Abstract
Background
Neuropsychiatric systemic lupus erythematosus (NPSLE) is a major complication for lupus patients, which often leads to cognitive disturbances and memory loss and contributes to a significant patient morbidity and mortality. The presence of anti-neuronal autoantibodies (aAbs) has been identified; as examples, anti-NMDA receptors and anti-Ribsomal P aAbs have been linked to certain pathophysiological features of NPSLE.
Methods and Findings
In the current study, we used a proteomic approach to identify an intermediate neurofilament alpha-internexin (INA) as a pathogenetically relevant autoantigen in NPSLE. The significance of this finding was then validated in an expanded of a cohort of NPSLE patients (n = 67) and controls (n = 270) by demonstrating that high titers of anti-INA aAb was found in both the serum and cerebrospinal fluid (CSF) of ∼50% NPSLE. Subsequently, a murine model was developed by INA immunization that resulted in pronounced cognitive dysfunction that mimicked features of NPSLE. Histopathology in affected animals displayed cortical and hippocampal neuron apoptosis. In vitro studies further demonstrated that anti-INA Ab mediated neuronal damage via inhibiting axonal elongation and eventually driving the cells to apoptosis.
Conclusions
Taken together, this study identified a novel anti-neurofilament aAb in NPSLE, and established a hitherto undescribed mechanism of aAb-mediated neuron damage that could have relevance to the pathophysiology of NPSLE.
Introduction
Systemic lupus erythematosus (SLE) is the prototypic autoimmune disorder characterized by protean systemic manifestations and the presence of a wide spectrum of autoantibodies (aAbs). Currently, ∼200 aAbs have been identified in SLE and the number continues to grow [1]–[5]. However, only few of the aAbs have demonstrated clinical significance or value as biomarkers to facilitate diagnosis, disease activity assessment, disease phenotype dissection or prediction of prognosis. Furthermore, even fewer aAbs have established causal roles in the pathogenesis of SLE [6]–[9]. Therefore, most of the SLE-related aAbs were interpreted as the immune responses secondary to tissue injury and/or represent quantitative amplification of natural aAbs secondary to SLE polyclonal B cell activation [10]–[15].
Neuropsychiatric SLE (NPSLE) is a clinical feature of SLE attended by cognitive dysfunction and memory loss that contributes to significant patient morbidity and mortality [7], [16]–[19]. The presence of anti-neuronal aAb has been known in SLE for over 2 decades and several specific aAb potentially associated with NPSLE have been identified [2], [8], [20]–[30]. A seminal study was reported by Diamond and colleagues who demonstrated that a subset of anti-dsDNA from SLE patients binds NR2 glutamate receptors in the CNS [31], [32], and found that these aAb mediated cognitive impairment and emotional disturbances [33], [34]. Recently, another important finding demonstrated that anti-ribosomal P aAb could induce depression in mice via targeting a novel neuronal surface protein causing calcium influx and apoptosis [35], [36]. These findings support the hypothesis that certain aAbs against CNS autoantigens are pathogenic and display different mechanisms that could help understand the various NPSLE clinical phenotypes.
In the current study, we indentified the intermediate neurofilament alpha-internexin (INA) as a target antigen in NPSLE by using a proteomics approac\h. This finding was then validated in an expanded of a cohort of NPSLE patients and controls showing that significantly higher titers of aAb against INA are found in both the serum and more importantly, the cerebrospinal fluid (CSF) of NPSLE. Subsequently, a murine model was developed by INA immunization that bears pronounced cognitive dysfunction which mimics NPSLE. Brain tissue histopathology displayed cortical and hippocampal neuron apoptosis. In vitro studies further demonstrated that anti-INA Ab could mediate neuronal damage by inhibiting axonal elongation and driving the neurons to apoptosis. Taken together, this study identified a novel anti-neurofilament aAb in NPSLE, and established a hitherto undescribed mechanism of aAb-mediated neuron damage that could have relevance to the pathophysiology of NPSLE.
Materials and Methods
Ethics Statement
The study was approved by the Institutional Review Board of Renji Hospital. All subjects or their families gave written informed consent. All experimental protocols were approved by the Animal Care and Use Committee of Shanghai Jiao Tong University School of Medicine, the approval numbers for this study is 2007126 and 2008078. The cerebellar tissue slides of non-human primate were purchased from EUROIMMUN(BIOCHIP Mosaic™ Cerebellum, Germany).
NPSLE Patients and Controls
Two hundred and fifty-six hospitalized patients admitted to the Departments of Rheumatology, Neurology, or Emergency Medicine, Shanghai Renji Hospital from January 5, 2005 to December 26, 2008, were enrolled in the study. All SLE were diagnosed according to the 1997 American College of Rheumatology (ACR) revised classification criteria. NPSLE (n = 67) was classified according to the ACR nomenclature and case definitions [16], [37], [38]. Control groups included (i) a separate group of SLE (n = 12) manifested as cerebral infarction (CI) with or without anti-phospholipid aAbs; (ii) SLE that had developed septic meningitis (n = 22) where the diagnosis was established when a specific bacterial or fungal pathogen was isolated in CSF; (iii) active SLE without CNS involvement (n = 85); (iv) rheumatoid arthritis (n = 30); (v) other neurological diseases (n = 40); and (vi) healthy donors (n = 81) where hospital staff and medical students served as normal controls. Serum samples from patients and healthy donors, and totally 177 CSF samples from NPSLE and disease controls were obtained. The characteristics of the study populations are summarized in Table 1. The majority of the CSF samples have been used in our published reports [39], [40].
Table 1. Characteristics of the study population.
| Groups | Gender: M/F | Age: years (Mean±SD) | Sera/CSF: number | Descriptions |
| *NPSLE | 8/59 | 29.5±11.6 | 67/60 | Acute confusional state in 40 patients (22 complicated with seizure, 4 psychosis, 2 myelopathy, 2 seizure and psychosis, 2 seizure and myelopathy, 1 aseptic meningitis, 1 chorea, 1 myasthenia gravis), isolated cognitive dysfunction in 6 (2 with headache), seizure in 6, psychosis in 3, Demyelinating Syndrome in 2, movement disorder (chorea) and cranial neuropathy in 1, Guillain-Barré Syndrome in 1 and myelopathy in 7 patients. |
| SLE with Cerebral Infarction(CI) | 3/9 | 35.5±12.1 | 12/10 | 6 with anti-phospholipid antibodies. |
| SLE Control | 8/77 | 32.4±10.4 | 85/28 | Active SLE without CNS manifestation. |
| SLE with Septic Meningitis | 1/21 | 46.3±11.2 | 0/22 | Mycobacterium tuberculosis in 13, Cryptococcus neoformans in 9 patients. |
| Rheumatoid Arthritis(RA) | 4/26 | 36.7±13.3 | 30/0 | _ |
| Neuro-disease | 25/15 | 42.9±14.5 | 0/40 | cerebrovascular disease in 6, epilepsy in 2, migraine in 5, demyelinating disease in 4, spinal stenosis in 1, leukodystrophy in 1, myelopathy in 2, mild head trauma in 3, and CNS infection in 16 patients. |
| Normal Control | 21/60 | 39.3±13.2 | 81/0 | _ |
* All of the 67 NPSLE patients were evaluated by Glasgow or Mini Mental State Examination (MMSE) and showed conscious disturbance or a cognitive deficit.
Animals
SD rats and C57BL/6 mice, all females, were purchased from Shanghai SLAC Laboratory Animal Co. Ltd. Pregnant SD rats were used for primary embryo neuron cell culture.
Protein preparation, 2-D electrophoresis, immunoblotting and mass spectrometry
Brain and spinal cords were isolated from adult SD rats, and protein was extracted by a commercial protein-extraction kit (CALBIOCHEM Proteo Extract, 539779, Darmstadt, Germany). 2-DE was performed according to manufacturer's instructions (BIO-RAD, 163-2105, USA). After the electrophoresis, the gels were stained with Coomassie brilliant blue or used for protein transfer onto nitrocellulose membranes. Western blotting was performed as described previously [24], [26], [27], [41]. The serum samples were diluted to 1∶100 for immunoblotting the membranes and the bound antibodies were visualized by 5-Bromo-4-chloro-3-indolylphosphate/Nitroblue etrazolium (BCIP/NBT, CALBIOCHEM, 203790). The positive spot in the gel corresponding to the one identified on the nitrocellulose membranes were isolated, digested with trypsin and then subjected to MALDI-TOF MS (Applied Biosystems, USA) operated in the reflectron-delayed extraction mode (Central Research of Medical College of Fu Dan University, Shanghai). The peptide mass data were searched against the protein database SwissProt.
Antigen cloning and antibodies
A commercial plasmid (pReceiver-Z0330-B01, Fulengen, China) containing an insert of the full length open reading frame of the human INA gene was transduced into E. coli BL21-DE3 (Novagen, Sweden), and the expressed recombinant protein was purified by Ni2+ resin (20 mM Tris buffer, pH 10.0) (File S1). Rabbit anti-human polyclonal antibodies to INA were generated by immunizing rabbits with recombinant INA (rINA), purified by protein A and affinity chromatography, and a control IgG was prepared in parallel (technical service provided by Chinese Academy of Science). Monoclonal antibodies to INA (Chemicon, MAB 5224, Temecula, CA), alkaline phosphatase-conjugated goat anti-human IgG (KPL, 05-10-06, Gaithersburg, MD, USA), anti-caspase 3 antibody (Santa Cruz Biotechnology, sc-22140, CA, USA, produced in Goat; and AbCam, ab13847, Cambridge, MA, USA, produced in Rabbit), FITC-conjugated goat anti-rabbit IgG (KPL, 02-15-06), TRITC-conjugated goat anti-mouse IgG (KPL, 03-18-09), TRITC-conjugated goat anti-Rabbit IgG (KPL, 03-15-06) FITC-conjugated donkey anti-rabbit IgG (Jackson ImmunoResearch, 711-095-152, West Grove, PA), TRITC-conjugated donkey anti-goat IgG (Jackson ImmunoResearch, 705-025-003), anti-His-tag polyclonal antibody (Cell Signaling, 2365, Danvers, MA), were used in experiments.
Enzyme-linked immunosorbent assay (ELISA), immunoblotting and indirect immunofluorescence
Fifty µl of purified rINA (2 µg/ml) was coated onto 96-well micro-plates (Corning Costar, 9018, USA). After the plates were blocked with 1% gelatin in PBS, sera diluted at 1∶100, or undiluted CSF were then added. The anti-INA pAb diluted at 1∶10000 was used as the positive control. In the immunoblotting assay, rINA was subjected to 10% SDS-PAGE under reducing conditions and transferred onto nitrocellulose membranes. After blocking, the membrane was probed with serum (diluted from 1∶200 to 1∶1000) and CSF (dilution of 1∶ 10 or 1∶20). The ELISA and immunoblotting assays were performed according to standardized protocol. Mice, SD rats, monkey cerebral, spinal cord or cerebellar tissue slides (EUROIMMUN, BIOCHIP Mosaic™ Cerebellum, Germany), and SD rat embryo neuron substrate coverslips were used in indirect immunofluorescence study. Serum or CSF samples were diluted to 1∶100, or undiluted, respectively. The anti-INA pAb diluted to 1∶200 was used as the positive control. Secondary antibodies were conjugated to either FITC or TRITC as described above. In some experiments, serum was pre-incubated and absorbed with rINA [42], [43].
Immunization Protocol
Six to 8 week old female C57BL/6 mice were immunized intraperitoneally (i.p.) with vehicle alone or 300 µg rINA, per mouse, per immunization, in 100 µl of saline. The first immunization was performed using Complete Freund's Adjuvant (CFA) (Sigma-Aldrich, F5581, St. Louis, USA). Four boosters were given at bi-weekly intervals in Incomplete Freund's Adjuvant (IFA) (Sigma-Aldrich, F5506). To facilitate the increased permeability of the blood-brain barrier, LPS (E. coli, 055:B5, Sigma), at a dose of 3 mg/kg diluted in lactated Ringers solution to 0.3 mg/ml, was given as an i.p. injection twice, 48 hr apart at 8 weeks after the last INA immunization. The histology, cognitive and behavioral studies were performed at 1–2 weeks after the LPS treatment. The experimental protocol was adapted from previous publications[31]–[33]. Animals were sacrificed after the cognitive test.
Behavioral Assays
An experimental group (INA immunized, LPS-treated, n = 16) and two control groups (normal, n = 10 and INA immunized alone, n = 12) were studied. The studies included: the Morris water maze (spatial learning and reference memory), open-field activity, and beam-walking. The water maze task comprised two phases and lasted for 5 consecutive days [44], which included a place navigation test in the initial 4 days of testing and a probe trial on day 5. The data were collected as described previously [45].
Immunohistochemical staining
Animals were sacrificed by deeply anesthetizing with sodium pentobarbital (i.p., 40 mg/kg of body weight) and then transcardially perfused with saline followed by a fixative containing 4% paraformaldehyde and 0.05% glutaraldehyde in 0.1 M phosphate buffer (pH 7.4). For paraffin sections, the brains were removed, post-fixed over 48 h in 4% paraformaldehyde, and then embedded in paraffin. Coronal brain sections of hippocampal and cortex tissue were cut at 5 um. The TUNEL assay for apoptosis was carried out by using ApopTag® Plus Peroxidase In Situ Apoptosis Detection Kit (Chemicon, S7101).
Primary cultures of cortical neurons
Cultures of pure cortical neurons were obtained from E16-17 embryos of SD rats as previously reported [46], [47]. Single-cell suspensions were collected and plated into cell culture plates pre-coated with poly-L-lysine (Sigma-Aldrich, p2636) at a density of 0.5×105 cells/well for a 96-well plate (for MTT reduction assay) or 0.3×105 cells/well for a 24-well chamber slide (for immunocytochemisty), and cultured in Dulbecco's minimum essential medium (DMEM) containing 10% heat-inactivated fetal bovine serum and 5% heat-inactivated horse serum at 37°C in a humidified 5% CO2 incubator. After attachment, the medium was replaced by serum-free Neurobasal medium supplemented with 2% B27 and 2 mM glutamine (all purchased from Gibco, Grand Island, NY). Neuronal cultures were subjected to various concentrations of sterile anti-INA pAb or control IgG. The neurite length assessment and cell viability was performed 24 or 96 hours later. In some experiments, caspase-3 fmk Inhibitor Z-DEVD (R&D, FMK004) at final working concentrations of 100 uM was added to the cell culture.
Immunocytochemistry
The MTT (3(4,5-dimethylthiazol-2-yl)2,5-diphenyltetrazolium bromide)(Sigma-Aldrich) assay was used to study the reduction capacity of cortical neurons cultured in vitro as described previously [46], [47]. Survival of control group neurons was defined as 100% and the treated groups were expressed as percent of control group in MTT assay. Other cells were fixed with 4% paraformaldehyde, blocked with 10% normal goat serum for 20 min, permeabilized with 0.2% Triton X-100 for 10 min, and then washed three times with 0.01 mM PBS. Monoclonal antibody against INA, anti-caspase 3 antibody, Hoechst 33342 to stain nuclei (Sigma-Aldrich, B 2261), and then secondary antibodies were applied in cell staining. Some cultures were stained with secondary antibody alone. The coverslips were rinsed and mounted with Gel/Mount aqueous anti-fade mounting media (Biomeda Corp). The results of immunostaining were examined with an Olympus BX 60 microscope or confocal laser scanning microscope (ZEISS LSM 510 META). Image-Pro Plus software was used to allow quantitative analysis. The longest neurite from each single cell of different groups was measured at 24 h after pAb treatment. 200 cells from each preparation were randomly selected and each experiment was performed in triplicate cover slips, more than 600 cells of each cell group per experiment were measured.
Statistical analysis
Data were expressed as mean±S.E.M. Student's t-test, ANOVAs with repeated measures, and one-way ANOVA followed by post hoc Dunnett's t-test were used for statistical evaluation of differences between groups. An alpha level of 0.05 was used as the criterion for significance.
Results
Identification of the 56 kDa internexin as target autoantigen in NPSLE
Our studies began by utilizing the brain or spinal cord tissue sections from mice, rat, and monkey as substrates for screening anti-neuronal aAbs in the sera of NPSLE patients by indirect immunofluorescence. Four NPSLE sera (two patients with severe cerebralitis and myelitis, one with seizures, one with psychosis) were identified by their reactivity to all species (Figure S1). All sera probes are ANA positive without cytoplasmic staining against Hep2 cells, and neither have anti-ribsomal P antibodies. Brain and spinal cord proteins of the Sprague-Dawley (SD) rat were extracted, then resolved by 2-dimention electrophoresis (2-DE) and immunoblotted with these four sera, all of which recognized a protein spot at 56 kDa/pI 5.2 (Figure 1). The spot was excised from the gel, cleaved with trypsin, and subjected to matrix-assisted laser desorption ionization time of flight mass spectrometry (MALDI-TOF MS). The determined peptide mass data with the highest score matched rat α-internexin (INA) (SwissProt accession no. Theoretical Mr = 56115.6 and pI = 5.20). BLAST analysis revealed that INA is highly conserved from rodents to Homo sapiens (91–94% homology) [48]–[50]. Of note, it has been reported that there is no cross antigenicity of INA with other neurofilament proteins [51], [52].
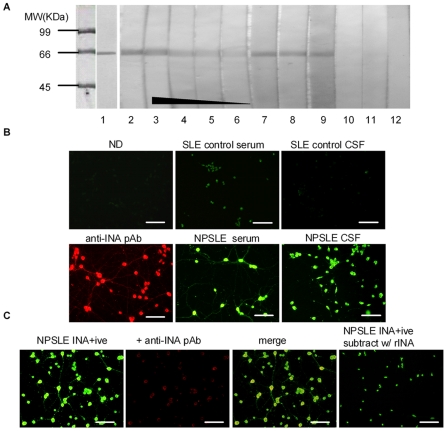
Figure 1. Identification of α-internexin (INA) as target antigen in NPSLE serum.
The proteins extract from rat brain and spinal cord were separated by 2-DE and stained with colloidal Coomassie blue (upper panels), or immunoblotted with NPSLE (lower left panel) or control (lower right panel) sera. An immunoreactive spot at ∼56 kDa/pI 5.2 was excised and subjected to MALDI-TOF MS. By searching the protein database SwissProt, the peptide mass-mapping matched rat α-internexin (INA, alpha;α-INA; Rattus norvegicus, gi|9506811, kDa 56081.6, PI 5.2, protein score 99.99%). The data is representative of 4 independent experiments.
Anti-INA is a novel aAb in the sera and CSF of NPSLE and the CSF anti-INA levels correlate with cognitive impairment
To confirm that anti-INA aAbs are found in the sera of NPSLE patients, purified His-tagged recombinant human INA was used in a western blot. As expected, sera probes have a dose-dependent reactivity to INA as opposed to control samples (Figure 2A). Of note, anti-INA aAb was also detected in 3 of 4 CSF from the probe NPSLE. In a parallel indirect immunofluorescence assay, anti-INA positive serum/CSF probes from NPSLE reacted with primary cultured rat cortical neurons, with a distinctive cytoplasmic and neurite staining pattern compared to a faint anti-nuclear staining pattern from control SLE samples (Figure 2B). Anti-INA polyclonal antibody (pAb) obtained from rabbit showed a similar staining pattern as the probes, and when double-stained with the probe, a co-localization and competitive effect can be observed under fluorescent microscope. Finally, pre-incubated with INA, the probes lost their cytoplasmic staining to neurons (Figure 2C).
Figure 2. Anti-INA aAb in the sera and CSF of NPSLE.
(A) Purified His-tagged recombinant human INA (66 kDa) was blotted with anti-His antibody (lane 1), anti-INA pAb (lane 2), NPSLE serum probe at serial dilutions of 1∶200, 1∶400, 1∶800, 1∶1000 (lane 3–6), the same patient's CSF diluted in 1∶10 and 1∶20 (lane 7–8), another NPSLE serum probe and the patient's CSF (lane 9–10), CSF from a SLE control and a neurological disease control (lane 11–12). (B) SD rat primary neuron substrate stained with serum of normal donor (ND), anti-INA pAb, serum or CSF from SLE patients as indicated. (C) NPSLE serum probe competitive inhibit anti-INA pAb staining. After pre-incubated with recombinant INA (rINA), the serum probe lost its cytoplasmic staining.
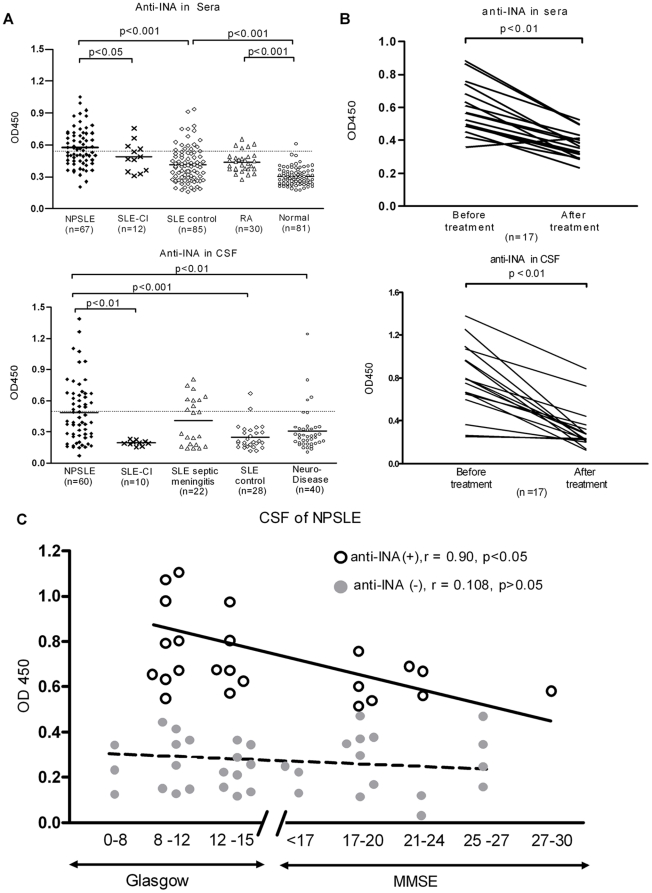
After the thorough confirmation of the existence of anti-INA aAb in NPSLE, a further validation ELISA was carried out in a cohort of patients (Figure 3A). We tested for anti-INA aAbs in the sera of NPSLE (n = 67), SLE manifested as cerebral infarction (CI) with or without aPL aAbs (n = 12), active SLE without CNS involvement (n = 85), rheumatoid arthritis (RA) patients (n = 30) and normal controls (n = 81), and the positive anti-INA Ab rates in sera among aforementioned groups were 52.2% (35/67), 33.3% (4/12), 18.8% (16/85), 13.3% (5/30) and 1.2% (1/81), respectively. The different frequencies of anti-INA Ab between NPSLE group and other control groups was statistically significant (p<0.001). More importantly, the OD of anti-INA Ab in CSF of NPSLE patients was significant higher than that of SLE-CI, SLE controls and neurological diseases controls. At a cutoff value determined by the average OD of SLE controls plus 2SD, the rates of positive anti-INA in CSF of NPSLE (n = 60), SLE-CI (n = 12), SLE controls (n = 28), neurological disease controls (n = 40) were 41.7% (25/60), 0% (0/12), 7.1% (2/28), 10% (4/40), respectively. Unexpectedly, 40.9% (9/22) SLE with CNS infections also had detectable anti-INA Ab in CSF. Nevertheless, longitudinal analysis of both sera and CSF among 17 NPSLE patients showed that the levels of anti-INA Ab significantly declined after initiation of therapy and eventual clinical remission (Figure 3B). The titer of the Ab was inversely correlated with the cognitive status as measured by Glasgow coma scale or Mini Mental State Examination (MMSE) in the NPSLE patients who had anti-INA Abs in their CSF (Figure 3C).
Figure 3. Anti-INA aAb in the sera and CSF is correlated with NPSLE activity.
(A) Anti-INA aAbs in sera or CSF were determined by ELISA. SLE-CI = SLE with cerebral infarction. (B) Dynamic changes anti-INA Ab levels in the sera or CSF from NPSLE patients before and after induction therapy which lead to clinical remission. (C) The NPSLE patients who have positive anti-INA Abs in CSF, the titer of the Ab was inversely correlated with the cognitive status as measured by Glasgow coma scale or MMSE.
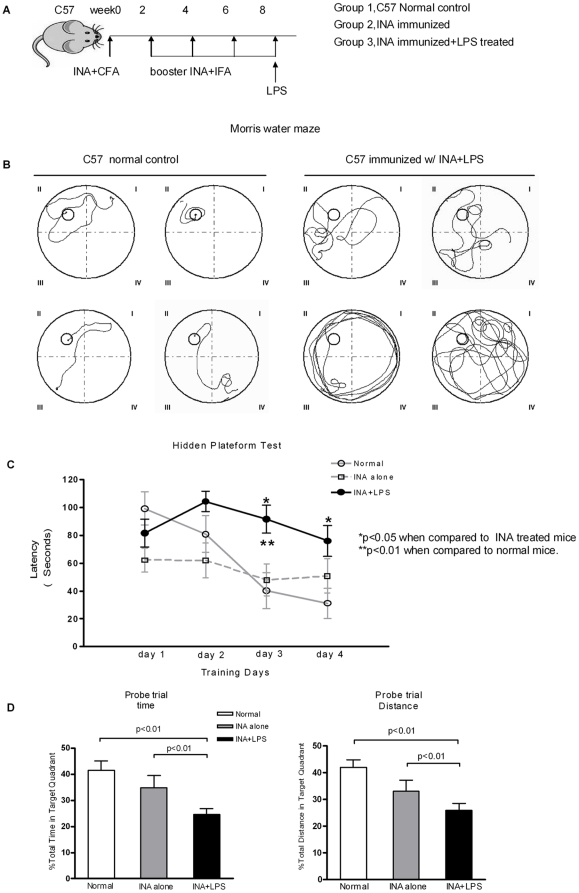
Mice immunized with INA plus LPS display cognitive impairments that mimic NPSLE
A key question was whether anti-INA Abs are pathogenic or merely a coincidental phenomenon. To address this question, a murine model was established in order to assess the in vivo effects of anti-INA on CNS (Figure 4A). Briefly, all mice immunized with INA developed high titer anti-INA Abs 8–9 weeks after immunization (data not shown). Only the mice immunized with INA plus LPS, which facilitates increasing the permeability of the blood-brain barrier (BBB), displayed distinctive learning and memory deficits on tasks that depend on the integrity of the hippocampus and cortex as gauged by Morris water maze test (Figure 4B). The time latency for the mice finding a submerged hidden platform in the water maze remained prolonged over the 4 days of training in the INA+LPS group (Figure 4C). In addition, when the platform was removed at day 5, the control groups of mice spent more time and effort in the quadrant where the previous platform placed, as opposed to the INA+LPS group thus suggesting a significant memory impairment (Figure 4D). This impairment in learning and memory function is consistent with the neuropsychiatric studies of lupus-prone murine models which demonstrate poor performance in spatial memory tasks [53]–[57]. Other profound neurological dysfunction, such as exploratory behavior and motor coordination, was also observed in INA+LPS mice in open field activity and beam walking tasks (Figure S2).
Figure 4. Mice immunized with INA plus LPS display cognitive impairments.
(A) Immunization protocol in C57 mice. Normal control (n = 10), INA immunized (n = 12), INA+LPS treated (n = 16). (B) Morris water maze test. Representative swimming traces of mice from different groups on the third training day. The hidden platform is located in quadrant II. (C) The time latency to find the hidden platform in different groups of mice during consecutive 4 training days. (D) The platform was removed at day 5, and the time (left) and efforts (right) mice spent in the quadrant where the previous platform placed were calculated. All data were presented as mean±S.E.M.
INA immunized and LPS treated mice exhibited hippocampal and cortical neuron apoptosis
As evidence that anti-INA Ab indeed penetrated the BBB and gained access to its cognate CNS targets, it was observed that there was IgG staining of the choroid plexus in INA+LPS treated mice (Figure 5A). The effects of anti-INA penetration can be appreciated as prominent diffuse hippocampal (CA1, CA3 and dentate gyrus regions) and cortical neuron apoptosis as gauged by TUNEL staining in INA+LPS treated mice, but not in mice immunized with INA alone or in sham controls (Figure 5B).
Figure 5. INA immunized plus LPS treated mice exhibited hippocampus and cortex neuron apoptosis.
(A) IgG deposition at the choroid plexus (left) and hippocampus (right) in different groups of mice. (B) CA1, CA3 and dentate gyrus regions of hippocampal, and cortex areas from indicated group of mice. TUNEL staining demonstrated neuron apoptosis. (×400, Bar = 50 µm; ×100, Bar = 200 µm).
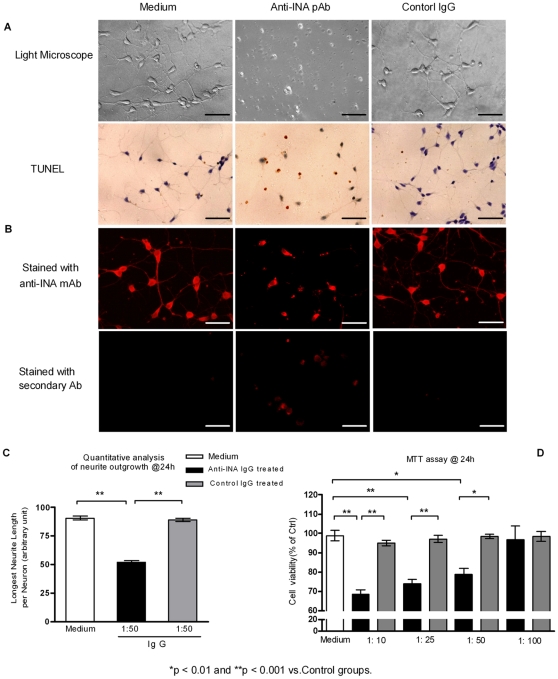
The anti-INA pAb inhibit the growth of neurites and result in neuron apoptosis in vitro
To determine whether there is a pathogenic effect of anti-INA Ab on neurons, rat embryo cortical neurons were subjected to anti-INA pAb or control IgG. After 96 h of culture, cells exposed to anti-INA pAb displayed a significant neurotoxicity as gauged by impeded axonal outgrowth and cell viability (TUNEL staining) (Figure 6A). Of note, anti-INA pAb, but not control IgG, could penetrate the cells as demonstrated by directly secondary antibody staining. As an intermediate neurofilament component, the normal staining pattern of INA by an anti-INA monoclonal Ab (mAb) was characterized within the cytoplasm of the cells and also in the cell processes (Figure 6B, also seen in Figure 2B–C). Seemingly related to these observations, it was noted that cells treated with anti-INA pAb sequestrated INA in a cytoplasmic compartment surrounding the nuclei.
Figure 6. The anti-INA pAb inhibit the growth of neurites and result in neuron apoptosis in vitro.
(A) Primary rat embryo neurons were co-cultured with medium, sterile anti-INA pAb (1∶50), or control IgG for 96 hrs. The neurite outgrowth and cell viability was observed by light microscopy. Apoptotic cells were detected by TUNEL assay. (B) A monoclonal antibody (Mab 5224) against INA was used for displaying INA location. The TRITC goat anti-rabbit secondary antibody staining was to demonstrate the internalization of co-cultured Abs during the neuron cell growth. (Bar = 25 µm) (C) Quantitative measurement of cultured neurons axonal length at 24 hrs. (D) Viability of primary cultured neurons subject to indicated concentrations of anti-INA pAb or control IgG after 24 h. The percentage of cell survival normalized to control cells was applied in MTT assay. Data are represented as mean±SEM of three independent experiments.
The neurotoxic effect of anti-INA pAb could be appreciated as early as the 24th hour of culture. Quantitative measurement of neurite length illustrated a significant reduction by ∼50% after 24 h exposure of anti-INA pAb (Figure 6C). In parallel, the MTT assay showed that anti-INA pAb impaired neuron viability in a dose-dependent manner (Figure 6D). Furthermore, the anti-INA pAb-induced neuron apoptosis process was detected by Caspase-3 activation. The perfectly overlapped co-localization of Caspase-3 and INA in the cytoplasm indicated a possible link between those two molecules. Interestingly, when Caspase-3 was blocked by a specific inhibitor, the neurite outgrowth was still impeded by anti-INA pAb, which suggested that apoptosis is the downstream effect of anti-INA mediated neuron damage (Figure 7).
Figure 7. Apoptosis with caspase-3 activation is the downstream effect of anti-INA mediated neuron damage.
Primary rat cortical neurons were co-cultured with anti-INA pAb or control IgG for 24 h. Caspase-3 inhibitor was added as indicated. The cells were triple-labeled Hoechst (blue), caspase-3 (red), and INA (green). (Scale bar = 10 µm).
Discussion
In the current study, alpha-internexin was identified as a new target autoantigen for NPSLE, in that the anti-INA aAbs in the sera of NPSLE patients are significantly increased in ∼50% of NPSLE sera. More importantly, even by using SLE control values (mean±2SD) as cut-off, anti-INA Ab is still positive in >40% of the CSF of NPSLE, which indicated a strong association between this aAb and an intrathecal autoimmune processes. In addition, the titer of anti-INA, both in the serum and CSF was correlated with disease activity, further suggesting its potential usefulness as a biomarker in NPSLE. However, its specificity and clinical value may have limitations as evidenced by a similar positive rate in the CSF of SLE patients with CNS infections [58]–[60]. It is noteworthy that the pathogenesis of NPSLE is likely multi-factorial and that antibodies to other targets may work independently or in concert to produce the various NPSLE clinical phenotypes.
INA is a constitutional intermediate neurofilament (IF) protein first described in 1985 [61].
In the mammalian nervous system, three types of IF proteins are expressed in differentiated neurons, which include light (NF-L), medium (NF-M), heavy (NF-H) neurofilament triplet proteins (NFTPs). INA is expressed abundantly to form the group of type IV IF throughout the development of the peripheral and central nervous system, and is restricted to the central nervous system in the adulthood [62]–[65]. Neuro-cytoskeletal filament proteins ingeneral [59], [60], or their components such as glial fibrillary acid protein [3], microtubule associated protein-2 [27], [66], and more recently, INA have been described as potential target autoantigens in SLE[58]. However, due to lack of sufficient validation and CSF aAb analyses in the aforementioned studies, aAbs against neurofilament proteins in NPSLE have been considered somewhat insignificant [67].
Our data not only demonstrated a link between anti-INA aAbs and NPSLE, but also took one step further to illustrate a direct neurotoxic effect of this aAb. A murine model displayed anti-INA access to its target protein when the permeability of the BBB was interrupted by LPS, resulting in profound cortical and hippocampal dependent cognitive impairment/memory loss. A plausible mechanistic explanation of the pathological NPSLE phenotype was supported by the observations that anti-INA Ab could inhibit neurite outgrowth and axonal elongation, and subsequently induced neuron apoptosis both in vivo and ex vivo.
It is known that, in adult CNS, INA is selectively expressed in the gray and underlying white matter, such as neuron cell bodies and processes of cortical layer II neuron, CA1 subfield and granule neurons of the dentate gyrus of hippocampus, cerebellar granule cells, and thin-caliber parallel fibers, as well as in the basal ganglia, thalamus, midbrain, pons and gray matter of the spinal cord [52], [61], [65], [68]–[72]. The functions of INA include a scaffold for IF formation and regulating the expression of other neurofilaments during neuronal development, and it can self-assemble into homopolymers or coassemble with other IF proteins to form NFTPs in mature neurons [64], [65], [68], [69], [73]–[76]. The contribution of INA to cytoskeletal integrity is important for axonal calibre and nerve conduction speed, and INA plays an important role in facilitating the neurite outgrowth [64], [68], [77]–[79]. Of potential relevance to our findings, it is well established that abnormal accumulation or mislocation of neurofilaments is a pathological hallmark of many human neurodegenerative disorders including amyotrophic lateral sclerosis, dementia with Lewy bodies, and Parkinson disease.More specifically, INA along with other NF proteins, are found to form pathological inclusions in a newly defined neuronal intermediate filament inclusion disease (NIFID), which presented as progressive early-onset dementia, pyramidal, and extrapyramidal dysfunctions [72], [80]. Studies with transgenic mice overexpressing IF proteins, including INA, provide evidence that dis-organization of the IF network can cause neurofilament misaccumulation, progressive neurodegeneration, and ultimate loss of neurons [73]. The findings that genetically modified mice for IF successfully mimic certain degenerative neuropathological phenotype [81]. It was also found that overexpression of INA in PC12 cells induced apoptosis-like cell death [78]. Taken together, these data support our observations that anti-INA Ab may interfere with the location and function of INA, which in turn contribute to neuronal damage.
Nevertheless, the precise mechanism of anti-INA mediated neuron damage remains unclear. Previous studies suggested that aAb induced neuronal death can occur without complement activation or Fc receptor engagement, and demonstrated that aAbs can alter behavior without causing inflammation in the CNS [32]–[35]. The role of aAb directed against NFTPs or their individual subunits in certain neurodegenerative conditions has also been implicated [82]. Although according to previous literatures that autoantibodies have been shown to penetrate various living cells, how anti-INA internalize into neurons and gain access to target proteins is still not known [83]–[86]. The possibilities of that it is LPS alters the localization of INA or allows anti-INA into cells can not be excluded, in addition, there may be another cross reactivity exists which plays a role in the anti-INA internalization process. Another key question needs to be answered is that how anti-INA Ab inhibits neurite outgrowth and drives the neuron to programmed death. A plausible explanation would be a two step process according to our data. First, anti-INA binds to INA, therefore interfere INA assembly/coassembly for neurofilament transportation, which result in INA accumulation and failure of axonal elongation. Subsequently, caspase 3 dependent apoptosis is activated due to neuron cytoskeleton “strangulation” [87], [88]. Further investigations are required to address these questions.
Supporting Information
Gene information, ORF sequence information, and vector information of EX-Z0330-B01.
(0.06 MB DOC)
Screening anti-neuronal aAbs in the sera/CSF of NPSLE and SLE control patients by indirect immunofluorescence. NPSLE serum from a patients with severe cerebralitis and myelitis was identified by its reactivity to all species. All sera/CSF of SLE probes are ANA positive without cytoplasmic staining against Hep2 cells, and neither have anti-ribsomal P antibodies. Scale bar = 50 µm.
(2.09 MB TIF)
An experimental group (INA immunized, LPS-treated, n = 16) and two control groups (normal, n = 10 and INA immunized alone, n = 12) were studied. Neurological dysfunctions including exploratory behavior and motor coordination, was observed in INA+LPS mice in open field activity and beam walking tasks.
(0.20 MB TIF)
Acknowledgments
We acknowledge technical support from the Department of Pharmacy, Shanghai Jiao Tong University School of Medicine. We appreciate Drs. Marvin Fritzler and Peihua Lu's critical review and comments on the manuscript.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
Funding: This study was supported by Shanghai Health Bureau Outstanding Young Medical Professional Program (S.Y.) and Shanghai Jiao Tong University SMC Scholar (S.Y). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Sherer Y, Gorstein A, Fritzler MJ, Shoenfeld Y. Autoantibody explosion in systemic lupus erythematosus: more than 100 different antibodies found in SLE patients. Semin Arthritis Rheum. 2004;34:501–537. doi: 10.1016/j.semarthrit.2004.07.002. [DOI] [PubMed] [Google Scholar]
- 2.Sanna G, Bertolaccini ML, Cuadrado MJ, Khamashta MA, Hughes GR. Central nervous system involvement in the antiphospholipid (Hughes) syndrome. Rheumatology (Oxford) 2003;42:200–213. doi: 10.1093/rheumatology/keg080. [DOI] [PubMed] [Google Scholar]
- 3.Sanna G, Piga M, Terryberry JW, Peltz MT, Giagheddu S, et al. Central nervous system involvement in systemic lupus erythematosus: cerebral imaging and serological profile in patients with and without overt neuropsychiatric manifestations. Lupus. 2000;9:573–583. doi: 10.1191/096120300678828695. [DOI] [PubMed] [Google Scholar]
- 4.Stinton LM, Eystathioy T, Selak S, Chan EK, Fritzler MJ. Autoantibodies to protein transport and messenger RNA processing pathways: endosomes, lysosomes, Golgi complex, proteasomes, assemblyosomes, exosomes, and GW bodies. Clin Immunol. 2004;110:30–44. doi: 10.1016/j.clim.2003.10.005. [DOI] [PubMed] [Google Scholar]
- 5.Bhanji RA, Eystathioy T, Chan EK, Bloch DB, Fritzler MJ. Clinical and serological features of patients with autoantibodies to GW/P bodies. Clin Immunol. 2007;125:247–256. doi: 10.1016/j.clim.2007.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Afeltra A, Garzia P, Mitterhofer AP, Vadacca M, Galluzzo S, et al. Neuropsychiatric lupus syndromes: relationship with antiphospholipid antibodies. Neurology. 2003;61:108–110. doi: 10.1212/01.wnl.0000058904.94330.a7. [DOI] [PubMed] [Google Scholar]
- 7.Diamond B, Volpe B. On the track of neuropsychiatric lupus. Arthritis Rheum. 2003;48:2710–2712. doi: 10.1002/art.11278. [DOI] [PubMed] [Google Scholar]
- 8.Fragoso-Loyo H, Cabiedes J, Orozco-Narvaez A, Davila-Maldonado L, Atisha-Fregoso Y, et al. Serum and cerebrospinal fluid autoantibodies in patients with neuropsychiatric lupus erythematosus. Implications for diagnosis and pathogenesis. PLoS One. 2008;3:e3347. doi: 10.1371/journal.pone.0003347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhang J, Jacobi AM, Wang T, Berlin R, Volpe BT, et al. Polyreactive autoantibodies in systemic lupus erythematosus have pathogenic potential. J Autoimmun. 2009;33:270–274. doi: 10.1016/j.jaut.2009.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Trysberg E, Nylen K, Rosengren LE, Tarkowski A. Neuronal and astrocytic damage in systemic lupus erythematosus patients with central nervous system involvement. Arthritis Rheum. 2003;48:2881–2887. doi: 10.1002/art.11279. [DOI] [PubMed] [Google Scholar]
- 11.Zameer A, Hoffman SA. B and T cells in the brains of autoimmune mice. J Neuroimmunol. 2004;146:133–139. doi: 10.1016/j.jneuroim.2003.10.052. [DOI] [PubMed] [Google Scholar]
- 12.Sidor MM, Sakic B, Malinowski PM, Ballok DA, Oleschuk CJ, et al. Elevated immunoglobulin levels in the cerebrospinal fluid from lupus-prone mice. J Neuroimmunol. 2005;165:104–113. doi: 10.1016/j.jneuroim.2005.04.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ma X, Foster J, Sakic B. Distribution and prevalence of leukocyte phenotypes in brains of lupus-prone mice. J Neuroimmunol. 2006;179:26–36. doi: 10.1016/j.jneuroim.2006.06.023. [DOI] [PubMed] [Google Scholar]
- 14.Lawrence DA, Bolivar VJ, Hudson CA, Mondal TK, Pabello NG. Antibody induction of lupus-like neuropsychiatric manifestations. J Neuroimmunol. 2007;182:185–194. doi: 10.1016/j.jneuroim.2006.10.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sled JG, Spring S, van Eede M, Lerch JP, Ullal S, et al. Time course and nature of brain atrophy in the MRL mouse model of central nervous system lupus. Arthritis Rheum. 2009;60:1764–1774. doi: 10.1002/art.24523. [DOI] [PubMed] [Google Scholar]
- 16.The American College of Rheumatology nomenclature and case definitions for neuropsychiatric lupus syndromes. Arthritis Rheum. 1999;42:599–608. doi: 10.1002/1529-0131(199904)42:4<599::AID-ANR2>3.0.CO;2-F. [DOI] [PubMed] [Google Scholar]
- 17.Sabbadini MG, Manfredi AA, Bozzolo E, Ferrario L, Rugarli C, et al. Central nervous system involvement in systemic lupus erythematosus patients without overt neuropsychiatric manifestations. Lupus. 1999;8:11–19. doi: 10.1191/096120399678847344. [DOI] [PubMed] [Google Scholar]
- 18.Ainiala H, Loukkola J, Peltola J, Korpela M, Hietaharju A. The prevalence of neuropsychiatric syndromes in systemic lupus erythematosus. Neurology. 2001;57:496–500. doi: 10.1212/wnl.57.3.496. [DOI] [PubMed] [Google Scholar]
- 19.Monastero R, Bettini P, Del Zotto E, Cottini E, Tincani A, et al. Prevalence and pattern of cognitive impairment in systemic lupus erythematosus patients with and without overt neuropsychiatric manifestations. J Neurol Sci. 2001;184:33–39. doi: 10.1016/s0022-510x(00)00492-5. [DOI] [PubMed] [Google Scholar]
- 20.Diamond B, Kowal C, Huerta PT, Aranow C, Mackay M, et al. Immunity and acquired alterations in cognition and emotion: lessons from SLE. Adv Immunol. 2006;89:289–320. doi: 10.1016/S0065-2776(05)89007-8. [DOI] [PubMed] [Google Scholar]
- 21.Hoffman SA, Arbogast DN, Ford PM, Shucard DW, Harbeck RJ. Brain-reactive autoantibody levels in the sera of ageing autoimmune mice. Clin Exp Immunol. 1987;70:74–83. [PMC free article] [PubMed] [Google Scholar]
- 22.Shoenfeld Y, Nahum A, Korczyn AD, Dano M, Rabinowitz R, et al. Neuronal-binding antibodies from patients with antiphospholipid syndrome induce cognitive deficits following intrathecal passive transfer. Lupus. 2003;12:436–442. doi: 10.1191/0961203303lu409oa. [DOI] [PubMed] [Google Scholar]
- 23.Shoenfeld Y, Twig G, Katz U, Sherer Y. Autoantibody explosion in antiphospholipid syndrome. J Autoimmun. 2008;30:74–83. doi: 10.1016/j.jaut.2007.11.011. [DOI] [PubMed] [Google Scholar]
- 24.Tin SK, Xu Q, Thumboo J, Lee LY, Tse C, et al. Novel brain reactive autoantibodies: prevalence in systemic lupus erythematosus and association with psychoses and seizures. J Neuroimmunol. 2005;169:153–160. doi: 10.1016/j.jneuroim.2005.07.015. [DOI] [PubMed] [Google Scholar]
- 25.Diamond B, Volpe BT. Antibodies and brain disease: a convergence of immunology and physiology. PLoS Med. 2006;3:e498. doi: 10.1371/journal.pmed.0030498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sasajima T, Watanabe H, Sato S, Sato Y, Ohira H. Anti-triosephosphate isomerase antibodies in cerebrospinal fluid are associated with neuropsychiatric lupus. J Neuroimmunol. 2006;181:150–156. doi: 10.1016/j.jneuroim.2006.09.003. [DOI] [PubMed] [Google Scholar]
- 27.Lefranc D, Launay D, Dubucquoi S, de Seze J, Dussart P, et al. Characterization of discriminant human brain antigenic targets in neuropsychiatric systemic lupus erythematosus using an immunoproteomic approach. Arthritis Rheum. 2007;56:3420–3432. doi: 10.1002/art.22863. [DOI] [PubMed] [Google Scholar]
- 28.Huizinga TW, Diamond B. Lupus and the central nervous system. Lupus. 2008;17:376–379. doi: 10.1177/0961203308090112. [DOI] [PubMed] [Google Scholar]
- 29.Colasanti T, Delunardo F, Margutti P, Vacirca D, Piro E, et al. Autoantibodies involved in neuropsychiatric manifestations associated with systemic lupus erythematosus. J Neuroimmunol. 2009;212:3–9. doi: 10.1016/j.jneuroim.2009.05.003. [DOI] [PubMed] [Google Scholar]
- 30.Lee JY, Huerta PT, Zhang J, Kowal C, Bertini E, et al. Neurotoxic autoantibodies mediate congenital cortical impairment of offspring in maternal lupus. Nat Med. 2009;15:91–96. doi: 10.1038/nm.1892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.DeGiorgio LA, Konstantinov KN, Lee SC, Hardin JA, Volpe BT, et al. A subset of lupus anti-DNA antibodies cross-reacts with the NR2 glutamate receptor in systemic lupus erythematosus. Nat Med. 2001;7:1189–1193. doi: 10.1038/nm1101-1189. [DOI] [PubMed] [Google Scholar]
- 32.Kowal C, DeGiorgio LA, Nakaoka T, Hetherington H, Huerta PT, et al. Cognition and immunity; antibody impairs memory. Immunity. 2004;21:179–188. doi: 10.1016/j.immuni.2004.07.011. [DOI] [PubMed] [Google Scholar]
- 33.Kowal C, Degiorgio LA, Lee JY, Edgar MA, Huerta PT, et al. Human lupus autoantibodies against NMDA receptors mediate cognitive impairment. Proc Natl Acad Sci U S A. 2006;103:19854–19859. doi: 10.1073/pnas.0608397104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Huerta PT, Kowal C, DeGiorgio LA, Volpe BT, Diamond B. Immunity and behavior: antibodies alter emotion. Proc Natl Acad Sci U S A. 2006;103:678–683. doi: 10.1073/pnas.0510055103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Katzav A, Ben-Ziv T, Chapman J, Blank M, Reichlin M, et al. Anti-P ribosomal antibodies induce defect in smell capability in a model of CNS -SLE (depression). J Autoimmun. 2008;31:393–398. doi: 10.1016/j.jaut.2008.09.002. [DOI] [PubMed] [Google Scholar]
- 36.Matus S, Burgos PV, Bravo-Zehnder M, Kraft R, Porras OH, et al. Antiribosomal-P autoantibodies from psychiatric lupus target a novel neuronal surface protein causing calcium influx and apoptosis. J Exp Med. 2007;204:3221–3234. doi: 10.1084/jem.20071285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Nived O, Sturfelt G, Liang MH, De Pablo P. The ACR nomenclature for CNS lupus revisited. Lupus. 2003;12:872–876. doi: 10.1191/0961203303lu495oa. [DOI] [PubMed] [Google Scholar]
- 38.Kozora E, Ellison MC, West S. Reliability and validity of the proposed American College of Rheumatology neuropsychological battery for systemic lupus erythematosus. Arthritis Rheum. 2004;51:810–818. doi: 10.1002/art.20692. [DOI] [PubMed] [Google Scholar]
- 39.Lu X, Gu Y, Wang Y, Chen S, Ye S. Prognostic factors of lupus myelopathy. Lupus. 2008;17:323–328. doi: 10.1177/0961203307088005. [DOI] [PubMed] [Google Scholar]
- 40.Lu X, Zhu C, Qian J, Chen X, Ye S, Gu Y. Intrathecal cytokine and chemokine profiling in neuropsychiatric lupus or lupus complicated with central nervous system infection. Lupus. 2010;2010 Feb 23 doi: 10.1177/0961203309357061. [DOI] [PubMed] [Google Scholar]
- 41.Rajasalu T, Teesalu K, Janmey PA, Uibo R. Demonstration of natural autoantibodies against the neurofilament protein alpha-internexin in sera of patients with endocrine autoimmunity and healthy individuals. Immunol Lett. 2004;94:153–160. doi: 10.1016/j.imlet.2004.05.002. [DOI] [PubMed] [Google Scholar]
- 42.Watanabe H, Seino T, Sato Y. Antibodies to triosephosphate isomerase in patients with neuropsychiatric lupus. Biochem Biophys Res Commun. 2004;321:949–953. doi: 10.1016/j.bbrc.2004.07.051. [DOI] [PubMed] [Google Scholar]
- 43.Lennon VA, Wingerchuk DM, Kryzer TJ, Pittock SJ, Lucchinetti CF, et al. A serum autoantibody marker of neuromyelitis optica: distinction from multiple sclerosis. Lancet. 2004;364:2106–2112. doi: 10.1016/S0140-6736(04)17551-X. [DOI] [PubMed] [Google Scholar]
- 44.D'Hooge R, De Deyn PP. Applications of the Morris water maze in the study of learning and memory. Brain Res Brain Res Rev. 2001;36:60–90. doi: 10.1016/s0165-0173(01)00067-4. [DOI] [PubMed] [Google Scholar]
- 45.Zhang WW, Song MK, Cui YY, Wang H, Zhu L, et al. Differential neuropsychopharmacological influences of naturally occurring tropane alkaloids anisodamine versus scopolamine. Neurosci Lett. 2008;443:241–245. doi: 10.1016/j.neulet.2008.07.048. [DOI] [PubMed] [Google Scholar]
- 46.Nie BM, Jiang XY, Cai JX, Fu SL, Yang LM, et al. Panaxydol and panaxynol protect cultured cortical neurons against Abeta25-35-induced toxicity. Neuropharmacology. 2008;54:845–853. doi: 10.1016/j.neuropharm.2008.01.003. [DOI] [PubMed] [Google Scholar]
- 47.Nie BM, Yang LM, Fu SL, Jiang XY, Lu PH, et al. Protective effect of panaxydol and panaxynol on sodium nitroprusside-induced apoptosis in cortical neurons. Chem Biol Interact. 2006;160:225–231. doi: 10.1016/j.cbi.2006.02.001. [DOI] [PubMed] [Google Scholar]
- 48.Chien CL, Liem RK. Characterization of the mouse gene encoding the neuronal intermediate filament protein alpha-internexin. Gene. 1994;149:289–292. doi: 10.1016/0378-1119(94)90163-5. [DOI] [PubMed] [Google Scholar]
- 49.Chan SO, Chiu FC. The 66-kDa neurofilament protein (NF-66): sequence analysis and evolution. Neurochem Res. 1996;21:449–455. doi: 10.1007/BF02527709. [DOI] [PubMed] [Google Scholar]
- 50.Chan SO, Peng D, Chiu FC. Heterogeneous expression of neurofilament proteins in forebrain and cerebellum during development: clinical implications for spinocerebellar ataxia. Brain Res. 1997;775:107–118. doi: 10.1016/s0006-8993(97)00834-2. [DOI] [PubMed] [Google Scholar]
- 51.Kaplan MP, Chin SS, Fliegner KH, Liem RK. Alpha-internexin, a novel neuronal intermediate filament protein, precedes the low molecular weight neurofilament protein (NF-L) in the developing rat brain. J Neurosci. 1990;10:2735–2748. doi: 10.1523/JNEUROSCI.10-08-02735.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Chien CL, Mason CA, Liem RK. alpha-Internexin is the only neuronal intermediate filament expressed in developing cerebellar granule neurons. J Neurobiol. 1996;29:304–318. doi: 10.1002/(SICI)1097-4695(199603)29:3<304::AID-NEU3>3.0.CO;2-D. [DOI] [PubMed] [Google Scholar]
- 53.Narendran A, Hoffman SA. Characterization of brain-reactive autoantibodies in murine models of systemic lupus erythematosus. J Neuroimmunol. 1989;24:113–123. doi: 10.1016/0165-5728(89)90105-7. [DOI] [PubMed] [Google Scholar]
- 54.Maric D, Millward JM, Ballok DA, Szechtman H, Denburg JA, et al. Neurotoxic properties of cerebrospinal fluid from behaviorally impaired autoimmune mice. Brain Res. 2001;920:183–193. doi: 10.1016/s0006-8993(01)03060-8. [DOI] [PubMed] [Google Scholar]
- 55.Arabo A, Costa O, Tron F, Caston J. Spatial and motor abilities during the course of autoimmune disease in (NZW x BXSB)F1 lupus-prone mice. Behav Brain Res. 2005;165:126–137. doi: 10.1016/j.bbr.2005.06.038. [DOI] [PubMed] [Google Scholar]
- 56.Sakic B, Hanna SE, Millward JM. Behavioral heterogeneity in an animal model of neuropsychiatric lupus. Biol Psychiatry. 2005;57:679–687. doi: 10.1016/j.biopsych.2004.11.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Mondal TK, Saha SK, Miller VM, Seegal RF, Lawrence DA. Autoantibody-mediated neuroinflammation: pathogenesis of neuropsychiatric systemic lupus erythematosus in the NZM88 murine model. Brain Behav Immun. 2008;22:949–959. doi: 10.1016/j.bbi.2008.01.013. [DOI] [PubMed] [Google Scholar]
- 58.Kimura A, Sakurai T, Tanaka Y, Hozumi I, Takahashi K, et al. Proteomic analysis of autoantibodies in neuropsychiatric systemic lupus erythematosus patient with white matter hyperintensities on brain MRI. Lupus. 2008;17:16–20. doi: 10.1177/0961203307085112. [DOI] [PubMed] [Google Scholar]
- 59.Robbins ML, Kornguth SE, Bell CL, Kalinke T, England D, et al. Antineurofilament antibody evaluation in neuropsychiatric systemic lupus erythematosus. Combination with anticardiolipin antibody assay and magnetic resonance imaging. Arthritis Rheum. 1988;31:623–631. doi: 10.1002/art.1780310507. [DOI] [PubMed] [Google Scholar]
- 60.Senecal JL, Rauch J. Hybridoma lupus autoantibodies can bind major cytoskeletal filaments in the absence of DNA-binding activity. Arthritis Rheum. 1988;31:864–875. doi: 10.1002/art.1780310707. [DOI] [PubMed] [Google Scholar]
- 61.Pachter JS, Liem RK. alpha-Internexin, a 66-kD intermediate filament-binding protein from mammalian central nervous tissues. J Cell Biol. 1985;101:1316–1322. doi: 10.1083/jcb.101.4.1316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Fliegner KH, Ching GY, Liem RK. The predicted amino acid sequence of alpha-internexin is that of a novel neuronal intermediate filament protein. EMBO J. 1990;9:749–755. doi: 10.1002/j.1460-2075.1990.tb08169.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ho CL, Liem RK. Intermediate filaments in the nervous system: implications in cancer. Cancer Metastasis Rev. 1996;15:483–497. doi: 10.1007/BF00054014. [DOI] [PubMed] [Google Scholar]
- 64.Lee MK, Cleveland DW. Neurofilament function and dysfunction: involvement in axonal growth and neuronal disease. Curr Opin Cell Biol. 1994;6:34–40. doi: 10.1016/0955-0674(94)90113-9. [DOI] [PubMed] [Google Scholar]
- 65.Yuan A, Rao MV, Sasaki T, Chen Y, Kumar A, et al. Alpha-internexin is structurally and functionally associated with the neurofilament triplet proteins in the mature CNS. J Neurosci. 2006;26:10006–10019. doi: 10.1523/JNEUROSCI.2580-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Williams RC, Jr, Sugiura K, Tan EM. Antibodies to microtubule-associated protein 2 in patients with neuropsychiatric systemic lupus erythematosus. Arthritis Rheum. 2004;50:1239–1247. doi: 10.1002/art.20156. [DOI] [PubMed] [Google Scholar]
- 67.Senecal JL, Raymond Y. The pathogenesis of neuropsychiatric manifestations in systemic lupus erythematosus: a disease in search of autoantibodies, or autoantibodies in search of a disease? J Rheumatol. 2004;31:2093–2098. [PubMed] [Google Scholar]
- 68.Fliegner KH, Kaplan MP, Wood TL, Pintar JE, Liem RK. Expression of the gene for the neuronal intermediate filament protein alpha-internexin coincides with the onset of neuronal differentiation in the developing rat nervous system. J Comp Neurol. 1994;342:161–173. doi: 10.1002/cne.903420202. [DOI] [PubMed] [Google Scholar]
- 69.Lee MK, Cleveland DW. Neuronal intermediate filaments. Annu Rev Neurosci. 1996;19:187–217. doi: 10.1146/annurev.ne.19.030196.001155. [DOI] [PubMed] [Google Scholar]
- 70.Arnold SE, Trojanowski JQ. Human fetal hippocampal development: II. The neuronal cytoskeleton. J Comp Neurol. 1996;367:293–307. doi: 10.1002/(SICI)1096-9861(19960401)367:2<293::AID-CNE10>3.0.CO;2-S. [DOI] [PubMed] [Google Scholar]
- 71.Athlan ES, Mushynski WE. Heterodimeric associations between neuronal intermediate filament proteins. J Biol Chem. 1997;272:31073–31078. doi: 10.1074/jbc.272.49.31073. [DOI] [PubMed] [Google Scholar]
- 72.Cairns NJ, Grossman M, Arnold SE, Burn DJ, Jaros E, et al. Clinical and neuropathologic variation in neuronal intermediate filament inclusion disease. Neurology. 2004;63:1376–1384. doi: 10.1212/01.wnl.0000139809.16817.dd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Ching GY, Chien CL, Flores R, Liem RK. Overexpression of alpha-internexin causes abnormal neurofilamentous accumulations and motor coordination deficits in transgenic mice. J Neurosci. 1999;19:2974–2986. doi: 10.1523/JNEUROSCI.19-08-02974.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Ching GY, Liem RK. Structure of the gene for the neuronal intermediate filament protein alpha-internexin and functional analysis of its promoter. J Biol Chem. 1991;266:19459–19468. [PubMed] [Google Scholar]
- 75.Lee MK, Xu Z, Wong PC, Cleveland DW. Neurofilaments are obligate heteropolymers in vivo. J Cell Biol. 1993;122:1337–1350. doi: 10.1083/jcb.122.6.1337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Beaulieu JM, Robertson J, Julien JP. Interactions between peripherin and neurofilaments in cultured cells: disruption of peripherin assembly by the NF-M and NF-H subunits. Biochem Cell Biol. 1999;77:41–45. [PubMed] [Google Scholar]
- 77.Shea TB, Beermann ML. Neuronal intermediate filament protein alpha-internexin facilitates axonal neurite elongation in neuroblastoma cells. Cell Motil Cytoskeleton. 1999;43:322–333. doi: 10.1002/(SICI)1097-0169(1999)43:4<322::AID-CM5>3.0.CO;2-B. [DOI] [PubMed] [Google Scholar]
- 78.Chien CL, Liu TC, Ho CL, Lu KS. Overexpression of neuronal intermediate filament protein alpha-internexin in PC12 cells. J Neurosci Res. 2005;80:693–706. doi: 10.1002/jnr.20506. [DOI] [PubMed] [Google Scholar]
- 79.Barry DM, Millecamps S, Julien JP, Garcia ML. New movements in neurofilament transport, turnover and disease. Exp Cell Res. 2007;313:2110–2120. doi: 10.1016/j.yexcr.2007.03.011. [DOI] [PubMed] [Google Scholar]
- 80.Cairns NJ, Uryu K, Bigio EH, Mackenzie IR, Gearing M, et al. alpha-Internexin aggregates are abundant in neuronal intermediate filament inclusion disease (NIFID) but rare in other neurodegenerative diseases. Acta Neuropathol. 2004;108:213–223. doi: 10.1007/s00401-004-0882-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Lalonde R, Strazielle C. Neurobehavioral characteristics of mice with modified intermediate filament genes. Rev Neurosci. 2003;14:369–385. doi: 10.1515/revneuro.2003.14.4.369. [DOI] [PubMed] [Google Scholar]
- 82.Lariviere RC, Julien JP. Functions of intermediate filaments in neuronal development and disease. J Neurobiol. 2004;58:131–148. doi: 10.1002/neu.10270. [DOI] [PubMed] [Google Scholar]
- 83.Alarcon-Segovia D, Ruiz-Arguelles A, Fishbein E. Antibody to nuclear ribonucleoprotein penetrates live human mononuclear cells through Fc receptors. Nature. 1978;271:67–69. doi: 10.1038/271067a0. [DOI] [PubMed] [Google Scholar]
- 84.Alarcon-Segovia D, Ruiz-Arguelles A, Llorente L. Broken dogma: penetration of autoantibodies into living cells. Immunol Today. 1996;17:163–164. doi: 10.1016/s0167-5699(96)90258-3. [DOI] [PubMed] [Google Scholar]
- 85.Zack DJ, Stempniak M, Wong AL, Taylor C, Weisbart RH. Mechanisms of cellular penetration and nuclear localization of an anti-double strand DNA autoantibody. J Immunol. 1996;157:2082–2088. [PubMed] [Google Scholar]
- 86.Williams RC, Jr, Peen E. Apoptosis and cell penetration by autoantibody may represent linked processes. Clin Exp Rheumatol. 1999;17:643–647. [PubMed] [Google Scholar]
- 87.Cleveland DW, Rothstein JD. From Charcot to Lou Gehrig: deciphering selective motor neuron death in ALS. Nat Rev Neurosci. 2001;2:806–819. doi: 10.1038/35097565. [DOI] [PubMed] [Google Scholar]
- 88.Robertson J, Kriz J, Nguyen MD, Julien JP. Pathways to motor neuron degeneration in transgenic mouse models. Biochimie. 2002;84:1151–1160. doi: 10.1016/s0300-9084(02)00025-1. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Gene information, ORF sequence information, and vector information of EX-Z0330-B01.
(0.06 MB DOC)
Screening anti-neuronal aAbs in the sera/CSF of NPSLE and SLE control patients by indirect immunofluorescence. NPSLE serum from a patients with severe cerebralitis and myelitis was identified by its reactivity to all species. All sera/CSF of SLE probes are ANA positive without cytoplasmic staining against Hep2 cells, and neither have anti-ribsomal P antibodies. Scale bar = 50 µm.
(2.09 MB TIF)
An experimental group (INA immunized, LPS-treated, n = 16) and two control groups (normal, n = 10 and INA immunized alone, n = 12) were studied. Neurological dysfunctions including exploratory behavior and motor coordination, was observed in INA+LPS mice in open field activity and beam walking tasks.
(0.20 MB TIF)