Abstract
Objective
Most Americans do not meet physical activity recommendations. Statewide campaigns can effectively increase activity levels. Reported herein are physical activity outcomes from Shape Up Rhode Island (SURI) 2007, a statewide campaign to increase steps through team-based competition. Given the importance of social networks in behavior change, this paper focused on the effects of team and team characteristics on activity outcomes.
Method
For 16-weeks, 5333 adults comprising 652 teams wore pedometers and reported their steps online.
Results
Participants’ daily steps increased from 7029(3915) at baseline to 9393(5976) at SURI end (p<.001). There was a significant intraclass correlation for step change among team members (ICC=.09); thus, an individual’s change in steps was influenced by what team they were on. Moreover, baseline team characteristics predicted individual step change; being on a more active team was associated with greater increases in activity for individual members (p<.001), whereas being on a team with a broad range of steps was associated with smaller changes in activity for individual members (p=.02).
Conclusion
These findings are the first to suggest that team members influence individual activity outcomes in team-based statewide campaigns. Future research should explore ways to use social network factors to enhance team-based physical activity programs.
Keywords: statewide pedometer intervention, physical activity, social networks, social influence
Introduction
Regular physical activity decreases risk for obesity, cardiovascular disease, type 2 diabetes, and all-cause mortality (Pate et al., 1995). Despite its benefits, over two-thirds of American adults are not regularly active and one-quarter are completely inactive (CDC, 2007). The public health recommendation is to accumulate at least 30-minutes of moderate-intensity physical activity on 5 or more days per week (USDHHS, 2008). Ten-thousand steps per day is another well-adopted guideline consistent with these recommendations and associated with significant health benefits (Tudor-Locke et al., 2008); in a review Bravata (2007) found that pedometer interventions with a goal of 10,000 steps/day increased activity by 2491 steps/day and improved Body Mass Index (BMI), blood pressure, cholesterol, and glucose tolerance.
To address the public health problem of the large number of Americans who are inactive and at increased health risk, there has been a surge in team-based community or statewide competitions that promote physical activity with the use of pedometers. These interventions encourage teams to work together and compete with other teams on physical activity. Step change associated with these interventions has ranged from an increase in 388 steps/week (Behrens et al., 2007) to over 2000 steps/day (Wyatt et al., 2004). Even though teams are an important aspect of these programs and evidence suggests that social networks influence health behavior change (Christakis & Fowler, 2008), no one has examined the impact of team and team characteristics on individuals’ activity outcomes during these large, team-based competitions.
This study examines the effects of a statewide team-based physical activity campaign on step change. Although weight change associated with this campaign was previously reported for participants in the weight competition (Wing et al., 2009), this paper focuses on the primary outcome of the intervention, physical activity. Change in pedometer steps was the dependent variable, with a particular focus on team as a determinant of step change. Specifically, this paper addresses the important question of whether team membership and team characteristics influence individual team members’ step change.
Methods
Participants
All adults who lived or worked in Rhode Island were eligible to participate in the 2007 Shape Up Rhode Island (SURI) campaign. Participants were recruited via televised advertisements, press releases, and the distribution of campaign information to employers. Participants enrolled in teams of 7 to 10 members. A total of 5333 individuals on 652 teams entered the pedometer division of the campaign and provided baseline pedometer data. See Table 1.
Table 1.
Baseline characteristics of participants in the Shape Up Rhode Island statewide campaign, USA, 2007.
| All Enrolled (n = 5333) | Completers (n = 4087) | Non- completers (n = 1246) | Completers vs. Non- completers | ||
|---|---|---|---|---|---|
| X2 or F value | p | ||||
| Male (n (%)) | 877 (16.4) | 692 (16.9%) | 185 (14.8) | 3.0 | .08 |
| Age (years; M (SD)) | 42.6 (11.0) | 43.2 (11.0) | 40.7 (11.0) | 48.1 | <.001 |
| Weight (lbs; M (SD))* | 178.0 (43.4) | 176.7 (43.1) | 181.7 (44.2) | 10.4 | .001 |
| BMI (kg/m2M (SD))* | 29.3 (6.4) | 29.1 (6.3) | 30.0 (6.5) | 17.6 | <.001 |
| Company Pay (n (%)) | 3516 (65.9) | 2709 (66.3) | 807 (64.8) | 1.0 | .32 |
| Steps/day (M (SD)) | 7029 (3915) | 7268 (3650) | 6244 (4594) | 66.1 | <.001 |
| Activity Level (steps/day) | n (%) | n (%) | n (%) | 33.8 (overall) | <.001 |
| Sedentary (< 5,000) | 1511 (28.3) | 994 (24.3) | 517 (41.5) | 131.8 | <.001 |
| Low Active (5,000–7,499) | 1601 (30.0) | 1265 (31.0) | 336 (27.0) | 5.7 | .01 |
| Somewhat Active (7,500–9,999) | 1367 (25.6) | 1130 (27.6) | 237 (19.0) | 38.1 | <.001 |
| Active (≥ 10,000) | 854 (16.0) | 698 (17.1) | 156 (12.5) | 14.0 | <.001 |
Note: Weight and height were requested only from participants who entered the weight loss division of Shape Up Rhode Island (n=4,082).
Procedure
SURI 2007 was a 16-week team-based online competition focused on increasing physical activity. A $15 registration fee was charged, however, for most individuals, their employer paid this fee. Teams were formed by a self-selected captain who recruited team members, monitored their team’s progress, and motivated their team by setting goals. Team captains received no formal training and were free to choose whomever they wanted on their team.
Program components were consistent with social cognitive and social learning theories (Bandura, 1977; Bandura, 1977), with a particular focus on self-monitoring, goal setting, feedback, and social support. At the beginning of SURI, participants were provided pedometers and a log to record steps; pedometers and self-monitoring records allowed participants to track progress towards step goals. Participants had access to an online tracking system throughout the entire 16-week competition, which consisted of 8 rounds lasting 2-weeks each. At the end of each round (every 2-weeks) participants entered the sum of their steps from their previous 2-weeks’ pedometer log and received feedback on their performance relative to their personal and team goals via the online system. SURI encouraged teams to exercise together and support one another in pursuit of activity goals. SURI also provided motivational and educational activities including an opening event, media promotion, free fitness events, healthy eating and activity workshops and newsletters, and a closing event attended by local and national politicians.
Measures
Participants were given a Sportline 340 Step and Distance Pedometer®. This instrument is 99% reliable (walking the same distance several times produces nearly identical step-counts) and valid (distance indicated on the device is consistent with odometer readings) (Pope, 2005). Demographics and team variables were obtained from the online system. The following team variables were examined: Team Size (number of participants on each team), Team Age Range (age of oldest member minus age of youngest), Percent Male, Team Baseline Steps (average steps of each team at baseline), and Team Baseline Step Range (steps of most active member minus steps of the least).
Statistical analyses
Analyses examined the effects of SURI and the effects of team and team characteristics on individual step change:
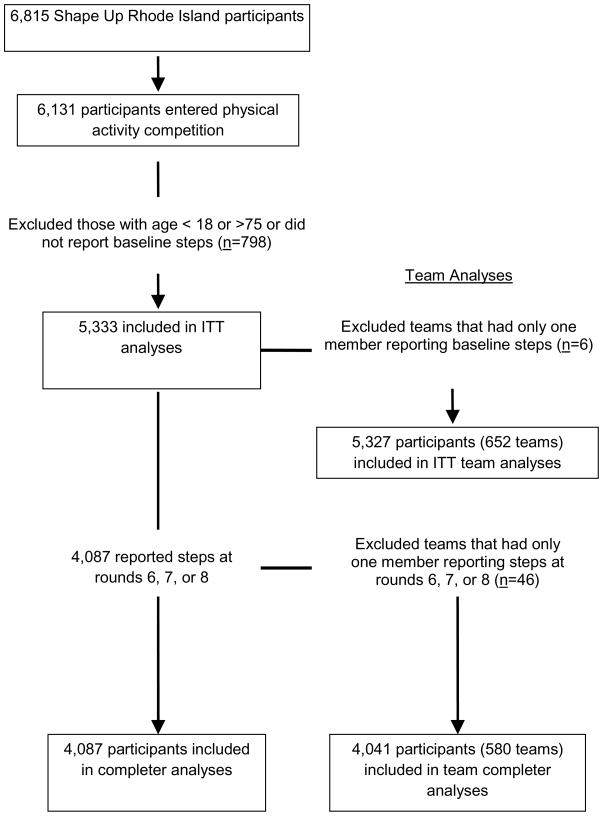
Given that similar pedometer interventions are 12–14 weeks long (e.g., Behrens et al., 2007; Dishman et al., 2009; Wyatt et al., 2004), SURI completers were defined as individuals who reported steps at Rounds 6, 7, or 8, which corresponded to weeks 12, 14, or 16 of the competition. See Figure 1 for participant and team flow. Of the 4087 completers, 3430 (84%) last reported steps at Round 8; whereas only 328 participants and 329 participants last reported their steps at Rounds 7 and 6, respectively. For completers (n=4087; Teams=580), step change was computed as steps/day at Rounds 6, 7, or 8 minus steps/day at baseline. Intent-to-treat (ITT) analyses were also conducted (n=5333; Teams=652); participants who dropped out before Round 6 were assumed to have not sustained any changes in activity, but rather returned to their baseline steps. Step change and group differences in step change were analyzed using analyses of covariance, adjusting for baseline steps. Adjustments were made for multiple comparisons. Given that step categories (e.g., sedentary, active) are associated with health parameters (e.g., cardiovascular disease), a McNemar test was conducted to examine whether the proportion of participants in each step category changed from baseline to SURI end. Means and standard deviations are reported, where appropriate. Data were analyzed using Statistical Package for the Social Sciences, Version 14.0.
Figure 1.
Participant and team flow for the Shape Up Rhode Island statewide campaign, USA, 2007.
The effects of team and team characteristics on individuals’ change in steps were examined using Hierarchical Linear Modeling (HLM) (Bryk & Raudenbush, 1992). Variables were grand mean centered and the following equations were used:
Level-1:1
Level-2:1
Individual step change was the dependent variable. To examine team effects beyond individual effects, participant gender, age, and baseline steps were included in Level-1. At Level-2, individuals were nested within teams to examine the effects of team variables (e.g., Team Size) on individual step change.
Results
Baseline steps & demographics
Participants reported 7029(3915) steps/day at program entry. Seventy-six percent of participants (n=4087) completed at least 6 of the 8 rounds. Compared to non-completers, completers were older, had a lower BMI and reported more baseline steps. See Table 1.
Changes in Physical Activity
Individual effects
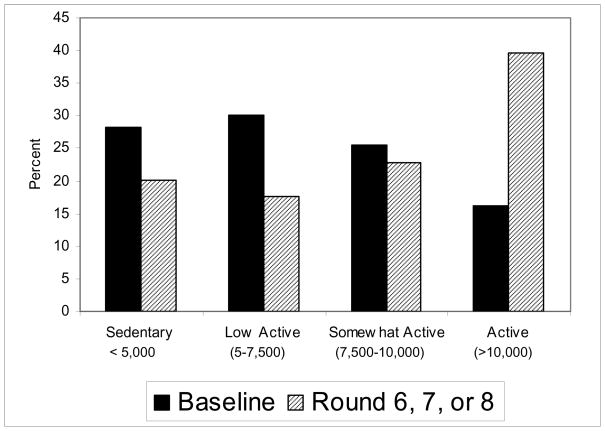
On average, physical activity increased by 3085 steps/day for completers and by 2364 steps/day for the full sample (ITT analyses). Using ITT outcomes, SURI produced dramatic changes in the proportion of individuals who reported being active (Figure 2). The percent of participants who were considered sedentary, low active, or somewhat active decreased from 84% at baseline to 61% at SURI end. In contrast, the proportion considered active increased from 16% at baseline to 40% at the end (p<.001).
Figure 2.
Change in percentage of participants at each activity level during the Shape Up Rhode Island statewide campaign, USA, 2007.
The strongest individual characteristic associated with step change was baseline activity, with greater increases in those less active at baseline (p<.001). Step change was also greater for men (p=.02), less overweight individuals (p=.03), and individuals whose company paid their enrollment (p=.05). Effects were similar for completers. See Table 2.
Table 2.
Differences in change in steps by baseline characteristics for intent-to-treat and completer samples in Shape Up Rhode Island statewide campaign, USA, 2007.
| Intent-to-treat (n = 5333) | Completers (n = 4087) | |
|---|---|---|
| Mean (SD) | Mean (SD) | |
| Overall | 2364 (5107) | 3085 (5640) |
| Gender | ||
| Male | 2606 (5656) a | 3303 (6186) a |
| Female | 2317 (4991)b | 3040 (5522) b |
| Age (years) | ||
| 18–35 | 2472 (5304) a | 3453 (5993) a |
| 36–50 | 2420 (5220) a | 3137 (5751) a |
| >50 | 2151 (4671) a | 2650 (5056) b |
| BMI* | ||
| Normal | 2450 (4669) a | 3183 (5099) a |
| Overweight | 2291 (5036) a | 3011 (5582) a,b |
| Obese | 1923 (5693) b | 2687 (6576) b |
| Payment | ||
| Company Pay | 2475 (4934) a | 3212 (5407) a |
| Self Pay | 2150 (5421) b | 2834 (6067) a |
| Baseline PA Level | ||
| Sedentary | 2696 (4503) a | 4098 (5008) a |
| Low Active | 2506 (4853) a,b | 3172 (5263) b |
| Somewhat Active | 2206 (4724) b | 2669 (5076) b,c |
| Active | 1764 (6826) c | 2163 (7534) c |
Within groupings, values with different subscripts (a,b,c) differ significantly from each other (p<.05). For example, in Completer BMI analyses, normal weight participants had a greater increase in steps compared to obese participants (a v. b); however, overweight participants did not differ in change in steps from normal weight or obese participants (as shown by shared subscripts (a,b) with both normal weight and obese).
Normal weight =18.5 to 24.9kg/m2; Overweight = 25 to 29.9kg/m2; Obese ≥ 30kg/m2
Team Effects
Participants in SURI represented 652 teams. On average teams had 8.2(2.4) members, a large age range (26.1(8.8)years), and a small percentage of men (16.3(18.6)). Average number of daily steps completed by each team at baseline was 6887(2048). The average range of steps within teams was 9360.
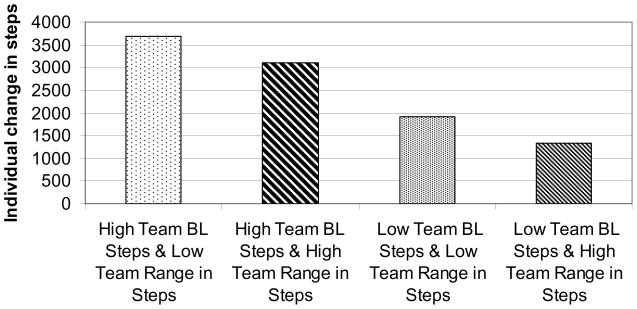
HLM analyses (Table 3) showed a team effect for step change (p<.001; ICC=.09, indicating a small/medium effect (Hox, 2002)), suggesting that an individual’s step change was influenced by which team they were on. In addition, there was a positive effect of Team Baseline Steps (p<.001) and a negative effect for Baseline Step Range (p=.02). Being on a team with higher baseline steps was associated with greater increases in activity for an individual member of the team, whereas being on a team with a broad range of activity levels (some active and some inactive members) was associated with smaller changes in activity for individual members. Similar results were obtained in completer analyses.
Table 3.
Effects of team and team characteristics on change in steps in Shape Up Rhode Island statewide campaign, USA, 2007.
| Intent-to-treat | Completers | |||||
|---|---|---|---|---|---|---|
| γ* | (SE) | p | γ* | (SE) | p | |
| Team | 2356.6 | (91.1) | <.001 | 3043.1 | (107.7) | <.001 |
| Team size | 18.4 | (48.5) | .71 | −124.5 | (61.6) | .04 |
| Age range# | 62.4 | (60.3) | .30 | 43.6 | (72.3) | .55 |
| % male | 5.0 | (5.3) | .35 | 1.8 | (5.7) | .75 |
| Baseline step range‡ | −49.4 | (21.5) | .02 | −37.4 | (19.6) | .06 |
| Baseline step mean‡ | 435.6 | (92.3) | <.001 | 452.8 | (109.6) | <.001 |
γ is the main effect for each team variable on participants’ change in steps.
Age range is in 5 year units.
Baseline step range and baseline step mean are per 1000 steps.
To illustrate these findings, two examples are provided using the HLM equations and coefficients. “High” and “low” team baseline step and step range are defined as one standard deviation above and below the mean, respectively. If the average SURI participant (gender=female, age=42) was placed on a team with “high” baseline steps and “low” baseline step range, that participant would be predicted to increase activity by 3442 steps/day. However, if the same participant were put on a team with a “low” level of baseline steps and a “high” range, activity would only increase by 1072 steps/day. See Figure 3.
Figure 3.
Four hypothetical scenarios: Individual change in steps depending on team characteristics during the Shape Up Rhode Island statewide campaign, USA, 2007.
Discussion
Shape Up Rhode Island (SURI) increased physical activity by an average of over 2000 steps/day. Moreover, this campaign increased the proportion of individuals considered “active” from 16% at baseline to 40% at follow-up. The primary focus of this study was to determine whether teammates and team characteristics influenced change in steps during the campaign; interestingly, findings suggest that social contacts (i.e. teammates) and network characteristics (i.e. team characteristics) influence individual step change.
The effects of SURI on step change are as good as or better than those observed in other pedometer campaigns. A 14-week program associated with Colorado on the Move increased daily steps from 7669 to 10417 (Wyatt et al., 2004). Recently, Dishman et al. (2009) reported on a 12-week intervention in Georgia that increased pedometer steps by an average of approximately 1000/day. Increases in pedometer steps of the magnitude achieved in SURI have been shown to improve blood pressure, cholesterol, and glucose tolerance (Araiza et al., 2006; Haines et al., 2007; Moreau et al., 2001; Sugiura et al., 2002; Swartz et al., 2003), suggesting that the change in activity associated with this intervention may have important health implications.
While SURI produced significant increases in activity, there was large variability in step change. Both individual and team characteristics accounted for some of the variance. Regarding individual characteristics, the strongest predictor of step increase was baseline steps; those who started low reported the greatest step increases, a finding noted in prior pedometer interventions (Dishman et al., 2009). These findings are important given that increases in activity among inactive individuals (opposed to already active) is associated with the greatest health benefits (Blair et al., 1989). Male and less overweight participants also had greater step increases. Those less overweight may have fewer barriers associated with increasing activity (e.g., less discomfort associated with exercise), resulting in better activity outcomes. There was a trend for participants whose company paid for enrollment to have greater step increases, which may reflect more company support, including promotion of physical activity during work hours (breaks, lunch hour). These findings also suggest that those unemployed or employed by a company that does not support their involvement in a physical activity campaign may be at a disadvantage. Future team-based competitions may increase support for these individuals by helping them develop structured activity plans and identify an exercise partner.
Health behavior change has shown to spread through social networks; Christakis and Fowler (2008) found that smoking cessation is influenced by social contacts. Given these findings, analyses were conducted that examined whether an individual’s team and team characteristics influenced their step change. Team membership affected individual step change; the amount of step change achieved by an individual participant was influenced by what team they were on. Also, being on a team with higher baseline steps and a smaller range in steps was associated with greater increases in individual team members’ step change. Results from the present study provide support that increases in physical activity may spread through social ties. Thus, future team-based public health campaigns may consider manipulating team composition to include individuals who already engage in positive health behaviors to take advantage of social influences, and thereby optimize program effectiveness.
Social comparison may be one mechanism by which social contacts influence health behavior. According to social comparison theory (Festinger, 1954), individuals determine their potential performance based on others’ performance. Studies have shown that social comparisons with “better” performing (healthier) role models increase motivation, enhance effective modeling, and improve health behaviors (Stanton et al., 1999). SURI team effects are consistent with these findings; being on a team with members who were relatively active at baseline enhanced individuals’ physical activity outcomes. Also consistent with social comparison theory are the findings that homogeneity in team baseline steps improves activity outcomes; being relatively similar to comparison targets on the domain of interest increases perceived attainability and the likelihood of adopting the targets’ behaviors. Taken together, these findings suggest that optimal teams would be those that strike a balance between providing upward comparison role models and being comprised of individuals with a relatively small range of physical activity ability at baseline.
While task related team variables (e.g., team baseline activity level) were associated with individual step change, team demographic characteristics (e.g. gender composition) were not. These results are consistent with previous findings that personal attributes (e.g., gender) are less associated with team performance than task-related attributes (e.g., physical ability) (Pelled, 1996). Future research should continue to examine the effects of task-related team variables on activity outcomes.
This study has some limitations. Consistent with previous pedometer interventions, only 16% of participants were males. Future team-based activity programs may consider increasing enrollment of males by using advertisements targeting men. Ethnicity and socioeconomic status were not assessed. Given that this intervention was internet based, it may have excluded individuals from disadvantaged backgrounds without internet access. However, recent data suggest that 60% of individuals with a household income of less than $30,000/year use the internet (Pew Research Group, 2010). Moreover, internet access is increasing at all income levels (Pew Research Group, 2010), suggesting that internet-based interventions may reach larger audiences in future years. Participants who did not complete the program were less active at baseline; future statewide interventions may consider providing additional motivational supports to less active enrollees. Physical activity changes were self-reported; however, self-reported activity data were based on pedometer readings, which are an objective measure of activity and are related to other physical activity measures (LeMasurier & Tudor-Locke, 2003; DeCocker et al., 2008). Although a conservative baseline carried forward approach was used in the intent-to-treat analyses, it may have underestimated the effects of SURI on step change. Finally, this study did not include a control group, limiting the ability to rule out alternative explanations for the observed effects. Strengths of SURI include the large sample and high completion rate. Furthermore, this is the only study that has examined the effects of team and team characteristics on individuals’ step change during a large physical activity campaign. Future studies should continue to examine team variables that influence targeted health behaviors in team-based public health interventions.
Conclusion
This study shows that statewide campaigns may increase physical activity by over 2000 steps/day and double the proportion of individuals who meet criteria for being physically active. Moreover, this paper is the first to suggest that team factors affect individual health outcomes in team-based public health interventions. Findings from this study highlight the importance of social influence in team-based interventions; by manipulating team and social factors in large-scale public health campaigns, it may be possible to enhance the effectiveness of team-based health interventions.
Acknowledgments
We thank the staff from The Miriam Hospital’s Weight Control and Diabetes Research Center and Shape Up Rhode Island who made this study possible.
Footnotes
Conflict of Interest Statement
The authors have the following disclosures: R.K. is founder and Chairman of Shape Up Rhode Island and R.K. and B.W. are managing partners of Shape Up the Nation. The other authors declare no conflict of interest.
In level 1, β0j represents step change for the jth participant when Level-1 predictor variables equal zero; β1j, β2j, and β3j represent the gender-, age-, baseline steps-step change slopes for participant j; ri is the random error associated with participant j’s step change. In level 2, β0j (individual step change) becomes the dependent variable; γ00 is the average step change across teams; γ01, γ02, γ03, γ04, γ05, and γ06 represent the main effect for each team variable on participants’ change in steps; μ0j represents the random error term.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Araiza P, Hewes H, Gashetewa C, Vella CA, Burge MR. Efficacy of a pedometer- based physical activity program on parameters of diabetes control in type 2 diabetes mellitus. Metabolism. 2006;55:1382–1387. doi: 10.1016/j.metabol.2006.06.009. [DOI] [PubMed] [Google Scholar]
- Bandura A. Social Learning Theory. New York: General Learning Press; 1977. [Google Scholar]
- Behrens TK, Domina L, Fletcher GM. Evaluation of an employer-sponsored pedometer-based physical activity program. Percept Mot Skills. 2007;105:968–976. doi: 10.2466/pms.105.3.968-976. [DOI] [PubMed] [Google Scholar]
- Blair SN, Kohl HW, Paffenbarger RS, Clark DG, Cooper KH, Gibbons LW. Physical fitness and all-cause mortality. JAMA. 1989;262:2395–2401. doi: 10.1001/jama.262.17.2395. [DOI] [PubMed] [Google Scholar]
- Bravata DM, Smith-Spangler C, Sundaram V, et al. Using pedometers to increase physical activity and improve health. JAMA. 2007;298:2296–2304. doi: 10.1001/jama.298.19.2296. [DOI] [PubMed] [Google Scholar]
- Brown WJ, Mummery K, Eakin E, Schofield G. 10,000 Steps Rockhampton: Evaluation of a whole community approach to improving population levels of physical activity. J Phys Act Health. 2006;3:1–14. [Google Scholar]
- Bryk AS, Raudenbush SW. Hierarchical linear models: Applications and data analysis methods. Sage Publications; Newberry Park: 1992. [Google Scholar]
- CDC. Prevalence of regular physical activity among adults—United States, 2001 and 2005. MMWR. 2007;56:1209–1212. [PubMed] [Google Scholar]
- Christakis NA, Fowler JH. The spread of obesity in a large social network over 32 years. N Engl J Med. 2007;357:370–379. doi: 10.1056/NEJMsa066082. [DOI] [PubMed] [Google Scholar]
- Christakis NA, Fowler JH. The collective dynamics of smoking in a large social network. N Engl J Med. 2008;358:2249–2258. doi: 10.1056/NEJMsa0706154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Cocker KA, De Bourdeaudhuij IM, Brown WJ, Cardon GM. Effects of “10,000 Steps Ghent”: A whole-community intervention. Am J Prev Med. 2007;33:455–463. doi: 10.1016/j.amepre.2007.07.037. [DOI] [PubMed] [Google Scholar]
- De Cocker KA, De Bourdeaudhuij IM, Cardon GM. What do pedometer counts represent? A comparison between pedometer data and data from four different questionnaires. Public Health Nutr. 2008;12:74–81. doi: 10.1017/S1368980008001973. [DOI] [PubMed] [Google Scholar]
- Dishman RK, DeJoy DM, Wilson MG, Vandenberg RJ. A randomized workplace trial to increase physical activity. Am J Prev Med. 2009;36:133–141. doi: 10.1016/j.amepre.2008.09.038. [DOI] [PubMed] [Google Scholar]
- Festinger L. A theory of social comparison processes. Hum Relat. 1954;7:117–140. [Google Scholar]
- Haines DJ, Davis L, Rancour P, Robinson M, Neel-Wilson T, Wagner S. A pilot intervention to promote walking and wellness and to improve the health of college faculty and staff. J Am Coll Health. 2007;55:219–225. doi: 10.3200/JACH.55.4.219-225. [DOI] [PubMed] [Google Scholar]
- Hox J. Multilevel Analysis: Techniques and Application. Mahwah, NJ: Lawrence Erlbaum; 2002. [Google Scholar]
- Le Masurier GC, Tudor-Locke C. Comparison of pedometer and accelerometer accuracy under controlled conditions. Med Sci Sports Exerc. 2003;35:867–871. doi: 10.1249/01.MSS.0000064996.63632.10. [DOI] [PubMed] [Google Scholar]
- Moreau KL, Degarmo R, Langley J, et al. Increasing daily walking lowers blood pressure in postmenopausal women. Med Sci Sports Exerc. 2001;33:1825–1831. doi: 10.1097/00005768-200111000-00005. [DOI] [PubMed] [Google Scholar]
- Pate RR, Pratt M, Blair SN, et al. Physical activity and public health: a recommendation from the Centers for Disease Control and Prevention and the American College of Sports Medicine. JAMA. 1995;273:402–407. doi: 10.1001/jama.273.5.402. [DOI] [PubMed] [Google Scholar]
- Pelled LH. Demographic diversity, conflict, and work group outcomes: An intervening process theory. Organ Sci. 1996;7:615–631. [Google Scholar]
- Pew Research Group. Internet, broadband, and cell phone statistics. 2010 Jan 5; http://www.pewinternet.org/~/media//files/reports/2010/PIP_December09_update.pdf.
- Pope S. Sportline 340 Step and Distance Pedometer®: Surprisingly accurate, excellent value. 2005 May 8; http://sportline-SP2795BK-340-Strider-Pedometer/dp/B0006VWRX6.
- Stanton AL, Danoff-Burg S, Cameron CL, Snider PR, Kirk SB. Social comparison and adjustment to breast cancer: An experimental examination of upward affiliation and downward evaluation. Health Psychol. 1999;18:151–158. doi: 10.1037/0278-6133.18.2.151. [DOI] [PubMed] [Google Scholar]
- Sugiura H, Sugiura H, Kajima K, Mirbod SM, Iwata H, Matsuoka T. Effects of long-term moderate exercise and increase in number of daily steps on serum lipids in women: Randomised controlled trial. BMC Womens Health. 2002:2–3. doi: 10.1186/1472-6874-2-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swartz AM, Strath SJ, Bassett DR, et al. Increasing daily walking improves glucose tolerance in overweight women. Prev Med. 2003;37:356–362. doi: 10.1016/s0091-7435(03)00144-0. [DOI] [PubMed] [Google Scholar]
- Tudor-Locke C, Hatano Y, Pangrazi RP, et al. Revisiting “How many steps are enough. Med Sci Sports Exerc. 2008;40:S537–43. doi: 10.1249/MSS.0b013e31817c7133. [DOI] [PubMed] [Google Scholar]
- USDHHS. 2008 physical activity guidelines for Americans. 2008 Available at http://www.health.gov/paguidelines.
- Wyatt HR, Peters JC, Reed GW, et al. Using electronic step counters to increase lifestyle physical activity: Colorado on the Move. J Phys Act Health. 2004;1:178–188. [Google Scholar]
- Wing RR, Pinto AM, Crane MM, Kumar R, Weinberg BM, Gorin AA. A statewide intervention reduces BMI in adults: Shape Up Rhode Island Results. Obesity. 2009;17:991–995. doi: 10.1038/oby.2008.655. [DOI] [PMC free article] [PubMed] [Google Scholar]