Abstract
Refractory ascites is defined as ascites that does not recede or that recurs shortly after therapeutic paracentesis, despite sodium restriction and diuretic treatment. To date, there is no approved medical therapy specifically for refractory ascites. Management of these patients is based upon procedures such as large-volume paracentesis and transjugular intrahepatic portosystemic shunts (TIPS), which temporarily alleviate symptoms but are not curative. These patients have a poor prognosis and are at risk for a series of complications that are associated with the condition or are secondary to therapy. The most common complications include spontaneous bacterial peritonitis, hepatic hydrothorax, spontaneous bacterial empyema, and umbilical hernia. The predicted survival rate is as low as 50% at 1 year, and prognosis worsens as patients present with comorbidities such as hepatorenal syndrome, renal failure, and hepatocellular carcinoma. The only curative treatment is liver transplantation, though current studies have shown that TIPS also increases survival.
Keywords: Refractory ascites, paracentesis, TIPS, spontaneous bacterial peritonitis, spontaneous bacterial empyema
Cirrhosis, the final common pathway for a variety of chronic liver injuries, is defined by the replacement of liver tissue by fibrous scar tissue and characterized by architectural derangements that lead to regenerative nodules. Clinically, the severity of cirrhosis is classified by a spectrum of portal hypertension manifestations.1 Patients at one end of the spectrum may be entirely asymptomatic, whereas at the other end, they may have findings such as hepatic encephalopathy, gastroesophageal varices, and ascites. One of the most serious signs of decompensated liver disease is refractory ascites, which has a prevalence of 5–10% in patients with ascites2 and a survival rate as low as 50% at 6–12 months postdiagnosis.3-5
Fortunately, the results of a survey administered by practicing gastroenterologists in 2006 regarding patients presenting with cirrhosis and ascites revealed satisfactory compliance of physicians with ascites management guidelines. The use of diuretics and salt intake restriction was emphasized by 100% of the respondent physicians, with serial body weight emphasized by 67% of the physicians.6
Moreover, refractory ascites refers to the inability to mobilize ascitic fluid (Table 1). Although these patients are on a sodium-restricted diet (≤90 mmol/d), they still excrete less sodium than they consume.3 In addition, despite being on maximal doses of diuretics (spironolactone 400 mg and furosemide 160 mg) for at least 1 week, ascites persists with a mean weight loss of less than 0.8 kg over 4 days.3 In other cases, physicians are unable to achieve maximal diuretic dosage due to the development of clinical adverse effects or electrolyte disturbances. Finally, multiple early recurrence of ascites, which is usually seen within 4 weeks of fluid mobilization, may be the first presentation of refractory ascites in many patients.3
Table 1.
Diagnostic Criteria of Refractory Ascites
| Adapted from Moore KP, et al.15 |
|
Refractory ascites has a poor prognosis and is associated with complications such as dilutional hyponatremia, hepatorenal syndrome (HRS), spontaneous bacterial empyema (SBEM), hepatic hydrothorax, spontaneous bacterial peritonitis (SBP), and umbilical hernia in the absence of any other precipitating factors3 (Table 2). Additionally, patients presenting with comorbidities such as diabetes, age greater than 60, and hepatocellular carcinoma have been shown to have decreased survival rates.3,4 The current management primarily includes measures to temporarily alleviate symptoms but is generally not curative. Diuretic therapy alone does not improve the quality of life of these patients, as the two main factors defining the subgroups of refractory ascites are unsuccessful medical therapy trials and the development of diuretic-induced side effects such as hyper- or hypokalemia and encephalopathy.
Table 2.
Clinical Implications of Refractory Ascites
|
Effective treatments for controlling refractory ascites include large-volume paracentesis and transjugular intrahepatic portosystemic shunts (TIPS), which has the advantage of increased safety and efficacy. Indeed, the survival rate in patients with normal liver function and normal sodium could be as high as 80% at 3 years.7 Nevertheless, liver transplantation remains the only curative treatment for refractory ascites.
Pathophysiology
Different theories have been proposed to explain the pathophysiology of ascites. The three main theories include the underfill, overflow, and peripheral vasodilation theories.8
The overflow theory proposes that extracellular volume expands secondary to increased reabsorption of sodium at the proximal and distal tubules and the activation of the renin-angiotensin-aldosterone system (RAAS) and the sympathetic nervous system (SNS). On the other hand, the underfill theory suggests that increased portal pressure, in the presence of portal hypertension, causes splanchnic vasodilation. This results in increased portal venous blood flow and lymph formation by the splanchnic circulation, eventually leaking into the peritoneal cavity. Furthermore, splanchnic vasodilation causes a decrease in arterial blood volume, activating central baroreceptors. As a result, the SNS is activated, causing arterial vasoconstriction. The RAAS is also activated, promoting further sodium retention.8
Finally, a commonly accepted theory of ascites formation is based upon the peripheral vasodilation theory, which states that ascites develops secondary to the continuous retention of sodium. Splanchnic vasodilation causes arterial system underfilling; as a result, vasopressin activity increases and causes hypervolemia. Initially, there is no sodium retention; however, the body is eventually unable to maintain homeostasis, and fluid starts leaking into the peritoneal cavity. Sodium and water retention develop as the SNS and RAAS are activated to compensate for arterial underfilling. This theory is believed to explain the development of HRS and dilutional hyponatremia in patients with refractory ascites.1,9-11
Splanchnic circulation remains patent in portal hypertension as a result of its own production of vasodilators such as prostaglandin E, prostacyclin, and nitric oxide.1 The production of these vasodilators results in a hyperdynamic state of the splanchnic circulation, causing low vascular resistance, increased cardiac output, and decreased blood pressure.12 As a result of elevated sinusoidal pressure, there is an increase in venous blood flow and, therefore, increased lymph formation in the splanchnic circulation. The rate of lymph production exceeds the flow rate into the thoracic duct. Hence, fluid leaks into the peritoneal cavity, forming ascites.12,13
According to Arroyo and Gines,13 shear stress in the systemic circulation and the increased production of vasoactive substances (vasopressin, norepinephrine, endothelin, angiotensin II) increase endothelin synthase and nitric oxide production. Therefore, vasodilation by nitric oxide increases in the splanchnic circulation as an adaptive response to an increase in blood flow.14
In 1988, the International Ascites Club divided refractory ascites into two categories: type 1, or diuretic-resistant ascites, which is defined as the inability to mobilize ascites fluid despite intensive medical therapy and salt restriction diet for at least 1 week; and type 2, or diuretic-intractable ascites, which is characterized by the recurrence of ascites secondary to the development of diuretic-induced complications, which prevents the use of the maximal dose of diuretics.13,15 Side effects include hepatic encephalopathy (4%),2 renal failure (24%),2 and electrolyte disturbances such as hyponatremia and/or hyper- or hypokalemia.
The diagnostic criteria of refractory ascites consist of ascites that cannot be mobilized with early recurrence within 4 weeks of abdominal paracentesis and lack of response to maximal doses of diuretic (spironolactone 400 mg/d and furosemide 160 mg/d) for at least 1 week. Furthermore, other diagnostic criteria involve diuretic-induced complications such as hyponatremia, hepatic encephalopathy, renal failure, or hyperkalemia in the absence of other precipitating factors. Lastly, other authors such as Ring-Larsen2 and Moore and colleagues15 revised the diagnostic criteria of refractory ascites to include persistent ascites despite sodium restriction (50–90 mmol/d, varying among authors), mean weight loss of less than 0.8 kg over 4 days, and urinary sodium excretion that is less than sodium intake (<50 mmol/d).2
Furthermore, several parameters have been used to determine the likelihood that a patient with ascites will respond to therapy. For example, initial fractional excretion of sodium (FeNa) greater than 0.2% may predict the development of refractory ascites in patients receiving diuretic therapy.2 FeNa is defined as the amount of sodium that is excreted compared to the amount reabsorbed by the kidneys and is based upon sodium and creatinine concentrations in the serum and urine. Furthermore, it has been shown by Angeli and associates that serum sodium levels less than 130 mmol/L are associated with complications such as HRS (odds ratio=3.45), hepatic encephalopathy (odds ratio=3.40), and SBP (odds ratio=2.36).16
Clinical Impact
Refractory ascites is associated with multiple comorbidities characteristic of patients who have failed standard treatment for ascites. However, specific morbidity and mortality data for refractory ascites are not available. The data currently available are based upon patient populations with ascites and cirrhosis. Further studies are required to determine the clinical impact of these complications in patients with only refractory ascites.
Dilutional Hyponatremia
Dilutional hyponatremia develops in the presence of ascites when serum sodium levels are less than 130 mmol/L.8 This condition occurs in 30% of patients with ascites and is associated with poor survival.8 It has been shown that hyponatremia increases the risk of death in patients with cirrhosis and ascites, and serum levels less than 125 mEq/L increase the risk of mortality by 48% in these patients.17,18
The development of dilutional hyponatremia involves several mechanisms. Splanchnic vasodilation and subsequent activation of the SNS and RAAS cause sodium and water retention, as well as expansion of extracellular volume.1 As a result, absorption of sodium in the proximal tubule, loop of Henle, and distal renal tubule increases; nonosmotic vasopressin production increases; and urine sodium may decrease to less than 10 mEq/L.3 It has also been observed that decreased prostaglandin production (particularly prostaglandin E2) prevents free water excretion, contributing to dilutional hyponatremia. Continuous sodium and water retention in the intravascular system by these different mechanisms lead to dilutional hyponatremia.1,8
Moreover, the presence of dilutional hyponatremia predicts poor prognosis in patients with cirrhosis. Several studies have shown that sodium enhances the model for end-stage liver disease (MELD) score’s ability to predict mortality (Table 3).17,19-23 Hyponatremia is usually associated with higher inpatient mortality, and patients are more likely to present with other complications of portal hypertension such as hepatic encephalopathy and SBP because of the presence of advanced liver disease.16,24
Table 3.
Impact of Hyponatremia on Survival
| Month | Study | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Luca et al.22 | Heuman et al.20 | Ruf et al.17 | Wong et al.19 | Londono et al.23 | Huo et al.21 | |||||||
| MELD | iMELD | MELD | MELD-AS | MELD | MELD-NA | MELD | MELD-NA | MELD | MELD-NA | MELD | MESO | |
| iMELD=integrated model for end-stage liver disease; MELD=model for end-stage liver disease; MELD-AS=MELD-ascites sodium | [MELD + 4.53 × (sodium <135 mEq/L × 0.1) + 4.46 × (persistent ascites × 0.1)]; MELD-NA=MELD with sodium integrated; | MESO=model for end-stage liver disease/sodium ratio. | ||||||||||
| 3 | 0.894 | 0.905 | 0.72 | 0.75 | 0.79 | 0.83 | 0.78 | 0.795 | ||||
| 6 | 0.809 | 0.863 | ||||||||||
| 12 | 0.69 | 0.78 | 0.75 | 0.79 | 0.77 | 0.77 | ||||||
The management of dilutional hyponatremia is reserved for severely symptomatic cases. Dilutional hyponatremia alone may not cause symptoms because it develops slowly, giving the brain time to adapt.2 The severity of symptoms is related to the degree and potential rate at which hyponatremia develops. Patients with hyponatremia rarely have specific symptoms. If present, affected patients present with fatigue and even confusion. Therefore, when sodium levels are no more than 120 mEq daily, patients may be treated with fluid restriction.1 Hypertonic saline is not recommended for fear of precipitating central pontine myelinolysis.
Hepatorenal Syndrome
HRS results from continuous sodium and water retention caused by increased production of vasoactive substances activated by splanchnic vasodilation in the setting of severe liver disease. Approximately 10% of patients with acute renal failure or advanced cirrhosis will present with HRS.8,25 The survival rate of patients presenting with this condition is poor, particularly those with HRS type 1, given that creatinine doubles in less than 2 weeks. The development of HRS increases mortality when compared to refractory ascites alone (Figure 1).25
Figure 1.
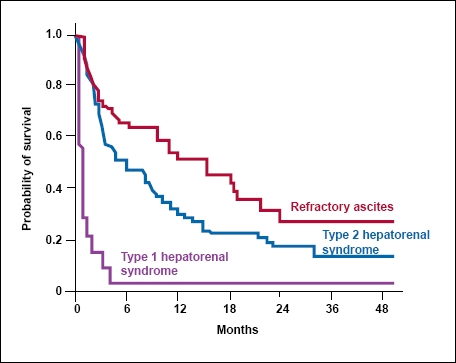
Probability of patient survival in patients with cirrhosis and refractory ascites, hepatorenal syndrome 1, and hepatorenal syndrome 2.
Reproduced from Gines P, et al. with permision.25
Vasoconstriction leads to renal hypoperfusion and decreased estimated glomerular filtration rate (GRF), further reducing vasodilator production (prostaglandin E2, nitric oxide, and so on) in the renal vascular bed.1,26 The major characteristics of HRS include a creatinine level of at least 1.5 mg/dL or a decrease in GFR of no more than 40 mL/min in less than 24 hours.1,27 Other findings include proteinuria of less than 500 mg daily and continuous renal failure after stopping diuretics in the absence of other precipitating factors.1
HRS is divided into two types: type 1 and type 2. Type 1 is defined as acute deterioration of the kidneys, with a mortality rate of 80% within 2 weeks of onset. Type 1 HRS is manifested by rapidly rising creatinine levels to more than 2.5 mg/dL, with the level approximately doubling from the patient’s baseline.26 Patients may also present with a 50% decrease of 24-h creatinine clearance from baseline to less than 20 mL/min in less than 2 weeks.9,26 HRS type 1 is associated with SBP in 20% of patients with dilutional hyponatremia. Type 1 HRS is associated with type 2 HRS, the more common type of HRS, which is defined by the slow progression of mild renal insufficiency (creatinine >1.5 mg/ dL) and moderate ascites, with a survival rate of up to 6 months.9,26 Type 2 HRS is often associated with refractory ascites.
The goal of therapy is to reverse splanchnic vasodilation and renal vasoconstriction. Initially, diuretics should be discontinued to prevent worsening of renal failure.26 A combination of vasoconstricting agents in conjunction with albumin infusion has been shown to increase survival by reversing splanchnic arterial vasodilation.1 Some authors report effectiveness in up to two thirds of cases.9,25 Vasoconstrictors such as a vasopressin agonist (terlipressin) or alpha adrenergic agonists (midodrine or noradrenaline) are the main drugs studied. Midodrine in combination with octreotide improves renal perfusion and blocks splanchnic vasodilators, redistributing blood volume. Midodrine 7.5–12.5 mg three times daily in combination with octreotide 100–200 μg three times daily, or terlipressin 0.5–2.0 mg every 4–12 hours for 5–15 days, has been shown to decrease the serum creatinine level to no more than 1 mg/dL and bring serum sodium concentration to near normal.9,28 The use of terlipressin has shown significant improvement of renal function (in 60–75% of patients), increasing survival.25,26
When albumin is used with these agents, it maintains systemic plasma volume expansion. It is known to improve renal function by increasing oncotic pressure, consequently increasing total blood volume. The treatment effect of this therapy is maintained after treatment cessation. The infusion rate of albumin consists of 1.5 g/kg, followed by 1 g/kg two days later.9 Lastly, TIPS has shown to improve renal function in patients with HRS, but further studies are required in order to determine its long-term impact on survival.26
Spontaneous Bacterial Peritonitis
The prevalence of SBP in refractory ascites is believed to be higher than in cirrhotic patients. SBP occurs in 10–30% of cirrhotic hospitalized patients, with a mortality rate of approximately 20%,29 and 13–60% of patients will develop SBEM. Patients who develop SBP are at risk for recurrence, at a rate of 69% in 1 year.30
SBP is believed to develop from bacterial translocation from gut flora. Portal hypertension, volume overload, reticuloendothelial system impairment, and malnourishment in patients with refractory ascites increase intestinal wall permeability. In addition, ascites fluid has low complement levels and a decreased number of phagocytes contributing to bacterial translocation to the blood stream and ascites fluid.30
The clinical manifestation of SBP may be abdominal pain, tense abdomen, fever, progressive encephalopathy, or none of these symptoms. The diagnosis is often based upon the presence of hepatic encephalitis, leukocytosis, and renal impairment, but confirmatory diagnosis is required via abdominal paracentesis. The most common organisms found in ascitic fluid are Escherichia coli, Staphylococcus aureus, Streptococcus viridans, and Enterococcus sp.31 When more than two organisms are identified, secondary bacterial peritonitis is suspected, and further studies are suggested to rule out bowel perforation. Hospitalization of the patient is prompted when ascites fluid in the presence of SBP is found to have a polymor-phonuclear leukocyte count greater than 250 cells/μL, a white cell count of at least 500 cells/μL, and a protein concentration of no more than 1 g/dL.29,30
SBP is treated with a third-generation cephalosporin such as cefotaxime 2 g intravenous every 8 hours or ampicillin 8–14 mg intravenous every 3–4 hours for 10–14 days. Use of gentamycin is associated with renal failure in patients with cirrhosis and is thus avoided. Prophy-laxis treatment with ciprofloxacin, norfloxacin, or sulfamethoxazole/trimethoprim (Bactrim DS, Mutual) is recommended in patients with an ascites fluid protein level of less than 1 g/dL, a history of upper gastrointestinal bleeding, or a previous episode of SBP.32,33 The rate of recurrence of SBP is 40–70%, and the 1-year mortality rate is 50–70%.34 In addition, if clinical presentation does not improve in the first 48 hours, further evaluation is required to rule out bowel perforation or intra-abdominal abscess.
Finally, approximately 30% of patients with SBP develop renal failure secondary to the accumulation of bacterial toxins, inflammatory reactants, and the hemodynamic imbalance already present. The addition of renal failure in the setting of SBP and refractory ascites increases the risk of HRS and mortality.26 It has been shown that the decline in renal function can be prevented by the administration of an albumin infusion in addition to the antibiotic therapy for SBP.26,35 Patients can be treated with 1.5 g/kg albumin followed by 1 g/kg 3 days after the first infusion, decreasing the risk of HRS.26,29,35
Hepatic Hydrothorax
The development of pleural effusion in the absence of cardiac or pulmonary disease in patients with severe cirrhosis and ascites occurs in 6–10% of patients.36 Hepatic hydrothorax is defined as the presence of pleural fluid greater than 500 mL in a patient with cirrhosis. The accumulation of ascites fluid in the pleural space occurs 85% of the time on the right, 13% on the left, and 2% bilaterally.36 Ascites fluid accumulation into the pleural space is primarily believed to occur by diffusion of peritoneal fluid through diaphragmatic defects or transdiaphragmatic lymphatics.36,37
The increased intra-abdominal pressure forces fluid into the pleural space through microscopic defects in the diaphragm. Concurrently, the diaphragm is stretched by the high pressure in the abdomen, creating blebs, and with the progression of ascites, they may rupture, contributing to the accumulation of fluid into the pleural space. As a result, severe dyspnea, dry cough, pleuritic chest pain, cardiac tamponade, and empyema may develop. Empyema increases the mortality rate to 20% yearly.36
Reversing ascites and preventing complications from hepatic hydrothorax are the goals of management.38 The resolution and prevention of recurrence is accomplished by decreasing the pressure in the abdominal cavity, adhering to a low-salt diet, and using therapeutic thoracentesis.36,38 Initial relief of symptoms can occur by draining ascites from the abdomen. However, if symptoms do not improve, thoracentesis can be performed. Patients requiring thoracentesis more than every 2–3 weeks may require TIPS to help decrease portal pressure and, therefore, improve sinusoidal drainage of lymph into the thoracic duct.38 Although TIPS is successful in most patients (60–70%),29 shunt stenosis occurs in 75% of patients.9 Finally, TIPS and video-assisted thoracoscopy are temporary measures prior to liver transplantation.36
Some physicians believe that fluid collected from thoracentesis and paracentesis should be compared before making the diagnosis of hepatic hydrothorax to ascertain that refractory ascites is the only causative agent contributing to this diagnosis. Both fluids will present with a low protein count, and albumin, cholesterol, and total lipid levels may be higher in the pleural fluid.36
Finally, surgical interventions (ie, pleurodesis and video-assisted thoracoscopy) to repair diaphragmatic defects are reserved for a select group of patients with refractory hepatic hydrothorax.36 The success rate of these procedures is controversial and varies from 48% to 75%, with some studies presenting high mortality rates.36 Further studies are required to establish survival benefits.
Spontaneous Bacterial Empyema
SBEM is defined as an infection of a preexisting pleural effusion (hydrothorax) in a patient with cirrhosis. Approximately 13–60% of cirrhosis cases are associated with SBP. The responsible microorganisms are similar to those associated with SBP: E. coli, Klebsiella, and the Streptococcus and Enterococcus sp.36,39,40 Patients with SBEM have a lower level of C3 and total protein.36 SBEM may occur in the absence of peritonitis, considering that phagocytosis may be more severely impaired in the pleural cavity. SBEM is treated similarly to SBP with intravenous third-generation cephalosporin, cefotaxime, 2 g every 8 hours for 7–10 days.36
Umbilical Hernia
Umbilical hernias occur in 20% of cirrhotic patients with ascites41 secondary to the increased intra-abdominal pressure contributing to omentum rupture at the umbilicus.
Increased intra-abdominal pressure from the ascites causes stretching of the umbilical ring. An umbilical hernia is then formed with bulging of the omentum and bowel through the abdominal wall fascia and umbilical ring, forming a pouch. Patients with cirrhosis and umbilical hernias can also be at risk of inguinal hernia development from increased intra-abdominal pressures.
When an umbilical hernia develops in a patient with refractory ascites, the first step is to decrease intra-abdominal pressure by paracentesis. However, the segment of bowel or omentum may become trapped in the pouch after large-volume paracentesis, leading to an incarcerated hernia.42
In patients with refractory ascites, elective surgery is best avoided because of the risk of fluid leakage and infection. Mortality with even umbilical herniorrhaphy ranges from 15% to 30%.43 In order to gain control of blood flow intra-operatively, patients are submitted to multiple pre-operative paracenteses.43
In addition, as patients with ascites present with coagulopathy and fragile immune systems, the procedure, which is normally low risk in healthy patients, becomes delicate in patients with ascites. Perioperative complications include incarceration, strangulation, leakage of ascites fluid, SBP, infection, or necrosis of abdominal wall secondary to vasoconstriction. Although variceal bleed may occur after surgery, sepsis remains the major cause of death.43
Survival
Refractory ascites is associated with high mortality, with rates as high as 50% at 6– 12 months postdiagnosis.3,4,44 Indeed, the survival rate in patients with normal liver function and normal sodium could be as high as 80% at 3 years.7 Furthermore, recent studies have revealed that individual patients with normal hepatic function, plasma sodium levels, and refractory ascites who undergo TIPS can significantly improve transplant-free survival when compared to patients who receive large-volume paracentesis (P=.035).7 Furthermore, high levels of plasma renin, norepinephrine, and hypotension are markers of poor prognosis.31
Patients with worse outcomes are between 50 and 60 years of age, have renal insufficiency, are on mechanical ventilation, have HRS (type 1 > type 2),9 have been diagnosed with hepatocellular carcinoma, are diabetic, and/or are heavy alcohol drinkers.3,4,16,43 The development of HRS remains the highest contributor to mortality in patients presenting with ascites. The long-term survival rate for patients with HRS is 60% at 3 years after transplantation.30 This rate is only slightly less than the survival rate for patients without HRS and transplantation. However, any complication in addition to refractory ascites increases mortality drastically.
Variations on the MELD score may improve accuracy in predicting survival. For example, the MELD/sodium ratio (MESO), integrated MELD (iMELD), and MELD with sodium integrated (MELD-NA) scores appear to significantly improve survival prediction (Table 3).17,19-22
Furthermore, age and MELD score can be used to predict survival of patients with ascites requiring major surgery. Emergency surgery was found to be an independent predictor of postoperative hospitalization.45
Management
Refractory ascites is associated with multiple comorbidities characteristic of patients who have failed standard treatment for ascites. Multiple approaches have been developed to control portal hypertension, thus decreasing ascites (Figure 2).46
Figure 2.
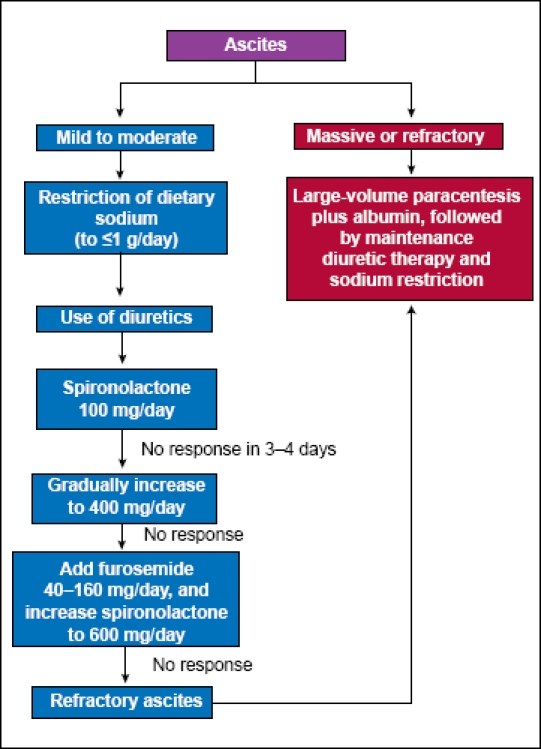
Management of refractory ascites. The maximal dose of spironolactone is 400 mg per day.46 Patients with refractory ascites should be considered for liver transplantation.
Initially, patients should be evaluated for compliance with a restricted salt diet (≤90 mmol/d)25,30 by collecting 24-h urine or recording urine sodium to potassium ratio, and daily weights.30 Daily weight loss should be limited to 0.5 kg daily to avoid hypovolemia. Free water restriction, though still practiced by many physicians when patients have ascites and hyponatremia, is controversial because it may cause hypovolemia, further increasing vasopressin and RAAS.25,30 Finally, a thorough dietary history should be obtained, as patients may be inadvertently consuming a high-salt diet, as shown by a recent case report whose detailed history-taking revealed elevated sodium consumption by patients.47
The survival rate of patients with refractory ascites is poor, as mentioned earlier, and the quality of life of these patients has little or no improvement with only diuretic management. Currently accepted nonmedical treatments for refractory ascites involve procedures such as large-volume paracentesis, TIPS, and liver transplantation. These procedures are directed toward improving quality of life, and recent studies have shown increased survival not only after liver transplantation but also after placement of TIPS.
Medical therapies such as aquaretics are being studied but are not yet approved by the US Food and Drug Administration for use in the United States. Some studies have shown that vasopressin 2 receptor antagonists may reverse dilutional hyponatremia.9,29,48,49
Abdominal Paracentesis
Paracentesis is commonly the first therapeutic step in the setting of refractory ascites to achieve immediate relief of intra-abdominal pressure. Paracentesis has been shown to decrease the length of hospital stay and the number of complications when compared to medical therapy alone.15,29 However, recurrence rates of ascites and the survival rate do not differ between paracentesis and diuretics.30 Large-volume paracentesis (4–6 L) and total paracentesis are equally effective, though patients presenting with an ascites volume greater than 10 L should have the paracentesis performed with at least a 2-week interim period.30,50
The indications of large-volume paracentesis are respiratory distress, umbilical hernia, or poor response to medical therapy, which is the case of patients with refractory ascites.9 The short-term effects of large-volume para-centesis were studied by Pozzi and colleagues, who noted a significant decrease of intra-abdominal, intrathoracic, right atrial, and pulmonary capillary wedge pressures. In addition, increased cardiac output was noted to be the result of decreased intra-abdominal and inferior vena cava pressures in the first 24 hours.15,29,51,52 Six days after the procedure, there was an increase in vasoconstrictive hormones, which can predispose patients to the development of circulatory dysfunction.51 Approximately 20% of large-volume paracentesis cases (over 4–6 L) are associated with postparacentesis circulatory dysfunction when not followed by volume expansion.9
Circulatory dysfunction involves the worsening of hyponatremia and hypovolemia. The decrease in vascular resistance experienced by patients after large-volume paracentesis triggers the SNS and RAAS, increasing the risk of renal failure, worsening hyponatremia, and decreasing survival.9,25 Therefore, intravenous infusion of albumin (6–8 g/L of ascites removed) usually follows large-volume paracentesis (over 4–6 L) to prevent renal perfusion impairment causing blood volume expansion.
The administration of diuretics at least 2 days after the procedure decreases the chances of ascites recurrence to 18% compared to 93% if diuretics are not continued. The administration of diuretics also shortens hospital stay and reduces the likelihood of readmission.15 A number of artificial plasma expanders have been developed to substitute for albumin, including dextrans, collagen-based colloids, and hydroxyethyl starches. To date, albumin remains the first choice of volume expanders.15,25,29,30
Furthermore, complications associated with abdominal paracentesis are rare. For instance, abdominal hematomas occur in approximately 1% of cases, and hemoperitoneum or bowel perforation occurs at rates of less than 1/1,000.29
The main contraindications to paracentesis are fibrinolysis and disseminated intravascular coagulation. Severe hemorrhage after paracentesis is rare (0.19%)53 but may cause severe complications in patients with coagulopathy (international normalization ratio [INR]>2) and thrombocytopenia (>40,000).30 Therefore, some researchers suggest correction of these parameters prior to the procedure, though coagulopathy and thrombocytopenia are not absolute contraindications.29,30 Other complications associated with paracentesis include abdominal wall hematoma (0.1%), hemoperitoneum (0.01%), infection (0.01%), and leakage of ascites fluid.30
Transjugular Intrahepatic Portosystemic Shunts
TIPS is a noninvasive method used to treat refractory ascites. This procedure decreases portosystemic pressure by creating a shunt between the hepatic vein and the portal vein, relieving intra-abdominal pressure and improving renal function. Consequently, RAAS activity decreases, improving urinary sodium excretion.3,15,54 The success rate associated with TIPS is between 75% and 90%, depending upon the local expertise.29,55
Recurrence of ascites is known to occur in patients with refractory ascites after TIPS placement. However, TIPS patients have a lower recurrence rate than those undergoing paracentesis.54 The rate of recurrence for TIPS was shown to be 42% compared to 89% for large-volume paracentesis (P<.0001) in a study.7 Furthermore, a recent study revealed that individual patients with normal hepatic function, plasma sodium levels, and refractory ascites undergoing TIPS placement can significantly improve transplant-free survival when compared to large-volume paracentesis (P=.035). A significant increase in survival rate was also demonstrated (P=.009).7 Finally, TIPS is shown to improve hydrothorax in 60–70% of patients.29
TIPS is usually indicated in patients with refractory ascites who require repeated paracentesis more than 3 times a month, have loculated ascites, or have multiple abdominal adhesions.15,25 The contraindications for TIPS include portal vein thrombosis, hepatic encephalopathy, an INR greater than 2, presence of SBP, age older than 60, ejection fraction less than 55%, and a Child-Pugh score (used for assessing prognosis of cirrhosis) greater than 12.29,30
Finally, the complications involving TIPS include intra-abdominal bleeding, hepatic encephalopathy (30%), heart failure in patients with a history of heart disease, an increase in liver function enzymes secondary to decreased blood flow to hepatocytes, and shunt stenosis (40%).11 The high incidence of hepatic encephalopathy and shunt dysfunction rates after TIPS placement remain disadvantages to this procedure (P=.006).7 After TIPS placement, heart failure may occur in patients with previous history of heart disease because of increased preload increasing work and oxygen demand on an already failing heart. However, the rate at which these complications and others occur is approximately equal to that of abdominal paracentesis.56
Liver Transplantation
Liver transplantation is the ultimate treatment for refractory ascites in patients with advanced liver disease. Unfortunately, the current system for organ allocation does not take into consideration manifestations of portal hypertension such as refractory ascites. The MELD score utilizes objective measures of serum value of creatinine, INR, and total bilirubin.17 Because of the large discrepancy between patients waiting for liver transplantation and those undergoing transplantation, many patients with refractory ascites succumb to their disease before receiving a transplant.57-59 TIPS and recurrent paracentesis are used as bridges prior to liver transplantation to control ascites. As discussed above, TIPS may be associated with acceptable survival rates in those patients with normal liver function and serum sodium levels.7
Summary
Refractory ascites is defined as ascites that does not recede after medical therapy or that reoccurs shortly after fluid has been removed from the abdominal cavity via paracentesis. Patients presenting with this condition have been on a sodium-restricted diet while maximizing diuretic doses, when appropriate, for at least 1 week. Refractory ascites also delineates the group of patients with persistent ascites who do not tolerate maximal doses of diuretics secondary to debilitating side effects such as renal failure or hepatic encephalopathy.
Patients presenting with this condition have a poor prognosis and quickly develop complications such as HRS, dilutional hyponatremia, and SBP. Furthermore, liver transplantation and TIPS are the only measures that increase survival. Liver transplantation increases survival to 85% post-transplant after ascites has been stabilized.60 The pathophysiology and treatment of refractory ascites are poorly understood. Furthermore, studies are necessary to help physicians prevent the formation of refractory ascites and to define the prevalence of complications associated with this condition. Finally, physicians must be aware of other conditions that may be disguised by ascites and lead to refractory ascites such as hepatocellular carcinoma, tuberculosis, or merely noncompliance to diet.47,61
Acknowledgments
The authors thank Cindy Lee for editorial assistance.
Contributor Information
Fabiolla Siqueira, Dr. Siqueira is a resident in the Department of Medicine at Kern Medical Center in Bakersfield, California.
Traci Kelly, Ms. Kelly is a nurse practitioner in the Division of Gastroenterology at the Digestive Health Center of Arizona in Phoenix, Arizona.
Sammy Saab, Dr. Saab serves as Associate Professor of Medicine and Surgery at the University of California at Los Angeles.
References
- 1.Arroyo V. Pathophysiology, diagnosis and treatment of ascites in cirrhosis. Ann Hepatol. 2002;1:72–79. [PubMed] [Google Scholar]
- 2.Ring-Larsen H. Therapy of Ascites and Renal Dysfunction in Cirrhosis. Malden, Massachusetts: Blackwell Co; 1999. Treatment of refractory ascites in cirrhosis; pp. 480–491. [Google Scholar]
- 3.Cardenas A, Arroyo V. Refractory ascites. Dig Dis. 2005;23:30–38. doi: 10.1159/000084723. [DOI] [PubMed] [Google Scholar]
- 4.Moreau R, Delègue P, Pessione F, Hillaire S, Durand F, et al. Clinical characteristics and outcome of patients with cirrhosis and refractory ascites. Liver Int. 2004;24:457–464. doi: 10.1111/j.1478-3231.2004.0991.x. [DOI] [PubMed] [Google Scholar]
- 5.Guardiola J, Baliellas C, Xiol X, Fernandez Esparrach G, Ginès P, et al. External validation of a prognostic model for predicting survival of cirrhotic patients with refractory ascites. Am J Gastroenterol. 2002;97:2374–2378. doi: 10.1111/j.1572-0241.2002.05928.x. [DOI] [PubMed] [Google Scholar]
- 6.Saab S, Nguyen S, Ibrahim A, Vierling JM, Tong MJ. Management of patients with cirrhosis in Southern California: Results of a practitioner survey. J Clin Gastroenterol. 2006;40:156–161. doi: 10.1097/01.mcg.0000196189.65167.53. [DOI] [PubMed] [Google Scholar]
- 7.Salerno F, Cammà C, Enea M, Rössle M, Wong F. Transjugular intrahepatic portosystemic shunt for refractory ascites: a metanalysis of individual patient data. Gastroenterology 2007133825–834. [DOI] [PubMed] [Google Scholar]
- 8.Cardenas A, Arroyo V. Mechanism of water and sodium retention in cirrhosis and the pathogenesis of ascites. Best Pract Res Clin Endocrinol Metab. 2003;17:607–622. doi: 10.1016/s1521-690x(03)00052-6. [DOI] [PubMed] [Google Scholar]
- 9.Sandhu BS, Sanyal AJ. Management of ascites in cirrhosis. Clin Liver Dis. 2005;9:715–732. doi: 10.1016/j.cld.2005.07.008. [DOI] [PubMed] [Google Scholar]
- 10.Arroyo V, Ginès P, Gerbes AL, Dudley FJ, Gentilini P, et al. Definition and diagnostic criteria of refractory ascites and hepatorenal syndrome in cirrhosis. Hepatology. 1996;23:164–176. doi: 10.1002/hep.510230122. [DOI] [PubMed] [Google Scholar]
- 11.Zervos EE, Rosemurgy AS. Management of medically refractory ascites. Am J Surg. 2001;181:256–264. doi: 10.1016/s0002-9610(01)00565-7. [DOI] [PubMed] [Google Scholar]
- 12.Mamie H, Dong M, Saab S. Complications of cirrhosis. Dis Mon. 2008;54:445–456. doi: 10.1016/j.disamonth.2008.03.006. [DOI] [PubMed] [Google Scholar]
- 13.Arroyo V, Gines P. Mechanism of sodium retention and ascites formation in cirrhosis. J Hepatol. 1993;17(2):S24–S28. doi: 10.1016/s0168-8278(05)80451-9. [DOI] [PubMed] [Google Scholar]
- 14.Sieber CC, Lopez-Talavera JC, Groszmann RJ. Role of nitric oxide in the in vitro splanchnic vascular hyporeactivity in ascitic cirrhotic rats. Gastroenterology. 1993;104:1750–1754. doi: 10.1016/0016-5085(93)90655-v. [DOI] [PubMed] [Google Scholar]
- 15.Moore KP, Wong F, Gines P, Bernardi M, Ochs A, et al. The management of ascites in cirrhosis: Report on the consensus conference of the International Ascites Club. Hepatology. 2003;38:258–266. doi: 10.1053/jhep.2003.50315. [DOI] [PubMed] [Google Scholar]
- 16.Angeli P, Wong F, Watson H, Ginès P. CAPPS Investigators. Hyponatremia in cirrhosis: Results of a patient population survey. Hepatology. 2006;44:1535–1542. doi: 10.1002/hep.21412. [DOI] [PubMed] [Google Scholar]
- 17.Ruf AE, Kremers WK, Chavez LL, Descalzi VI, Podesta LG, Villamil FG. Addition of serum into the MELD score predicts waiting list mortality better than MELD alone. Liver Transpl. 2005;11:336–343. doi: 10.1002/lt.20329. [DOI] [PubMed] [Google Scholar]
- 18.Borroni G, Maggi A, Sangiovanni A, Cazzaniga M, Salerno F. Clinical relevance of hyponatremia for the hospital outcome of cirrhotic patients. Dig Liver Dis. 2000;32:605–610. doi: 10.1016/s1590-8658(00)80844-0. [DOI] [PubMed] [Google Scholar]
- 19.Wong VW, Chim AM, Wong GL, Sung JJ, Chan HL. Performance of the new MELD-Na score in predicting 3 month and 1 year mortality in Chinese patients with chronic hepatitis B. Liver Transpl. 2007;13:1228–1235. doi: 10.1002/lt.21222. [DOI] [PubMed] [Google Scholar]
- 20.Heuman DM, Abou-Assi SG, Habib A, Williams LM, Stravitz RT, et al. Persistent ascites and low serum sodium identify patients with cirrhosis and low MELD scores who are at high risk for early death. Hepatology. 2004;40:802–810. doi: 10.1002/hep.20405. [DOI] [PubMed] [Google Scholar]
- 21.Huo T, Lee SD, Lin HC. Selecting an optimal prognostic system for liver cirrhosis: The model for end-stage liver disease and beyond. Liver Int. 2008;28:606–613. doi: 10.1111/j.1478-3231.2008.01727.x. [DOI] [PubMed] [Google Scholar]
- 22.Luca A, Angermayr B, Bertolini G, Koenig F, Vizzini G, et al. An integrated MELD model including serum sodium and age improves the prediction of early mortality in patients with cirrhosis. Liver Transpl. 2007;13:1174–1180. doi: 10.1002/lt.21197. [DOI] [PubMed] [Google Scholar]
- 23.Londono MC, Cárdenas A, Guevara M, Quintó L, de Las Heras D, et al. MELD score and serum sodium in the prediction of survival of patients with cirrhosis awaiting liver transplantation. Gut. 2007;56:1283–1290. doi: 10.1136/gut.2006.102764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Saab S, Landaverde C, Ibrahim A. The MELD score in advanced liver disease: association with clinical portal hypertension and mortality. Exp Clin Transplant. 2006;4:395–399. [PubMed] [Google Scholar]
- 25.Gines P, Cardenas A, Arroyo V. Management of ascites and cirrhosis. N Engl J Med. 2004;350:1646–1654. doi: 10.1056/NEJMra035021. [DOI] [PubMed] [Google Scholar]
- 26.Turban S, Thuluvath PJ, Atta MG. Hepatorenal syndrome. World J Gastroenterol. 2007;13:4046–4055. doi: 10.3748/wjg.v13.i30.4046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Salerno F, Gerbes A, Ginès P, Wong F, Arroyo V. Diagnosis, prevention and treatment of hepatorenal syndrome in cirrhosis. Gut. 2007;56:1310–1318. doi: 10.1136/gut.2006.107789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wong F, Pantea L, Sniderman K. Midodrine, octreotide, albumin, and TIPS in selected patients with cirrhosis and Type 1 hepatorenal syndrome. Hepatology. 2004;40:55–64. doi: 10.1002/hep.20262. [DOI] [PubMed] [Google Scholar]
- 29.Moore KP, Aithal GP. Guidelines on the management of ascites in cirrhosis. Gut. 2006;55:1–12. doi: 10.1136/gut.2006.099580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yeung E, Wong FS. The management of cirrhotic ascites. MedGenMed. 2002;4:8. [PubMed] [Google Scholar]
- 31.Chavez-Tapia NC, Soares-Weiser K, Brezis M, Leibovici L. Antibiotics for spontaneous bacterial peritonitis in cirrhotic patients. Cochrane Database Syst Rev. 2009;1 doi: 10.1002/14651858.CD002232.pub2. CD002232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Runyon B. Early events in spontaneous bacterial peritonitis. Gut. 2004;53:782–784. doi: 10.1136/gut.2003.035311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Alaniz C, Regal RE. Spontaneous bacterial peritonitis: a review of treatment options. PT. 2009;34:204–210. [PMC free article] [PubMed] [Google Scholar]
- 34.Ghassemi H, Garcia-Tsao G. Prevention and treatment of infections in patients with cirrhosis. Best Pract Res Clin Gastroenterol. 2007;21:77–93. doi: 10.1016/j.bpg.2006.07.004. [DOI] [PubMed] [Google Scholar]
- 35.Sort P, Navasa M, Arroyo V, Aldeguer X, Planas R, et al. Effect of intravenous albumin on renal impairment and mortality in patients with cirrhosis and spontaneous bacterial peritonitis. N Engl J Med. 1999;341:403–409. doi: 10.1056/NEJM199908053410603. [DOI] [PubMed] [Google Scholar]
- 36.Kiafar C, Nooman G. Hepatic hydrothorax: Current concepts of pathophysiology and treatment options. Ann Hepatol. 2008;7:313–320. [PubMed] [Google Scholar]
- 37.Lieberman FL, Hidemura R, Peters RL, Reynolds TB. Pathogenesis and treatment of hydrothorax complicating cirrhosis with ascites. Ann Intern Med. 1966;64:341–351. doi: 10.7326/0003-4819-64-2-341. [DOI] [PubMed] [Google Scholar]
- 38.Rodriguez-Roisin R, Krowka MJ. Hepatopulmonary syndrome: A liver induced lung vascular disease. N Engl J Med. 2008;358:2378–2387. doi: 10.1056/NEJMra0707185. [DOI] [PubMed] [Google Scholar]
- 39.Behnia M, Clay AS, Hart CM. Enterococcus faecalis causing empyema in a patient with liver disease. South Med J. 2002;95:1201–1203. [PubMed] [Google Scholar]
- 40.Strauss RM, Sawyer TO. Hepatic hydrothorax. Semin Liver Dis. 1997;17:227–231. doi: 10.1055/s-2007-1007200. [DOI] [PubMed] [Google Scholar]
- 41.Perkins JD. Another patient with an umbilical hernia and massive ascites: What to do? Liver Transpl. 2008;14:110–114. doi: 10.1002/lt.21390. [DOI] [PubMed] [Google Scholar]
- 42.Marsman HA, Heisterkamp J, Halm JA, Tilanus HW, Metselaar HJ, Kazemier G. Management in patients with liver cirrhosis and an umbilical hernia. Surgery. 2007;142:372–375. doi: 10.1016/j.surg.2007.05.006. [DOI] [PubMed] [Google Scholar]
- 43.O’Hara ET, Oliai A, Patek AJ, Jr, Nabseth DC. Management of umbilical hernias associated with hepatic cirrhosis and ascites. Ann Surg. 1975;181:85–87. doi: 10.1097/00000658-197501000-00018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Suzuki H, Stanley AJ. Current management and novel therapeutic strategies for refractory ascites and hepatorenal syndrome. QJM. 2001;94:293–300. doi: 10.1093/qjmed/94.6.293. [DOI] [PubMed] [Google Scholar]
- 45.Teh SH, Nagorney DM, Stevens SR, Offord KP, Therneau TM, et al. Risk factors for mortality after surgery in patients with cirrhosis. Gastroenterology. 2007;132:1261–1269. doi: 10.1053/j.gastro.2007.01.040. [DOI] [PubMed] [Google Scholar]
- 46.Poryako MK, Weisner RH. Management of ascites in patients with cirrhosis. What to do when diuretics fail. Postgrad Med. 1992;92:155–166. doi: 10.1080/00325481.1992.11701557. [DOI] [PubMed] [Google Scholar]
- 47.Riley TR. Two cases of refractory ascites: Associated with dill pickle ingestion. Dig Dis Sci. (3) 2000;45:1119–1120. doi: 10.1023/a:1005506220369. [DOI] [PubMed] [Google Scholar]
- 48.Wong F, Blei AT, Blends LM, Thuluvath PJ. A vasopressin receptor antagonist (VPA-985) improves serum sodium concentration in patients with hyponatremia: A multicenter, randomized, placebo-controlled trial. Hepatology. 2003;37:182–191. doi: 10.1053/jhep.2003.50021. [DOI] [PubMed] [Google Scholar]
- 49.Ginès P, Wong F, Watson H, Milutinovic S, del Arbol LR, et al. Effects of satavaptan, a selective vasopressin V2 receptor antagonist, on ascites and serum sodium in cirrhosis with hyponatremia: a randomized trial. Hepatology. 2008;48:204–213. doi: 10.1002/hep.22293. [DOI] [PubMed] [Google Scholar]
- 50.Titó L, Ginès P, Arroyo V, Planas R, Panés J, et al. Total paracentesis associated with intravenous albumin infusion management of patients with cirrhosis and ascites. Gastroenterology. 1990;98:146–151. doi: 10.1016/0016-5085(90)91303-n. [DOI] [PubMed] [Google Scholar]
- 51.Umgelter A, Reindl W, Franzen M, Lenhardt C, Huber W, Schmid RM. Renal resistive index and renal function before and after paracentesis in patients with hepatorenal syndrome and tense ascites. Intensive Care Med. 2009;35:152–156. doi: 10.1007/s00134-008-1253-y. [DOI] [PubMed] [Google Scholar]
- 52.Pozzi M, Osculati G, Boari G, Serboli P, Colombo P, et al. Time course of circulatory and humoral effects of rapid total paracentesis in cirrhotic patients with tense, refractory ascites. Gastroenterology. 1994;106:709–719. doi: 10.1016/0016-5085(94)90706-4. [DOI] [PubMed] [Google Scholar]
- 53.Pache I, Bilodeau M. Severe haemorrhage following abdominal paracentesis for ascites in patients with liver disease. Aliment Pharmacol Ther. 2005;21:525–529. doi: 10.1111/j.1365-2036.2005.02387.x. [DOI] [PubMed] [Google Scholar]
- 54.Campbell MS, Brensinger CM, Sanyal AJ, Gennings C, Wong F, et al. Quality of life in refractory ascites: Transjugular intrahepatic portal-systemic shunting versus medical therapy. Hepatology. 2005;42:635–640. doi: 10.1002/hep.20840. [DOI] [PubMed] [Google Scholar]
- 55.Boyer TD. Transjugular intrahepatic portosystemic shunt in the management of complications of portal hypertension. Curr Gastroenterol Rep. 2008;10:30–35. doi: 10.1007/s11894-008-0006-y. [DOI] [PubMed] [Google Scholar]
- 56.Saab S, Nieto JM, Lewis SK, Runyon BA. TIPS versus paracentesis for cirrhotic patients with refractory ascites. Cochrane Database Syst Rev. 2004;(3) doi: 10.1002/14651858.CD004889.pub2. CD004889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Landaverde C, Saab S. Deciding liver transplant candidacy: Tools of the trade. Liver Int. 2008;28:1186–1189. doi: 10.1111/j.1478-3231.2008.01854.x. [DOI] [PubMed] [Google Scholar]
- 58.Sharma P, Rakela J. Management of pre–liver transplantation patient—Part 2. Liver Transpl. 2005;11:249–260. doi: 10.1002/lt.20379. [DOI] [PubMed] [Google Scholar]
- 59.Busuttil RW, Farmer DG, Yersiz H. Analysis of long term outcomes of 3200 liver transplantation over two decades. Ann Surg. 2005;241:905–918. doi: 10.1097/01.sla.0000164077.77912.98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Rimola A, Navasa M, Grande L. Therapy of Ascites and Renal Dysfunction in Cirrhosis. Malden, Massachusetts: 1999. Liver transplantation in cirrhotic patients with ascites; pp. 522–527. [Google Scholar]
- 61.Runyon A. Management of adult patients with ascites due to cirrhosis. Hepatology. 2004;39:1–16. doi: 10.1002/hep.20066. [DOI] [PubMed] [Google Scholar]


