condition. Differences in discharge status and recovery status were examined using chi-square analysis. Treatment process measures were examined using one-way ANOVAs. Outcome analyses of continuous variables were conducted using mixed effects repeated measure models with random intercepts to test the effect of time, condition, and time by condition. Additionally, a priori contrasts were used to test for the effect of outpatient type (CBOP vs. MET/CBT7), continuing care (without ACC vs. ACC), and their interactions with time.
There was very little missing data (i.e., less than 10% of the participants missed any given interview wave and less than 4% had missing data on any one variable), and any missing data were addressed with the mixed effects analyses, which generated estimates using restricted (by condition) maximum likelihood. This approach calculates fixed effects first and then estimates random effects (partitioning out these differences within condition), so that it improves statistical power without biasing the outcome analysis. When differences from more than one group were analyzed, Cohen’s effect size f-index was calculated as the average of the absolute value of the difference between each group mean and the grand mean.
3. Results
3.1. Treatment Received by Condition
As seen in Figure 1, 84% to 94% of the adolescents received at least four sessions, with 65% to 76% doing so within the first 44 days of treatment, which constitutes the Washington Circle criteria for outpatient engagement (Garnick et al., 2009). Of those assigned to CBOP with ACC, 49% received at least four sessions of continuing care, 19% received 1–3 sessions, and 33% participated in no sessions. Of those assigned to MET/CBT7 with ACC, 73% received at least four sessions of continuing care, 14% received 1–3 sessions, and 14% participated in no sessions. Table 2 shows several treatment process measures based on services reported by staff and participant self-report by condition. All these variables were significantly different by condition, with adolescents assigned to CBOP generally receiving more treatment hours than those assigned to MET/CBT7, and adolescents assigned to ACC generally receiving more treatment hours than those without ACC within the same outpatient treatment. MET/CBT7 participants had a higher rate of planned discharges. ACC led to longer retention within each outpatient condition.
Table 2.
Treatment Received by Condition
| CBOP |
MET/CBT7 |
|||
|---|---|---|---|---|
| Treatment | No ACC (n = 80) | ACC (n = 80) | No ACC (n = 79) | ACC (n = 81) |
| Treatment hours and retention | ||||
| Total OP + ACC hoursa* | 33.8 (25.7) | 44.3 (26.8) | 8.5 (3.4) | 16.5 (7.5) |
| OP hoursb* | 33.8 (25.7) | 39.5 (25.5) | 8.5 (3.4) | 8.7 (2.9) |
| ACC hoursc* | 4.7 (5.4) | 7.8 (6.0) | ||
| Retention (days)d* | 103.8 (57.4) | 172.4 (91.5) | 83.6 (27.9) | 143.4 (44.2) |
| OP discharged as plannede* | 53% | 58% | 71% | 83% |
| Number and type of sessions | ||||
| Individual | 3.4 (3.6) | 9.6 (7.2) | 2.4 (1.3) | 8.8 (4.5) |
| Group | 15.6 (12.5) | 20.7 (15.2) | 2.1 (1.2) | 2.4 (1.1) |
| Collateral | 0.1 (0.5) | 1.3 (2.0) | 0.1 (0.3) | 1.9 (1.9) |
| Family | 1.5 (1.0) | 2.3 (2.4) | 2.4 (0.8) | 3.3 (1.4) |
| OP family nights | 1.4 (3.1) | 1.3 (2.5) | ||
Note. CBOP = Chestnut Bloomington outpatient; MET/CBT7 = Motivational Enhancement Therapy/Cognitive Behavior Treatment-7 sessions; ACC = Assertive Continuing Care; OP = outpatient.
F(3, 316) = 58.37, p < .01.
F(3, 316) = 64.62, p < .01.
t(159) = 3.42, p < .01.
F(3, 316) = 34.98, p < .01.
χ2(3) = 19.98, p < .01.
p < .01.
3.2. Clinical Outcome Analysis
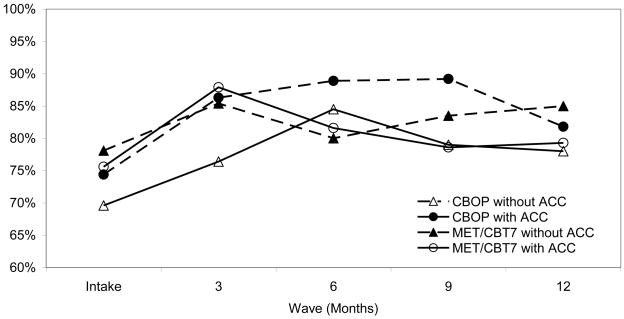
One-way analysis of variance tests revealed no significant differences in the outcome variables at intake (see Table 1). Table 3 provides means and standard deviations across the four measurement intervals for each condition for days reported abstinent and the Substance Problem Scale. Table 4 shows the summary tables for mixed linear analysis results including statistics and between group effect sizes. For days abstinent from alcohol and other drugs, there was a significant time by condition interaction (F(12,729) = 2.03, p < .05, f-index = 0.10). A priori contrasts suggest that this was primarily due to an effect of time by CBOP (F(4,729) = 4.08, p < .01, f-index = 0.08). Figure 2 shows mean values of the percentage of days abstinent from alcohol and drugs at intake and across the four follow-up waves. Overall, the average percentage of days abstinent at follow-up was higher than baseline in all four conditions, with the increase in the percentage of days abstinent higher for the two CBOP conditions (10.6% and 10.9%) than the two MET/CBT7 conditions (5.0% and 6.1%). While adolescents assigned to ACC had slightly higher increases in the percentage of days abstinent than those without it, the differences were not statistically significant. When we examined the change in percentage of days abstinent from alcohol use only, there were no significant time effects, condition effects, nor interactions between time and condition for this outcome. The only significant finding for the Substance Problem Scale was a time effect (F(4,687) = 40.99, p < .001, f-index = 0.29). Adolescents across conditions reported average decreases from approximately 3 problems at baseline to 1.2 to 1.68 at the 12-month follow-up.
Table 3.
Mean Outcomes Scores by Condition
| CBOP |
MET/CBT7 |
Total |
||||
|---|---|---|---|---|---|---|
| Wave | No ACC (n = 80) | ACC (n = 80) | No ACC (n = 79) | ACC (n = 81) | M | SD |
| Percent of days abstinent from alcohol or other drugs (0 – 100)a | ||||||
| Intake | 69.6 | 74.4 | 78.1 | 75.6 | 74.4 | 28.5 |
| 3 month | 76.4 | 86.3 | 85.4 | 87.9 | 83.9 | 23.4 |
| 6 month | 84.5 | 88.9 | 80.0 | 81.6 | 83.7 | 25.5 |
| 9 month | 79.0 | 89.2 | 83.5 | 78.6 | 82.5 | 27.8 |
| 12 month | 78.0 | 81.8 | 85.0 | 79.3 | 81.0 | 29.1 |
| Percent of days abstinent from alcohol (0 – 100)a | ||||||
| Intake | 93.3 | 96.2 | 96.0 | 95.5 | 95.2 | 8.9 |
| 3 month | 95.4 | 96.3 | 95.7 | 96.0 | 95.8 | 8.5 |
| 6 month | 95.6 | 95.9 | 95.0 | 95.9 | 95.6 | 9.4 |
| 9 month | 94.7 | 96.2 | 94.9 | 93.5 | 94.8 | 11.1 |
| 12 month | 94.0 | 94.0 | 95.1 | 93.4 | 94.1 | 11.2 |
| Substance Problem Scaleb | ||||||
| Intake | 3.69 | 2.55 | 3.05 | 2.85 | 3.03 | 3.27 |
| 3 month | 1.39 | 1.23 | 1.35 | 1.33 | 1.33 | 2.35 |
| 6 month | 1.19 | .88 | 1.25 | 1.31 | 1.16 | 2.38 |
| 9 month | 1.19 | .71 | .86 | 1.79 | 1.15 | 2.34 |
| 12 month | 1.68 | 1.2 | 1.2 | 1.2 | 1.32 | 2.46 |
Note. CBOP = Chestnut Bloomington outpatient; MET/CBT7 = Motivational Enhancement Therapy/Cognitive Behavior Treatment - 7 sessions; ACC = Assertive Continuing Care.
Percent of days abstinent out of the past 90 days.
Substance Problem Scale score for past month.
Table 4.
Results of Mixed Linear Analysis
| Effects | Wald Z | df | F | f-index |
|---|---|---|---|---|
| Percentage of days abstinent from alcohol or other drugs (0–100) | ||||
| Random intercept | 4.87** | |||
| Time | (4, 729) | 1.45** | 0.14 | |
| Condition | (3, 318) | 1.58 | 0.09 | |
| CBOP (vs. MET/CBT7) | (1, 317) | 0.12 | 0.01 | |
| ACC (vs. w/o ACC) | (1, 317) | 1.06 | 0.04 | |
| ACC × CBOP | (1, 317) | 3.57 | 0.08 | |
| Time * overall condition | (12, 729) | 2.03* | 0.10 | |
| Time * CBOP | (4, 729) | 4.08** | 0.08 | |
| Time * ACC | (4, 729) | 0.88 | 0.04 | |
| Time* CBOP * ACC | (4, 729) | 1.14 | 0.03 | |
| Percentage of days abstinent from alcohol (0–100) | ||||
| Random intercept | 4.99** | |||
| Time | (4, 687) | 1.57 | 0.06 | |
| Condition | (3, 315) | 0.44 | 0.04 | |
| CBOP (vs. MET/CBT7) | (1, 315) | 0.01 | 0.00 | |
| ACC (vs. w/o ACC) | (1, 315) | 0.19 | 0.00 | |
| ACC × CBOP | (1, 315) | 1.14 | 0.04 | |
| Time * overall condition | (12, 687) | 0.64 | 0.06 | |
| Time * CBOP | (4, 687) | 0.64 | 0.03 | |
| Time * ACC | (4, 687) | 0.57 | 0.03 | |
| Time* CBOP * ACC | (4, 687) | 0.70 | 0.03 | |
| Substance Problem Scale (past month) | ||||
| Random intercept | 5.50** | |||
| Time | (4, 687) | 40.99** | 0.29 | |
| Condition | (3, 318) | 1.38 | 0.07 | |
| CBOP (vs. MET/CBT7) | (1, 318) | 0.07 | 0.00 | |
| ACC (vs. w/o ACC) | (1, 318) | 0.71 | 0.03 | |
| ACC × CBOP | (1, 318) | 3.39 | 0.06 | |
| Time * overall condition | (12, 687) | 1.34 | 0.08 | |
| Time * CBOP | (4, 687) | 1.12 | 0.04 | |
| Time * ACC | (4, 687) | 1.80 | 0.05 | |
| Time* CBOP * ACC | (4, 687) | 1.05 | 0.04 | |
Note. Model used is DV= Ai +Tj + CBOP + ACC + CBOP*ACC + Tj*CBOP + Tj*ACC+ Tj*CBOP*ACC, where Ai is a random intercept for person ”i”, Tj is a Time fixed effect at month j, CBOP is a fixed effect for outpatient type (CBOP=1, MET/CBT= −1), and ACC is a fixed effect for the continuing care type (ACC=1, No Continuing Care= −1) within OP type, and CBOP*ACC is their interaction. CBOP = Chestnut Bloomington outpatient; MET/CBT7 = Motivational Enhancement Therapy/Cognitive Behavior Treatment – 7 sessions; ACC = Assertive Continuing Care.
p < .05.
p < .01.
Figure 2.
Data are shown for the mean values of percentage of days abstinent from alcohol and other drugs by condition [CBOP without ACC (n = 80), CBOP/ACC (n = 80), MET/CBT7 without ACC (n = 79), and MET/CBT7/ACC (n = 81)]. A mixed linear analysis revealed a significant time effect (F[4, 729] = 10.45, p < .001), a significant time by condition interaction (F[12, 729] = 2.03, p < .05), and a significant time by outpatient (CBOP vs. MET/CBT7) interaction (F[4, 729] = 4.08, p < .01). CBOP = Chestnut Bloomington outpatient; MET/CBT7 = Motivational Enhancement Therapy/Cognitive Behavior Treatment – 7 sessions; ACC = Assertive Continuing Care.
The urine tests used provided results for both marijuana and cocaine use. Adolescents reported very little cocaine use, and there were very few positive tests for cocaine, so positive cocaine and cannabis results were combined. These results were compared to recency of cannabis and/or cocaine use to check for false-negative reports. A false-negative report was defined as a positive urine screen when the adolescent reported no use in the past month. At the three-month follow-up, the false-negative rate was 13%, ranging from 11% for MET/CBT7 with ACC to 17% for CBOP with ACC. The percentage of false-negative reports was not significantly different by condition, χ2 (3) = 1.31, p = .731. At 12-months, the false-negative rate was 12%, ranging from 6% for CBOP with ACC to 17% for CBOP without ACC. Once again, these differences were not significant, χ2 (3) = 4.43, p = .215.
As noted above, recovery status was defined as being in the community with no past month substance problems and reporting abstinence from any alcohol or drugs in the 30 days preceding the 12-month follow-up interview corroborated by the urine test. The resultant findings by condition were that the percentage in recovery for each condition was: 29% for CBOP without ACC, 38% for CBOP with ACC, 44% for MET/CBT7 without ACC, and 30% for the MET/CBT7 with ACC condition. These findings were not significantly different by condition, χ2 (3) = 4.44, p = .215.
3.3. Cost-Effectiveness Analysis
While there was only one significant difference among conditions by outcome, there were significant differences in the costs per condition, F(3,316)=45.09, p<.001 (see Table 5). Thus, it was appropriate to examine the relative economic efficiency of each condition based on its clinical outcomes per the methodology used in the CYT study (Dennis et al., 2004). Table 5 provides the means and SD for the Cost-Per-Day-Abstinent and Cost-Per-Person-in-Recovery across the four conditions. The average Cost-Per-Day-Abstinent achieved over the 12-month follow-up period was $13.12 per day, with MET/CBT7 without ACC costing significantly less per day ($4.25) than the other three conditions, F(3,297)=16.15, p<.001. The average Cost-Per-Person-in-Recovery at the end of data collection was $9,982.20 and varied significantly by condition (F(3,316)=42.37, p<.001); Tukey HSD post-hoc tests revealed that MET/CBT7 without ACC cost significantly less per person in recovery than the other three conditions at $2,619.87 (p<.001), and CBOP/ACC cost significantly more per person in recovery than CBOP without ACC ($13,945.28 vs. $11,131.42, p=.049).
Table 5.
Treatment Costs by Treatment Condition
| CBOP |
MET/CBT7 |
|||
|---|---|---|---|---|
| Costs | No ACC (n = 80) | ACC (n = 80) | No ACC (n = 79) | ACC (n = 81) |
| Average cost per episodea | $3,246.66 | $5,303.14 | $1,143.89 | $3,665.95 |
| Average cost per day abstinentb | $14.00 | $19.37 | $4.25 | $14.97 |
| Average cost per person in recovery at 12 monthsc | $11,131.42 | $13,945.28 | $2,619.87 | $12,113.57 |
Note. CBOP/UCC = Chestnut Bloomington Outpatient with usual continuing care; CBOP = Chestnut Bloomington outpatient; MET/CBT7 = Motivational Enhancement Therapy/Cognitive Behavior Therapy - 7 sessions; ACC = Assertive Continuing Care. All data and calculations were performed with the DATCAP (www.DATCAP.com). All costs are reported in 2007 dollars. The original DATCAP estimates were prorated as follows: (total hours of service received/divided by the average hours of all clients in the same condition.
Average cost per episode = average weekly cost per client × mean length of stay in weeks.
Average cost per day abstinent = episode cost/total days abstinent.
Average cost per person in recovery at 12 months = episode cost/the percent of clients in the same condition in recovery at 12 months.
4. Discussion
4.1. Summary of Findings
All four conditions were associated with increased abstinence and reduced substance use problems. The findings do not support the study hypotheses that MET/CBT7 would be more effective than CBOP in terms of increasing days abstinent since the latter had a significant advantage with regard to days abstinent from alcohol and other drugs over the follow-up period even though effect sizes were small, possibly due to relatively high mean days abstinent (69%) at intake for those adolescents placed into outpatient treatment based on ASAM (2001) Patient Placement criteria. The addition of Assertive Continuing Care to the two types of outpatient treatment did result in slight increases in the percentage of days abstinent compared to the same type of outpatient treatment without continuing care; however, these differences did not reach statistical significance. The most important finding was that when the treatment Cost-Per-Day Abstinent and Cost-Per-Person-In-Recovery were computed, MET/CBT7 without the assertive continuing care was the most cost-effective condition. This finding replicates the effect found in the first study arm of the Cannabis Youth Treatment study (Dennis et al., 2004); however, since there was not a no treatment control group, it is not clear how cost-effectiveness of the different treatments would compare for improvement above and beyond recovery without treatment.
An examination of the longitudinal treatment outcomes in Figure 2 further supports the finding that no one outpatient treatment or combination with Assertive Continuing Care is clearly clinically superior. If the study had been terminated at the 6- and 9-month follow-up intervals, however, the findings would have supported the CBOP with ACC condition as the most effective. Kaminer et al. (2008) had such a result in a randomized trial of brief outpatient CBT for adolescents followed by 3 months of aftercare. They found significant improvement in substance use outcomes for the combined CBT-aftercare condition compared to the CBT-only condition at the end of the aftercare phase (approximately 5–6 months from the baseline assessment.
One possible explanation for the similarity in effectiveness among the conditions may be the relatively high rates of engagement and retention of participants across the conditions. Engagement rates were computed based on the quality of care performance measures developed by the Washington Circle group, which classifies engagement as attendance at 4 sessions within the first 44 days of treatment. The level of engagement across all four study conditions was very good compared to rates that have been computed for public sector substance abuse treatment systems (Garnick et al., 2009). Other explanations for the lack of differences over the course of the 12 month follow-up include the possibility of similar mechanisms of behavioral change or specific factors between the outpatient conditions (Siqueland et al., 2004). For example, both the CBOP and MET/CBT conditions included components of CBT, group education, and homework assignments. Research has also shown that therapists’ ability to develop therapeutic alliance and create positive expectancies for change can contribute to similar outcome findings (Carroll, Nich, & Rounsaville, 1997; Luborsky et al., 2002), and these factors may have been present in all conditions. It is also possible that the combination of both common and specific factors may have contributed to the findings. Taken together, the treatment outcome findings are consistent with prior meta-analyses of adolescent treatment and juvenile justice research, which has suggested that differences between multiple evidence-based practices are often small (Lipsey, 1997; Waldron & Turner, 2008). The similarity in treatment effectiveness outcomes also reinforces the importance of examining differences in cost-effectiveness, especially when the current economic environment is shrinking resources for treatment.
Since ACC has been found to improve treatment outcomes following residential treatment (e.g., Garner et al., 2007; Godley et al., 2007), it is important to consider why the findings were not replicated when it was added to outpatient treatment. One possible reason for these different outcomes may be that continuing care models like ACC might be more effective for participants with higher severity and recent periods of sustained abstinence (as is the case for adolescents discharged from residential treatment programs). Another possible explanation may be related to the degree of implementation. For example, adolescents in the prior ACC study averaged substantially more ACC sessions (11) than did participants in this study (average of eight ACC sessions for MET/CBT7 and an average of five sessions for CBOP participants). This disparity in implementation of ACC between studies may be due to the level of participant severity, the index episode being in residential versus an outpatient treatment setting, therapist effects, or an interaction of the above.
4.2. Strengths and Limitations
Strengths of this study included the use of randomization, the comparative effectiveness evaluation of well-developed research and practice interventions, and the use of multiple measures of implementation. This study is also the first experimental evaluation of Assertive Continuing Care following an outpatient treatment episode. There also are several limitations that should be considered while interpreting these results. Fidelity checks for MET/CBT7 and ACC were conducted based on reviews of taped therapy sessions, while the fidelity of CBOP was conducted using the program’s existing methods to avoid changing the intervention. It was not possible to blind the research staff who collected follow-up data to participants’ study condition assignment; however, separate staff were used for research interviews and treatment. Finally, the sample was primarily Caucasian males (80%) who lived in a small city and/or rural area in Illinois, which could limit generalizability.
4.3. Clinical and Research Implications
One goal of the study was to compare an evidence-informed intervention (CBOP) that based treatment discharge decisions on individual response to treatment with a brief, fixed length evidence-based treatment (MET/CBT7). The only way to make a valid comparison of an individualized treatment is to allow lengths of stay to vary naturally based on this paradigm. The addition of ACC as a factor in the study extended the outpatient interventions, further making them consistent with recent recommendations to provide extended interventions in recognition of the remission-relapse cycles characteristic of substance use disorders and other chronic conditions (McKay, 2005; McLellan et al., 2000). Some of our findings suggest that it may be challenging to maintain adolescents appropriate for outpatient treatment in extended interventions. Those adolescents who were assigned to the briefer outpatient intervention (MET/CBT7) had on average three more continuing care sessions than those assigned to the longer outpatient intervention (CBOP), suggesting that adolescents who attend a short outpatient treatment are more amenable to participating in continuing care. Future research might examine the use of motivational incentives to increase attendance during continuing care sessions or other approaches that would be less expensive and might prove more appealing to adolescents, such as web-based support paired with telephone or face-to-face contacts for monitoring and re-intervention as needed.
Prior research (Dennis et al., 2004) has suggested that brief interventions have performed at least as well as longer, more intensive interventions. This study adds additional support to the relative cost-effectiveness of briefer interventions. An important area of research for adoption and implementation of brief interventions is the “acceptability” of these briefer interventions by clinicians and referral sources. For example, in a recent study examining attempts of the U. S. Center for Substance Abuse Treatment grantees to replicate the fixed length MET/CBT5 intervention, clinicians at eight of nine sites modified the intervention by adding family sessions and further individualizing treatment (Riley et al., 2008) because they believed these additions were important. Future research will examine process and outcome data from several replications of these models to assess potential moderators, mediators, and other treatment processes that impact outcome. Future research should also examine adaptive treatment research designs (McKay, 2009) that incorporate brief treatment interventions and lower-intensity, lower-cost approaches to extended continuing care; especially those that test monitoring, support, and re-intervention for improving recovery outcomes for adolescents.
Supplementary Material
Footnotes
The CONSORT statement checklist for the randomized trial reported in this article is available with the online version of this article at doi:xxx/j.drugalcdep.xxx …
The CONSORT statement checklist of items to report for a randomized trial available with the full text online version of this paper at doi:xxx/j.drugalcdep.xxx …
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- American Society of Addiction Medicine (ASAM) Patient Placement Criteria for the Treatment of Substance-Related Disorders. 2. American Society of Addiction Medicine; Chevy Chase, MD: 2001. [Google Scholar]
- Bray JW, Zarkin GA, Ringwalt C, Qi J. The relationship between marijuana initiation and dropping out of high school. Health Econ. 2000;9:1–18. doi: 10.1002/(sici)1099-1050(200001)9:1<9::aid-hec471>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- Carroll KM, Nich C, Rounsaville BJ. Contributions of the therapeutic alliance to outcome in active versus control psychotherapies. J Consul Clin Psychol. 1997;65:510–514. doi: 10.1037//0022-006x.65.3.510. [DOI] [PubMed] [Google Scholar]
- Center for Substance Abuse Treatment. Treatment Improvement Protocol Series, Number 4. DHHS Publication No. 93-2010. Center for Substance Abuse Treatment; Rockville, MD: 1993. Guidelines for the Treatment of Alcohol- and Other Drug-Abusing Adolescents. [Google Scholar]
- Chan Y-F, Dennis ML, Funk RR. Prevalence and comorbidity of major internalizing and externalizing problems among adolescents and adults presenting to substance abuse treatment. J Subst Abuse Treat. 2008;34:14–24. doi: 10.1016/j.jsat.2006.12.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennis ML, Dawud-Noursi S, Muck RD, McDermeit M. The need for developing and evaluating adolescent treatment models. In: Stevens SJ, Morral AR, editors. Adolescent Substance Abuse Treatment in the United States: Exemplary Models from a National Evaluation Study. Haworth Press; Binghamton, NY: 2003. pp. 3–34. [Google Scholar]
- Dennis ML, Godley SH, Diamond G, Tims FM, Babor T, Donaldson J, Liddle H, Titus JC, Kaminer Y, Webb C, Hamilton N, Funk RR. The Cannabis Youth Treatment (CYT) Study: Main findings from two randomized trials. J Subst Abuse Treat. 2004;27:197–213. doi: 10.1016/j.jsat.2003.09.005. [DOI] [PubMed] [Google Scholar]
- Dennis ML, Titus JC, White M, Unsicker J, Hodgkins D. Global Appraisal of Individual Needs (GAIN): Administration Guide for the GAIN and Related Measures. Chestnut Health Systems; Bloomington, IL: 2003. [Google Scholar]
- Dennis ML, White M, Ives ML. Individual characteristics and needs associated with substance misuse of adolescents and young adults in addiction treatment. In: Leukefeld C, Gullotta T, Staton Tindall M, editors. Handbook on Adolescent Substance Abuse Prevention and Treatment: Evidence-Based Practice. Child and Family Agency Press; New London, CT: 2009. pp. 45–72. [Google Scholar]
- Diamond GS, Godley SH, Liddle HA, Sampl S, Webb C, Tims FM, Meyers R. Five outpatient treatment models for adolescent marijuana use: A description of the Cannabis Youth Treatment interventions. Addiction. 2002;97:S70–S83. doi: 10.1046/j.1360-0443.97.s01.3.x. [DOI] [PubMed] [Google Scholar]
- Drug Strategies. Treating Teens: A Guide to Adolescent Drug Programs. Author; Washington, DC: 2003. [Google Scholar]
- Ellis A, McInerney JF, DiGuiseppe R, Yeager RJ. Rational-Emotive Therapy with Alcoholics and Substance Abusers. Pergamon Press; Elmsford, NY: 1988. [Google Scholar]
- Fergusson DM, Horwood LJ, Beautais AL. Cannabis and educational achievement. Addiction. 2003;98:1681–1692. doi: 10.1111/j.1360-0443.2003.00573.x. [DOI] [PubMed] [Google Scholar]
- Fixsen DL, Naoom SF, Blasé KA, Friedman RM, Wallace F. Implementation Research: A Synthesis of the Literature. National Implementation Research Network; Tampa, FL: 2005. [Google Scholar]
- French MT. Drug Abuse Treatment Cost Analysis Program (DATCAP): Program Version. 8. University of Miami; Coral Gables, FL: 2003. [Accessed 10-21-09]. from www.DATCAP.com. [Google Scholar]
- French MT, Dunlap LJ, Zarkin GA, McGeary KA, McLellan AT. A structured instrument for estimating the economic cost of drug abuse treatment: The Drug Abuse Treatment Cost Analysis Program (DATCAP) J Subst Abuse Treat. 1997;14:445–455. doi: 10.1016/s0740-5472(97)00132-3. [DOI] [PubMed] [Google Scholar]
- French MT, Roebuck MC, Dennis ML, Diamond G, Godley SH, Tims F, Webb C, Herrell JM. The economic cost of outpatient marijuana treatment for adolescents: Findings from a multi-site field experiment. Addiction. 2002;97:S84–S97. doi: 10.1046/j.1360-0443.97.s01.4.x. [DOI] [PubMed] [Google Scholar]
- Garner BR, Godley MD, Funk RR, Dennis ML, Godley SH. The impact of continuing care adherence on environmental risks, substance use, and substance-related problems following adolescent residential treatment. Psychol Addict Behav. 2007;21:488–497. doi: 10.1037/0893-164X.21.4.488. [DOI] [PubMed] [Google Scholar]
- Garnick DW, Lee MT, Horgan CM, Acevedo A. Adapting Washington Circle performance measures for public sector substance abuse treatment systems. J Subst Abuse Treat. 2009;36:265–277. doi: 10.1016/j.jsat.2008.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Godley MD, Godley SH, Dennis ML, Funk R, Passetti L. Preliminary outcomes from the assertive continuing care experiment for adolescents discharged from residential treatment. J Subst Abuse Treat. 2002;23:21–32. doi: 10.1016/s0740-5472(02)00230-1. [DOI] [PubMed] [Google Scholar]
- Godley MD, Godley SH, Dennis ML, Funk RR, Passetti LL. The effect of Assertive Continuing Care (ACC) on continuing care linkage, adherence and abstinence following residential treatment for adolescents. Addiction. 2007;102:81–93. doi: 10.1111/j.1360-0443.2006.01648.x. [DOI] [PubMed] [Google Scholar]
- Godley SH, Godley MD, Karvinen T, Slown LL, Wright KL. The Assertive Continuing Care Protocol: A Clinician’s Manual for Working with Adolescents after Residential Treatment of Alcohol and Other Substance Use Disorders. Lighthouse Institute; Bloomington, IL: 2006. [Google Scholar]
- Godley SH, Jones N, Funk R, Ives M, Passetti LL. Comparing outcomes of best-practice and research-based outpatient treatment protocols for adolescents. J Psychoactive Drugs. 2004;36:35–48. doi: 10.1080/02791072.2004.10399722. [DOI] [PubMed] [Google Scholar]
- Godley SH, Meyers RJ, Smith JE, Godley MD, Titus JC, Karvinen T, Dent G, Passetti L, Kelberg P. Cannabis Youth Treatment (CYT) Manual Series. DHHS Publication No. (SMA) 01-3489. Vol. 4. Center for Substance Abuse Treatment, Substance Abuse and Mental Health Services Administration; Rockville, MD: 2001. The Adolescent Community Reinforcement Approach (ACRA) for Adolescent Cannabis Users. [Google Scholar]
- Godley SH, Risberg RA, Adams L, Sodetz A. Chestnut Health Systems’ Bloomington Outpatient and Intensive Outpatient Treatment Model. Chestnut Health Systems; Bloomington, IL: 2003. [Google Scholar]
- Godley SH, White WL, Diamond G, Passetti L, Titus J. Therapist reactions to manual-guided therapies for the treatment of adolescent marijuana users. Clin Psychol Sci Prac. 2001;8:405–417. [Google Scholar]
- Gotham HJ. Advancing the implementation of evidence-based practices into clinical practice: How do we get there from here? Prof Psychol Res Pr. 2006;37:606–613. [Google Scholar]
- Henggeler SW, Halliday-Boykins CA, Cunningham PB, Randall J, Shapiro SB, Chapman JE. Juvenile drug court: Enhancing outcomes by integrating evidence-based treatments. J Consult Clin Psychol. 2006;74:42–54. doi: 10.1037/0022-006X.74.1.42. [DOI] [PubMed] [Google Scholar]
- Hester RK, Miller WR. Handbook of Alcoholism Treatment Approaches: Effective Alternatives. Allyn and Bacon; Boston, MA: 1989. [Google Scholar]
- Hser YI, Grella CE, Hubbard RL, Hsieh SC, Fletcher BW, Brown BS, Anglin MD. An evaluation of drug treatments for adolescents in four U.S. cities. Arch Gen Psychiatry. 2001;58:689–695. doi: 10.1001/archpsyc.58.7.689. [DOI] [PubMed] [Google Scholar]
- Ito J, Donovan DM. Aftercare in alcoholism treatment: A review. In: Miller WR, Heather N, editors. Treating Addictive Behaviors: Process of Change. Plenum Press; New York: 1986. pp. 435–452. [Google Scholar]
- Kaminer Y, Bukstein OG. Adolescent Substance Abuse: Psychiatric Comorbidity and High-Risk Behaviors. Routledge Taylor & Francis Group; New York: 2008. [Google Scholar]
- Kaminer Y, Burleson JA, Burke RH. Efficacy of outpatient aftercare with adolescents with alcohol use disorders: A randomized controlled study. J Am Acad Child Adolesc Psychiatry. 2008;47:1405–1412. doi: 10.1097/CHI.0b013e318189147c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kazdin AE. Behavior Modification in Applied Settings. 6. Dorsey Press; Chicago: 2000. [Google Scholar]
- Liddle HA, Dakoff GA, Parker K, Diamond GS, Barrett K, Tejeda M. Multidimensional family therapy for adolescent substance abuse: Results of a randomized clinical trial. Am J Drug Alcohol Abuse. 2001;27:651–688. doi: 10.1081/ada-100107661. [DOI] [PubMed] [Google Scholar]
- Lipsey MW. What can you build with thousands of bricks? Musings on the cumulation of knowledge in program evaluation. New Directions for Evaluation. 1997;76:7–23. [Google Scholar]
- Luborsky L, Rosenthal R, Diguer L, Andrusyna TP, Berman JS, Levitt JT, Seligman DA, Krause ED. The dodo bird verdict is alive and well — mostly. Clin Psychol Sci Prac. 2002;9:2–12. [Google Scholar]
- McKay JR. Is there a case for extended interventions for alcohol and drug use disorders? Addiction. 2005;100:1594–1610. doi: 10.1111/j.1360-0443.2005.01208.x. [DOI] [PubMed] [Google Scholar]
- McKay JR. Continuing care research: What we have learned and where we are going. J Subst Abuse Treat. 2009;36:131–145. doi: 10.1016/j.jsat.2008.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLellan AT, Lewis DC, O’Brien CP, Kleber HD. Drug dependence, a chronic medical illness: Implications for treatment, insurance, and outcomes evaluation. JAMA. 2000;284:1689–1695. doi: 10.1001/jama.284.13.1689. [DOI] [PubMed] [Google Scholar]
- Miller WR, Rollnick S. Motivational Interviewing: Preparing People to Change Addictive Behavior. Guilford Press; New York: 1991. [Google Scholar]
- Monti PM, Abrams DB, Kadden RM, Cooney NL. Treating Alcohol Dependence: A Coping Skills Training Guide. Guilford; New York: 1989. [Google Scholar]
- Monti PM, Barnett NP, O’Leary TA, Colby SM. Motivational enhancements for alcohol-involved adolescents. In: Monti PM, Colby SM, O’Leary TA, editors. Adolescents, Alcohol, and Substance Abuse: Reaching Teens Through Brief Interventions. Guilford Press; New York: 2001. pp. 145–182. [Google Scholar]
- Prochaska JO, DiClemente CC. The Transtheoretical Approach: Crossing Traditional Boundaries of Therapy. Dow Jones/Irwin; Homewood, IL: 1984. [Google Scholar]
- Riley KJ, Rieckmann T, McCarty D. Implementation of MET/CBT-5 for adolescents. J Behav Health Serv Res. 2008;35:304–314. doi: 10.1007/s11414-008-9111-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Risberg RA, Funk RR. Evaluating the perceived helpfulness of a family night program for adolescent substance abusers. J Child Adolesc Subst Abuse. 2000;10:51–67. [Google Scholar]
- Rogers CR. Client-Centered Therapy. Houghton-Mifflin; Boston, MA: 1951. [Google Scholar]
- Rogers CR. A theory of therapy, personality, and interpersonal relationships as developed in the client-centered framework. In: Koch S, editor. Psychology: A Study of a Science: Volume III. Formulations of a Person and the Social Context. McGraw-Hill; New York: 1959. pp. 184–256. [Google Scholar]
- Sampl S, Kadden R. Motivational Enhancement Therapy and Cognitive Behavioral Therapy for Adolescent Cannabis Users: 5 Sessions. Center for Substance Abuse Treatment, Substance Abuse and Mental Health Services Administration; Rockville, MD: 2001. [Google Scholar]
- Siqueland L, Crits-Christoph P, Barber JP, Gibbons MG, Gallop R, Griffin M, Frank A, Thase M, Luborsky L, Liese B. What aspects of treatment matter to the patient in the treatment of cocaine dependence? J Subst Abuse Treat. 2004;27:169–178. doi: 10.1016/j.jsat.2004.06.007. [DOI] [PubMed] [Google Scholar]
- SPSS. Statistical Program for the Social Sciences, Version 16. SPSS; Chicago, IL: 2007. [Google Scholar]
- Substance Abuse and Mental Health Services Administration (SAMHSA), & Office of Applied Studies (OAS) National Survey on Drug Use and Health, 2004 and 2005. 2007a Accessed March 11, 2008 from: www.oas.samhsa.gov/NSDUH/2k5NSDUH/tabs/Sect5peTabs1to82.htm#Tab5.1A.
- Substance Abuse and Mental Health Services Administration (SAMHSA), & Office of Applied Studies (OAS) The OAS Report: A Day in the Life of American Adolescents: Substance Use Facts. Author; Rockville, MD: Oct 18, 2007b. [Google Scholar]
- Szapocznik J, Hervis O, Schwartz S. Brief Strategic Family Therapy for Adolescent Drug Abuse. NIH Publication No. 03-4751. National Institute on Drug Abuse; Rockville, MD: 2003. [Google Scholar]
- Szapocznik J, Kurtines WM, Foote FH, Perez-Vidal A, Hervis O. Conjoint versus one-person family therapy: Further evidence for the effectiveness of conduction family therapy through one person with drug-abusing adolescents. J Consult Clin Psychol. 1986;54:395–397. doi: 10.1037//0022-006x.54.3.395. [DOI] [PubMed] [Google Scholar]
- Waldron HB, Slesnick N, Brody JL, Turner CW, Peterson TR. Treatment outcomes for adolescent substance abuse at four- and seven-month assessments. J Consult Clin Psychol. 2001;69:802–813. [PubMed] [Google Scholar]
- Waldron HB, Turner CW. Evidence-based psychosocial treatments for adolescent substance abuse: A review and meta-analyses. J Clin Child Adolesc Psychol. 2008;37:238–261. doi: 10.1080/15374410701820133. [DOI] [PubMed] [Google Scholar]
- Walen SR, DiGiuseppe R, Dryden W. A Practitioner’s Guide to Rational-Emotive Therapy. Oxford University Press; New York: 1992. [Google Scholar]
- White WL. Peer-Based Addiction Recovery Support: History, Theory, Practice, and Scientific Evaluation. Great Lakes Addiction Technology Transfer Center and Philadelphia Department of Behavioral Health and Mental Retardation Services; Chicago: 2009. [Google Scholar]
- Williams RJ, Chang SY. A comprehensive and comparative review of adolescent substance abuse treatment outcome. Clin Psychol Sci Prac. 2000;7:138–166. [Google Scholar]
- Yankura J, Dryden W. Doing RET: Albert Ellis in Action. Springer Publishing Company; New York: 1990. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.