Abstract
Purpose: health-related quality of life (HRQOL) is an important psycho-social characteristic which may impact an individual’s ability to manage their chronic disease. We examined the association between HRQOL and antihypertensive medication adherence in older adults.
Methods: participants were part of a cohort study of older adults enrolled in a managed care organisation and treated for hypertension (n = 2,180). Physical and Mental Component Summary Scores (PCS and MCS) of HRQOL were assessed using the RAND Medical Outcomes Study 36-item tool. Adherence to antihypertensive medication was assessed with the eight-item Morisky Medication Adherence Scale.
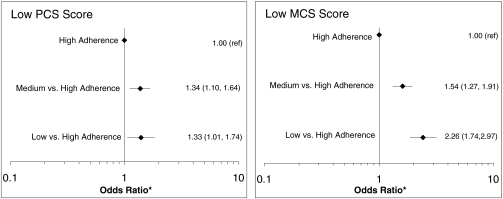
Results: the mean age of participants was 75.0 ± 5.6 years, 69.3% were white, 58.5% were women and 14.1% had low antihypertensive medication adherence. Low HRQOL scores were associated with lower levels of antihypertensive medication adherence in older adults. After adjustment for covariates, those with low PCS and MCS scores were 1.33 (95% CI 1.01, 1.74) and 2.26 (95% CI 1.74, 2.97) times more likely, respectively, to have low antihypertensive medication adherence than those with PCS and MCS scores in the top 2 tertiles.
Conclusions: low HRQOL may be an important barrier to achieving high medication adherence.
Keywords: HRQOL, medication adherence, hypertension, older adults, elderly
Introduction
Hypertension is a prevalent and often asymptomatic chronic disease which affects close to 70 million adults in the United States [1, 2]. Despite effective medical therapy and evidence-based treatment guidelines for managing high blood pressure, uncontrolled hypertension remains common [3, 4]. Low antihypertensive medication adherence has been proposed as an important barrier to achieving hypertension control. Demographic, treatment, clinical and behavioural factors have been shown to be associated with medication adherence, and previous studies have indicated that psycho-social factors are important determinants of antihypertensive medication adherence in older adults [5–9]. However, the impact of an individual’s physical and mental quality of life on their adherence to antihypertensive medications is less clear, particularly among older adults.
Results from prior studies examining the relationship between health-related quality of life (HRQOL) and antihypertensive medication adherence have been conflicting [5, 10, 11]. This may be due to variation in both the techniques used to measure HRQOL and the study populations examined [12]. To better understand the relationship between mental and physical HRQOL and medication adherence in older adults treated for hypertension, data were analysed from the baseline survey of the Cohort Study of Medication Adherence among Older Adults (CoSMO), a study of community-dwelling adults 65 years of age and older.
Methods
Study population and timeline
The primary goal of CoSMO is to investigate factors that influence adherence to antihypertensive medication in older adults; the study design and baseline characteristics have been published previously [13]. In brief, adults, 65 years and older with essential hypertension, were randomly selected from the roster of a large managed care organisation (MCO) in Southeastern Louisiana. Recruitment was conducted from 21 August 2006 to 30 September 2007: 7,020 patients were identified for screening, 3,545 met the eligibility criteria after a telephone screening and 2,194 were enrolled (31% of those identified for screening and 62% of those deemed eligible after telephone contact). For the current analysis, 14 participants who reported their race to be other than white or black were excluded. CoSMO was approved by the Ochsner Clinic Foundation’s Institutional Review Board and the privacy board of Humana, Inc., and all participants provided informed consent [13].
Study measures
Trained research staff administered the baseline CoSMO survey over the telephone and the interview lasted 30–45 min. Specific to this analysis, the survey included assessment of socio-demographic and clinical factors in addition to medication adherence, HRQOL and reduction in prescribed antihypertensive medication use due to cost. In addition, information regarding co-morbid conditions and number and frequency of antihypertensive medications filled was obtained from the administrative and pharmacy databases of the MCO.
Patient characteristics
Socio-demographic and clinical characteristics obtained by participant self-report included marital status, age, race, co-morbid conditions, educational attainment, height and weight and duration of hypertension. To assess whether participants reduced their antihypertensive medication use due to cost, we included a question, ‘In the last year, have you ended up taking less antihypertensive medication than was prescribed because of the cost?’. Body mass index was calculated as weight in kilogrammes divided by height in metres squared, and age was dichotomised into two groups (65–74 vs. ≥75 years) with approximately half of the study population in each group. Marital status was collapsed into two categories: married (currently married or co-habitating) and not married (currently divorced, separated, widowed or never married). The number of antihypertensive drug classes that participants were taking in the year prior to their baseline interview was extracted from pharmacy fill data, and the Charlson co-morbidity index score was constructed from administrative claims data [14].
HRQOL
HRQOL measures the extent to which a person’s day-to-day life is affected by their health and includes the physical, emotional and social impact of disease [15]. We assessed HRQOL using the RAND Medical Outcomes Study 36-item tool. The tool is comprised of 36 questions that measure four physical health subscales (physical functioning, role limitations due to physical health problems, bodily pain, general health perception) and four mental health subscales (social functioning, role limitations due to emotional problems, mental health and vitality) and has previously been used to measure HRQOL in similar populations [16, 17]. Physical and Mental Component Summary Scores (PCS and MCS, respectively) were created using standard norm-based scoring methods [16]. Scores on each of the eight subscales were calculated and standardised to the US population. Per established coding guidelines, seven participants were excluded from the analysis because they answered <50% of items on any of the eight subscales. Subscales were then weighted and aggregated to create PCS and MCS summary scores, which were standardised to a mean of 50 and a standard deviation of 10 in the normal US population. Lower scores on HRQOL scales indicate limitations in the ability to perform daily activities and work due to reduced physical or emotional functioning, interference with normal social activities, feelings of nervousness and depression, body pain that is severe and limiting, poor perception of personal health and persistent feelings of fatigue. Because no previously established cutpoints for defining low PCS and MCS scores are available, participants were categorised as having low PCS and low MCS if their score was in the lowest tertile of the distribution for the current study population (≤38.2 and ≤53.2 for PCS and MCS, respectively).
Medication adherence
The primary outcome for the current analysis was self-reported medication adherence, which was assessed using the eight-item Morisky Medication Adherence Scale (MMAS-8). The MMAS has been determined to be reliable [19] and significantly associated with blood pressure control (P < 0.05) in individuals with hypertension (i.e. low adherence levels were associated with lower rates of blood pressure control) [13, 19] and to have high concordance with antihypertensive medication pharmacy fill rates [18]. Scores on the MMAS can range from zero to eight, with MMAS scores of <6, 6 to <8 and 8 reflecting low, medium and high adherence, respectively [18, 19].
The medication possession ratio (MPR) was used in sensitivity analyses to provide an objective measure of adherence to antihypertensive medication. Data for the MPR was acquired from pharmacy fill data (i.e. the number of prescribed pills that an individual filled from a pharmacy) of the MCO in the year prior to the survey date. The MPR was calculated as the sum of the days’ supply of prescribed antihypertensive medications obtained between the first and last pharmacy fill, divided by the total number of days in that period. The MPR was calculated for each antihypertensive medication class and averaged across all classes to assign a single MPR to each participant. MPR values of less than 0.8, a previously published cutpoint, were designated as non-persistent [13, 18, 20, 21].
Statistical analysis
Characteristics of CoSMO participants were calculated for those with and without low MCS and PCS Scores and compared using chi-square tests. Mean HRQOL values on the eight mental and physical subscales were calculated for each of the MMAS-8 antihypertensive medication adherence groups (low, medium and high), using analysis of covariance (ANCOVA) to adjust for covariates. Trends in HRQOL values across groups were then assessed by ANCOVA, modelling medication adherence groups as a continuous ordinal variable. The relationships between dichotomised PCS or MCS scores and MMAS-8 levels were assessed using separate multinomial logistic regression models (using high antihypertensive medication adherence as the reference group). Sensitivity analyses were conducted to determine the association of low PCS and MCS scores with the outcome of non-persistent MPR. For MPR analyses, associations were determined using logistic regression models with adjustment for covariates. Subgroup analyses were also performed to determine the consistency of results across age, race and gender groups. All models were adjusted for age, gender, race, education and marital status. Analyses were performed using SAS 9.1 (Cary, NC).
Results
The mean age of CoSMO participants was 75.0 ± 5.6 years, 69.3% were white, 58.5% were women, 56.7% were married and 79.3% had a high school education. Also, 63.0% had been diagnosed with hypertension for 10 or more years, 49.6% had two or more co-morbid conditions and 51.2% had filled three or more classes of antihypertensive medication in the year prior to their baseline survey. Using published MMAS-8 cutpoints, 14.1% of participants had low, 34.2% had medium and 51.7% had high antihypertensive medication adherence.
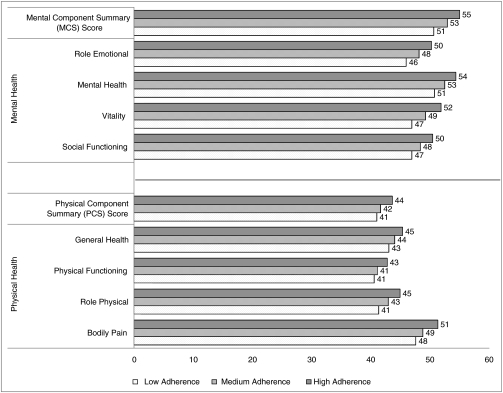
Table 1 shows characteristics of CoSMO participants by Physical and Mental Component Summary Scores. Participants with low PCS scores were more likely to be women, have lived with hypertension for 10 or more years, to be filling three or more classes of antihypertensive medications, to be overweight or obese, to have two or more co-morbid conditions, to report reducing antihypertensive medication use due to cost and less likely to be a high school graduate. Participants with low MCS scores were more likely to be women, to be filling three or more classes of antihypertensive medications, to have two or more co-morbid conditions and to report reducing antihypertensive medication use due to cost, but less likely to be white, to be married and to be a high school graduate. Figure 1 shows the adjusted mean HRQOL values by MMAS-8 category for the four physical health subscales, four mental health subscales and the aggregate MCS and PCS scales. On each subscale, mean HRQOL scores were highest among participants with high medication adherence and lowest among those with low medication adherence (for PCS, MCS and each subscale, P < 0.005 for the trend across adherence levels).
Table 1.
Characteristics of CoSMO participants by Physical and Mental Component Summary scores
| PCS score | MCS score | |||
|---|---|---|---|---|
| Lowan = 717 | Not lown = 1,456 | Lowan = 717 | Not lown = 1,456 | |
| ≥75 years old, % | 51.2 | 47.8 | 51.5 | 47.7 |
| Women, % | 63.3** | 56.0 | 63.9*** | 55.8 |
| White, % | 69.0 | 69.5 | 63.9*** | 72.1 |
| Married, % | 54.1 | 58.2 | 51.9** | 59.3 |
| High school graduate, % | 73.9*** | 82.0 | 74.2*** | 81.9 |
| Reduced antihypertensive medication use due to cost | 4.9* | 2.9 | 7.5*** | 1.6 |
| Hypertension duration ≥10 years, % | 67.9** | 60.7 | 62.5 | 63.3 |
| 3 or more classes of hypertensive drugs, % | 61.1*** | 46.1 | 55.2** | 49.1 |
| Co-morbid index score ≥2, % | 64.2*** | 42.5 | 55.5*** | 46.8 |
| Body mass index: ≥25 kg/m2, % | 82.9*** | 73.6 | 77.1 | 76.4 |
Participants were categorised as having low PCS and low MCS if their scores were in the lowest tertile of the distribution for the study population (≤38.2 and ≤53.2, respectively).
PCS, Physical Component Summary Score; MCS, Mental Component Summary Score.
*P < 0.05, **P < 0.01, ***P < 0.001.
Figure 1.
Mean HRQOL scores by antihypertensive medication adherence level.
Among participants with low PCS scores, 15.8% had low and 37.7% had medium antihypertensive medication adherence, compared to 13.4 and 32.5% of those without low PCS scores (P = 0.003). For participants with low MCS scores, 20.2% had low and 38.2% had medium antihypertensive medication adherence, compared to 11.2 and 32.2% of those without low MCS scores (P < 0.001). After adjustment for socio-demographic characteristics and reduction in antihypertensive medication use due to cost, having low PCS and low MCS scores were associated with lower antihypertensive medication adherence (Figure 2). Results of subgroup analyses showed that associations between HRQOL and antihypertensive medication adherence were consistent across race, gender and age groups (data not shown).
Figure 2.
Odds ratios for low and medium antihypertensive medication adherence associated with low PCS and MCS scores.
Results were also consistent when analyses were repeated using non-persistent MPR as the medication adherence outcome. Among participants with low PCS scores, 33.3% had a non-persistent MPR, compared to 24.0% of those without low PCS scores (P < 0.001). Among participants with low MCS scores, 30.4% had a non-persistent MPR, compared to 25.3% of those without low MCS scores (P < 0.05). After multivariable adjustment, those with low PCS and MCS scores were 1.25 (95% CI 1.01, 1.54) and 1.38 (95% CI 1.12, 1.71) times more likely, respectively, to have a non-persistent MPR than those without low MCS and PCS scores.
Discussion
In the current study, participants with low PCS and MCS HRQOL scores were more likely to have low or medium antihypertensive medication adherence, even after adjusting for age, race, education, gender and marital status. The associations remained consistent in subgroup analyses and when the outcome was defined using both a self-report adherence measure and an adherence measure based on pharmacy fill data.
These results add to the literature in that they reveal a relationship between physical and mental measures of HRQOL and antihypertensive medication adherence in older adults. Previous studies assessing the relationship between HRQOL and medication adherence have produced conflicting results. In a sample of geriatric patients, no relationship was detected between HRQOL and self-reported antihypertensive medication adherence [10]. In a separate sample of hypertensive adults ages 35–80 years, weak negative correlations were identified between self-reported medication adherence and HRQOL [11]. A third study of hypertensive patients ages 25–92 showed that adults with lower MCS scores had correspondingly lower adherence to their antihypertensive medications; however, this relationship was not significant in adjusted analyses [5]. Our study suggests that an association exists between low HRQOL and low antihypertensive medication adherence in a large sample of community-dwelling adults older than 65 years.
HRQOL may be associated with low antihypertensive medication adherence for numerous reasons including patients’ attitudes towards taking medications and their psycho-social well-being [21–24]. The exact mechanism through which HRQOL is associated with medication adherence is unknown; however, HRQOL appears to be part of a complex web of psycho-social characteristics which can negatively impact a patient’s ability to manage their chronic disease. Previous studies conducted among patients with diabetes have linked HRQOL to factors identified as precursors to medication adherence, including patients’ beliefs that they are able to carry out a behaviour (self-efficacy) [25], their attitudes and knowledge about disease treatment [26], their perceived level of competence [25] and their overall outlook on life (optimism) [27]. Further research is needed to understand the mechanisms through which HRQOL affects adherence to antihypertensive medications and ultimately cardiovascular health.
This analysis showed that both physical and mental measures of HRQOL are correlated with antihypertensive medication adherence, with stronger associations seen in the mental, social and emotional domains. These results correspond with those of previous studies which identify clinical depression and the presence of depressive symptoms as important correlates of antihypertensive medication adherence in patients with chronic disease [7–9]. In the CoSMO sample, participants who reported that they felt tired and worn out all the time (assessed via the vitality subscale), had frequent interference with normal social activities due to emotional problems (assessed via the social subscale), experienced problems with work or daily activities due to emotional problems (assessed via the emotion role functioning subscale) and constant feelings of nervousness and depression (assessed via the mental subscale) had increased odds of lower antihypertensive medication adherence. These results suggest that older adults with hypertension who have worse emotional well-being may also have lower adherence to antihypertensive medications.
Study limitations and strengths
The results presented are observational. Because the data are self-reported, there is potential for misclassification. Also, the cross-sectional nature of these analyses does not allow the direction of the associations to be determined. The study population was a selected one: recruitment of participants was restricted to English-speaking older adults with health insurance living in one region of the US. Only 31% of patients in the MCO who were identified for screening agreed to enrol in the study (62% of those deemed to be eligible after telephone contact), thus, there is the possibility that selection bias may be present.
This study has many strengths, including its large sample size and broad data collection. Also, because the CoSMO sample is limited to community-dwelling older adults in an MCO, confounding by access to care and health insurance is reduced. The inclusion of both self-reported medication adherence behaviour and pharmacy fill data allowed us to confirm our results using objective measures. The consistency of our findings using self-report and pharmacy fill data to assess adherence is noteworthy. These findings reduce the possibility that the relationship between low HRQOL and low antihypertensive medication adherence using MMAS-8 is due to reporting bias or chance. Scores on mental and physical HRQOL scales in this study were comparable to those reported in other populations of older adults. Specifically, trends in norm-based scores among participants in the CoSMO cohort were similar to those from the Medicare Health Outcomes Study (HOS), a large cohort of 177,714 older (65+) adults enrolled in a Medicare Managed Care Program [28]. In both the HOS cohort and in the CoSMO cohort, scores on scales measuring physical health were consistently lower than the general population means of 50, and scores on scales measuring mental and emotional health were closer to US population means of 50. This is not surprising, given that previous studies have shown that physical HRQOL declines with increased prevalence of chronic disease and advanced age [10, 29]. Mental HRQOL has been shown to remain more stable — even with advancing age and increased chronic conditions [29].
Conclusions
In the current analysis, older adults with low physical and mental HRQOL were more likely to have lower adherence to antihypertensive medications, whether adherence was measured by self-report or pharmacy fill. HRQOL may be an important factor in understanding antihypertensive medication adherence, with mental, emotional and social domains having the greatest impact. Further research is needed to clarify the longitudinal relationship between HRQOL, antihypertensive medication adherence and health outcomes in older adults and to determine whether improvements in quality of life can lead to corresponding increases in antihypertensive medication adherence and improvements in cardiovascular health outcomes.
Key points
Low HRQOL scores were associated with lower levels of antihypertensive medication adherence in a cohort of older adults.
The mental, social and emotional HRQOL domains had the greatest impact on adherence to prescribed antihypertensive medications.
Associations remained consistent when adherence was measured using both pharmacy fill data and self-report.
Acknowledgments
Use of MMAS-8: Permission for use of MMAS-8 is required. Licensure agreement is available from Donald E. Morisky, ScD, ScM, MSPH, Department of Community Health Sciences, UCLA School of Public Health, 650 Charles E. Young Drive South, Los Angeles, CA 90095-1772.
Conflicts of interest
There are no conflict of interests to report.
Funding
This work was supported by the National Institute on Aging [grant number R01 AG022536, Krousel-Wood—principal investigator]. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Aging or the National Institutes of Health.
References
- 1.Chobanian AV, Bakris GL, Black HR, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289:2560–72. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 2.Ong KL, Cheung BM, Man YB, Lau CP, Lam KS. Prevalence, awareness, treatment, and control of hypertension among United States adults 1999–2004. Hypertension. 2007;49:69–75. doi: 10.1161/01.HYP.0000252676.46043.18. [DOI] [PubMed] [Google Scholar]
- 3.Garfield FB, Caro JJ. Compliance and hypertension. Curr Hypertens Rep. 1999;1:502–6. doi: 10.1007/s11906-996-0022-y. [DOI] [PubMed] [Google Scholar]
- 4.Haynes RB, McDonald HP, Garg AX. Helping patients follow prescribed treatment: clinical applications. JAMA. 2002;288:2880–3. doi: 10.1001/jama.288.22.2880. [DOI] [PubMed] [Google Scholar]
- 5.Trivedi RB, Ayotte B, Edelman D, Bosworth HB. The association of emotional well-being and marital status with treatment adherence among patients with hypertension. J Behav Med. 2008;31:489–97. doi: 10.1007/s10865-008-9173-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.DiMatteo MR, Lepper HS, Croghan TW. Depression is a risk factor for noncompliance with medical treatment: meta-analysis of the effects of anxiety and depression on patient adherence. Arch Intern Med. 2000;160:2101–7. doi: 10.1001/archinte.160.14.2101. [DOI] [PubMed] [Google Scholar]
- 7.Wang PS, Bohn RL, Knight E, Glynn RJ, Mogun H, Avorn J. Noncompliance with antihypertensive medications: the impact of depressive symptoms and psychosocial factors. J Gen Intern Med. 2002;17:504–11. doi: 10.1046/j.1525-1497.2002.00406.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kim MT, Han HR, Hill MN, Rose L, Roary M. Depression, substance use, adherence behaviors, and blood pressure in urban hypertensive black men. Ann Behav Med. 2003;26:24–31. doi: 10.1207/S15324796ABM2601_04. [DOI] [PubMed] [Google Scholar]
- 9.Schoenthaler A, Ogedegbe G, Allegrante JP. Self-efficacy mediates the relationship between depressive symptoms and medication adherence among hypertensive African Americans. Health Educ Behav. 2009;36:127–37. doi: 10.1177/1090198107309459. [DOI] [PubMed] [Google Scholar]
- 10.Pippalla RS, Chinburapa V, Duval R, Akula RS. Interrelationships of quality of life, compliance, clinical outcomes and life satisfaction: a cross-sectional study on hypertensive geriatrics. J Clin Pharm Ther. 1997;22:357–69. doi: 10.1111/j.1365-2710.1997.tb00019.x. [DOI] [PubMed] [Google Scholar]
- 11.Cote I, Farris K, Feeny D. Is adherence to drug treatment correlated with health-related quality of life? Qual Life Res. 2003;12:621–33. doi: 10.1023/a:1025180524614. [DOI] [PubMed] [Google Scholar]
- 12.Coyne KS, Davis D, Frech F, Hill MN. Health-related quality of life in patients treated for hypertension: a review of the literature from 1990 to 2000. Clin Ther. 2002;24:142–69. doi: 10.1016/s0149-2918(02)85012-3. [DOI] [PubMed] [Google Scholar]
- 13.Krousel-Wood MA, Muntner P, Islam T, Morisky DE, Webber LS. Barriers to and determinants of medication adherence in hypertension management: perspective of the cohort study of medication adherence among older adults. Med Clin North Am. 2009;93:753–69. doi: 10.1016/j.mcna.2009.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–83. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 15.Guyatt GH, Feeny DH, Patrick DL. Measuring health-related quality of life. Ann Intern Med. 1993;118:622–9. doi: 10.7326/0003-4819-118-8-199304150-00009. [DOI] [PubMed] [Google Scholar]
- 16.Hays RD, Sherbourne CD, Mazel RM. The RAND 36-Item Health Survey 1.0. Health Econ. 1993;2:217–27. doi: 10.1002/hec.4730020305. [DOI] [PubMed] [Google Scholar]
- 17.Krousel-Wood MA, Re R. Health status assessment in a hypertension section of an internal medicine clinic. Am J Med Sci. 1994;308:211–7. doi: 10.1097/00000441-199430840-00001. [DOI] [PubMed] [Google Scholar]
- 18.Krousel-Wood M, Islam T, Webber LS, Re RN, Morisky DE, Muntner P. New medication adherence scale versus pharmacy fill rates in seniors with hypertension. Am J Manag Care. 2009;15:59–66. [PMC free article] [PubMed] [Google Scholar]
- 19.Morisky DE, Ang A, Krousel-Wood M, Ward HJ. Predictive validity of a medication adherence measure in an outpatient setting. J Clin Hypertens (Greenwich) 2008;10:348–54. doi: 10.1111/j.1751-7176.2008.07572.x. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 20.Sikka R, Xia F, Aubert RE. Estimating medication persistency using administrative claims data. Am J Manag Care. 2005;11:449–57. [PubMed] [Google Scholar]
- 21.Krousel-Wood M, Thomas S, Muntner P, Morisky D. Medication adherence: a key factor in achieving blood pressure control and good clinical outcomes in hypertensive patients. Curr Opin Cardiol. 2004;19:357–62. doi: 10.1097/01.hco.0000126978.03828.9e. [DOI] [PubMed] [Google Scholar]
- 22.Holzemer WL, Corless IB, Nokes KM, et al. Predictors of self-reported adherence in persons living with HIV disease. AIDS Patient Care STDS. 1999;13:185–97. doi: 10.1089/apc.1999.13.185. [DOI] [PubMed] [Google Scholar]
- 23.Sung JC, Nichol MB, Venturini F, Bailey KL, McCombs JS, Cody M. Factors affecting patient compliance with antihyperlipidemic medications in an HMO population. Am J Manag Care. 1998;4:1421–30. [PubMed] [Google Scholar]
- 24.Dosse C, Cesarino CB, Martin JF, Castedo MC. Factors associated to patients’ noncompliance with hypertension treatment. Rev Lat Am Enfermagem. 2009;17:201–6. doi: 10.1590/s0104-11692009000200010. [DOI] [PubMed] [Google Scholar]
- 25.Williams GC, Patrick H, Niemiec CP, et al. Reducing the health risks of diabetes: how self-determination theory may help improve medication adherence and quality of life. Diabetes Educ. 2009;35:484–92. doi: 10.1177/0145721709333856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Martinez YV, Prado-Aguilar CA, Rascon-Pacheco RA, Valdivia-Martinez JJ. Quality of life associated with treatment adherence in patients with type 2 diabetes: a cross-sectional study. BMC Health Serv Res. 2008;8:164. doi: 10.1186/1472-6963-8-164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rose M, Fliege H, Hildebrandt M, Schirop T, Klapp BF. The network of psychological variables in patients with diabetes and their importance for quality of life and metabolic control. Diabetes Care. 2002;25:35–42. doi: 10.2337/diacare.25.1.35. [DOI] [PubMed] [Google Scholar]
- 28.Gandek B, Sinclair SJ, Kosinski M, Ware JE., Jr Psychometric evaluation of the SF-36 health survey in Medicare managed care. Health Care Financ Rev. 2004;25:5–25. [PMC free article] [PubMed] [Google Scholar]
- 29.Hopman WM, Harrison MB, Coo H, Friedberg E, Buchanan M, VanDenKerkhof EG. Associations between chronic disease, age and physical and mental health status. Chronic Dis Can. 2009;29:108–16. [PubMed] [Google Scholar]