Abstract
Adenovirus (Ad) based vectors have been utilized in human gene transfer clinical trials since 1993. Unfortunately, innate immune responses directed against the Ad capsid and/or its genetic cargo can significantly limit the usage of Ad vectors. Previous studies have demonstrated that several signaling pathways are triggered by Ads, inclusive of TLR dependent pathways. The G- protein coupled receptor adaptors β-arrestin1 (β-Arr1) and β-arrestin2 (β-Arr2) are known to have pivotal roles in regulating TLR4 triggered signaling and inflammatory responses. In this study, we examined the role of β-arrestins in Ad5 vector-induced inflammatory responses. Our studies reveal that both β-arrestins are capable of modulating Ad5-vector-induced inflammatory responses in vivo and in vitro. Importantly, our studies divulge another level of complexity to these responses, as our results demonstrate β-Arr1 to be a positive regulator, and β-Arr2 a negative regulator of Ad5 induced innate immune responses. These data may allow gene therapy biologists to more accurately study the mechanisms underlying Ad5 vector induced immune responses, and may also direct future efforts to modulate these mechanisms to improve the safety and/or efficacy of this important gene transfer vector.
Keywords: innate immunity, liver, recombinant Adenovirus, β-Arrestin-1, β-Arrestin-2
Introduction
β-Arrestin-1 and -2 (β-Arr1 and 2) were originally discovered to play a major role in G protein coupled receptor desensitization, due to their ability to bind to phosphorylated G protein coupled receptors and sterically block their ability to signal downstream (DeWire et al., 2007). Subsequent studies revealed more versatile roles of β-Arr1 (arrestin-2) and β-Arr2 (arrestin-3), including broader regulation of cell signaling in general, serving as scaffolds, as well as having roles in transcriptional regulation (DeWire et al., 2007). Recent studies demonstrate β-arrestins as negative regulators of TLR-stimulated NFκB and ERK signaling pathways in macrophages and fibroblasts (Parameswaran et al., 2006; Wang et al., 2006). Consistent with this role of β-arrestins, Wang et. al. showed that deficiency of β-Arr2 significantly enhances endotoxic mortality in mice (Wang et al., 2006). In contrast to these studies, Fan et. al. (Fan et al., 2007) demonstrated differential effects of β-Arr1 and -2 in lipopolysaccharide signaling in mouse embryo fibroblasts, suggesting that β-arrestin’s effect on TLR signaling might depend on the cellular context. Although a role for β-arrestins has been established using selective TLR ligands, their role in microbial infections (which activate multiple TLRs) is not known.
Innate immune responses associated with systemic injection of Adenovirus (Ad) based vectors remain to be one of the most important obstacles limiting the usage of these vectors in numerous clinically important applications. For example, systemic administration of Ads results in acute thrombocytopenia (Kiang et al., 2006; Wolins et al., 2003), activation of the complement, TLR and IFN systems, a robust cytokine release into the circulation sometimes referred to as a “cytokine storm” (Appledorn et al., 2008b; Appledorn et al., 2008c; Kiang et al., 2006; Seregin et al., 2009a), activation of endothelial cells (Liu et al., 2003) as well as massive inductions of pro-inflammatory gene expression in multiple tissues, including the liver, spleen and lung (Appledorn et al., 2008a; Barrington et al., 2001; Cichon et al., 2001; Hartman et al., 2007b; Kiang et al., 2006; Kirschfink, 1997; Makrides, 1998). Therefore, understanding the mechanisms mediating Ad induction of these processes may allow for focused efforts to interfere with these mechanisms to foster improved safety and/or efficacy of Ad mediated gene transfer applications. Because TLRs significantly modulate Ad vector responses, and since β-arrestins play a crucial role in TLR signaling, in this study we analyzed the role of β-arr-1 and -2 in Ad5-induced innate immune responses both in vitro and in vivo. Our results confirm that multiple Ad5 induced innate immune responses are mediated by β-arrestin functionality. Moreover β-Arr1 and β-Arr2 differentially mediate Ad5 induced innate responses, having somewhat opposite functions: β-Arr2 clearly down-regulates Ad5 induced gene induction and cytokine responses, whereas β-Arr1 enhances portions of these responses.
Materials and Methods
Adenovirus vector production and characterization
A first-generation, human Adenovirus type 5 derived replication deficient vector (deleted for the E1 genes) encoding β-galactosidase (LacZ) as a transgene (Ad5-LacZ) was used in this study. Virus construction, propagation and purification were performed as previously described (Hodges et al., 2001; Ng and Graham, 2002). Briefly, a number of serial passages on HEK293 cells allowed high titer purification of Ad5-LacZ by sequential, cesium chloride density gradient centrifugations. Purified virus was dialyzed against 10 mM Tris (pH 8.0) and stored in 1% sucrose, 1 X PBS at −80° C until use. Viral particle (vp) and transducing unit titers (bfu/ml) were determined as previously described, and were 2.6 × 1012 vp/ml and 1.8 × 1011 bfu/ml respectively (Amalfitano et al., 1998; Kiang et al., 2006). The vp to bfu ration was ~14:1. Virus was found to be RCA free both by RCA PCR (E1 region amplification) and direct sequencing, methods as previously described (Hartman et al., 2007b). Ad5-LacZ have also been tested for the presence of bacterial endotoxin as previously described (Cotter et al., 2005) and was found to contain <0.1 EU per ml.
Peritoneal macrophages isolation and infection
Murine peritoneal macrophages were elicited by injection of 1 ml of sterile Brewer’s thioglycollate medium (4.05 g/100 ml; Sigma) into the peritoneal cavity of C57BL/6 WT, β-Arr1-KO or β-Arr2-KO mice. After 4 days, mice were euthanized. PBS (10 ml) was injected into the peritoneum, and lavage fluid was removed as previously described (Jia et al., 2006; Loniewski et al., 2008). Peritoneal cells were washed twice by centrifugation, resuspended in 10% fetal bovine serum (US origin, endotoxin tested (less than 0.3 EU/ml), heat inactivated, mycoplasma, virus and bacteriophage tested from Gibco/Invitrogen) supplemented RPMI-1640 medium (Gibco/Invitrogen) and then plated in 12-well plates and allowed to adhere to the wells for 8 h in 5% CO2 at 37 °C. Nonadherent cells were removed by two washes with fresh culture medium (RPMI supplemented with 0.5% FBS), and the remaining adherent peritoneal macrophages were used for the subsequent infection with 20,000 vp/cell of Ad5-LacZ. Perotineal macrophages were extracted from four WT mice, four β-Arr1-KO mice and six β-Arr2-KO mice and plated onto multiple wells at the concentration of 1.5×106 cells/well. For every time point independent wells were utilized: N=4 for WT and β-Arr1-KO, N=6 for β-Arr2-KO. Total media was collected at corresponding time point (6, 24 or 48 hpi) and stored at −80° C until use.
Animal procedures
Adult C57BL/6 mice were purchased from Jackson Laboratory (Bar Harbor, ME). β-arrestin-1 and -2 KO mice have been backcrossed to C57BL6 background for more than 10 generations and have been described previously (Rajagopal et al., 2006). They were kindly provided by Dr. Robert Lefkowitz (Duke University). The Ad vector was injected intravenously (via the retro-orbital sinus) into 8–10 week old male C57BL/6 mice after performing proper anesthesia with isofluorane. A total of 0.75 × 1011 vp in 200 μl of PBS was injected per mouse. For both β-Arr and β-Arr2 four groups of mice were analyzed: Wild-type (WT) mice mock injected with PBS, β-Arr or β-Arr2-KO mice mock-injected with PBS, WT mice injected with Ad5-LacZ, and β-Arr or β-Arr2-KO mice injected with Ad5-LacZ. Control and experimental mice were sacrificed at 6 hours after mock or virus treatment: N=4 for virus injected groups, N=3 for Mock injected groups). Plasma and tissue samples were collected and processed in accordance with Michigan State University Institutional Animal Care and Use Committee. All procedures with recombinant Ads were performed under BSL-2, and all vector treated animals were maintained in ABSL-2 conditions. All animal procedures were reviewed and approved by the Michigan State University ORCBS and IACUC. Care for mice was provided in accordance with PHS and AAALAC standards.
Cytokines/Chemokines release measurement
To determine if β-Arr1 or β-Arr2 have any effect on Ad mediated release of cytokines/chemokines, Ad induced systemic release of pro-inflammatory cytokines/chemokines in murine plasma was measured in all groups of mice utilizing a multiplex bead array system. Plasma samples were collected at 1 and 6 hpi using heparinized capillary tubes and EDTA coated microvettes (Sarstedt, Nümbrecht, Germany) and centrifuged at 3400 rpm for 10 min to retrieve plasma samples. Samples were assayed for 7 independent cytokines/chemokines, which we have previously shown to be rapidly induced by systemically injected Ad vectors (MCP-1, KC, MIP-1β, IL-6, IL-12p40, G-SCF, RANTES) (Hartman et al., 2008; Hartman et al., 2007b; Kiang et al., 2006). All procedures were performed exactly as previously described according to manufacturer’s instructions (Bio-Rad, Hercules, CA) via Luminex 100 technology (Luminex, Austin, TX) (Hartman et al., 2007b). For in vitro experiments utilizing peritoneal macrophages, media collected at specified time points was assayed for the same 7 analytes as per manufacturer’s instructions.
β-Galactosidase enzyme activity and in situ X-gal staining
Ad mediated transduction of the transgene LacZ was measured both qualitatively and quantitatively. Liver sections from animals sacrificed at 6 hpi were embedded in Optimal Cutting Temperature (OCT) compound, frozen and stored at −80° C until use. Frozen samples were sectioned (7 μm sections) on a Leica cryostat and were fixed and in situ stained for LacZ expression using 5-bromo-4-chloro-3-indolyl-b-D-galactopyranoside (X-Gal, 1 mg/ml) as previously described (Everett et al., 2003). For quantitative assay, enzyme β-Galactosidase (β-gal) activity was measured in snap frozen liver and spleen samples. Tissue samples (<0.1 g) were homogenized and total protein concentrations were determined by bicinchoninic acid (BCA) assay, Pierce (Rockford, IL). β-gal activity was quantified by use of a β-gal activity detection kit (Stratagene, La Jolla, CA) according to manufacturer’s instructions and as previously described (Hu et al., 1999). Data were reported as Units of β-gal activity per μg of total protein.
qRT-PCR Analysis
To determine relative levels of a specific, liver or spleen derived RNA transcript, corresponding tissues were snap frozen in liquid nitrogen and RNA was harvested from ≈ 100mg of frozen tissue using TRIzol reagent (Invitrogen, Carlsbad, CA) per the manufacturer’s protocol. Following RNA isolation, reverse transcription was performed on 180ng of total RNA using SuperScript II (Invitrogen, Carlsbad, CA) reverse transcriptase and random hexamers (Applied Biosystems, Foster City, CA) per manufacturer’s protocol. RT reactions were diluted to a total volume of 80μl and 2μl was used as the template in the subsequent PCR reactions. Primers were designed using Primer Bank web based software (http://pga.mgh.harvard.edu/primerbank/). All primers used for amplification have been previously described (Appledorn et al., 2008a; Kiang et al., 2006; Seregin et al., 2009b). Q-PCR was carried out on an ABI 7900HT Fast Real-Time PCR System using SYBR Green PCR Mastermix (Applied Biosystems, Foster City, CA) in a 15μl reaction. All PCRs were subjected to the following procedure: 95.0° C for 10 minutes followed by 40 cycles of 95.0° C for 15 seconds followed by 60.0° C for 1 minute. The comparative Ct method was used to determine relative gene expression using GAPDH to standardize expression levels across all samples. Relative expression changes were calculated based on comparing experimental levels of a respective liver transcript to those quantified in liver samples derived from Mock injected animals.
Ad genome copy number per liver cell
To determine if β-Arrestins were critical for Ad localization into important tissues, the number of Ad genome copies per liver and spleen cell at different time points post-transduction was determined. Tissue samples (<0.1 g) were snap frozen in liquid nitrogen, crushed to a fine powder using a mortar and pestle and total DNA was extracted from as previously described (Hofstetter et al., 1997). Ad genome copy numbers were assessed using Real-Time PCR based quantification. PCR reactions were performed on an ABI 7900HT Fast Real-Time PCR System using the SYBR Green PCR Mastermix as described for qRT-PCR technique. Primers generated against the Ad5 Hexon gene have been previously described (Appledorn et al., 2008a). As an internal control for ensuring adequate DNA amplification, liver DNA was quantified using primers spanning the GAPDH gene. Standard curves were run in duplicate and consisted of 6 half-log dilutions using total genomic DNA, or DNA extracted from the purified Ad5-LacZ virus. These standard curves were used to determine the number of viral genomes present per liver cell. Melting curve analysis confirmed the quality and specificity of the PCR (data not shown).
Statistical analysis
Statistically significant differences in gene induction profiles were determined using One Way ANOVA with a Student-Newman-Keuls post-hoc test (p value < 0.05). Furthermore, a Two Way ANOVA with a Bonferroni post-hoc test was used to analyze the plasma levels of cytokines at 1 and 6 hpi (or media levels at 6, 24 and 48 hpi) to determine significant differences (p value < 0.05) between groups. For β-Gal activity and Ad genomes in mouse tissues, a two-tailed Student t-test was used to compare 2 groups of virus injected animals (p < 0.05). All graphs in this paper are presented as Mean of the average ± SD. GraphPad Prism software was utilized for statistical analysis.
Results
β-Arrestins differentially mediate Ad5 induced cytokine and chemokine release from peritoneal macrophages in vitro
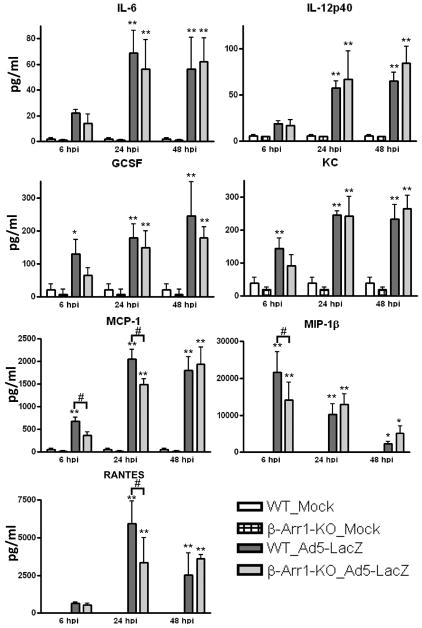
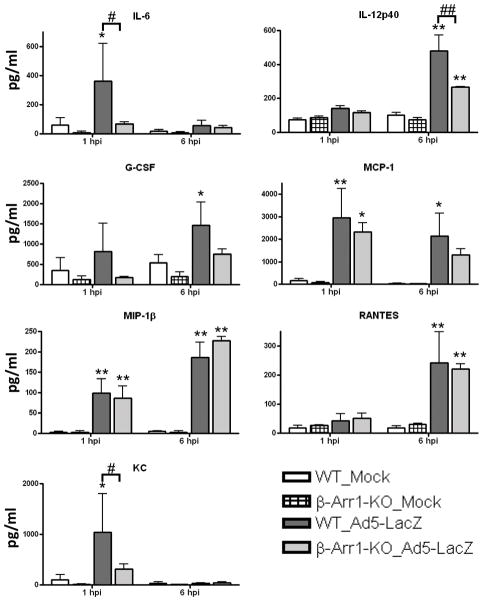
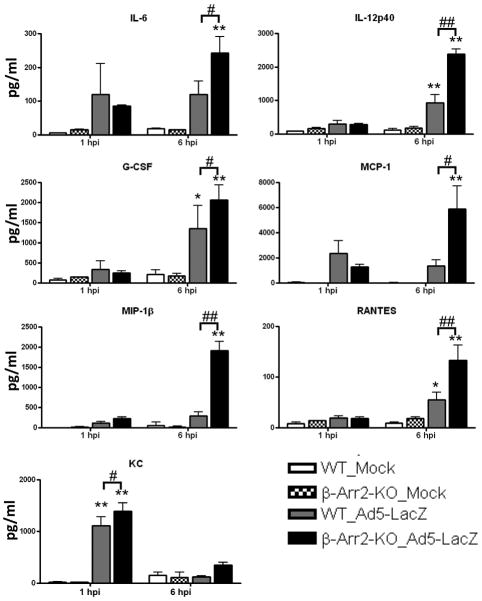
Macrophages participate in the first line of defense against invading pathogens by functioning as phagocytes, antigen presenting cells, and activators of both innate and adaptive immune responses via secretion of cytokines and chemokines that serve as co-activating factors. Numerous studies have indicated that the induction of cytokines and chemokines by Ad5 injection is dependent upon the presence of macrophages, specifically liver resident macrophages known as Kupffer cells. We have shown that the inductions of KC, MCP-1, IL-12(p40) and RANTES are Kupffer cell dependent in vivo (Appledorn et al., 2008c). To determine if β-Arrestins also play a role in the secretion of cytokines and chemokines from macrophages, we isolated peritoneal macrophages from wild type, β-Arr1, and β-Arr2 knockout mice, exposed them to Ad5-LacZ, and measured the concentration of pro-inflammatory cytokines in the growth media at various time points post Ad exposure (Figures 1–2). Interestingly we observed that levels of MIP-1β, MCP-1 and RANTES were significantly lower (p<0.05) in the β-Arr-1-KO macrophages compared to the wild types. We also observed that the decrease was time-dependent, i.e. MIP1β was lower at 6 h.p.i., whereas MCP-1 and RANTES were decreased at 24 h.p.i., suggesting that these are potentially regulated by distinct mechanisms (Figure 1). In contrast to these results, levels of IL-12(p40) and MCP-1 (at 24 and 48 h.p.i.) were significantly enhanced (p<0.05) in macrophages derived from β-Arr-2-KO mice compared to WT macrophages (Figure 2). These results, taken together, suggest that β-Arr1 may act as a positive regulator, and β-Arr2 as a negative regulator of Ad5-induced inflammatory responses.
Figure 1. Functional β-arrestin-1 acts as positive regulator for several chemokines released in response to Ad infection in vitro.
Peritoneal macrophages derived from WT or β-Arr1-KO C57BL/6 mice were isolated, plated and infected with Ad5-LacZ exactly as described in Materials and Methods. Media samples were collected at 6, 24 and 48 hours post virus infection (hpi) and assayed using a multiplexed bead array based system. The bars represent Mean ± SD. Statistical analysis was completed using Two Way ANOVA with a Bonferroni post-hoc test. The N=4 for all groups of peritoneal macrophages, including mock infected groups.
*, ** - indicate media cytokine values that are statistically different from those in Mock infected groups of the same genotype at the same time point, p<0.05, p<0.001 respectively. #, ## - indicate statistically different values in the same treatment group at the same time point, p<0.05, p<0.001 respectively.
Figure 2. Functional β-arrestin-2 acts as negative regulator for several chemokines released in response to Ad infection in vitro.
Peritoneal macrophages derived from WT or β-Arr2-KO C57BL/6 mice were isolated, plated and infected with Ad5-LacZ exactly as described in Materials and Methods. Media samples were collected at 6, 24 and 48 hours post virus infection (hpi) and assayed using a multiplexed bead array based system. The bars represent Mean ± SD. Statistical analysis was completed using Two Way ANOVA with a Bonferroni post-hoc test. The N=4 for WT_Mock and WT_Ad5-LacZ groups, N=6 for β-Arr2-KO_Mock and β-Arr2-KO_Ad5-LacZ groups.
*, ** - indicate media cytokine values that are statistically different from those in Mock infected groups of the same genotype at the same time point, p<0.05, p<0.001 respectively. #, ## - indicate statistically different values in the same treatment group at the same time point, p<0.05, p<0.001 respectively.
Positive and negative roles for β-Arrestins in Ad5 induced cytokine and chemokine release
Our results using primary macrophages from β-Arr-1 and -2 KO mice clearly demonstrate important but differential roles for β-arrestins in Ad-induced inflammatory responses. Therefore, we evaluated the potential that β-arrestin-1 and -2 also play a pivotal role in the release of inflammatory cytokines and chemokines following systemic Ad5 administrations in vivo. To accomplish this, the plasma levels of seven cytokines/chemokines, commonly induced following Ad5 injection were evaluated, following systemic delivery of 7.5×1010 vps Ad5-LacZ. As expected, all seven cytokines/chemokines tested were significantly induced within 1 h.p.i. (IL-6, MCP-1, MIP-1β, and KC, p<0.001, p<0.05), and/or 6 h.p.i (IL-12(p40), G-CSF, MCP-1, MIP-1β, and RANTES; p<0.001, p<0.05) in wild-type C57BL/6 mice (Figures 3–4). Identically injected β-Arr-1-KO mice also exhibited significant inductions of MCP-1 and MIP-1β at 1 h.p.i. (p<0.05 and p<0.001, respectively). However, at this time point, levels of IL-6 and KC were significantly lower than levels found in the wild types (p<0.05) and were not statistically induced over mock levels. Furthermore, the induction of IL-12(p40) was significantly lower at 6 h.p.i. in Ad5-injected β-Arr-1-KO as compared to wild-type animals. Although levels of G-CSF and MCP-1 in β-Arr1-KO did not reach statistically significant differences as compared to identically injected C57BL/6 mice, the levels of these factors were not statistically induced over background levels in β-Arr1-KO mice in contrast to WT mice. No significant differences in either MIP-1β or RANTES were observed (Figure 3). Overall, the results demonstrate that β-Arr1 regulates induction of an important subset of Ad5-induced cytokines and chemokines following systemic injection of Ad5 vectors in vivo.
Figure 3. Functional β-arrestin-1 acts as positive regulator of Ad mediated systemic cytokine and chemokine release in C57BL/6 mice.
WT or β-Arr1-KO C57BL/6 mice were intravenously injected with 0.75×1011 vp/mouse of Ad5-LacZ vector. Plasma samples were collected at 1 and 6 hours post virus injection (hpi). Plasma samples were analyzed using a multiplexed bead array based system. The bars represent Mean ± SD. Statistical analysis was completed using Two Way ANOVA with a Bonferroni post-hoc test. The N=3 for Mock (PBS) injected animals, N=4 for virus injected mice.
*, ** - indicate plasma cytokine values that are statistically different from those in Mock injected animals of the same genotype at the same time point, p<0.05, p<0.001 respectively. #, ## - indicate statistically different values in the same treatment group at the same time point, p<0.05, p<0.001 respectively.
Figure 4. Functional β-arrestin-2 acts as potent suppressor of Ad mediated systemic cytokine and chemokine release in C57BL/6 mice.
WT or β-Arr2-KO C57BL/6 mice were intravenously injected with 0.75×1011 vp/mouse of Ad5-LacZ vector. Plasma samples were collected at 1 and 6 hours post virus injection (hpi). Plasma samples were analyzed using a multiplexed bead array based system. The bars represent Mean ± SD. Statistical analysis was completed using Two Way ANOVA with a Bonferroni post-hoc test. The N=3 for Mock (PBS) injected animals, N=4 for virus injected mice.
*, ** - indicate plasma cytokine values that are statistically different from those in Mock injected animals of the same genotype at the same time point, p<0.05, p<0.001 respectively. #, ## - indicate statistically different values in the same treatment group at the same time point, p<0.05, p<0.001 respectively.
In contrast to observations in β-Arr1-KO mice, levels of all cytokines and chemokines tested in the plasma of Ad5 injected β-Arr2-KO mice were significantly enhanced when compared to identically injected wild type mice. Specifically, at the peak of the KC response, significantly higher levels of this chemokine were detected in Ad injected β-Arr2-KO animals as compared to wild-type mice. Additionally, significantly higher levels of IL-6 (2-fold), IL-12(p40) (2-fold), G-CSF (1.4-fold), and MCP-1 (6-fold) were detected in the plasma of β-Arr2-KO compared to wild type mice at 6 h.p.i. (Figure 4). Importantly, the absolute numbers of Ad5 genomes present in the liver in either β-Arr1-KO or β-Arr2-KO mice were not different from WT mice as measured by Ad5-genome levels (Supplemental Figure 1). While there were differences in Ad genome content of the spleens, these differences did not result in differential transduction of these tissues as measured by LacZ protein expression, as determined using a qualitative analysis of β-gal staining and quantitative β-Gal activity measurements in both liver and spleen tissues (Supplemental Figure 2). Therefore the results presented here were most likely not attributable to differential transduction of murine tissues per se. Together these data indicate that β-Arr1 positively regulates the induction of a subset of Ad5-induced cytokines and chemokines, while β-Arr2 functions more globally as a negative regulator of the induction of these innate immune factors.
β-Arrestins differentially mediate the induction of pro-inflammatory genes in livers and spleens following systemic Ad5 injection
We have previously characterized tissue specific transcriptome changes rapidly induced after transduction by Ad5 vectors both in vitro and in vivo (Hartman et al., 2007a; Hartman et al., 2007b; Kiang et al., 2006; Seregin et al., 2009b). Therefore we have selected a panel of genes and analyzed their expression in the liver and spleen of Ad5 injected WT, β-Arr1-KO and β-Arr2-KO mice at 6 h.p.i. (Tables 1–4). Selected genes include those involved in innate immune responses, such as pattern recognition receptors (TLRs, NODs), TLR signaling pathways (MyD88, TRIF, TRAF6, TRAF2bp, TBK1), markers of endothelial cells activation (e-Selectin, ICAM-1, VCAM-1), interferon responsive genes (OAS1a, IRF7, IRF8), negative regulators of cytokine signaling (SOCS-1, SOCS-3), and dsRNA editing enzymes (ADAR) (Hartman et al., 2007a; Hartman et al., 2007b; Seregin et al., 2009b). Our results demonstrate that Ad5-induced activation of a number of genes in the liver of Ad5-injected β-Arr1-KO mice were significantly reduced compared to corresponding Ad treated WT mice (Table 1). Specifically, β-Arr1-KO mice completely lacked Ad5-induced ADAR, CD14, TLR6 and VCAM-1 transcripts. However, baseline levels of TLR6 were significantly lower in the tissues of β-Arr1-KO mock injected animals, which may have partially obscured these results. In contrast to Ad5 injected WT mice, NOD-2 and TRIM-30 were not induced in Ad5 treated β-Arr1-KO mice. We also observed a significant reduction in TLR3 transcripts in the liver of Ad5 injected β-Arr1-KO mice as compared to identically injected WT mice. A transcriptome profile observed in spleens isolated from these same animals, revealed significantly reduced levels of TLR3 transcript in β-Arr1-KO mice (Table 2).
Table 1.
Ad5-LacZ induced gene expression in the liver (fold over C57BL/6 Mock, 6 h.p.i.)
| C57BL/6 (Mock) | β-Arr1-KO (Mock) | C57BL/6 (Ad5-LacZ) | β-Arr1-KO (Ad5-LacZ) | |
|---|---|---|---|---|
| ADAR | 1.0 ± 0.2 | 0.7 ± 0.1 | 2.2 ± 0.5 |
1.6 ± 0.2 |
| CD14 | 1.0 ± 0.2 | 0.7 ± 0.1 | 2.3 ± 0.5 |
1.3 ± 0.7 |
| CXCL-9 | 1.0 ± 0.1 | 1.0 ± 0.1 | 10.3 ± 2.4 | 9.9 ± 4.7 |
| DAF | 1.0 ± 0.2 | 0.9 ± 0.1 | 1.2 ± 0.1 | 1.4 ± 0.2 |
| e-Selectin | 1.0 ± 0.1 | 0.6 ± 0.2 | 2.1 ± 0.3 | 2.0 ± 0.7 |
| ICAM | 1.0 ± 0.2 | 0.7 ± 0.1 | 2.2 ± 0.2 | 2.2 ± 0.4 |
| IFNα | 1.0 ± 0.2 | 0.6 ± 0.1 | 1.2 ± 0.3 | 0.7 ± 0.2 |
| IFNβ | 1.0 ± 0.4 | 0.8 ± 0.2 | 1.6 ± 0.4 | 1.0 ± 0.1 |
| IRF-3 | 1.0 ± 0.2 | 0.9 ± 0.1 | 1.2 ± 0.2 | 1.0 ± 0.1 |
| IRF-7 | 1.0 ± 0.1 | 0.9 ± 0.2 | 15.3 ± 1.5 |
18.0 ± 1.5 |
| IRF-8 | 1.0 ± 0.1 | 0.8 ± 0.1* | 2.1 ± 0.3 | 2.3 ± 0.4 |
| Jak-1 | 1.0 ± 0.2 | 0.8 ± 0.1 | 1.4 ± 0.2 | 1.1 ± 0.1 |
| Jak-3 | 1.0 ± 0.1 | 0.7 ± 0.2 | 1.3 ± 0.1 | 1.3 ± 0.1 |
| MyD88 | 1.0 ± 0.1 | 0.8 ± 0.2 | 4.1 ± 0.5 | 4.6 ± 0.9 |
| NFkB-RelA | 1.0 ± 0.1 | 1.0 ± 0.1 | 1.7 ± 0.2 | 1.6 ± 0.2 |
| NOD-1 | 1.0 ± 0.1 | 0.7 ± 0.1* | 1.7 ± 0.2 | 1.4 ± 0.4 |
| NOD-2 | 1.0 ± 0.1 | 0.6 ± 0.2* | 1.3 ± 0.3 | 1.0 ± 0.2 |
| OAS-1a | 1.0 ± 0.3 | 0.7 ± 0.1 | 3.1 ± 0.3 | 2.6 ± 0.5 |
| SOCS-1 | 1.0 ± 0.2 | 0.7 ± 0.1 | 4.6 ± 0.6 | 4.6 ± 1.4 |
| SOCS-3 | 1.0 ± 0.2 | 0.3 ± 0.1 | 2.3 ± 0.2 | 2.5 ± 1.4 |
| TBK-1 | 1.0 ± 0.1 | 0.9 ± 0.1 | 3.9 ± 0.2 | 3.8 ± 1.0 |
| TLR-2 | 1.0 ± 0.1 | 0.7 ± 0.1 | 21.7 ± 7.0 | 25.9 ± 10.9 |
| TLR-3 | 1.0 ± 0.2 | 0.7 ± 0.1 | 11.6 ± 1.4 |
7.9 ± 3.9 |
| TLR-6 | 1.0 ± 0.1 | 0.6 ± 0.1* | 2.0 ± 0.5 |
1.5 ± 0.2 |
| TLR-9 | 1.0 ± 0.2 | 0.6 ± 0.1 | 2.0 ± 0.3 | 1.8 ± 0.2 |
| TRAF2bp | 1.0 ± 0.2 | 0.6 ± 0.2 | 6.1 ± 1.1 | 5.9 ± 3.3 |
| TRAF6 | 1.0 ± 0.2 | 1.2 ± 0.1 | 1.3 ± 0.1 | 1.3 ± 0.1 |
| TRIF | 1.0 ± 0.1 | 1.2 ± 0.1 | 1.4 ± 0.3 | 1.7 ± 0.1 |
| TRIM30 | 1.0 ± 0.2 | 0.6 ± 0.1 | 11.4 ± 1.5 | 7.0 ± 5.1 |
| VCAM | 1.0 ± 0.2 | 0.7 ± 0.1 | 1.5 ± 0.2 | 1.0 ± 0.1 |
Values represent Mean ± SD. Statistical analysis was completed using One Way ANOVA with a Student-Newman-Keuls post-hoc test, p<0.05 was deemed statistically significant. N=3 for Mock injected groups, N=4 for Ad5-LacZ injected groups. Significant differences compared to WT_Mock are highlighted in light grey color. Significant differences in transcriptional activation in β-Arr1-KO (Ad5-LacZ) group compared to WT (Ad5-LacZ) group are indicated in table by black frame and boldface font.
Indicate significant differences between mock injected animals.
Table 4.
Ad5-LacZ induced gene expression in the spleen (fold over C57BL/6 Mock, 6 h.p.i.)
| C57BL/6 (Mock) | β-Arr2-KO (Mock) | C57BL/6 (Ad5-LacZ) | β-Arr2-KO (Ad5-LacZ) | |
|---|---|---|---|---|
| ADAR | 1.1 ± 0.8 | 0.9 ± 0.3 | 1.3 ± 0.5 | 1.6 ± 0.1 |
| CXCL-9 | 1.1 ± 0.9 | 1.2 ± 0.9 | 3.6 ± 3.3 | 4.6 ± 1.9 |
| e-Selectin | 1.0 ± 0.2 | 1.0 ± 0.3 | 0.7 ± 0.1 | 1.0 ± 0.2 |
| ICAM | 1.0 ± 0.5 | 0.5 ± 0.2 | 1.3 ± 0.4 | 2.3 ± 0.7 |
| IFNα | 1.0 ± 0.1 | 1.6 ± 1.1 | 1.5 ± 1.0 | 2.3 ± 0.1 |
| IRF-7 | 1.0 ± 0.1 | 0.7 ± 0.2 | 21.4 ± 5.3 |
30.9 ± 3.0 |
| IRF-8 | 1.0 ± 0.1 | 0.7 ± 0.4 | 0.9 ± 0.2 |
1.7 ± 0.1 |
| MyD88 | 1.0 ± 0.4 | 1.0 ± 0.1 | 2.6 ± 0.1 |
3.2 ± 0.1 |
| NFkB-RelA | 1.0 ± 0.3 | 0.7 ± 0.6 | 0.7 ± 0.4 | 1.0 ± 0.2 |
| OAS-1a | 1.0 ± 0.1 | 3.4 ± 3.1 | 12.9 ± 3.3 | 15.9 ± 2.1 |
| SOCS-1 | 1.0 ± 0.4 | 0.11 ± 0.04* | 1.9 ± 1.0 | 3.3 ± 0.7 |
| SOCS-3 | 1.0 ± 0.4 | 2.9 ± 0.4* | 12.5 ± 4.4 | 12.6 ± 4.0 |
| TBK-1 | 1.0 ± 0.2 | 0.7 ± 0.4 | 0.9 ± 0.5 | 1.3 ± 0.2 |
| TLR-2 | 1.0 ± 0.3 | 0.9 ± 0.3 | 2.0 ± 0.2 | 4.1 ± 1.6 |
| TLR-3 | 1.0 ± 0.3 | 2.2 ± 1.4 | 6.1 ± 0.9 | 5.4 ± 0.3 |
| TLR-6 | 1.0 ± 0.3 | 2.0 ± 1.4 | 0.9 ± 0.1 | 1.0 ± 0.2 |
| TLR-9 | 1.0 ± 0.2 | 0.6 ± 0.3 | 1.5 ± 1.3 | 1.8 ± 0.2 |
| TRAF2bp | 1.0 ± 0.7 | 1.1 ± 0.5 | 1.0 ± 0.2 | 1.1 ± 0.1 |
Values represent Mean ± SD. Statistical analysis was completed using One Way ANOVA with a Student-Newman-Keuls post-hoc test, p<0.05 was deemed statistically significant. N=3 for Mock injected groups, N=4 for Ad5-LacZ injected groups. Significant differences compared to WT_Mock are highlighted in light grey color. Significant differences in transcriptional activation in β-Arr2-KO (Ad5-LacZ) group compared to WT (Ad5-LacZ) group are indicated in table by black frame and boldface font.
Indicate significant differences between mock injected animals.
Table 2.
Ad5-LacZ induced gene expression in the spleen (fold over C57BL/6 Mock, 6 h.p.i.)
| C57BL/6 (Mock) | β-Arr1-KO (Mock) | C57BL/6 (Ad5-LacZ) | β-Arr1-KO (Ad5-LacZ) | |
|---|---|---|---|---|
| ADAR | 1.0 ± 0.6 | 1.5 ± 0.4 | 2.7 ± 0.2 | 3.0 ± 0.2 |
| CD14 | 1.0 ± 0.5 | 1.9 ± 0.7 | 2.0 ± 0.1 | 1.5 ± 0.5 |
| CXCL-9 | 1.1 ± 1.0 | 3.3 ± 1.0 | 12.4 ± 2.9 | 8.9 ± 3.5 |
| e-Selectin | 1.0 ± 0.2 | 1.5 ± 0.4 | 1.2 ± 0.1 | 1.5 ± 0.3 |
| ICAM | 1.0 ± 0.4 | 1.3 ± 0.1 | 4.1 ± 0.2 | 4.3 ± 0.6 |
| IFNα | 1.0 ± 0.6 | 2.0 ± 0.8 | 1.8 ± 0.6 | 1.7 ± 0.3 |
| IRF-7 | 1.0 ± 0.3 | 1.4 ± 0.3 | 34.3 ± 4.7 | 38.4 ± 1.4 |
| IRF-8 | 1.0 ± 0.3 | 1.2 ± 0.2 | 2.6 ± 0.4 | 2.4 ± 0.3 |
| Jak-1 | 1.0 ± 0.5 | 1.9 ± 0.3 | 0.7 ± 0.1 | 0.7 ± 0.1 |
| MyD88 | 1.0 ± 0.1 | 1.5 ± 0.4 | 3.3 ± 0.3 | 3.4 ± 0.4 |
| NFkB-RelA | 1.0 ± 0.4 | 0.8 ± 0.1 | 0.9 ± 0.1 | 1.0 ± 0.4 |
| OAS-1a | 1.0 ± 0.5 | 2.6 ± 0.4* | 13.4 ± 2.6 | 11.4 ± 0.3 |
| SOCS-1 | 1.1 ± 0.8 | 1.3 ± 0.2 | 3.9 ± 0.2 | 3.4 ± 1.0 |
| SOCS-3 | 1.1 ± 0.9 | 2.2 ± 0.1 | 30.4 ± 3.6 | 33.3 ± 10.3 |
| TBK-1 | 1.0 ± 0.1 | 1.0 ± 0.1 | 1.6 ± 0.1 | 2.1 ± 0.3 |
| TLR-2 | 1.0 ± 0.4 | 1.6 ± 0.1 | 3.8 ± 0.1 | 4.3 ± 1.0 |
| TLR-3 | 1.0 ± 0.3 | 1.9 ± 0.2* | 10.0 ± 0.6 |
7.6 ± 0.9 |
| TLR-6 | 1.0 ± 0.5 | 1.6 ± 0.5 | 0.9 ± 0.1 | 1.0 ± 0.1 |
| TLR-9 | 1.1 ± 0.8 | 1.1 ± 0.1 | 4.3 ± 0.7 | 5.2 ± 1.1 |
| TRAF2bp | 1.0 ± 0.1 | 1.3 ± 0.1 | 1.3 ± 0.1 | 1.7 ± 0.5 |
Values represent Mean ± SD. Statistical analysis was completed using One Way ANOVA with a Student-Newman-Keuls post-hoc test, p<0.05 was deemed statistically significant. N=3 for Mock injected groups, N=4 for Ad5-LacZ injected groups. Significant differences compared to WT_Mock are highlighted in light grey color. Significant differences in transcriptional activation in β-Arr1-KO (Ad5-LacZ) group compared to WT (Ad5-LacZ) group are indicated in table by black frame and boldface font.
Indicate significant differences between mock injected animals.
Opposite results were obtained in Ad5 injected β-Arr2-KO mice, results that positively correlated with the increased cytokines and chemokines levels observed in these same mice. Over half of the genes tested were induced to significantly higher levels in livers of Ad injected β-Arr2-KO as compared to identically injected WT mice (Table 3). Specifically, we detected significantly higher amounts of CXCL-9, ICAM-1, IRF-7, MyD88, SOCS-1, SOCS-3, TBK-1, TLR-2, and TRAF-2bp transcripts in livers of Ad5 injected β-Arr2-KO mice, as compared to wild type mice. Moreover, several genes, including ADAR, IRF8, Oas1a, which were not induced in Ad5 injected WT mice, were significantly induced in Ad5 injected β-Arr2-KO mice. The levels of these same transcripts in the spleen followed a similar trend, as IRF-7, IRF-8 and MyD88 were present in significantly higher levels in spleens of Ad5 injected β-Arr2-KO compared to wild type mice. In addition, CXCL9, IFNα, SOCS-1 and TLR9, which were not induced in spleens of wild type C57BL/6 mice, were significantly induced in β-Arr2-KO mice following systemic Ad5 injection (Table 4). These results further support the notion that β-Arr2 functions as a negative regulator of Ad5-induced innate immune responses, whereas similar responses are positively mediated by β-Arr1.
Table 3.
Ad5-LacZ induced gene expression in the liver (fold over C57BL/6 Mock, 6 h.p.i.)
| C57BL/6 (Mock) | β-Arr2-KO (Mock) | C57BL/6 (Ad5-LacZ) | β-Arr2-KO (Ad5-LacZ) | |
|---|---|---|---|---|
| ADAR | 1.0 ± 0.1 | 0.7 ± 0.1 | 1.3 ± 0.3 | 1.6 ± 0.1 |
| CD14 | 1.0 ± 0.2 | 0.9 ± 0.1 | 2.1 ± 1.2 | 1.9 ± 1.2 |
| CXCL-9 | 1.0 ± 0.3 | 0.6 ± 0.1 | 5.2 ± 0.7 |
9.9 ± 2.7 |
| DAF | 1.0 ± 0.1 | 0.7 ± 0.1 | 1.1 ± 0.2 | 0.9 ± 0.1 |
| e-Selectin | 1.0 ± 0.2 | 0.7 ± 0.2 | 2.0 ± 0.8 | 3.0 ± 1.1 |
| ICAM | 1.0 ± 0.2 | 0.7 ± 0.2 | 1.9 ± 0.2 |
3.2 ± 0.6 |
| IFNα | 1.0 ± 0.2 | 0.7 ± 0.1 | 0.6 ± 0.2 | 0.6 ± 0.1 |
| IFNβ | 1.0 ± 0.2 | 0.6 ± 0.1 | 0.6 ± 0.2 | 0.6 ± 0.1 |
| IRF-3 | 1.0 ± 0.1 | 0.6 ± 0.1* | 0.7 ± 0.1 | 0.6 ± 0.1 |
| IRF-7 | 1.0 ± 0.1 | 0.7 ± 0.1 | 9.1 ± 2.4 |
13.2 ± 1.3 |
| IRF-8 | 1.0 ± 0.1 | 0.7 ± 0.1* | 1.6 ± 0.4 |
2.8 ± 0.6 |
| Jak-1 | 1.0 ± 0.1 | 0.7 ± 0.1* | 0.7 ± 0.2 | 0.7 ± 0.1 |
| Jak-3 | 1.0 ± 0.1 | 0.7 ± 0.1 | 1.0 ± 0.3 | 1.1 ± 0.1 |
| MyD88 | 1.0 ± 0.1 | 0.6 ± 0.1* | 2.7 ± 1.0 |
4.1 ± 1.0 |
| NFkB-RelA | 1.0 ± 0.1 | 0.7 ± 0.1 | 1.0 ± 0.3 | 1.4 ± 0.2 |
| NOD-1 | 1.0 ± 0.3 | 0.8 ± 0.1 | 1.1 ± 0.1 | 1.4 ± 0.1 |
| NOD-2 | 1.0 ± 0.2 | 0.7 ± 0.1 | 0.7 ± 0.1 | 0.9 ± 0.1 |
| OAS-1a | 1.0 ± 0.2 | 0.6 ± 0.1 | 1.5 ± 0.4 |
2.2 ± 0.3 |
| SOCS-1 | 1.0 ± 0.1 | 0.8 ± 0.1 | 3.9 ± 1.4 |
7.5 ± 1.4 |
| SOCS-3 | 1.0 ± 0.4 | 0.9 ± 0.6 | 2.2 ± 0.7 |
4.5 ± 0.5 |
| TBK-1 | 1.0 ± 0.1 | 0.8 ± 0.1 | 2.7 ± 0.4 |
3.4 ± 0.5 |
| TLR-2 | 1.0 ± 0.1 | 0.9 ± 0.3 | 18.6 ± 8.5 |
75.8 ± 28.1 |
| TLR-3 | 1.0 ± 0.1 | 0.6 ± 0.1* | 5.9 ± 1.3 | 9.0 ± 3.0 |
| TLR-6 | 1.0 ± 0.1 | 0.9 ± 0.1 | 1.2 ± 0.2 | 1.6 ± 0.4 |
| TLR-9 | 1.0 ± 0.1 | 0.6 ± 0.1* | 1.2 ± 0.3 | 1.2 ± 0.1 |
| TRAF2bp | 1.0 ± 0.3 | 0.6 ± 0.1 | 3.7 ± 1.5 |
11.5 ± 2.7 |
| TRAF6 | 1.0 ± 0.1 | 0.8 ± 0.1* | 0.9 ± 0.1 | 0.8 ± 0.1 |
| TRIF | 1.0 ± 0.1 | 0.9 ± 0.1* | 0.9 ± 0.2 | 1.1 ± 0.2 |
| TRIM30 | 1.0 ± 0.1 | 0.6 ± 0.1* | 6.7 ± 2.3 | 8.7 ± 1.0 |
| VCAM | 1.0 ± 0.1 | 0.8 ± 0.1 | 0.7 ± 0.2 | 0.9 ± 0.1 |
Values represent Mean ± SD. Statistical analysis was completed using One Way ANOVA with a Student-Newman-Keuls post-hoc test, p<0.05 was deemed statistically significant. N=3 for Mock injected groups, N=3 for Ad5-LacZ injected groups. Significant differences compared to WT_Mock are highlighted in light grey color. Significant differences in transcriptional activation in β-Arr2-KO (Ad5-LacZ) group compared to WT (Ad5-LacZ) group are indicated in table by black frame and boldface font.
Indicate significant differences between mock injected animals.
Discussion
Ad based vectors possess an enormous potential for numerous gene transfer applications based upon their broad tropism, highly efficient transductional capability, and their ease for scalable production. Based upon these facts, Ad vectors have been the most utilized gene transfer vector in humans to date (http://www.wiley.co.uk/wileychi/genmed/clinical/). However, the robust innate immune response elicited shortly after intravascular Ad delivery poses a significant limitation to the use of this vector for numerous applications that could benefit from such administrations, such as gene transduction into the liver. Intravascular delivery of Ads into animal models facilitates detection of Ad induced innate immune responses, which may not be detectable when other routes of administration (such as intramuscular) are utilized. These innate responses include acute thrombocytopenia (Kiang et al., 2006; Wolins et al., 2003), robust cytokine and chemokine releases (Appledorn et al., 2008b; Appledorn et al., 2008c; Kiang et al., 2006; Seregin et al., 2009b), activation of endothelial cells (Liu et al., 2003; Schiedner et al., 2003) and inductions of inflammatory gene networks in multiple tissues, including both the liver and the spleen (Appledorn et al., 2008a; Hartman et al., 2007b; Kiang et al., 2006). Various strategies designed to minimize these acute immune responses, including non-covalent modification of Ad capsids (PEGylation) (Croyle et al., 2005), usage of immunosuppressive drugs, such as Dexamethasone (Seregin et al., 2009b), TNFα blockers (Song et al., 2008) or TLR9 inhibitors (Cerullo et al., 2007) have shown promising results, but may have limited applicability due to either non-specific off target effects, a significant alteration of Ad transductional efficiency, lack of scalability, and/or alteration of Ad vector biodistribution profiles. As a result, continued investigations of Ad-induced innate immune responses are required in order to more fully understand the mechanisms by which immune responses against Ad vectors are generated within the host.
It is well established that Ad5-induced innate immune responses are mediated by the TLR adaptor proteins MyD88 and TRIF. As a receptor that utilizes both MyD88 and TRIF, TLR4 is activated by LPS (Fan et al., 2007; Parameswaran et al., 2006; Wang et al., 2006). Because both β-Arr1 and β-Arr2 proteins have been shown to modulate LPS induced TLR4 mediated signaling, we sought to determine if these proteins also played a role in Ad5-induced innate immune responses. Utilizing β-Arr1-KO and β-Arr2-KO mouse models, we show that whereas β-Arr1 served as positive regulator of a portion of Ad5 induced innate immune responses, β-Arr2 appears to function as a negative regulator of Ad5 induced innate immune responses.
For example, following intravenous Ad5 injection into β-Arr1-KO mice, we observed significantly reduced levels of pro-inflammatory mediators including IL-6, IL-12(p40) and KC, relative to levels measured in Ad5 injected WT mice. Furthermore, we observed significantly reduced transcription of innate immune response genes in transdcued tissues of Ad5 injected β-Arr1-KO mice. We additionally detected reduced expression levels of MCP-1, MIP-1β, and RANTES in peritoneal macrophages from β-Arr1-KO mice following exposure to Ad5 vectors in vitro. The results suggest that β-Arr1 may serve as a mediator of Ad-induced immune responses downstream of TLR signaling, specifically those that require MyD88 as an adaptor. The findings also highlight a relatively underappreciated role for β-Arr1 as a positive regulator of pro-inflammatory responses, a role that contrasts the previously reported role for β-Arr1 as playing a negative role in the induction of cytokine responses following LPS challenge (Wang et al., 2006). Our present results however, are consistent with our recent study where we found that β-Arr1 is necessary for the sustained production of some cytokines/chemokines after LPS challenge in vivo (Porter et al, 2009. Manuscript submitted for publication).
The role of β-Arr2 in the induction of innate immune responses by Ad vectors was diametrically opposite to that of β-Arr1. This was evidenced by significantly higher inductions by Ads of multiple cytokines and chemokines, and inflammatory gene expression responses after injection into β-Arr2-KO mice. These responses were corroborated in vitro as detected in Ad5 infected peritoneal macrophages, suggesting that this cell type may play an important role in mediating this response in vivo. Interestingly, the profile of innate immune responses observed in β-Arr2-KO mice paralleled the role that TLR4 plays in innate immune responses noted after systemic Ad5 injection(Appledorn et al., 2009). Our previous work indicated that TLR4 plays a negative role in the induction of IL-12(p40) and G-CSF following intravenous Ad5 injection. It is possible that the negative role that TLR4 plays in Ad5 induced innate immune responses is mediated by β-Arr2, such that loss of either protein results in a more pronounced innate immune response triggered by Ad5. However, it is also clear that other factors must also play a role in these responses, since the phenotype in Ad5 injected β-Arr2-KO animals did not completely mimic that found in Ad5 injected TLR4-KO mice (Appledorn et al., 2009). Interestingly, in a recent study, we found that β-Arr-2 also mediates LPS/TLR4-induced cytokine responses in vivo (Porter et al, 2009, Manuscript submitted for publication). Although the biochemical mechanisms by which β-arrestins mediate or inhibit the innate immune responses of Ad5 are not known, previously reported interactions of β-arrestins with TRAF6, IκBα and p105 might play a role in this process (Gao et al., 2004; Parameswaran et al., 2006; Wang et al., 2006). It is also possible that scaffolding functions of β-arrestins unique to Ad5 signaling pathways might be important. It has recently been shown that Ad5 vectors trigger TLR-independent pathways, such as NALP3/ASC inflammasomes (cytoplasmic NOD-like receptors) (Muruve et al., 2008), resulting in activation of IL-1β and IL-18, IL-1α/IL-1RI mediated, nucleic acid independent signaling, and Ad interactions with mucosal defensins have also been identified as mediating Ad5-induced innate immune responses (Di Paolo et al., 2009; Smith and Nemerow, 2008). The potential roles of β-arrestins in mediating these responses remain to be determined.
In summary, our data demonstrate important roles for both β-Arr1 and β-Arr2 as positive and negative regulators in modulating Ad5 induced innate immune responses. β-Arr-1 and -2 interaction partners that mediate β-arrestin’s actions in response to Ad5 administration may include proteins of the TLR pathways or other unique proteins of the Ad5 responsive signaling pathways.
Supplementary Material
Acknowledgments
We wish to thank Michigan State University Laboratory Animal support facility for their assistance in the humane care and maintenance of the animals utilized in this work. S.S.S. was supported by American Heart Association Midwest Affiliate Fellowship 0815660G. A.A. was supported by the National Institutes of Health grants RO1DK-069884, P01 CA078673, the MSU Foundation and the Osteopathic Heritage Foundation. N.P. is supported by the National Institutes of Health grants R01AR056680, R01HL095637, and R21AR055726.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Amalfitano A, Hauser MA, Hu H, Serra D, Begy CR, Chamberlain JS. Production and characterization of improved adenovirus vectors with the E1, E2b, and E3 genes deleted. J Virol. 1998;72(2):926–33. doi: 10.1128/jvi.72.2.926-933.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Appledorn DM, Kiang A, McBride A, Jiang H, Seregin S, Scott JM, Stringer R, Kousa Y, Hoban M, Frank MM, Amalfitano A. Wild-type adenoviruses from groups A-F evoke unique innate immune responses, of which HAd3 and SAd23 are partially complement dependent. Gene Ther. 2008a doi: 10.1038/gt.2008.18. [DOI] [PubMed] [Google Scholar]
- Appledorn DM, McBride A, Seregin S, Scott JM, Schuldt N, Kiang A, Godbehere S, Amalfitano A. Complex interactions with several arms of the complement system dictate innate and humoral immunity to adenoviral vectors. Gene Ther. 2008b doi: 10.1038/gt.2008.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Appledorn DM, Patial S, Godbehere S, Parameswaran N, AA TRIF, and TRIF-Interacting TLRs Differentially Modulate Several Adenovirus Vector-Induced Immune Responses. Journal of Innate Immunity. 2009;1(4):376–388. doi: 10.1159/000207194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Appledorn DM, Patial S, McBride A, Godbehere S, Van Rooijen N, Parameswaran N, Amalfitano A. Adenovirus vector-induced innate inflammatory mediators, MAPK signaling, as well as adaptive immune responses are dependent upon both TLR2 and TLR9 in vivo. J Immunol. 2008c;181(3):2134–44. doi: 10.4049/jimmunol.181.3.2134. [DOI] [PubMed] [Google Scholar]
- Barrington R, Zhang M, Fischer M, Carroll MC. The role of complement in inflammation and adaptive immunity. Immunol Rev. 2001;180:5–15. doi: 10.1034/j.1600-065x.2001.1800101.x. [DOI] [PubMed] [Google Scholar]
- Cerullo V, Seiler MP, Mane V, Brunetti-Pierri N, Clarke C, Bertin TK, Rodgers JR, Lee B. Toll-like receptor 9 triggers an innate immune response to helper-dependent adenoviral vectors. Mol Ther. 2007;15(2):378–85. doi: 10.1038/sj.mt.6300031. [DOI] [PubMed] [Google Scholar]
- Cichon G, Boeckh-Herwig S, Schmidt HH, Wehnes E, Muller T, Pring-Akerblom P, Burger R. Complement activation by recombinant adenoviruses. Gene Ther. 2001;8(23):1794–800. doi: 10.1038/sj.gt.3301611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cotter MJ, Zaiss AK, Muruve DA. Neutrophils interact with adenovirus vectors via Fc receptors and complement receptor 1. J Virol. 2005;79(23):14622–31. doi: 10.1128/JVI.79.23.14622-14631.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Croyle MA, Le HT, Linse KD, Cerullo V, Toietta G, Beaudet A, Pastore L. PEGylated helper-dependent adenoviral vectors: highly efficient vectors with an enhanced safety profile. Gene Ther. 2005;12(7):579–87. doi: 10.1038/sj.gt.3302441. [DOI] [PubMed] [Google Scholar]
- DeWire SM, Ahn S, Lefkowitz RJ, Shenoy SK. Beta-arrestins and cell signaling. Annu Rev Physiol. 2007;69:483–510. doi: 10.1146/annurev.physiol.69.022405.154749. [DOI] [PubMed] [Google Scholar]
- Di Paolo NC, Miao EA, Iwakura Y, Murali-Krishna K, Aderem A, Flavell RA, Papayannopoulou T, Shayakhmetov DM. Virus binding to a plasma membrane receptor triggers interleukin-1 alpha-mediated proinflammatory macrophage response in vivo. Immunity. 2009;31(1):110–21. doi: 10.1016/j.immuni.2009.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Everett RS, Hodges BL, Ding EY, Xu F, Serra D, Amalfitano A. Liver toxicities typically induced by first-generation adenoviral vectors can be reduced by use of E1, E2b-deleted adenoviral vectors. Hum Gene Ther. 2003;14(18):1715–26. doi: 10.1089/104303403322611737. [DOI] [PubMed] [Google Scholar]
- Fan H, Luttrell LM, Tempel GE, Senn JJ, Halushka PV, Cook JA. Beta-arrestins 1 and 2 differentially regulate LPS-induced signaling and pro-inflammatory gene expression. Mol Immunol. 2007;44(12):3092–9. doi: 10.1016/j.molimm.2007.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao H, Sun Y, Wu Y, Luan B, Wang Y, Qu B, Pei G. Identification of beta-arrestin2 as a G protein-coupled receptor-stimulated regulator of NF-kappaB pathways. Mol Cell. 2004;14(3):303–17. doi: 10.1016/s1097-2765(04)00216-3. [DOI] [PubMed] [Google Scholar]
- Hartman ZC, Appledorn DM, Amalfitano A. Adenovirus vector induced innate immune responses: impact upon efficacy and toxicity in gene therapy and vaccine applications. Virus Res. 2008;132(1–2):1–14. doi: 10.1016/j.virusres.2007.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartman ZC, Black EP, Amalfitano A. Adenoviral infection induces a multi-faceted innate cellular immune response that is mediated by the toll-like receptor pathway in A549 cells. Virology. 2007a;358(2):357–72. doi: 10.1016/j.virol.2006.08.041. [DOI] [PubMed] [Google Scholar]
- Hartman ZC, Kiang A, Everett RS, Serra D, Yang XY, Clay TM, Amalfitano A. Adenovirus infection triggers a rapid, MyD88-regulated transcriptome response critical to acute-phase and adaptive immune responses in vivo. J Virol. 2007b;81(4):1796–812. doi: 10.1128/JVI.01936-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hodges BL, Evans HK, Everett RS, Ding EY, Serra D, Amalfitano A. Adenovirus vectors with the 100K gene deleted and their potential for multiple gene therapy applications. J Virol. 2001;75(13):5913–20. doi: 10.1128/JVI.75.13.5913-5920.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofstetter JR, Zhang A, Mayeda AR, Guscar T, Nurnberger JI, Jr, Lahiri DK. Genomic DNA from mice: a comparison of recovery methods and tissue sources. Biochem Mol Med. 1997;62(2):197–202. doi: 10.1006/bmme.1997.2637. [DOI] [PubMed] [Google Scholar]
- Hu H, Serra D, Amalfitano A. Persistence of an [E1-, polymerase-] adenovirus vector despite transduction of a neoantigen into immune-competent mice. Hum Gene Ther. 1999;10(3):355–64. doi: 10.1089/10430349950018805. [DOI] [PubMed] [Google Scholar]
- Jia Q, Zhou HR, Shi Y, Pestka JJ. Docosahexaenoic acid consumption inhibits deoxynivalenol-induced CREB/ATF1 activation and IL-6 gene transcription in mouse macrophages. J Nutr. 2006;136(2):366–72. doi: 10.1093/jn/136.2.366. [DOI] [PubMed] [Google Scholar]
- Kiang A, Hartman ZC, Everett RS, Serra D, Jiang H, Frank MM, Amalfitano A. Multiple innate inflammatory responses induced after systemic adenovirus vector delivery depend on a functional complement system. Mol Ther. 2006;14(4):588–98. doi: 10.1016/j.ymthe.2006.03.024. [DOI] [PubMed] [Google Scholar]
- Kirschfink M. Controlling the complement system in inflammation. Immunopharmacology. 1997;38(1–2):51–62. doi: 10.1016/s0162-3109(97)00057-x. [DOI] [PubMed] [Google Scholar]
- Liu Q, Zaiss AK, Colarusso P, Patel K, Haljan G, Wickham TJ, Muruve DA. The role of capsid-endothelial interactions in the innate immune response to adenovirus vectors. Hum Gene Ther. 2003;14(7):627–43. doi: 10.1089/104303403321618146. [DOI] [PubMed] [Google Scholar]
- Loniewski K, Shi Y, Pestka J, Parameswaran N. Toll-like receptors differentially regulate GPCR kinases and arrestins in primary macrophages. Mol Immunol. 2008;45(8):2312–22. doi: 10.1016/j.molimm.2007.11.012. [DOI] [PubMed] [Google Scholar]
- Makrides SC. Therapeutic inhibition of the complement system. Pharmacol Rev. 1998;50(1):59–87. [PubMed] [Google Scholar]
- Muruve DA, Petrilli V, Zaiss AK, White LR, Clark SA, Ross PJ, Parks RJ, Tschopp J. The inflammasome recognizes cytosolic microbial and host DNA and triggers an innate immune response. Nature. 2008;452(7183):103–7. doi: 10.1038/nature06664. [DOI] [PubMed] [Google Scholar]
- Ng P, Graham FL. Construction of first-generation adenoviral vectors. Methods Mol Med. 2002;69:389–414. doi: 10.1385/1-59259-141-8:389. [DOI] [PubMed] [Google Scholar]
- Parameswaran N, Pao CS, Leonhard KS, Kang DS, Kratz M, Ley SC, Benovic JL. Arrestin-2 and G protein-coupled receptor kinase 5 interact with NFkappaB1 p105 and negatively regulate lipopolysaccharide-stimulated ERK1/2 activation in macrophages. J Biol Chem. 2006;281(45):34159–70. doi: 10.1074/jbc.M605376200. [DOI] [PubMed] [Google Scholar]
- Rajagopal K, Whalen EJ, Violin JD, Stiber JA, Rosenberg PB, Premont RT, Coffman TM, Rockman HA, Lefkowitz RJ. Beta-arrestin2-mediated inotropic effects of the angiotensin II type 1A receptor in isolated cardiac myocytes. Proc Natl Acad Sci U S A. 2006;103(44):16284–9. doi: 10.1073/pnas.0607583103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schiedner G, Bloch W, Hertel S, Johnston M, Molojavyi A, Dries V, Varga G, Van Rooijen N, Kochanek S. A hemodynamic response to intravenous adenovirus vector particles is caused by systemic Kupffer cell-mediated activation of endothelial cells. Hum Gene Ther. 2003;14(17):1631–41. doi: 10.1089/104303403322542275. [DOI] [PubMed] [Google Scholar]
- Seregin SS, Aldhamen YA, Appledorn DM, Schuldt NJ, McBride AJ, Bujold M, Godbehere SS, Amalfitano A. CR1/2 is an important suppressor of Adenovirus-induced innate immune responses and is required for induction of neutralizing antibodies. Gene Ther. 2009a doi: 10.1038/gt.2009.77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seregin SS, Appledorn DM, McBride AJ, Schuldt NJ, Aldhamen YA, Voss T, Wei J, Bujold M, Nance W, Godbehere S, Amalfitano A. Transient Pretreatment With Glucocorticoid Ablates Innate Toxicity of Systemically Delivered Adenoviral Vectors Without Reducing Efficacy. Mol Ther. 2009b doi: 10.1038/mt.2008.297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith JG, Nemerow GR. Mechanism of adenovirus neutralization by Human alpha-defensins. Cell Host Microbe. 2008;3(1):11–9. doi: 10.1016/j.chom.2007.12.001. [DOI] [PubMed] [Google Scholar]
- Song MY, Park SK, Kim CS, Yoo TH, Kim B, Kim MS, Kim YS, Kwag WJ, Lee BK, Baek K. Characterization of a novel anti-human TNF-alpha murine monoclonal antibody with high binding affinity and neutralizing activity. Exp Mol Med. 2008;40(1):35–42. doi: 10.3858/emm.2008.40.1.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y, Tang Y, Teng L, Wu Y, Zhao X, Pei G. Association of beta-arrestin and TRAF6 negatively regulates Toll-like receptor-interleukin 1 receptor signaling. Nat Immunol. 2006;7(2):139–47. doi: 10.1038/ni1294. [DOI] [PubMed] [Google Scholar]
- Wolins N, Lozier J, Eggerman TL, Jones E, Aguilar-Cordova E, Vostal JG. Intravenous administration of replication-incompetent adenovirus to rhesus monkeys induces thrombocytopenia by increasing in vivo platelet clearance. Br J Haematol. 2003;123(5):903–5. doi: 10.1046/j.1365-2141.2003.04719.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.