Abstract
Work-related stress among physicians has been an issue of growing concern in recent years. How and why this may vary between different health care systems remains poorly understood. Using an established theoretical model (effort-reward imbalance), this study analyses levels of work stress among primary care physicians (PCPs) in three different health care systems, the United States, the United Kingdom and Germany. Whether professional autonomy and specific features of the work environment are associated with work stress and account for possible country differences are examined.
Data are derived from self-administered questionnaires obtained from 640 randomly sampled physicians recruited for an international comparative study of medical decision making conducted from 2005–2007. Results demonstrate country-specific differences in work stress- with the highest level in Germany, intermediate level in the US and lowest level among UK physicians. A negative correlation between professional autonomy and work stress is observed in all three countries, but neither this association nor features of the work environment account for the observed country differences.
Whether there will be adequate numbers of PCPs, or even a field of primary care in the future, is of increasing concern in several countries. To the extent that work-related stress contributes to this, identification of its organizational correlates in different health care systems may offer opportunities for remedial interventions.
Keywords: primary care physicians, work stress, effort-reward imbalance, health care systems, professional autonomy, USA, UK, Germany
Background
Work-related stress among physicians has been an issue of growing concern in recent years (Bond & Bond, 2000). It appears most evident among primary care physicians, who care for the majority of illness in society. Recent organisational and legal changes are thought to impact physician autonomy (clinical guidelines and performance measures), while heavier workloads, and changing reimbursement methods (pay-for-performance and salaried positions) appear to contribute to the growing levels of job pressure reported by primary care providers (Calnan, Wainwright, Forsythe, Wall, & Almond, 2001; Firth-Conzens & Payne, 1999; Linzer, McMurray, Visser, Oort, Smets, & de Haes, 2002; Routh, Cooper, & Routh, 1996; Sundquist & Johansson, 2000; Uncu, Bayram, & Bilgel, 2007). Heavy workload is also widespread among more specialised physicians, including those working in hospitals, but is less often combined with threats to income security and job continuation (Collier, McCue, Markus, & Smith, 2002; Li, Yang, & Cho, 2006; Richter, Stoll, & Plaff, 2007; Spickard, Gabbe, & Christensen, 2002).
Despite this evidence, scientific knowledge on the determinants and consequences of physicians’ work stress remains limited for several reasons. First, with some notable exceptions (Calnan, Wainwright, & Almond, 2000; Li et al., 2006; Richter et al., 2007; Sundquist & Johansson, 2000), most studies are not based on a theoretical model that delineates stressful experience at a level of generalisation that allows for its identification in a wide range of complex and different work settings. Several such theoretical models have been developed, in particular the person-environment-fit model (French, Caplan, & Harrison, 1982), the demand-control model (Karasek & Theorell, 1990), and the effort-reward imbalance model (Siegrist, 1996). The latter two models are most often tested in epidemiological studies. The demand-control model (Karasek & Theorell, 1990) defines stressful work as the combination of two major task characteristics, high demands and low control or decision latitude. An additional assumption claims that social support at work moderates their adverse effects on health. According to the effort-reward imbalance model (Siegrist, 1996) stressful experience at work is elicited by continued non-reciprocal exchange in terms of high cost (high level of effort spent) and low gain (low reward received in turn). Rewards are defined by three transmitter systems: money, esteem/ recognition, and career opportunities including job security. The two models complement each other, the former deals with job characteristics while the latter deals with work contract-related aspects. They both are measured with standardised, psychometrically validated questionnaires that provide reliable data, permitting comparisons across study populations (Karasek, Brisson, Kawakami, Houtman, Bongers, & Amick, 1998; Siegrist, Starke, Chandola, Godin, Marmot, Niedhammer et al., 2004).
Second, there is a dearth of evidence from longitudinal observational investigations that predict prospective changes in physicians’ performance, well being and health on the basis of their initial exposure to work stress. Third, while a high level of work stress among primary care physicians is generally recognised, research so far largely failed to analyse the potential impact of different service systems within and between countries on physicians’ well-being and performance ((Linzer et al., 2002).
This study attempts to fill two of these gaps, first, by assessing physicians’ level of work stress by a theory-based measurement approach, and second, by comparing work stress among physicians in three different national health care systems, the United States (US), the United Kingdom (UK), and Germany. For the following reasons, the assessment of a stressful psychosocial work environment was based on the effort-reward imbalance model. First, the condition defined by this model was found to be frequent in person-based service occupations and professions (such as physicians and nurses) (Bakker, Killmer, Siegrist, & Schaufeli, 2000; Calnan et al., 2001). Second, at least three studies of work stress among physicians applied this model and documented consistent associations with reduced health and well being (Calnan et al., 2000; Li et al., 2006; Richter et al., 2007). Third, cumulative evidence on adverse effects of effort-reward imbalance on physical and mental health is available from prospective epidemiological investigations conducted in working populations from several countries, including two of the countries represented in this study (Siegrist & Wahrendorf, 2009; Tsutsumi & Kawakami, 2004).
To examine organizational variations in the level of work stress among physicians, as measured by this model, we compared primary care physicians in three different systems of health care provision: 1) a largely private insurance-based system (US), 2) a government-supported, tax based system (UK), and 3) a mixed system with corporatist and federalist features, administered by social security agencies (Germany). Additionally, we assessed the degree of physicians’ perceived professional autonomy as this latter variable is thought to be of crucial importance in mediating upstream features of health care provision with everyday work experience (Coburn & Willis, 2000; McKinlay & Marceau, 2002).
Methods
Study design
In-depth interviews and self-administered questionnaires, including the questions on work stress which are of special interest for this analysis, were administered during two balanced factorial experiments designed to simultaneously measure the unconfounded effects of (a) patient attributes (age, gender, race/ethnicity, and socio-economic status), (b) physician characteristics (gender and years of clinical experience), and (c) health care system (United States (US), the United Kingdom (UK), and Germany) on medical decision making with respect to common medical problems: type 2 diabetes and coronary heart disease (CHD) ( McKinlay, Link, Arber, Marceau, O’Donnell, Adams et al., 2006). These studies were conducted concurrently from September of 2005 to July of 2007. These experiments included equal numbers of physicians in groups classified by gender and experience, and of their decisions on filmed patients categorised by gender, age, race/ethnicity, and socio-economic status. The diabetes experiment consisted of two vignettes (undiagnosed diabetes and diagnosed diabetes with an emerging complication) and was run in three countries (US, UK, and Germany). The coronary heart disease study was conducted in the US, but utilised the same experimental design as the diabetes study. Thus, our interview and questionnaire data are from two studies (Diabetes and CHD) with similar study designs. The data are drawn from primary care physicians practicing in three different health care systems (Diabetes – US, UK, and Germany; CHD – US only). The study protocols for both studies were approved by the ethical committees of the respective study sites, and all participants gave signed informed consent.
Study populations
To be eligible for selection for both studies, physicians had to (a) have completed a medical residency program in either internal medicine or family practice (US), or general practice (UK, Germany), (b) provide primary care at least 50 per cent of their time, and (c) work within the designated geographical area. For the Diabetes study, the physicians were required to have a medical degree from a recognised academic institution in the country of sampling. However, this inclusion criteria did not apply to the CHD study conducted in the US, where international medical graduates were included. As a factorial experiment, equal numbers of male and female participants with either greater (> 15 years) or less (< 5 years) clinical experience were randomly sampled from membership databases in each country.
In the US, physician participants were selected from a listing of physicians practicing in New Jersey, New York, and Pennsylvania (Diabetes study; n = 192) (study 1) and in North and South Carolina (CHD study, n = 256) (study 2).
In the UK, the sample of general practitioners was drawn from the National Primary Care Research and Development Centre database which is accessed for authorised research. Participants were recruited from urban and rural areas practicing within 150 miles of Manchester city (n=128). The UK participants were required to respond to a letter before being contacted by an interviewer. Therefore, there were more opportunities for passive refusal than in the other two countries, and reasons for any non-response could not be ascertained. Yet, in terms of demographic characteristics (see Table 1) the UK doctors did not differ from the US or German doctors, except that they were slightly younger.
Table 1.
Socio-demographic characteristics of the study samples
| Diabetes Study | CHD Study | |||
|---|---|---|---|---|
| Germany N=64 |
UK n=128 |
US N=192 |
US N=256 |
|
| Physician Age | ||||
| Mean ± Standard Deviation |
49.9 ± 7.45 |
43.4 ± 8.73 |
46.7 ± 9.04 |
46.2 ± 10.32 |
| Physician Race | ||||
| Non-white | 0.0% (0/64) |
9.4% (12/127) |
20.0% (38/190) |
27.3% (68/249) |
| White | 100.0% (64/64) |
90.6% (115/127) |
80.0% (152/190) |
72.7% (181/249) |
| Medical School Training (CHD Study Only) | ||||
| US Trained | N/A | N/A | N/A | 84.0% (215/256) |
| Non-US Trained | N/A | N/A | N/A | 16.0% (41/256) |
Each study includes equal numbers of male/female physicians and less/more experienced physicians
In Germany, the sample (n=64) was drawn from a list of 5,732 family doctors and GP-internists available for sampling, provided by the North Rhine Physicians Board. This region represents more than 10 per cent of the German population.
The German and British samples were smaller in the Diabetes study because not all race/ethnic categories of patients could be included in the factorial design (Black, White, and Hispanic) in these countries.
Apart from these few exceptions, the sampling and data collection procedures were similar in each country, as consistent eligibility criteria and specific regional criteria were observed. Data collection occurred in the doctor’s office during a usual practice day (not at a professional meeting, a course update, or in their home) to enhance external validity.
Demographic characteristics of the 640 participating primary care physicians from the two studies in three countries are summarized in Table 1. We do not claim that the samples are representative of doctors in the three countries.
Measures
Physicians’ work stress was measured by a standardised self-administered questionnaire with 9 Likert-scaled items. These items represent short versions of the two scales stress due to ‘effort’ (4 out of 6 items) and stress due to ‘rewards’, or lack thereof (5 out of 11 items) of the original effort-reward imbalance questionnaire (Siegrist et al. 2004). The items are listed in Table 2 with raw means by study for each individual item. Participants were asked to indicate whether or not the item content corresponds to their own typical experience. If this was the case, they reported the extent to which they usually felt distressed by this experience (5-point scale ranging from ‘no’, ‘yes, and I am not distressed’ to ‘yes, and I feel very distressed’). A high score on the scale ‘effort’ (item range 1–5) indicates a high amount of effort spent at work whereas a high score on the scale ‘reward’ (item range 1–5) reflects lack of appropriate rewards received in turn. This short version was tested previously in different samples and proved to be a reliable and economic indicator of the original measure. A third scale of the original questionnaire measuring the intrinsic component ‘over-commitment’ was not included in the current study protocol. Factor analysis and tests of internal consistency were performed to evaluate the psychometric properties of the measure. Internal consistency of the scales was satisfactory, with Cronbach’s alpha varying from 0.86 to 0.63. In all samples the two-factor structure of the items measuring ‘effort’ and ‘reward’ respectively was replicated, thus providing three work stress measures: (1) a score measuring ‘high effort’, (2) a score measuring ‘low reward’, and (3) an overall work stress score combining the two scales (all nine items) that aims at reflecting the extent to which the theoretical notion of high effort in combination with low reward is experienced by the responding physicians. Moderate to strong correlations between the ‘effort’ and ‘reward’ scales were observed, ranging from 0.26 to 0.60.
Table 2.
Individual Questions on the Work Stress Scale 1 (mean ± standard deviation)
| Diabetes Study | CHD Study | |||
|---|---|---|---|---|
| Germany N=64 |
UK n=128 |
US N=192 |
US Only N=256 |
|
| Effort | ||||
| I have constant time pressure due to a heavy work load |
3.5 ± 0.86 | 2.9 ± 0.76 | 3.1 ± 1.03 | 2.9 ± 1.01 |
| I have a lot of responsibility in my job |
3.0 ± 0.68 | 2.6 ± 0.62 | 3.0 ± 0.89 | 2.9 ± 0.83 |
| I have many interruptions and disturbances in my job |
2.8 ± 1.21 | 2.7 ± 0.89 | 3.0 ± 0.92 | 2.8 ± 1.00 |
| Over the past few years, my job has become more and more demanding |
3.2 ± 1.16 | 2.9 ± 0.87 | 3.2 ± 1.06 | 2.9 ± 1.16 |
| Reward | ||||
| The prospects of my further job development are poor |
1.9 ± 1.12 | 1.4 ± 0.81 | 2.0 ± 1.28 | 1.8 ± 1.17 |
| I have experienced or I expect to experience an undesirable change in my work situation |
3.5 ± 1.34 | 2.3 ± 1.21 | 2.2 ± 1.34 | 1.9 ± 1.28 |
| My job security is poor | 1.6 ± 1.29 | 1.1 ± 0.49 | 1.5 ± 1.02 | 1.3 ± 0.80 |
| Considering all my efforts and achievements, I receive the respect and prestige I deserve for my work2 |
2.5 ± 1.29 | 1.5 ± 0.81 | 2.0 ± 1.13 | 1.8 ± 1.10 |
| Considering all my efforts and achievements, my income is adequate2 |
3.1 ± 1.30 | 1.3 ± 0.63 | 2.8 ± 1.37 | 2.3 ± 1.27 |
Possible responses: 1= Disagree, 2= Agree, and I am not at all distressed, 3= Agree, and I am somewhat distressed, 4= Agree, and I am distressed, 5= Agree, and I am very distressed
Possible responses: 1= Agree, 2= Disagree, and I am not at all distressed, 3= Disagree, and I am somewhat distressed, 4= Disagree, and I am distressed, 5= Disagree, and I am very distressed
Physicians’ lack of professional autonomy was additionally assessed within the self-administered questionnaire containing 12 items that measure two crucial aspects of professional autonomy, clinical autonomy (7 items), and administrative autonomy (5 items) (Konrad, Williams, Linzer, McMurray, Pathman, Gerrity et al., 1999). Administrative autonomy focuses primarily on issues related to office management and provision of services while clinical autonomy deals primarily with diagnosis and management decisions related to patient care. The content of the 4-point Likert scaled items is given in Table 3 with raw means by study for each individual item. Higher scores indicate a greater lack of autonomy. Internal consistencies, as measured by Cronbach’s alpha varied from 0.81 to 0.54 (lower consistencies for clinical autonomy). A two factor construct worked well for the US samples, but varied in the UK and Germany (and was not consistent between countries).
Table 3.
Individual Questions on the Lack of Autonomy Scale 2 (mean ± standard deviation)
| Diabetes Study | CHD Study | |||
|---|---|---|---|---|
| How much of the time would you say you have control over: |
Germany N=64 |
UK n=128 |
US N=192 |
US Only N=256 |
|
Lack of Clinical Autonomy |
||||
| Deciding when to admit patients to the hospital |
1.7 ± 0.54 | 1.8 ± 0.50 | 1.9 ± 0.81 | 1.7 ± 0.86 |
| Determining the length of a patient's stay in the hospital |
3.4 ± 0.69 | 3.9 ± 0.26 | 2.7 ± 0.93 | 2.8 ± 1.09 |
| Getting approval for services you feel are necessary |
2.3 ± 0.63 | 2.9 ± 0.63 | 2.4 ± 0.56 | 2.3 ± 0.63 |
| Making referrals to a specialist whenever necessary |
1.4 ± 0.58 | 1.8 ± 0.63 | 1.8 ± 0.65 | 1.7 ± 0.64 |
| Prescribing patients with medications of your choice |
1.6 ± 0.56 | 1.8 ± 0.56 | 2.5 ± 0.53 | 2.3 ± 0.62 |
| Selecting which physicians you refer patients to |
1.9 ± 0.69 | 2.4 ± 0.73 | 2.2 ± 0.65 | 1.9 ± 0.66 |
| What diagnostic tests you can order |
1.4 ± 0.50 | 1.9 ± 0.50 | 2.1 ± 0.52 | 1.9 ± 0.57 |
|
Lack of Administrative Autonomy |
||||
| Spending sufficient time with your patients |
2.1 ± 0.54 | 2.5 ± 0.58 | 2.4 ± 0.73 | 2.3 ± 0.67 |
| The administrative details of your office or clinic schedule |
2.1 ± 0.70 | 2.4 ± 0.76 | 2.5 ± 0.83 | 2.5 ± 0.83 |
| The hours you are required to be in your office |
2.1 ± 0.83 | 2.4 ± 0.71 | 2.3 ± 0.87 | 2.2 ± 0.90 |
| The volume of paperwork you are required to do |
2.8 ± 1.00 | 3.3 ± 0.73 | 3.3 ± 0.76 | 3.2 ± 0.80 |
| The volume/size of your patient load/list |
2.7 ± 0.91 | 2.7 ± 0.88 | 2.3 ± 0.82 | 2.4 ± 0.86 |
Possible responses: 1= Always, 2= Usually, 3= Sometimes, 4=Never
Additional information on the following features of physicians’ working conditions was collected from the self-administered questionnaire: (1) estimated time needed and time allocated for different types of patient appointments; (2) availability of resources and tools, such as audit, feedback, or tracking records; web based chat room or bulletin boards; collaboration with a specialty trained nurse/educator/social worker who actively follows up with patients; availability of electronic reminders in medical records; availability of portable devices, electronic communication or education programs; (3) number of support staff by practice, (4) solo practice versus group practice (including practice size), and (5) use of clinical guidelines. This information was used to analyse the impact of physicians’ working conditions on their level of work stress.
Statistical analysis
Analysis of variance (ANOVA) was used to test the main effects of country/study on work stress, autonomy and several features of work condition. Tukey-Kramer tests were used when multiple comparisons were made (Kramer, 1956). Exact p-values were not reported when multiple comparison were made. Instead, 95% confidence intervals for all pair-wise differences between country/study are provided.
In addition to the main effects of country, interaction effects with the design variables physician gender and experience were examined. The model included as explanatory variables: country/study, physician gender, physician experience, the interaction of each design variable and country/study, and the three way interaction between country/study, physician gender and experience. All analyses were performed using the SAS System Version 9.1.3 (Cary, NC, US).
Results
Differences of work stress between health care systems
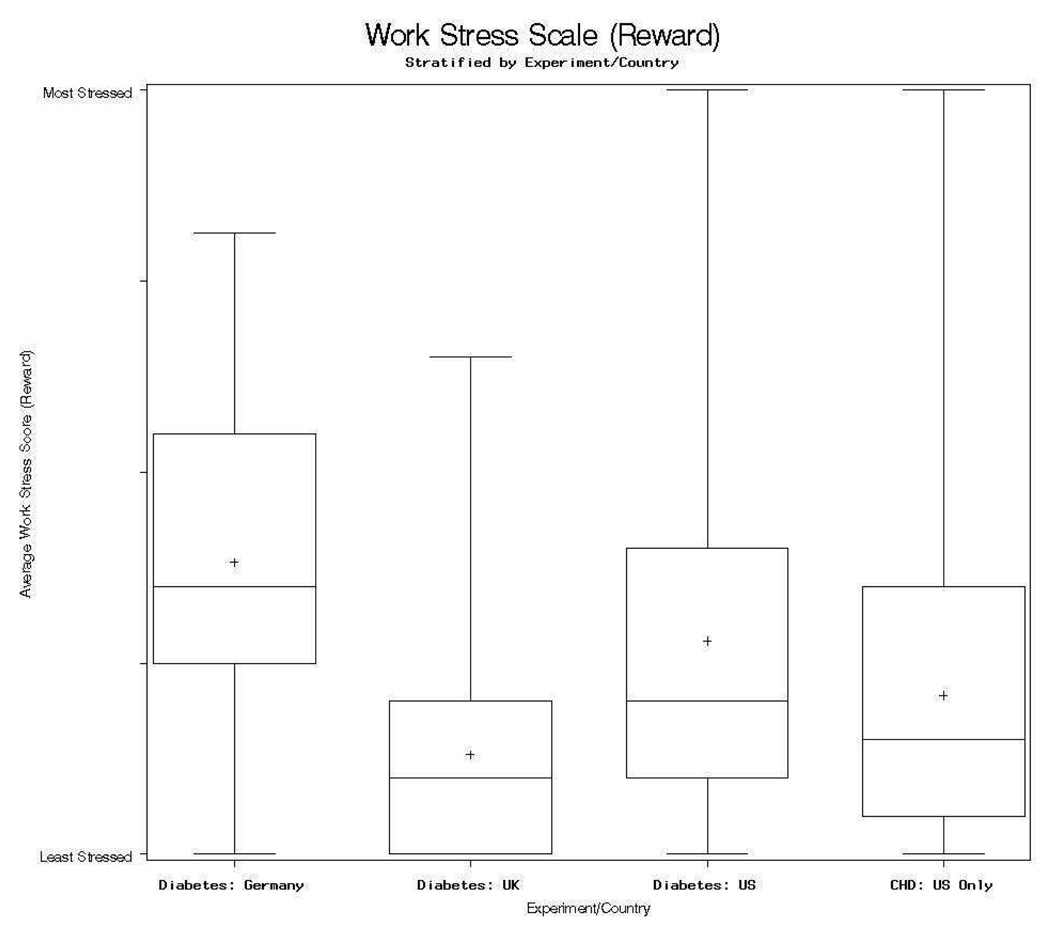
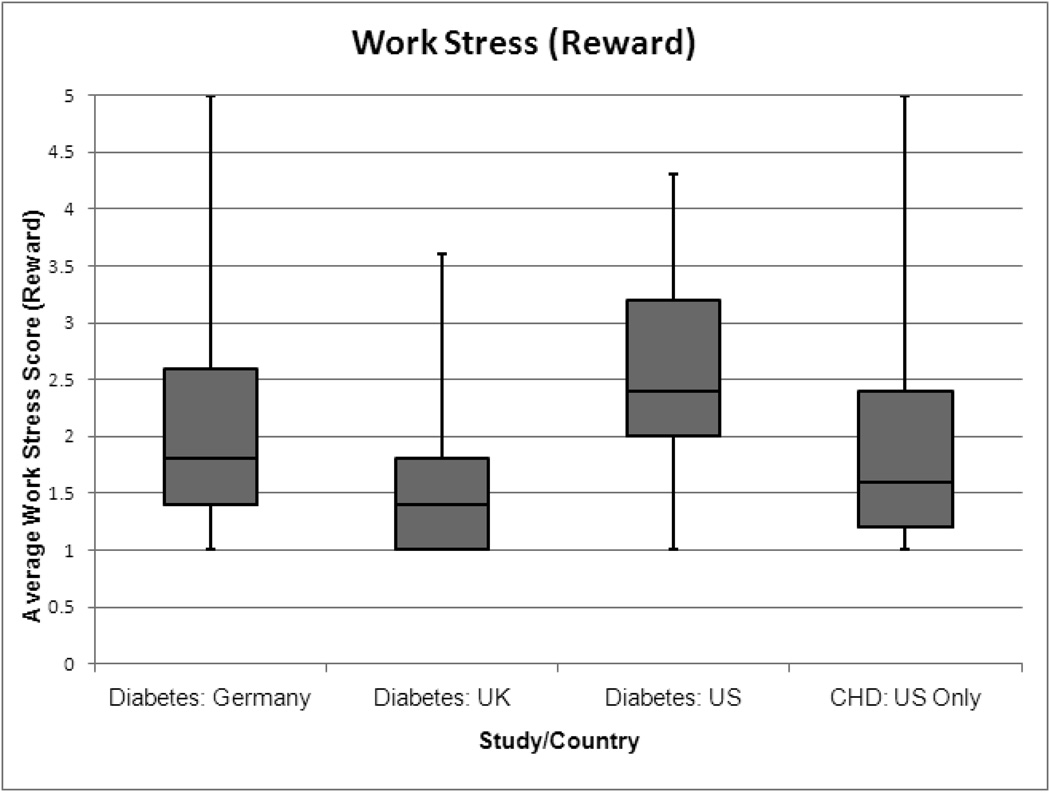
Table 5 (upper part) demonstrates significant differences in the mean level of work stress (overall scale) between the physicians in the three health care systems, with highest level in German physicians, intermediate level in US physicians (two studies), and lowest level in UK physicians. Pair-wise comparisons by country and study (Table 4) reveal a striking consistency of these differences. Further exploration based on the two subscales of work stress, effort and reward, indicates that significant differences across the reward subscale largely account for the observed study /country differences. The pattern is illustrated by box plots of average work stress (reward subscale) by country/study given in Figure 1. While no large variations exist in the effort related work stress among physicians of the three health care systems, there are clear, statistically significant variations with regard to reward related work stress (money, esteem, promotion prospects and security).
Table 5.
Differences in work stress (mean and standard deviation) (upper part) and in lack of autonomy (lower part) by experiment/country*
| Diabetes Study | CHD Study | ||||
|---|---|---|---|---|---|
| Work Stress | Germany | UK | US | US Only | p-value* |
| Mean (Overall Scale) ± Standard Deviation |
2.82 ± 0.63 |
2.08 ± 0.46 |
2.53 ± 0.77 |
2.30 ± 0.74 |
< 0.01 |
|
Autonomy | |||||
| Administrative (Mean ± Standard Deviation) |
2.35 ± 0.57 |
2.66 ± 0.50 |
2.54 ± 0.61 |
2.54 ± 0.61 |
< 0.01 |
| Clinical (Mean ± Standard Deviation) |
1.96 ± 0.32 |
2.36 ± 0.29 |
2.22 ± 0.38 |
2.10 ± 0.41 |
< 0.01 |
P-value from F-test (ANOVA) for experiment/country differences
Table 4.
Pair-wise comparisons in Work Stress (Overall) by Experiment/Country
| Difference between means (95% Confidence interval)* |
Diabetes Study | CHD Study | ||
|---|---|---|---|---|
| Germany | UK | US | US Only | |
| Diabetes - Germany |
- | −0.73 (−1.01, −0.45)** |
−0.25 (−0.51, 0.01) |
−0.51 (−0.76, −0.26)** |
| Diabetes - UK | 0.73 (0.45, 1.01)** |
- | 0.48 (0.28, 0.69)** |
0.22 (0.02, 0.41)** |
| Diabetes - US | 0.25 (−0.01, 0.51) |
−0.48 (−0.69, −0.28)** |
- | −0.26 (−0.44, −0.09)** |
| CHD - US Only | 0.51 (0.26, 0.76)** |
−0.22 (−0.41, −0.02)** |
0.26 (0.09, 0.44)** |
- |
Adjusted for multiple comparisons using Tukey-Kramer test
Significant after adjustment for multiple comparisons
Figure 1.
Boxplot of work stress (reward subscale) by study/country
The box-plot graphically depicts work stress by country/study through five-number summaries: 1) the sample minimum is represented by the lowest whisker, 2) the lower quartile (Q1) is represented by the lowest line of the box, 3) the median (Q2) is the middle box line, 3) the upper quartile (Q3) is represented by the highest line of the box, and the sample maximum is represented by the highest whisker. Finally the + represents the sample mean.
To control for possible confounding effects of physicians' gender and level of clinical experience on the observed associations, we conducted additional ANOVAs including physician gender and level of experience. Neither main effects nor interaction effects were observed that could reduce the documented health system/country effect (results not shown).
We considered the argument that variations in critical features of work environment across the health care systems could account for the associations between country/health care system and work stress. To rule out this argument, the following additional analyses were conducted (results not shown). First, mean work stress levels were compared between solo practitioners and group practitioners in each study. Stress levels were not significantly different with the exception of Germany where solo practitioners demonstrated higher stress due to lack of reward compared with group practitioners. Second, the same analysis was conducted with respect to number of support staff. Again, correlations between the support staff / physician ratio were low in all countries, indicating that this feature does not contribute to the differences of work stress across health care systems.
Third, the ratio of the time needed versus time allocated for different types of patient visits was calculated per sample. While differences of mean ratios between health care systems do exist (with the United States being allocated the most time as well as needing the most time) these differences do not explain variations in work stress between the systems (Konrad, Link, Shackelton, Marceau, von dem Knesebeck, Siegrist et al., 2010). Fourth, the same type of analysis was performed with respect to different resources available to physicians (i.e. audits, feedback, web tools, specially trained nurses or educators, electronic reminders, etc.). Again, there were no significant p-values for either the main effects or the interaction effects (results not shown).
It appears thus that physicians’ work stress, and specifically work-related reward, differs between the three health care systems, and that these differences are neither confounded by physician characteristics (gender, level of experience) nor by the features of the work environment under study. Therefore, in a final step, we analysed the association of work stress with lack of professional autonomy, and we tested whether differences in work stress might be partially related to differences in professional autonomy across the three health care systems.
Associations between work stress and lack of professional autonomy
To what extent do the two dimensions of lack of professional autonomy vary across the different health care systems? For administrative autonomy, differences were observed across health care systems with a greater lack of autonomy in the UK, compared to the US and Germany (Table 5, lower part; p < 0.01). However, pair-wise comparisons using the Tukey-Kramer test revealed that the only significant pair-wise difference was between the UK and Germany. For clinical autonomy, differences were more pronounced (Table 5, p < 0.01). Again, the greatest lack of autonomy was observed in UK physicians, with intermediate levels in the two US samples and the highest level was observed in Germany. All pair-wise comparisons were found to be statistically significant when adjusted for multiple comparisons. No effects of gender and clinical experience on these variations were observed.
Associations between lack of professional autonomy and work stress are shown in Table 6. Highly significant correlations of lack of administrative autonomy with work stress are observed in the US (p < 0.01) and the UK health care system, and a weaker association (p = 0.07) is observed for the German system. The same pattern is obvious for lack of clinical autonomy, although correlation coefficients are slightly smaller. If the two work stress subscales are analysed separately findings are consistent with those obtained from the overall scale. Interestingly, low reward at work is significantly associated with a greater lack of clinical autonomy in all three health care systems.
Table 6.
Correlations (p-values) of Work Stress with Lack of Administrative Autonomy (upper part) and Lack of Clinical Autonomy (lower part)
| Administrative Autonomy |
Overall work stress | Effort | Reward |
|---|---|---|---|
| Diabetes – Germany | 0.26 (0.07) | 0.11 (0.43) | 0.27 (0.06) |
| Diabetes – UK | 0.42 (<0.01) | 0.38 (<0.01) | 0.32 (<0.01) |
| Diabetes – US | 0.42 (<0.01) | 0.42 (<0.01) | 0.34 (<0.01) |
| CHD – US Only | 0.47 (<0.01) | 0.48 (<0.01) | 0.37 (<0.01) |
| Clinical Autonomy | Overall work stress | Effort | Reward |
| Diabetes – Germany | 0.26 (0.06) | 0.11 (0.43) | 0.27 (0.05) |
| Diabetes – UK | 0.35 (<0.01) | 0.27 (<0.01) | 0.31 (<0.01) |
| Diabetes – US | 0.25 (<0.01) | 0.20 (<0.01) | 0.25 (<0.01) |
| CHD – US Only | 0.22 (<0.01) | 0.23 (<0.01) | 0.18 (<0.01) |
Despite these associations of professional autonomy with work stress it is unlikely that the former condition mediates the association of work stress with type of health care system. Although within samples, less autonomy is associated with greater stress, we find that across samples, the opposite is true. For example, German physicians report the greatest autonomy and the highest level of work stress while UK physicians report the least autonomy and the lowest level of work stress.
Discussion
Firstly, employing data obtained from 640 randomly sampled primary care physicians working in three different health care systems, the United States, the United Kingdom, and Germany, we observed significant differences in mean level of psychosocial stress at work, measured by the effort-reward imbalance model. The highest level of work stress was reported by physicians in Germany and the lowest level by physicians in the UK, with US physicians reporting intermediate levels. The robustness of this finding is reinforced by the consistent results from the replication in the US CHD study. Differences were largely due to the reward component of the model. This finding was not modified when the impact of physician characteristics (gender, level of clinical experience) and of features of physicians’ work environment were examined (solo versus group practice; staff/physician ratio; time constraints regarding patient appointments; resources available to physicians). Secondly, we found a consistent (though not always significant) association of work stress with lack of professional autonomy. Lower levels of administrative and clinical autonomy were associated with higher work stress in all countries, most markedly in the US and the UK system.
We now turn to possible explanations for the observed differences in work stress, and specifically in work-related rewards, between the samples of physicians in the three health care systems? A methodological interpretation points to cultural or semantic differences in evaluating these aspects of subjectively perceived stressful work. For instance, physicians in the UK may be less inclined than their US and German colleges to express negative feelings about work. While we cannot rule out this argument it should be observed UK physicians score highest in expressing their negative feelings about limited professional autonomy. It is unlikely that they apply different evaluative standards to their judgments about the two topics.
Another interpretation emphasises the health policy context of physicians’ professional status at the time of data collection. Contrasting with the situation in the United States, practicing physicians in Germany were recently exposed to substantial changes in the organisation and remuneration of their work (Stock, Redaelli, & Lauterbach, 2007; Wörz & Busse, 2005). The implementation of disease management programs designed to promote quality of care and to foster competition were perceived as threats by many physicians, after an extended period of high professional independence and satisfying revenues. In line with this interpretation, we observe the clearest difference between Germany and the other countries under study on the scale measuring work-related rewards, in particular undesirable changes in one’s work situation and imbalance between efforts or achievements and income (Table 2). In the UK, primary care physicians received a 25 percent pay increase and stopped doing out-of-hours work when our study was conducted. This organizational change may have had a favourable impact on their evaluation of job-related rewards (Whalley, Gravelle, & Sibbald, 2008). While these post facto interpretations seem plausible a more detailed examination of organisational features within each health care system was unfortunately not within the scope of our study.
Scoring high on effort-reward imbalance at work was shown to be associated with elevated risks of stress-related physical and mental disorders and with poor functioning in a variety of occupational groups in prospective epidemiological studies (Kuper, Singh-Manoux, Siegrist, & Marmot, 2002; Siegrist, 2005; Stansfeld, Bosma, Hemingway, & Marmot, 1998). While prospective epidemiologic evidence of the effects of work stress among physicians is not available currently, at least three cross-sectional studies document significant associations of effort-reward imbalance at work with physicians’ reduced self-reported health and level of functioning and have shown that differences in the quartiles of effort-reward imbalance scores are meaningful in explaining elevated risks of subjective and objective health (Calnan et al., 2000; Li et al., 2006; Richter et al., 2007; Salavecz, Chandola, Pikhart, Dragano, Siegrist, Jöckel et al., 2010).
Thus, the measure used in this study was shown to have external validity. Moreover, results are in line with descriptive findings on adverse effects of high work stress on physicians’ health and well being that were not based on a specific theoretical model (Firth-Conzens & Payne, 1999; Linzer et al., 2002; Routh et al., 1996; Spickard et al., 2002; Uncu et al., 2007). The fact that physicians in the UK exhibit lower work stress (especially in terms of reward) than their US colleagues may reflect less concern about job security and income in a nationalized health care system (Gillies, Chenok, Shortell, Pawlson, & Wimbush, 2006).
Our study has several strengths and limitations. To our knowledge, this is the first report comparing a theoretically defined stressful psychosocial work environment of practicing physicians in different types of health care systems. Although reduced professional autonomy is associated with elevated work stress, this former condition does not account for the observed differences between health care systems. The same holds true for selected physician characteristics and features of the work setting. Second, we undertook this research in samples of randomly selected participants, and we combined data from two studies based on a largely identical study design (UK, Germany, and US). A second study within the US health care system tests the robustness of the results. Third, using analysis of variance, we tested main effects and two way and three way interactions with design variables to rule out confounding influences.
Despite these strengths several limitations are obvious. First, given a limited overall sample size (n = 640) and different size of the country sub-samples, results should not be generalized to all primary care physicians within each health care system. Yet, within the selection criteria stated, sample bias seems limited. An analysis of non-response within one country revealed that younger, female and urban physicians were somewhat more likely to participate in the study than the remaining groups and as mentioned earlier, UK participants may have had more opportunity for self-selection. (Bönte, 2008). Second, the study design only provides cross-sectional data, precluding any statements concerning the temporal sequence of associations. Reporting bias may account for associations of perceived work stress with reported professional autonomy. Moreover, cross-cultural comparability of the meaning of operational measures of work stress has not been sufficiently explored with item response theory (Raczek, Ware, Bjorner, Gandek, Haley, Aaronson et al., 1998). Third, as mentioned, our study did not identify in more detail those traits of the health care systems under study that may affect most directly physicians’ level of work stress and their restriction of clinical and administrative autonomy. Thus, the interpretation of respective findings was not embedded in theoretical reasoning about health system determinants of physicians’ work stress. Finally, we were not able to link variations of work stress with physicians’ level of performance, a critically important link in terms of policy implications of our findings (Firth-Conzens & Greenhalgh, 1997; Landon, Zaslavsky, Bernard, Cioffi, & Cleary, 2004).
In conclusion, this study revealed that physicians’ level of psychosocial stress at work varies considerably between the US, the UK and the German health care systems. As indicated by the theoretical model employed in this investigation, effort-reward imbalance, a substantial part of this variation appears due to work-related rewards in terms of money, career opportunities and esteem/recognition. Balancing efforts and rewards in physicians’ work may help to reduce the burden of their work-related stress. Whether there will be a sufficient number of primary care physicians in the future, or even a future for the field of primary care, is a source of concern in many countries (McKinlay & Marceau, 2009). To the extent that work-related stress contributes to this, reliable identification of its organizational origins across different health care systems may provide opportunities for future remedial interventions.
Acknowledgments
This project is supported by Grant No. AG 16747 from the National Institute on Aging, National Institutes of Health, United States of America. We also thank Markus Bonte, Martin Roland, and Stephen Campbell for their input.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The authors declare that they have no competing interests.
Contributor Information
Rebecca Shackelton, New England Research Institutes, Inc, Watertown, MA UNITED STATES, rshackelton@neriscience.com.
Johannes Siegrist, Department of Medical Sociology, University of Duesseldorf, Germany.
Carol Link, New England Research Institutes, Inc..
Lisa Marceau, New England Research Institutes, Inc..
References
- Bakker A, Killmer CH, Siegrist J, Schaufeli WB. Effort-reward imablance and burnout among nurses. Journal of Advanced Nursing. 2000;31:884–891. doi: 10.1046/j.1365-2648.2000.01361.x. [DOI] [PubMed] [Google Scholar]
- Bond D, Bond J. Work-related stress: can it be a thing of the past. The Lancet. 2000;355:124. doi: 10.1016/S0140-6736(05)72040-7. [DOI] [PubMed] [Google Scholar]
- Bönte M. Social determinants of physicians' performance (German) Berlin: Lit; 2008. [Google Scholar]
- Calnan M, Wainwright D, Almond S. Job strain, effort-reward imbalance and mental distress: a study of occupations in general medical practice. Work & Stress. 2000;14:297–311. [Google Scholar]
- Calnan M, Wainwright D, Forsythe M, Wall B, Almond S. Mental health and stress in the workplace: the case of general practice in the UK. Social Science and Medicine. 2001;52:499–507. doi: 10.1016/s0277-9536(00)00155-6. [DOI] [PubMed] [Google Scholar]
- Coburn D, Willis E. The medical profession: knowledge, power and autonomy. In: Albrecht G, Fitzpatrick S, S. S, editors. The handbook of social studies in health and medicine. London: Sage; 2000. pp. 377–393. [Google Scholar]
- Collier VU, McCue JD, Markus A, Smith L. Stress in emdical residency:: Status quo after a decade of reform. Annals of Internal Medicine. 2002;136 doi: 10.7326/0003-4819-136-5-200203050-00011. 384-367. [DOI] [PubMed] [Google Scholar]
- Firth-Conzens J, Greenhalgh J. Doctors' percentions of the links between stress and lowered clinical care. Social Science and Medicine. 1997;44:1017–1022. doi: 10.1016/s0277-9536(96)00227-4. [DOI] [PubMed] [Google Scholar]
- Firth-Conzens J, Payne R. Stress in health professionals. Chichester: Wiley; 1999. [Google Scholar]
- French J, Caplan R, Harrison RV. The mechanisms of job stress and strain. New York: Wiley; 1982. [Google Scholar]
- Gillies RR, Chenok KE, Shortell SM, Pawlson G, Wimbush JJ. The impact of health plan delivery system organisation on clinical quality and patient satisfaction. Health Services Research. 2006;41:1189–1199. doi: 10.1111/j.1475-6773.2006.00529.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karasek R, Brisson C, Kawakami N, Houtman I, Bongers P, Amick B. The job content questionnaire (JCQ): An instrument for internationally comparative assessments of psychosocial job characteristcs. Journal of Occupational Health Psychology. 1998;3:322–355. doi: 10.1037//1076-8998.3.4.322. [DOI] [PubMed] [Google Scholar]
- Karasek R, Theorell T. Health work. New York: Basic Books; 1990. [Google Scholar]
- Konrad T, Williams E, Linzer M, McMurray J, Pathman D, Gerrity M, et al. Measuring physician job satisfaction in a changing workplace and a challenging environment. Medical Care. 1999;37(11):1174–1182. doi: 10.1097/00005650-199911000-00010. [DOI] [PubMed] [Google Scholar]
- Konrad TR, Link CL, Shackelton RJ, Marceau LD, von dem Knesebeck O, Siegrist J, et al. It's about time: Physicians' perceptions of time constraints in primary care medical practice in three national healthcare systems. Medical Care(Jan 6) 2010 doi: 10.1097/MLR.0b013e3181c12e6a. EPub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kramer CY. Extension of multiple range tests to group means with unequal numbers of replications. Biometrics. 1956;12:307–310. [Google Scholar]
- Kuper H, Singh-Manoux A, Siegrist J, Marmot M. When reciprocity fails: effort-reward imbalance in relation to coronary heart disease and health functioning within the Whitehal II study. Occupational and Environmental Medicine. 2002;59:777–784. doi: 10.1136/oem.59.11.777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landon BE, Zaslavsky AM, Bernard SL, Cioffi MJ, Cleary PD. Comparison of performance of traditional Medicare vs. Medicare managed care. Journal of the American Medical Association. 2004;291:1744–1752. doi: 10.1001/jama.291.14.1744. [DOI] [PubMed] [Google Scholar]
- Li J, Yang W, Cho S. Gender differences in job strain, effort-reward imbalance, and health functioning among Chinese physicians. Social Science and Medicine. 2006;62(5):1066–1077. doi: 10.1016/j.socscimed.2005.07.011. [DOI] [PubMed] [Google Scholar]
- Linzer M, McMurray JE, Visser MR, Oort FJ, Smets E, de Haes HC. Sex differences in physician burnout in the United States and Netherlands. Journal of the American Medical Womens' Association. 2002;57:191–193. [PubMed] [Google Scholar]
- McKinlay J, Link C, Arber S, Marceau L, O’Donnell A, Adams A, et al. How do Doctors in Different Countries Manage the Same Patient? Results of a Factorial Experiment. Health Services Research. 2006;41(6):2182–2200. doi: 10.1111/j.1475-6773.2006.00595.x. [Erratum in 2141(2186):2303]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKinlay J, Marceau LD. The end of the golden age of doctoring. International Journal of Health Services. 2002;32(2):379–416. doi: 10.2190/JL1D-21BG-PK2N-J0KD. [DOI] [PubMed] [Google Scholar]
- Raczek AE, Ware JE, Bjorner JB, Gandek B, Haley SM, Aaronson NK, et al. Comparison of Rasch and summated rating scales constructed from SF-36 physical functioning items in seven countries: results from the IQOLA Project. International Quality of Life Assessment. Journal of Clinical Epidemiology. 1998;51:1203–1214. doi: 10.1016/s0895-4356(98)00112-7. [DOI] [PubMed] [Google Scholar]
- Richter P, Stoll A, Plaff H. Job demand-control, effort-reward models and burnout in hospitals. In: Richter P, Peiro JM, Schaufeli WB, editors. Psychosocial resources in health care systems. München: Hampp; 2007. pp. 111–124. [Google Scholar]
- Routh U, Cooper CL, Routh J. Job stress among British general practitioners: predictors of job dissatisfaction and mental ill-health. Stress Medicine. 1996;12:155–166. [Google Scholar]
- Salavecz G, Chandola T, Pikhart H, Dragano N, Siegrist J, Jöckel KH, et al. Work stress and health in Western European and post-communist countries: an East-West comparison study. Journal of Epidemiology and Community Health. 2010;64(1):57–62. doi: 10.1136/jech.2008.075978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siegrist J. Adverse effects of high effort/low reward conditions. Journal of Occupational Health Psychology. 1996;1:27–41. doi: 10.1037//1076-8998.1.1.27. [DOI] [PubMed] [Google Scholar]
- Siegrist J. Social reciprocity and health: new scientific evidence and policy implications. Psychoneuroendocrinology. 2005;30:1033–1038. doi: 10.1016/j.psyneuen.2005.03.017. [DOI] [PubMed] [Google Scholar]
- Siegrist J, Starke D, Chandola D, Godin I, Marmot M, Niedhammer I, et al. The measurement of effort-reward imbalance at work: European comparisons. Social Science and Medicine. 2004;58:1483–1499. doi: 10.1016/S0277-9536(03)00351-4. [DOI] [PubMed] [Google Scholar]
- Siegrist J, Wahrendorf M. Quality of work, health and retirement. Lancet. 2009;374:1872–1873. doi: 10.1016/S0140-6736(09)61666-4. [DOI] [PubMed] [Google Scholar]
- Spickard A, Gabbe SG, Christensen JF. Mid-career burnout in generalist and specialist physicians. Journal of the American Medical Association. 2002;288:1447–1450. doi: 10.1001/jama.288.12.1447. [DOI] [PubMed] [Google Scholar]
- Stansfeld SA, Bosma H, Hemingway H, Marmot M. Psychosocial work characteristics and socials upport as predictors of SF-36 functioning: the Whitehall II study. Psychosomatic Medicine. 1998;60:247–255. doi: 10.1097/00006842-199805000-00004. [DOI] [PubMed] [Google Scholar]
- Stock SAK, Redaelli M, Lauterbach KW. Disease management and health care reform in Germany - does more competition lead to less solidarity? Health Policy. 2007;80:86–96. doi: 10.1016/j.healthpol.2006.02.005. [DOI] [PubMed] [Google Scholar]
- Sundquist J, Johansson SE. High demand, low control, and impaired general health: Working conditions in a sample of Swedish general practitioners. Scandinavian Journal of Public Health. 2000;28:123–131. doi: 10.1177/140349480002800208. [DOI] [PubMed] [Google Scholar]
- Tsutsumi A, Kawakami N. A review of empirical studies on the model of effort-reward imbalance at work: reducing occupational stress by implementing a new theory. Social Science and Medicine. 2004;59:2235–2259. doi: 10.1016/j.socscimed.2004.03.030. [DOI] [PubMed] [Google Scholar]
- Uncu Y, Bayram N, Bilgel N. Job related affective well-being among primary health care physicians. European Journal of Public Health. 2007;17:514–519. doi: 10.1093/eurpub/ckl264. [DOI] [PubMed] [Google Scholar]
- Whalley D, Gravelle H, Sibbald B. Effect of the new contract of GP's working lives and perceptions of quality of care: longitudinal survey. British Journal of General Practice. 2008;58:8–14. doi: 10.3399/bjgp08X263758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wörz M, Busse R. Analysing the impact of health-care system change in the EU member states - Germany. Health Economics. 2005;14 Suppl. 1:S133–S149. doi: 10.1002/hec.1032. [DOI] [PubMed] [Google Scholar]