Abstract
Aim
Individuals who have both substance use disorders and mental health problems have poorer treatment outcomes. This study examines the relationship of service utilization and 12-step participation to outcomes at 1 and 5 years for patients treated in one of two integrated service delivery systems: the Department of Veterans Affairs (VA) system and a health maintenance organization (HMO).
Methods
Subsamples from each system were selected using multiple criteria indicating severity of mental health problems at admission to substance use disorder treatment (VA = 401; HMO = 331). Separate and multiple-group structural equation model analyses used baseline characteristics, service use, and 12-step participation as predictors of substance use and mental health outcomes at 1 and 5 years following admission.
Results
Substance use and related problems showed stability across time, however, these relationships were stronger among VA patients. More continuing care substance use outpatient visits were associated with reductions in mental health symptoms in both groups, whereas receipt of outpatient mental health services was associated with more severe psychological symptoms. Participation in 12-step groups had a stronger effect on reducing cocaine use among VA patients, whereas it had a stronger effect on reducing alcohol use among HMO patients. More outpatient psychological services had a stronger effect on reducing alcohol use among HMO patients.
Conclusion
Common findings across these two systems demonstrate the persistence of substance use and related psychological problems, but also show that continuing care services and participation in 12-step groups are associated with better outcomes in both systems.
Keywords: substance use disorder treatment, mental health services, continuing care, 12-step/self-help groups, longitudinal outcomes
1. Introduction
Individuals in with substance use disorders who also have mental health problems demonstrate poorer treatment outcomes and more enduring trajectories of substance use as compared with individuals with substance use disorders only. Poorer outcomes among this population have been demonstrated with regard to polydrug use (Compton et al., 2003) and more severe medical, social, and family problems following treatment (Chi et al., 2006). In addition, individuals with co-occurring substance use and mental health problems have lower rates of treatment completion, shorter stays in treatment, and higher rates of posttreatment relapse and rehospitalization (McLellan et al., 1983; Rounsaville et al., 1987; Carroll et al., 1993; Weisner, Matzger, et al., 2003).
In this paper, we briefly review research on longitudinal substance use and psychiatric outcomes among patients in treatment for substance use disorders. We also examine the relationship of services utilization, including continuing care services and participation in 12-step/self-help groups, with longitudinal outcomes. We then test a model derived from this literature on the relationship of continuing care services and participation in 12-step/self-help groups with longitudinal outcomes among patients in substance use disorder treatment who were treated in one of two integrated service delivery systems in which both substance use and mental health services were provided.
1.2. Longitudinal outcomes of patients with both substance use and mental health problems
A substantial number of individuals with both substance use disorders and mental health problems return to substance use, experience employment and social difficulties related to their drug problems, and report psychological distress and psychiatric symptoms following treatment (Drake et al., 2008). Further, individuals with co-occurring substance use and mental health problems have higher rates of service utilization (Gonzalez and Rosenheck, 2002) and more repeated treatment episodes (Rush et al., 2008) as compared with others. Although prior research has shown that individuals with greater problem severity receive more services while in treatment (Hser et al., 2004), it is not clear whether their repeated use of treatment services results in improved functioning over time.
Some research has shown that longer stays in residential treatment and participation in continuing care, including outpatient mental health treatment, have been associated with better post-treatment functioning for periods up to 5 years following treatment (Moos et al., 1996; Herman et al., 2000; Moos et al., 2000; Ouimette et al., 2000; Ritsher, Moos et al., 2002; Ray et al., 2005). Moreover, patients with co-occurring disorders show considerable variability in outcomes, although substance use and psychiatric symptoms are strongly inter-related over time (Chi and Weisner, 2008). In addition, individuals who exhibit high levels of psychological problems at treatment admission and following discharge are less likely to transition from substance use to abstinence (Scott et al., 2005). They also engage in longer periods of substance use prior to obtaining stable abstinence (Dennis et al., 2005), with fluctuations in mental health status depending on the duration of abstinence (Dennis et al., 2007).
1.3. Effects of continuing care and 12-step/self-help group participation on outcomes
Treatment for substance use disorders has recently emphasized the importance of “continuing care” interventions, consistent with the prevailing emphasis on the chronic nature of these disorders (McLellan 2002; McLellan et al., 2000) and the movement toward a longitudinal perspective on recovery (Laudet, 2008). Continuing care interventions typically provide a less-intensive form of treatment or support services following an initial phase of treatment and may include a variety of approaches such as group counseling, individual therapy, telephone counseling, brief checkups, “recovery support” services, and self-help meetings (McKay, 2009; McKay et al., 1998). Evaluations of continuing care interventions have shown mixed results (McKay, 2001), with more positive outcomes associated with a longer duration of participation, more structured interventions, and strategies to improve patients’ engagement (McKay, 2009).
In addition, there is a reinforcing relationship between participation in substance use disorder treatment and 12-step/self-help groups that enhances outcomes over time. Patients who combine outpatient treatment with participation in 12-step/self-help groups show improved outcomes over time compared with those who do not participate in 12-step/self-help groups (Moos et al., 2001). Participants in residential treatment who attend 12-step/self-help groups following treatment also demonstrate a greater likelihood of abstinence, although more positive effects have been found for alcohol use than for stimulants (Gossop et al., 2007). A longer duration of initial treatment is also associated with greater 12-step/self-help involvement following treatment, which then lessens the likelihood of subsequent treatment participation (Bond et al., 2003; Moos and Moos, 2004). Self-help participation has been associated with a greater likelihood of being in remission following treatment, although those with mental health problems still have poorer outcomes than others (Ritsher, McKellar et al., 2002). Moreover, more 12-step/self-help participation following initial treatment has been associated with reduced use of both inpatient and outpatient mental health services (Humphreys and Moos, 2007). Hence, both continuing care and 12-step/self-help involvement following initial treatment have been found to improve patient outcomes over time. Yet few studies have examined the effects of continuing care or other services received following treatment for individuals with co-occurring substance use and mental health problems (McGovern et al., 2005).
1.4. Current paper
This study uses two datasets that contain relatively comparable data on substance use and psychiatric severity for patients who were sampled from one of two integrated health care delivery systems and who were followed at comparable intervals. Subsamples who reported elevated mental health problems were selected for the current study. The study aimed to examine commonalities and differences in longitudinal substance use and mental health outcomes in relation to treatment and services utilization and participation in 12-step/self-help groups following an index treatment episode. Specifically, we sought to determine if the relationship between services received in the year following the index treatment episode, including (outpatient) continuing care for alcohol and drug (AOD) disorders, mental health services, and participation in 12-step/self-help groups, had similar relationships to outcomes at 1 and 5 years post-treatment for patients in the two service delivery systems. The hypothesized model that guided the analyses is presented in Figure 1.
Figure 1.
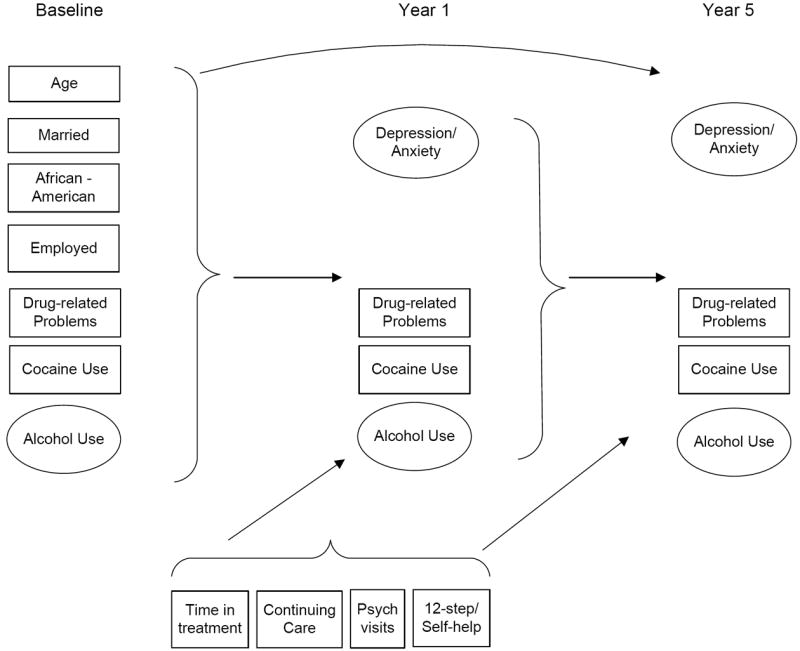
Hypothesized model of relationships among baseline characteristics, treatment/ services, continuing care, 12-step/self-help group participation, and outcomes at Years 1 and 5 following treatment.
2. Methods
2.1. Study samples
The original two studies were conducted at approximately the same historical time. They also had comparable data collection points (baseline, 1- and 5-year post-treatment follow-ups); similar instruments and methods for conducting assessments; and included administrative data on services utilization over the follow-up duration. Both health care systems were fully integrated and self-contained in that patients were provided substance use disorder treatment and mental health services within each health care system, rather than being referred to other providers.
2.1.1. VA sample
The original sample from the Department of Veterans Affairs (VA) consisted of patients (N = 3,698) who were admitted into VA inpatient substance use disorder treatment programs nationwide from 1992–1995 and completed a face-to-face assessment. Follow-up assessments were conducted at 1 and 5 years post-admission by phone. In addition, administrative data were obtained on continuing outpatient substance use disorder treatment and mental health services received over the 1-year follow-up period. The study research design and methods have been described in detail previously (Finney et al., 2001).
2.1.2. HMO sample
The original sample obtained from the health maintenance organization (HMO) consisted of patients (N = 747) who were admitted to an outpatient chemical dependency treatment program from 1997–1998. In-person assessments were conducted with consecutive treatment admissions and follow-up interviews were conducted by phone at 1 year and 5 years after intake. Data on the index treatment episode, mental health services, and outpatient chemical dependency treatment visits (within the HMO) over the 1-year follow-up period were obtained from the administrative data system. The study research design and methods have been described in detail previously (Weisner et al., 2001; Weisner, Ray et al., 2003).
2.1.3. Sample selection
Total sample sizes at admission, especially for the VA sample, were quite large (VA= 3,698, HMO=747) and both studies achieved acceptable follow-up rates (at least 80%) of participants verified as non-deceased over the 5-year follow-up interval. Sub-samples from each of the two original studies were selected for the current study using criteria that indicated symptoms of psychological problems and/or recent treatment for psychiatric disorders at the baseline assessment. The sample included individuals who met at least one of the following conditions (assessed at baseline): a hospital-based psychiatric stay in the past two years, symptoms of suicidality in the past 3 months, outpatient psychiatric treatment in the past 3 months, current use of medication for psychiatric problems, or current symptoms of serious depression, anxiety, or hallucinations. These criteria were selected on the basis of their comparability to items in the Addiction Severity Index pertaining to psychiatric severity (McLellan et al., 1983), which has been shown to have good correspondence with psychiatric disorders assessed with standardized diagnostic instruments (Cacciola et al., 2008). Similar criteria have been used in other studies to select sub-groups of patients with “high psychiatric problem severity” (Hser et al., 2006).
To keep the samples relatively equivalent in size and to avoid overly small but significant associations among the variables for only the VA sample, one quarter of the remaining VA sample was selected at random as the comparison group for the HMO sample. Final sample sizes were N = 331 for the HMO and N = 401 for the VA. Supplementary analyses using the total VA sample that met study inclusion criteria (N = 1605) were also conducted to ascertain whether any substantive associations were lost through use of the smaller sample.
2.1.4. Characteristics of study samples
The two samples differed on some baseline characteristics. African Americans made up about half (51%) of the VA sample and only 8% of the HMO sample. The HMO sample was also more stable, with 38% who were married (compared with 18% in the VA) and 62% who were employed (compared with 23% in the VA). The VA sample was older, with an average age of 41.3 (SD=7) years compared with 37.4 (SD=4) years for the HMO. The VA sample was all male, whereas the HMO sample was 50% male. Consequently, alternative models tested whether the inclusion of gender in the HMO model moderated any of the relationships observed in the principal comparison models.
With regard to substance use and mental disorders at admission (based on administrative data), among the VA sample, 15% had an alcohol disorder only, 46% had a drug disorder (with or without an alcohol disorder), and 39% had both an AOD and mental health disorder. Among those in the HMO, 20% had an alcohol disorder only, 28% had a drug disorder (with or without an alcohol disorder), and 50% had both an AOD and mental health disorder.
2.2. Study measures
Data were obtained from both participant interviews and administrative data systems and used to construct comparable measures across the two studies. Variables that addressed the same domains (i.e., alcohol and drug use, psychological symptoms, problems in functioning) were selected from both studies; ranges and distributions were inspected and rescaled to equivalent distributions. Many items were exactly the same and did not need rescaling. In some cases, items were based on different time spans. These items were modified appropriately to reflect equivalent time periods or usage patterns. For instance, cocaine use was based on a three-month assessment of typical daily usage for the VA sample, and number of days used out of the prior 30 days for the HMO sample. These items were changed to equivalency so that both groups were rated alike with estimates based on never, less than once a week, 1-3 days a week, 4-6 days a week, and every day.1 The core measures are briefly described below.
2.2.1. Substance use and mental health measures
These measures are based on self-report data obtained from baseline and follow-up interviews with participants. Drug-related problems refers to the number of problems (e.g., financial, legal, familial) associated with AOD use in past 3 months for the VA and in the past 30 days for the HMO and were scaled for equivalency with 1 (lowest level) to 4 (highest level). Cocaine use is based on frequency of use of either cocaine or crack in the past 3 months for the VA and in the past 30 days for the HMO and was scaled for equivalency with 1 (lowest level) to 5 (highest level). Alcohol use is a latent variables that consists of three items in the VA study (frequency of drinking, maximum amount of use, and amount of use per day) and two items in the HMO (days of drinking and days consumed at least 5 drinks in past 30 days). Symptoms of depression and anxiety is a latent variable consisting of the depression and anxiety subscales of the Basic Symptom Inventory (Derogatis and Melisaratos, 1983) in the VA sample and of two items referring to self-reported “serious depression” and “serious anxiety or tension” in the past 30 days in the HMO. Note: since the sample was selected on the basis of indicators of elevated mental health symptoms at treatment admission, this measure was not included at baseline.
2.2.2. Treatment/service use and 12-step participation variables
Administrative data obtained from the respective health care systems were used for the following treatment/service variables. Time in index treatment was measured in days and is based on the admission and discharge dates of the initial treatment episode. The index treatment episode consisted of group-based interventions that included group therapy, education, relapse prevention, family therapy, and limited individual counseling. Continuing care refers to participation in substance use services following the more intensive initial phase of treatment. This measure is based on the number of days of outpatient substance use treatment visits received following the index treatment episode through Year 1. Psychological service visits is the number of outpatient visits to the department of psychiatry following the index treatment episode through Year 1. These services included individual and group psychotherapy, education, and medication management. For more description of treatment services at the respective programs, see Chi et al. (2006) regarding the HMO and Finney et al. (2001) regarding the VA.
Participation in 12-step/self-help groups was based on participant self-report at the Year 1 follow-up of the number of 12-step/self-help meetings attended in the past 3 months in the VA and in the past 30 days in the HMO and was scaled for equivalency from 0 (none) to 4 (high) similar to the rescaling procedure described above for cocaine use.
2.3. Analyses
The analyses were performed using the EQS structural equations program (Bentler, in press). Goodness-of-fit of the models was assessed with the maximum-likelihood χ2 statistic, the Comparative Fit Index (CFI), the Satorra-Bentler χ2 (S-B χ2), the Robust Comparative Fit Index (RCFI), and the root mean squared error of approximation (RMSEA; Bentler and Dudgeon, 1996; Hu and Bentler, 1999; Bentler, in press). The Robust S-B χ2 was used in addition to the maximum likelihood χ2 because it is more appropriate when the data depart from multivariate normality. Mardia’s normalized multivariate kurtosis estimate was high in both groups (z- statistic = 47.76 (VA), 84.73 (HMO); Bentler and Dudgeon, 1996), rejecting multivariate normality. The RCFI ranges from 0 to 1 and reflects the improvement in fit of a hypothesized model over a model of complete independence among the measured variables. The RCFI adjusts for sample size; values at .95 or greater are desirable, indicating that the hypothesized model reproduces 95% or more of the covariation in the data (Hu and Bentler, 1999). The RMSEA is a measure of fit per degrees of freedom, controlling for sample size, and values less than .06 indicate a relatively good fit between the hypothesized model and the observed data (Hu and Bentler, 1999).
Two types of models were compared: (1) correlational models with no time-ordering and (2) path models. Confirmatory factor analyses examined the correlations among all of the variables in the model, and assessed the adequacy of the measurement models for the latent variables within each sample. Then, separate and initially identical predictive structural equation path models (see Figure 1) were tested in which baseline predictors included marital status (yes/no), African American ethnicity (yes/no), employment status (full or part time job vs. no employment), age in years, drug-related problems, cocaine use, and alcohol use. In addition, treatment/service predictors included time in the index treatment episode, continuing care substance use treatment visits, number of psychological service visits, and participation in 12-step/self-help groups. These items predicted cocaine use, alcohol use, and psychiatric status as reflected in symptoms of depression and anxiety, as well as drug-related problems at Year 1. Year 5 variables of cocaine use, alcohol use, symptoms of depression/anxiety, and drug-related problems were initially predicted by the Year 1 variables. Additional significant predictors of the Year 5 variables (baseline and service use predictors) were added if they were suggested by the LaGrange Multiplier (LM) test (Chou and Bentler, 1990). Correlations that were significant among the predictive background variables and among the outcome variables were retained in these models if they were significant. Nonsignificant paths and correlations in the path models were trimmed gradually, following the model-evaluation procedure of MacCallum (1986).
2.3.1. Multiple group models
To assess common and distinctive associations across the two study samples, we used multiple group assessment techniques to (1) contrast all of the correlations in the saturated confirmatory models from the two datasets (171 contrasts) and (2) compare the parameters in the path models. In both types of models, hypotheses of cross-sample equality were tested starting with an unrestricted model in which no assumptions were made about the comparability of various parameters across the groups under scrutiny. We then tested a more restrictive hypothesis through the use of equality constraints that equated all of the correlations (or path coefficients) among the constructs in the model for the two groups. The plausibility of the equality constraints was determined with the goodness-of-fit indexes described above, chi-square difference tests, and results of the LM test. In the context of a multiple group analysis, the LM test provides information concerning which equality constraints are not reasonable and should be released to improve the fit of the model. Due to the numerous comparisons in these large models, a χ2 value of 10.83 was used as the criterion for significance (1 df, p < .001) to avoid capitalizing on relatively small chance differences.
3. Results
3.1. Preliminary confirmatory analysis
The initial confirmatory factor models had an excellent fit in both groups: VA: ML χ2 = 282.91, 165 df; CFI = .98, RMSEA = .04; S-B χ2 = 266.23, 165 df; RCFI = .98; RMSEA = .04. HMO: ML χ2 = 121.69, 94 df; CFI = .99, RMSEA = .03; S-B χ2 = 112.95, 94 df; RCFI = .98; RMSEA = .03. Table 1 reports correlations among the baseline variables and Table 2 reports the correlations among the Year 1, Year 5, and treatment/service variables.
Table 1.
Correlations among baseline variables; VA below the diagonal, HMO above
| Baseline | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
|---|---|---|---|---|---|---|---|
| 1. Married | — | .08 | .12* | .11* | .03 | -.05 | -.06 |
| 2. African American | -.08 | — | .06 | .07 | -.09* | .26*** | .10* |
| 3. Employed | .10* | -.06 | — | .13* | -.02 | -.06 | .07 |
| 4. Age | .01 | -.16*** | -.09* | — | .03 | -.16*** | .21*** |
| 5 Drug-related problems | .04 | .09 | -.08 | -.17*** | — | .02 | .15** |
| 6. Cocaine use | -.06 | .48*** | -.11* | -.17*** | .26*** | — | -.03 |
| 7. Alcohol use | -.07 | -.14** | -.07 | .10* | .18*** | -.09* | — |
p ≤ .05.
p ≤ .01.
p ≤ .001
Table 2.
Correlations among Year 1 outcomes, Year 5 outcomes, and treatment/service variables; VA below the diagonal, HMO above
| Variables | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Year 1 variables | ||||||||||||
| 1. Drug-related problems | — | .03 | .35*** | .40*** | .20*** | .01 | .11* | .14* | -.08 | .07 | .09 | .02 |
| 2. Cocaine use | .45*** | — | .21*** | .03 | .09 | -.01 | .12* | .13* | -.06 | -.06 | -.10* | -.13* |
| 3. Alcohol use | .59*** | .30*** | — | .19*** | .08 | -.02 | .35*** | .00 | -.19*** | -.09 | -.22*** | -.30*** |
| 4. Depression /Anxiety | .60*** | .24*** | .44*** | — | .23*** | .13* | .02 | .33*** | -.15 | .02 | .20*** | .02 |
| Year 5 variables | ||||||||||||
| 5. Drug-related problems | .43*** | .20*** | .27*** | .30*** | — | .24*** | .38*** | .39*** | -.07 | -.02 | .01 | -.05 |
| 6. Cocaine use | .24*** | .36*** | .01 | .08 | .39*** | — | .01 | .06 | -.06 | -.03 | -.04 | -.06 |
| 7. Alcohol use | .20*** | .07 | .27*** | .12* | .43*** | .29*** | — | .14* | -.04 | -.12* | -.08 | -.10* |
| 8. Depression /Anxiety | .33*** | .07 | .18*** | .57*** | .47*** | .14** | .21*** | — | -.05 | .00 | .16** | -.01 |
| Service Delivery Variables | ||||||||||||
| 9. Time in index treatment | -.10* | -.09* | -.04 | -.05 | -.03 | -.10* | -.08 | -.05 | — | -.12* | .15** | .43*** |
| 10. Continuing care | -.14** | -.12* | -.09* | -.12* | -.10* | -.03 | -.02 | -.02 | .-.01 | — | .29*** | .31*** |
| 11. Psych service visits | -.07 | -.02 | -.06 | .08 | -.02 | -.06 | -.09* | .07 | .08 | .12* | — | .16** |
| 12. 12-step/self- help participation | -.14** | -.15*** | -.12* | -.18*** | -.07 | -.13* | -.13* | -.02 | .07 | .13** | .14** | — |
p ≤ .05.
p ≤ .01.
p ≤ .001.
In both samples, the strongest association was between African-American ethnicity and cocaine use at baseline. Older individuals were more likely to use alcohol and less likely to use cocaine in both samples. Associations among service-related variables and Year 1 and Year 5 outcomes were similar across the two samples and in expected directions (i.e., positive associations among service-related and 12-step/self-help group variables and, in general, between service use and 12-step/self-help group variables and better outcomes). Significant differences in associations across the two samples are discussed below.
3.2. Multiple group comparison of the correlations among the variables
When we contrasted the 171 correlations among the variables by constraining the correlations to equality between the groups, 17 correlations were significantly different based on the stringent criterion reported above (p < .001; see Table 3). Thus, 10% of the relationships were significantly and substantially different between the two groups. Many of these differences involved associations among participation in the index treatment episode, service delivery, and participation in 12-step/self-help groups. For instance, the largest difference was the association between a longer time in the index treatment episode and attendance at 12-step/self-help groups after treatment for HMO patients (r = .43), whereas this relationship was negligible for VA patients (r = .07). Similarly, 12-step/self-help group participation was positively associated with more continuing care substance use services for HMO patients (.31), whereas there was a weaker association between these variables for VA patients (.13). Associations between time in index treatment and continuing care substance use services were negative in both samples, but were significantly different (HMO = -.12, VA = -.01).
Table 3.
Significant differences between associations in the CFA Model in order of magnitude out of 171 contrasts
| Variables | Correlation coefficients | χ2Value1 | |
|---|---|---|---|
| HMO | VA | ||
| 1. 12-step/self-help, time in treatment | .43 | .07 | 45.12 |
| 2. Year 1 Depression/Anxiety, Year 5 Depression/Anxiety | .33 | .57 | 42.01 |
| 3. 12-step/self-help, Continuing care | .31 | .13 | 40.90 |
| 4. Year 5 Depression/Anxiety, Year 5 Drug-related Problems | .39 | .47 | 36.04 |
| 5. 12-step/self-help, Year 1 Alcohol Use | -.30 | -.12 | 26.69 |
| 6. Baseline Cocaine Use, Year 1 Cocaine Use | -.01 | .36 | 23.49 |
| 7. Year 1 Cocaine Use, Year 5 Cocaine Use | -.01 | .36 | 19.00 |
| 8. Year 1 Drug-related Problems, Year 5 Depression/anxiety | .14 | .33 | 17.91 |
| 9. Age, 12-step/self-help | .24 | -.12 | 14.28 |
| 10. Age, time in treatment | .24 | -.04 | 13.50 |
| 11. African-American, Year 5 Cocaine Use | -.02 | .25 | 16.08 |
| 12. Year 5 Depression/anxiety, Year 5 Alcohol Use | .14 | .21 | 14.90 |
| 13. Time in treatment, Continuing care | -.12 | -.01 | 13.78 |
| 14. Year 5 Alcohol Use, Year 5 Cocaine Use | .01 | .29 | 13.78 |
| 15. Year 5 Cocaine Use, Year 5 Drug-related Problems | .24 | .39 | 13.13 |
| 16. African-American, Age | .07 | -.16 | 12.00 |
| 17. African-American, Baseline Alcohol Use | .10 | -.14 | 11.87 |
χ2 > 10.83, p ≤ .001
There were also several differences in correlations related to age and ethnicity. African-American ethnicity was associated with younger age in the VA sample, but not in the HMO sample. African-American ethnicity was negatively associated with baseline alcohol use among the VA sample, but these were positively associated in the HMO model. There was a strong positive association between African-American ethnicity and cocaine use at Year 5 among patients in the VA sample, but not in the HMO sample. Age was positively associated with both time in index treatment and participation in 12-step/self-help groups among the HMO sample; however these associations were weaker and in the negative direction among the VA sample.
With regard to substance use over time, there were stronger and more persistent relationships among VA patients between cocaine use at baseline and Year 1 (VA = .48, HMO = .10) and between Year 1 and Year 5 (VA = .36, HMO = -.01). Similarly, there was a stronger relationship between alcohol use and cocaine use at Year 5 among VA patients (.29) than among those in the HMO (.01).
Symptoms of depression/anxiety at Year 1 and Year 5 were positively associated in both samples, but more strongly in the VA sample (.33 vs. .57). There was a significant relationship between more participation in 12-step/self-help groups and less alcohol use at Year 1 in both samples, but this relationship was stronger among the HMO sample (-.30 vs. -.12).
3.3. Path analysis
Fit indexes for the final trimmed path models based on the hypothesized model presented in Figure 1 were excellent: VA: ML χ2 = 390.33, 272 df; CFI = .98, RMSEA = .03; S-B χ2 = 372.33, 272 df; RCFI = .98; RMSEA = .03. HMO: ML χ2 = 313.59, 298 df; CFI = .99, RMSEA = .01; S-B χ2 = 319.24, 298 df; RCFI = .98; RMSEA = .01. The equality of pathways across the two study samples was tested with constrained models similar to those reported in Section 3.2. Pathways that were dropped due to non-significance in one sample were restored temporarily in order to test whether paths significant in one sample and not the other were significantly different from each other. We discuss first those pathways that were significant in both samples (although the common path coefficients may have significantly differed in strength), and then those pathways that were significant in only one of the samples.
3.3.1. Common significant pathways across the two study samples
Figure 2 depicts regression paths that were significant in both study samples. Common pathways that were significantly larger in one sample are indicated by asterisks. There were 13 common pathways in the two study samples; of these, eight were significantly stronger in one model than the other. At baseline, there were four common predictors of Year 1 outcomes. Drug-related problems at baseline were positively associated with drug-related problems and symptoms of depression/anxiety at Year 1. African American ethnicity was positively associated with Year 1 cocaine use. Alcohol use at baseline was positively associated with Year 1 alcohol use in both models, although this relationship was stronger in the VA sample. Alcohol use at baseline was also positively associated with Year 5 alcohol use in both models.
Figure 2.
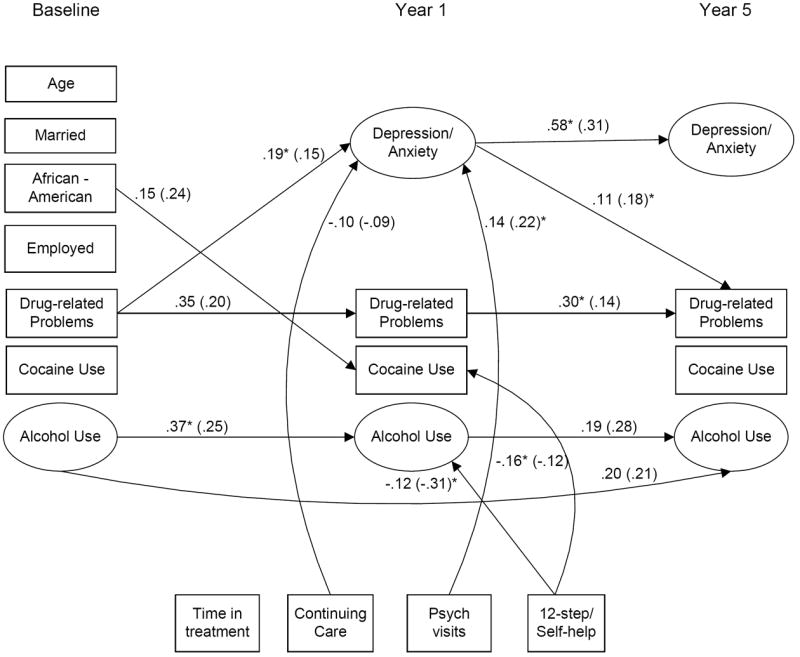
Significant predictors of outcomes common to the HMO and VA samples. HMO regression coefficients in parentheses. Asterisks indicate a significantly larger coefficient in one sample. a < .05, b < .01, c < .001
With regard to service-related predictors of Year 1 outcomes, more continuing care substance use services was associated with less depression/anxiety at Year 1. In contrast, more psychological services received was associated with more depression/anxiety at Year 1, although this relationship was stronger in the HMO sample. Participation in 12-step/self-help groups following treatment was associated with less cocaine and alcohol use in both models. However, the effects of 12-step/self-help participation were significantly stronger on alcohol use in the HMO model and on cocaine use in the VA model.
With regard to Year 1 predictors of Year 5 outcomes, depression/anxiety at Year 1 was positively associated with Year 5 depression/anxiety in both samples. Similarly, Year 1 depression/anxiety was positively associated with Year 5 drug problems. Year 1 drug-related problems and Year 1 alcohol use were both significantly associated with their respective Year 5 counterparts.
3.3.2. Pathways unique to the HMO sample
Figure 3 depicts the 5 significant paths that were unique to the HMO model; only two of these were significantly different when tested against the same (non-significant) pathway in the VA sample. Age was positively associated with Year 1 alcohol use in the HMO sample. More psychological service visits was associated with less Year 1 alcohol use in the HMO sample.
Figure 3.
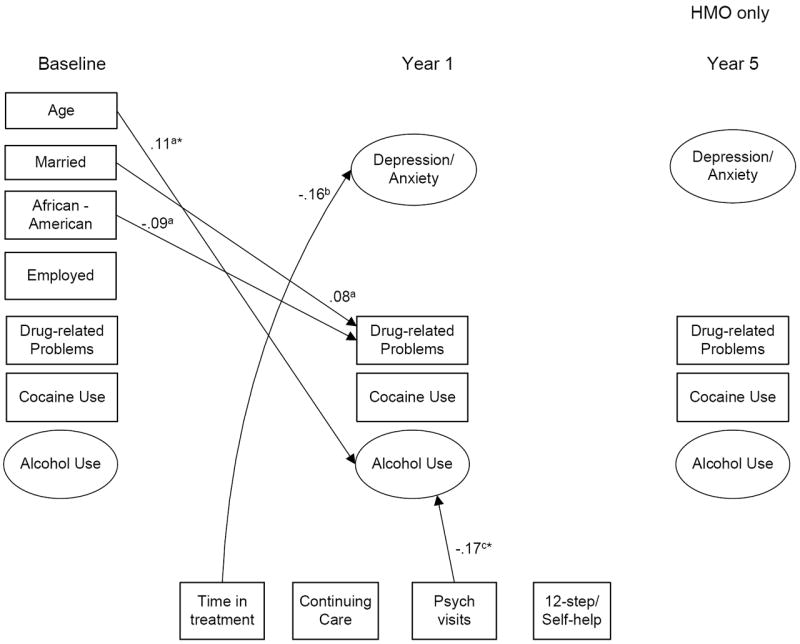
Significant predictors of outcomes unique to the HMO sample; asterisks indicate that the path coefficient is significantly different from VA path model. a < .05, b < .01, c < .001
3.3.3. Pathways unique to the VA sample
Figure 4 depicts the 16 significant paths that were unique to the VA model; of these, 8 were significantly different when tested against the parallel (non-significant) paths in the HMO sample. There were two unique relationships between baseline predictors and Year 1 outcomes. Baseline alcohol use was positively associated with Year 1 depression/anxiety and baseline cocaine use was positively associated with Year 1 cocaine use in the VA sample only.
Figure 4.
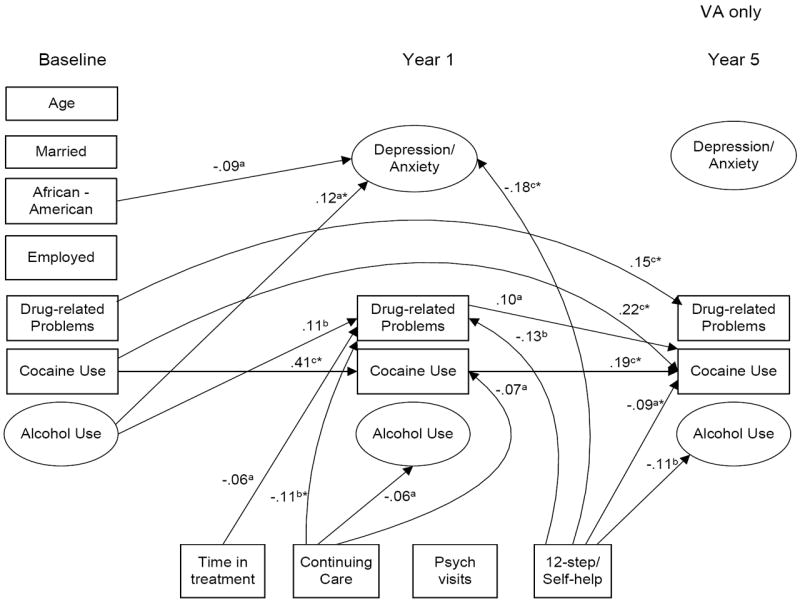
Significant predictors of outcomes unique to the VA sample; asterisks indicate that the path coefficient is significantly different from the HMO path model. a < .05, b < .01, c < .001
With regard to the service-related variables, more continuing care visits was negatively associated with Year 1 drug-related problems. More 12-step/self-help group participation was negatively associated with both Year 1 depression/anxiety and Year 5 cocaine use. Cocaine use and drug-related problems at baseline were positively associated with their respective Year 5 counterparts. Lastly, Year 1 cocaine use was positively associated with Year 5 cocaine use in the VA sample.
3.4. Supplementary analyses with full VA sample
The final path analysis model was tested with the full VA sample that met study inclusion criteria to ascertain whether any substantive relationships were lost because of less power in the smaller sub-sample as well as whether, by chance, some relationships found for the smaller sample did not hold for the larger sample. The LM test reported 3 additional substantial relationships in the larger sample that were not found in the model with the smaller sample: (1) positive effect of African American ethnicity on cocaine use at Year 5 (.12 [larger sample], .08 [smaller sample]), (2) greater effect of age on anxiety/depression at Year 1 (.08, .07), and (3) longer time in index treatment and more psychological service visits (.14, .08). There were no significant effects found in the smaller sample that were not also significant in the larger sample.
3.5 Supplementary analysis of gender differences in HMO sample
The initial CFA for the HMO was tested with an additional dichotomous variable representing gender in order to determine if gender moderated any of the relationships between predictors and outcome variables. Female gender was associated with less employment at baseline (r = -.15, p <.01), more psychological service visits (r = .20, p <.001), more symptoms of anxiety/depression at Year 5 (r = .20, p <.001), and less Alcohol Use at Year 5 (r = -.15, p <.01). The same differences reported in Table 3 emerged when the HMO CFA model included significant gender relationships in the cross-sample comparison.
The significant relationships found in the CFA including gender were added to the final path models both in the individual HMO model and in the multi-group comparison model to assure that the other relationships would still hold with the variance explained by gender included. No pathways changed substantially due to the addition of gender to the HMO model, although gender was an additional significant predictor of more depression/anxiety at Year 5 and less alcohol use at Year 5.
4. Discussion
The goal of this study was to assess relationships among (1) patient characteristics at admission to substance use disorder treatment, (2) continuing care services for substance use problems, mental health services, and 12-step/self-help group participation following treatment, and (3) mental health and substance use outcomes at 1 to 5 years post-treatment for patients with both substance use disorders and mental health problems. We sought to extend prior research in this area by contrasting the longitudinal relationships among common constructs for participants of comparable mental health severity who were sampled from one of two large integrated health care systems.
The main study findings are generally consistent with the literature on treatment outcomes of patients in substance use disorder treatment in that longer time in treatment, more continuing care services, and more participation in 12-step/self-help groups predicted better outcomes. Furthermore, mental health symptoms persisted over time and were associated with more enduring drug-related problems. This finding is consistent with the general consensus that both substance use and mental health disorders are chronic conditions that often necessitate long-term, continuing care interventions (McLellan et al., 2000; Drake et al., 2008). Receipt of more continuing care services was associated with greater reductions in symptoms of depression/anxiety, and more participation in 12-step/self-help groups was associated with greater reductions in cocaine and alcohol use. The study findings showed that these relationships were, for the most part, consistent across patients sampled from these two service delivery systems, despite some differences in the characteristics of the two samples, and provide additional support that the relationships are robust across treatment settings (Moggi et al., 2007).
As noted previously, the HMO sample was generally younger and more often married and employed, as compared with the VA sample, which had a higher proportion of African Americans. Although African Americans in both samples were more likely than others to use cocaine, there was a stronger association between African American ethnicity, younger age, less alcohol use, and more cocaine use among those in the VA. These differences most likely reflect eligibility-based selection factors influencing the populations that access these two health care systems. Although there were strong positive correlations between African Americans and cocaine use in both samples, African American ethnicity and drug-related problems at baseline were unrelated in the VA sample and were negatively associated in the HMO sample. This finding may be due to differential attribution of problems to substance use by ethnicity, a possibility that has been addressed in other studies (Longshore et al., 1998).
Further, the VA sample contained no women at the time the study was conducted; inclusion of gender in the HMO model did not change any of the substantive relationships between predictors and outcomes. Moreover, relationships with gender and outcomes (i.e., women had more depression/anxiety and less alcohol use at Year 5) are consistent with gender differences in these disorders in the general population (Grant and Weissman, 2007).
The study findings regarding commonalities in relationships over time, despite these differences in socio-demographic and substance use characteristics of the patient populations, provide further evidence of the longitudinal relationships between services utilization and treatment outcomes. Moreover, the current study is unique in its focus on two large health service providers in which substance use disorder treatment and mental health services are provided within self-contained health care delivery systems. Much of the prior research on service delivery patients with patients with co-occurring substance use and mental health problems has focused on single programs that are either specialized for treatment of one disorder or the other or in which specialized services or integrated treatment “tracks” are provided (Tiet and Mausbach, 2007). In the current study, all patients were eligible for the full range of services, including substance use disorder and mental health treatment. Thus, the obstacles to providing integrated treatment for co-occurring substance use and mental health disorders that are commonly cited by addiction treatment providers, such as lack of resources or staff with appropriate expertise (McGovern et al., 2006), or problems in linking patients to providers in two separate service delivery systems (Havassy et al., 2009), are minimized to the extent that patients are assessed and referred for needed services within these self-contained systems.
There were also some important differences in the direction and strength of some relationships. As noted, there were positive associations between substance use and related problems over time in both samples, but these appeared to be stronger and more enduring among the VA sample. Drug-related problems were persistent from baseline to Year 1 in both samples; however, more time in treatment and continuing care services and greater participation in 12-step/self-help groups was associated with reductions in drug use and related problems in Year 1 among the VA sample (but not the HMO sample). In contrast, greater participation in mental health services was associated with reductions in alcohol use at Year 1 in the HMO sample only. Similarly, there was a stronger relationship between participation in 12-step/self-help groups and less alcohol use among the HMO sample at Year 1. It is possible that mental health treatment had a greater impact on alcohol use among patients in the HMO, particularly for patients whose alcohol use was primarily a result of their mental health problems. Conversely, individuals who reduced their alcohol use may have been more likely to engage in mental health services. Similarly, participation in 12-step/self-help groups among patients in the VA may have led to greater reductions in psychological symptoms concurrent with reductions in their cocaine and alcohol use.
Interestingly, more continuing care visits for substance use treatment was associated with reductions in symptoms of depression/anxiety at follow-up in both samples. This finding may demonstrate the beneficial effects of continuing care following the index treatment episode for mental health outcomes; or conversely, that individuals with less psychological severity are more likely to engage in continuing care following treatment. This finding is consistent with a study of psychiatric inpatients with co-occurring disorders in the VA system, which demonstrated that receipt of continuing care for substance use disorders lessened the likelihood of psychiatric rehospitalization for up to 12 months (Ilgen et al., 2008). Thus, there may be a “cross-over” effect of continuing care for substance use disorders on reducing mental health problems (Tiet and Mausbach, 2007). In contrast, more outpatient mental health visits was associated with more symptoms of depression/anxiety at follow-up in both samples. Patients who were referred into mental health services from substance use disorder treatment may have more severe disorders and more enduring psychological problems, leading to higher levels of service use. Thus, the study findings help to clarify the question posed at the outset as to whether repeated use of services among individuals with co-occurring substance use and mental health problems results in their improved functioning over time, or is a marker for continued symptom severity. In the current study, greater involvement in continuing care and more 12-step/self-help participation were associated with improvements in substance use and mental health symptoms, whereas more mental health services received appeared to function as a marker for greater problem severity over time.
With regard to longer-term outcomes, drug-related problems were more enduring among the VA sample, with stronger positive relationships from baseline to Year 1 and from Year 1 to Year 5. Similarly, cocaine use was strongly associated across the three time points among patients in the VA, but not among those in the HMO, although alcohol use was strongly associated across the three time points in both samples. Of note, although cocaine use was more enduring among patients in the VA sample, both continuing care visits and participation in 12-step/self-help groups were associated with reductions in cocaine use over time among patients in the VA, but not among those in the HMO.
4.1. Study limitations
The findings from this study need to be interpreted within the context of several potential limitations stemming from the study design. In the process of constructing comparable variables, ranges and distributions were examined, and several variables were rescaled to create comparable distributions. It is possible that in doing so, ranges may have become overly restricted and the underlying structure of the data may have become somewhat distorted. However, we only used correlations or regression coefficients which should reflect the underlying relationships between the items of interest in the study even if their means and dispersion vary somewhat. Furthermore, many items are completely alike or highly comparable, especially those concerning demographics and service utilization. In addition, measures of “drug-related problems” are based on individual attributions; as noted previously, individuals may differ in how they construe their problems, which may be multiply caused by substance use and mental health problems. Nevertheless, the relative robustness of the findings across the two study samples suggest that these measurement issues may have reduced strength of the observed associations, yielding a conservative bias to our findings (i.e., increased confidence in observed associations despite possible bias introduced by lack of identical measures).
Another limitation is that administrative data obtained from the two service systems always contain the possibility of error that cannot be verified (Hser and Evans, 2008). Lastly, because of the observational study design, associations observed among variables in the path models, although longitudinal, cannot be assumed to be causal in nature ands study findings need to be interpreted in this context. It is possible that there is a bi-directional effect between services use and outcomes in which individuals who display better treatment outcomes are more likely to be retained in treatment longer or to engage in continuing care services, thus reflecting a possible self-selection effect.
4.2. Conclusions
In sum, similar relationships were observed in the longitudinal associations between participation in continuing care services and 12-step/self-help groups with substance use and mental health outcomes among patients treated in one of two integrated health delivery systems. The study findings provide support that these associations are independent of the unique characteristics of the treatment settings or patient populations. There were some differences across treatment settings with regard to outcomes associated with different types of substance use (i.e., alcohol, cocaine), which highlight the unique treatment needs of the two patient populations. Future research can aim to unpack the effects of treatment and services participation on patterns of substance use and mental health problems in order to determine the optimal organization of service delivery.
Supplementary Material
Footnotes
Supplementary material for this article is available with the full text online version at doi:xxx/J.drugalcdep.xxx …
Information on the exact wording of the relevant variables in each dataset, variable means (SD), ranges, and methods for recoding of measures is available as supplemental material to this article at doi:xxx/j.drugalcdep.xxx.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Bentler PM. EQS 6 Structural Equations Program Manual. Multivariate Software, Inc.; Encino, CA: in press. [Google Scholar]
- Bentler PM, Dudgeon P. Covariance structure analysis: statistical practice, theory, and directions. Ann Rev Psychol. 1996;47:563–592. doi: 10.1146/annurev.psych.47.1.563. [DOI] [PubMed] [Google Scholar]
- Bond J, Kaskutas LA, Weisner C. The persistent influence of social networks and alcoholics anonymous on abstinence. J Stud Alcohol. 2003;64(4):579–588. doi: 10.15288/jsa.2003.64.579. [DOI] [PubMed] [Google Scholar]
- Cacciola JS, Pecoraro A, Alterman AI. Development of ASI psychiatric severity cut-off scores to identify co-occurring psychiatric disorders. Int J Ment Health Addict. 2008;6:77–92. [Google Scholar]
- Carroll KM, Power MD, Bryant KJ, Rounsaville BJ. One-year follow-up status of treatment-seeking cocaine abusers: psychopathology and dependence severity as predictors of outcome. J Nerv Ment Dis. 1993;181(2):71–79. doi: 10.1097/00005053-199302000-00001. [DOI] [PubMed] [Google Scholar]
- Chi FW, Satre DD, Weisner C. Chemical dependency patients with co-occurring psychiatric diagnoses: service patterns and 1-year outcomes. Alcohol Clin Exp Res. 2006;30:851–859. doi: 10.1111/j.1530-0277.2006.00100.x. [DOI] [PubMed] [Google Scholar]
- Chi FW, Weisner CM. Nine-year psychiatric trajectories and substance use outcomes: an application of the group-based modeling approach. Eval Rev. 2008;32(1):39–58. doi: 10.1177/0193841X07307317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chou C-P, Bentler PM. Model modification in covariance structure modeling: a comparison among likelihood ratio, Lagrange multiplier, and Wald tests. Multivariate Behav Res. 1990;25:115–136. doi: 10.1207/s15327906mbr2501_13. [DOI] [PubMed] [Google Scholar]
- Compton WM, Cottler LB, Jacobs JL, Ben-Abdallah A, Spitznagel EL. The role of psychiatric disorders in predicting drug dependence treatment outcomes. Am J Soc Psychiatry. 2003;160(5):890–895. doi: 10.1176/appi.ajp.160.5.890. [DOI] [PubMed] [Google Scholar]
- Dennis ML, Foss MA, Scott CK. An eight-year perspective on the relationship between the duration of abstinence and other aspects of recovery. Eval Rev. 2007;31(6):585–612. doi: 10.1177/0193841X07307771. [DOI] [PubMed] [Google Scholar]
- Dennis ML, Scott CK, Funk R, Foss MA. The duration and correlates of addiction and treatment careers. J Subst Abuse Treat. 2005;28(supplement 1):S51–62. doi: 10.1016/j.jsat.2004.10.013. [DOI] [PubMed] [Google Scholar]
- Derogatis LR, Melisaratos N. The brief symptom inventory: an introduction report. Psych Med. 1983;13:595–605. [PubMed] [Google Scholar]
- Drake RE, O’Neal EL, Wallach MA. A systematic review of psychosocial research on psychosocial interventions for people with co-occurring severe mental and substance use disorders. J Subst Abuse Treat. 2008;34:123–138. doi: 10.1016/j.jsat.2007.01.011. [DOI] [PubMed] [Google Scholar]
- Finney J, Ouimette PC, Humphreys K, Moos RH. A comparative, process-evaluation of VA substance abuse treatment. In: Galanter M, editor. Recent Developments In Alcoholism: Services Research in the Era of Managed Care. Kluwer Academic/Plenum; New York: 2001. pp. 373–391. [DOI] [PubMed] [Google Scholar]
- Gonzalez G, Rosenheck RA. Outcomes and service use among homeless persons with serious mental illness and substance abuse. Psychiatr Serv. 2002;53:437–446. doi: 10.1176/appi.ps.53.4.437. [DOI] [PubMed] [Google Scholar]
- Gossop M, Steward D, Marsden J. Attendance at narcotics anonymous and alcoholics anonymous meetings, frequency of attendance and substance use outcomes after residential treatment for drug dependence: a 5-year follow-up study. Addiction. 2007;103:119–125. doi: 10.1111/j.1360-0443.2007.02050.x. [DOI] [PubMed] [Google Scholar]
- Grant BF, Weissman MM. Gender and the prevalence of psychiatric disorders. In: Narrow WE, First MB, Sirovatk M, Regier DA, editors. Age and Gender Considerations in Psychiatric Diagnosis: A Research Agenda for DSM-V. American Psychiatric Association; Arlington, VA: 2007. pp. 31–45. [Google Scholar]
- Havassy BE, Alvidrez J, Mericle AA. Disparities in use of mental health and substance abuse services by persons with co-occurring disorders. Psychiatr Serv. 2009;60(2):217–223. doi: 10.1176/appi.ps.60.2.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herman SE, Frank KA, Mowbray CT, Ribisl KM, Davidson WS, BootsMiller B, Jordan L, Greenfield AL, Loveland D, Luke DA. Longitudinal effects of integrated treatment on alcohol use for persons with serious mental illness and substance use disorders. J Behav Health Serv Res. 2000;27(3):286–302. doi: 10.1007/BF02291740. [DOI] [PubMed] [Google Scholar]
- Hser YI, Evans E. Cross-system data linkage for treatment outcome evaluation: lessons learned from the California Treatment Outcome Project. Eval Program Plann. 2008;31(2):125–135. doi: 10.1016/j.evalprogplan.2008.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hser YI, Evans E, Huang D, Anglin DM. Relationship between drug treatment services, retention, and outcomes. Psychiatr Serv. 2004;55(7):767–774. doi: 10.1176/appi.ps.55.7.767. [DOI] [PubMed] [Google Scholar]
- Hser YI, Grella CE, Evans E, Huang YC. Utilization and outcomes of mental health services among patients in drug treatment. J Addict Dis. 2006;25(1):73–85. doi: 10.1300/J069v25n01_10. [DOI] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equation Model. 1999;6:1–55. [Google Scholar]
- Humphreys K, Moos RH. Encouraging posttreatment self-help group involvement to reduce demand for continuing care services: two-year clinical and utilization outcomes. Alcohol Clin Exp Res. 2007;31(1):64–68. doi: 10.1111/j.1530-0277.2006.00273.x. [DOI] [PubMed] [Google Scholar]
- Ilgen MA, Hu KU, Moos RH, McKellar J. Continuing care after inpatient psychiatric treatment for patients with psychiatric and substance use disorders. Psychiatr Serv. 2008;59:982–988. doi: 10.1176/ps.2008.59.9.982. [DOI] [PubMed] [Google Scholar]
- Laudet AB. The road to recovery: where are we going and how do we get there? empirically driven conclusions and future directions for service development and research. Subst Use Misuse. 2008;43:2001–2020. doi: 10.1080/10826080802293459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Longshore D, Grills C, Annon K, Grady R. Promoting recovery from drug abuse: an Africentric intervention. J Black Stud. 1998;28(3):319–333. [Google Scholar]
- MacCallum R. Specification searches in covariance structure modeling. Psychol Bull. 1986;100:107–120. [Google Scholar]
- McGovern MP, Wrisley BR, Drake RE. Relapse of substance use disorder and its prevention among persons with co-occurring disorders. Psychiatr Serv. 2005;56(10):1270–1273. doi: 10.1176/appi.ps.56.10.1270. [DOI] [PubMed] [Google Scholar]
- McGovern MP, Xie H, Segal SR, Siembab L, Drake RE. Addiction treatment services and co-occurring disorders: prevalence estimates, treatment practices, and barriers. J Subst Abuse Treat. 2006;31:267–275. doi: 10.1016/j.jsat.2006.05.003. [DOI] [PubMed] [Google Scholar]
- McKay JR. Effectiveness of continuing care interventions for substance abusers: implications for the study of long-term treatment effects. Eval Rev. 2001;25:211–232. doi: 10.1177/0193841X0102500205. [DOI] [PubMed] [Google Scholar]
- McKay JR. Continuing care research: what we have learned and where we are going. J Subst Abuse Treat. 2009;36(2):131–145. doi: 10.1016/j.jsat.2008.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKay JR, McLellan AT, Alterman AI, Cacciola JS, Rutherford MR, O’Brien CP. Predictors of participation in aftercare sessions and self-help groups following completion of intensive outpatient treatment for substance abuse. J Stud Alcohol. 1998;59:152–162. doi: 10.15288/jsa.1998.59.152. [DOI] [PubMed] [Google Scholar]
- McLellan AT. Have we evaluated addiction treatment correctly? implications from a chronic care perspective. Addiction. 2002;97:249–252. doi: 10.1046/j.1360-0443.2002.00127.x. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Lewis DC, O’Brien CP, Kleber HD. Drug dependence, a chronic medical illness: implications for treatment, insurance, and outcomes evaluation. JAMA. 2000;284:1689–1695. doi: 10.1001/jama.284.13.1689. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Luborsky L, Woody GE, Druley KA, O’Brien CP. Predicting response to alcohol and drug abuse treatments: role of psychiatric severity. Arch Gen Psychiatry. 1983;40:620–625. doi: 10.1001/archpsyc.1983.04390010030004. [DOI] [PubMed] [Google Scholar]
- Moggi F, Giovanoli A, Strik W, Moos BS, Moos RH. Substance use disorder treatment programs in Switzerland and the USA: program characteristics and 1-year outcomes. Drug Alcohol Depend. 2007;86:75–83. doi: 10.1016/j.drugalcdep.2006.05.017. [DOI] [PubMed] [Google Scholar]
- Moos RH, Finney JW, Federman EB, Suchinsky R. Specialty mental health care improves patients’ outcomes: findings from a nationwide program to monitor the quality of care for patients with substance use disorders. J Stud Alcohol. 2000;61(5):704–713. doi: 10.15288/jsa.2000.61.704. [DOI] [PubMed] [Google Scholar]
- Moos RH, King MJ, Patterson MA. Outcomes of residential treatment of substance abuse in hospital- and community-based programs. Psychiatr Serv. 1996;47(1):68–74. doi: 10.1176/ps.47.1.68. [DOI] [PubMed] [Google Scholar]
- Moos RH, Moos BS. Help-seeking careers: connections between participation in professional treatment and alcoholics anonymous. J Subst Abuse Treat. 2004;26(3):167–173. doi: 10.1016/S0740-5472(03)00190-9. [DOI] [PubMed] [Google Scholar]
- Moos R, Schaefer J, Andrassy J, Moos B. Outpatient mental health care, self-help groups, and patients’ 1-year treatment outcomes. J Clinical Psych. 2001;57:273–287. doi: 10.1002/jclp.1011. [DOI] [PubMed] [Google Scholar]
- Ouimette PC, Moos RH, Finney JW. Two-year mental health service use and course of remission in patients with substance use and posttraumatic stress disorders. J Stud Alcohol. 2000;61(2):247–253. doi: 10.15288/jsa.2000.61.247. [DOI] [PubMed] [Google Scholar]
- Ray GT, Weisner CM, Mertens JR. Relationship between use of psychiatric services and five-year alcohol and drug treatment outcomes. Psychiatr Serv. 2005;56(2):164–171. doi: 10.1176/appi.ps.56.2.164. [DOI] [PubMed] [Google Scholar]
- Ritsher JB, McKellar JD, Finney JW, Otilingam PG, Moos RH. Psychiatric comorbidity, continuing care and mutual help as predictors of five-year remission from substance use disorders. J Stud Alcohol. 2002;63(6):709–715. doi: 10.15288/jsa.2002.63.709. [DOI] [PubMed] [Google Scholar]
- Ritsher JB, Moos RH, Finney JW. Relationship of treatment orientation and continuing care to remission among substance abuse patients. Psychiatr Serv. 2002;53(5):595–601. doi: 10.1176/appi.ps.53.5.595. [DOI] [PubMed] [Google Scholar]
- Rounsaville BJ, Dolinsky ZS, Babor TF, Meyer RE. Psychopathology as a predictor of treatment outcome in alcoholics. Arch Gen Psychiatry. 1987;44(6):505–513. doi: 10.1001/archpsyc.1987.01800180015002. [DOI] [PubMed] [Google Scholar]
- Rush BR, Dennis ML, Scott CK, Castel S, Funk RR. The interaction of co-occurring mental disorders and recovery management checkups on substance abuse treatment participation and recovery. Eval Rev. 0208;32(1):7–38. doi: 10.1177/0193841X07307532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott CK, Foss MA, Dennis ML. Pathways in the relapse-treatment-recovery cycle over 3 years. J Subst Abuse Treat. 2005;28:S63–S72. doi: 10.1016/j.jsat.2004.09.006. [DOI] [PubMed] [Google Scholar]
- Tiet QQ, Mausbach B. Treatments for patients with dual diagnosis: a review. Alcohol Clin Exp Res. 2007;31(4):513–536. doi: 10.1111/j.1530-0277.2007.00336.x. [DOI] [PubMed] [Google Scholar]
- Weisner C, Matzger H, Kaskutas LA. How important is treatment? one-year outcomes of treated and untreated alcohol-dependent individuals. Addiction. 2003;98(7):901–911. doi: 10.1046/j.1360-0443.2003.00438.x. [DOI] [PubMed] [Google Scholar]
- Weisner C, Mertens J, Tam T, Moore C. Factors affecting the initiation of substance abuse treatment in managed care. Addiction. 2001;96(5):705–716. doi: 10.1046/j.1360-0443.2001.9657056.x. [DOI] [PubMed] [Google Scholar]
- Weisner C, Ray GT, Mertens JR, Satre DD, Moore C. Short-term alcohol and drug treatment outcomes predict long-term outcome. Drug Alcohol Depend. 2003;71(3):281–294. doi: 10.1016/s0376-8716(03)00167-4. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


