Gastrinomas are the most common type of pancreatic neuroendocrine tumor and are usually located in the duodenum or pancreas, within the borders of the gastrinoma triangle. Sporadic gastri-nomas—those not associated with multiple endocrine neoplasia type 1 (MEN 1)—have been reported in other locations, but such ectopic gastrinomas are rare. Primary hepatic gastrinomas are exceedingly rare, with less than 20 reported cases in the literature. In this report, we discuss a patient with a primary hepatic gastrinoma that eluded diagnosis for more than one decade and was cured by surgical resection. Included in the discussion is a brief review of the tests used to localize gastrinomas in patients with suspected Zollinger-Ellison syndrome (ZES) as well as the usual approach to treatment of sporadic gastrinomas.
Case Report
A 46-year-old African-American woman with sickle-cell disease presented with melena. The patient was hemodynamically stable and had a benign abdominal examination. Hemoglobin measured 8 g/dL, and serum chemistry showed an elevated blood urea nitrogen of 43 mg/dL. The other blood and biochemical parameters were within their respective reference ranges. The patient was treated with intravenous pantoprazole and received a blood transfusion.
Esophagogastroduodenoscopy showed severe erosive esophagitis (Los Angeles class D), enlarged rugal folds in the stomach, and a 2-cm ulcer in the third portion of the duodenum, with an overlying clot. A Roth Net was used to remove the clot, revealing two visible nonbleeding vessels. To prevent rebleeding, 2 Resolution clips were successfully deployed (Figure 1).
Figure 1.
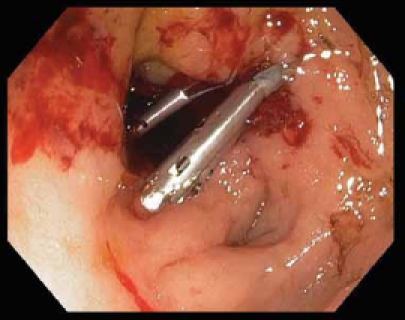
Large ulcer in the third portion of the duodenum revealing 2 visible vessels after removal of overlying clot. Treated with hemoclips.
The patient had not been taking nonsteroidal antiinflammatory drugs, and serologic testing for Helicobacter pylori infection was negative. A fasting gastrin level, taken on the following morning (while on pantoprazole), measured 3,120 pg/mL. Serum calcium, phosphorous, parathyroid hormone, and prolactin levels were all within their respective reference ranges.
Upon further review, the patient had a 20-year history of heartburn, dyspepsia, watery diarrhea, and nausea. She was uninsured and lacked routine primary care. She had not been taking her acid suppressive therapy recently and had developed intermittent solid food dysphagia and anorexia, resulting in a 5-kg weight loss over the preceding year. Upon review of the medical records at our institution, the patient had made several visits to our emergency department over the previous 15 years for abdominal pain. Basic laboratory work was generally unrevealing during these visits, but imaging studies included an ultrasound in 1995 that showed a 1.3 cm × 1.5 cm lesion in the left lobe of the liver that was thought to be a hemangioma; an abdominal computed tomography scan in 2004 that showed a 2.5 cm × 2.6 cm lesion in the left lobe of the liver; and an abdominal ultrasound in 2005 that showed a similar lesion measuring 2.5 cm × 2.6 cm. At that time, magnetic resonance imaging was recommended, but not performed.
After 72 hours of intravenous proton pump inhibitor therapy, the patient began to eat, her dysphagia resolved, and she regained her appetite. She was placed on 60 mg of oral pantoprazole twice daily. Magnetic resonance imaging was performed and showed a 4.1 cm × 3.5 cm well-circumscribed mass in the left lobe of the liver (Figure 2). Somatostatin-receptor scintigraphy showed a focus of markedly increased octreotide uptake in the left hepatic lobe corresponding to the lesion seen on magnetic resonance imaging and consistent with a neuroendocrine tumor (Figure 3). Endoscopic ultrasonography showed several very mildly enlarged lymph nodes in the periportal region but no other lesions in the gastrinoma triangle or pancreas. Fine-needle aspiration of the periportal lymph nodes showed normal tissue.
Figure 2.
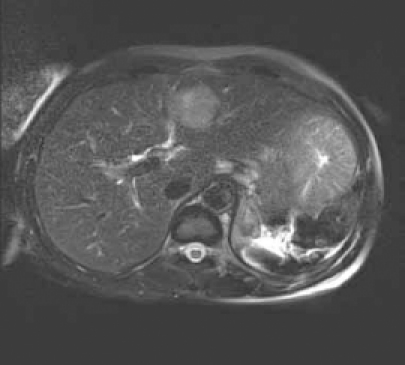
Magnetic resonance image showing a 4.1 cm × 3.5 cm well-circumscribed mass in the left lobe of the liver.
Figure 3.

Somatostatin-receptor scintigraphy (octreotide scan) showing markedly increased octreotide uptake in the left hepatic lobe corresponding to the lesion seen on the magnetic resonance image.
An exploratory laparotomy was performed. Thorough bimanual palpation of the pancreas, intraoperative ultrasound of the pancreas, kocherization of the duodenum, and removal of several mildly enlarged periportal and omental lymph nodes did not identify evidence of alternative primary sites of the gastrinoma or evidence of metastases. Frozen sections of the lymph nodes showed normal tissue. A left lateral segmentectomy was performed to remove the liver lesion, which was not palpable intraoperatively. Pathology showed a 2.9 cm × 4.0 cm neuroendocrine tumor consistent with a gastrinoma. Stains were positive for synaptophysin and chromogranin (Figure 4).
Figure 4.
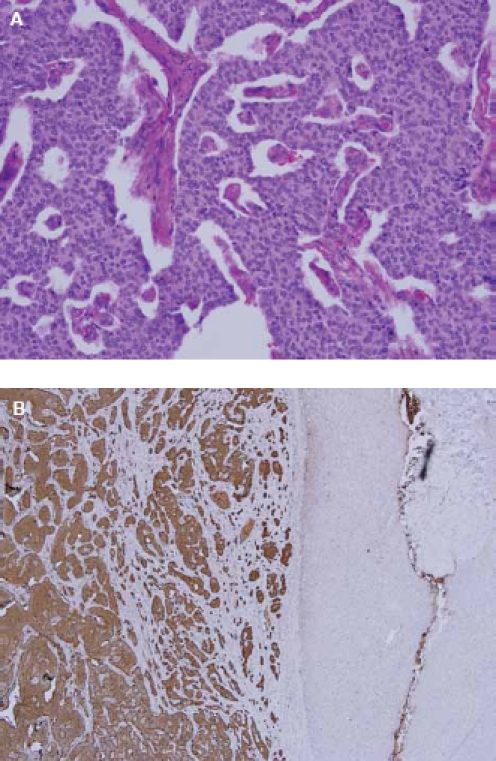
Pathology showing a 2.9 cm × 4.0 cm neuroendocrine tumor consistent with a gastrinoma. Stains were positive for synaptophysin (A) and chromogranin (B).
Thirty-six hours postoperatively, the patient's serum gastrin level was 41 pg/mL, consistent with a surgical cure of ZES. Two months postoperatively, she remains eugastrinemic (gastrin level, 55 pg/mL). The patient has dramatically improved: her symptoms have entirely resolved, she has regained 5 kg of weight, and her proton pump inhibitor therapy has now been decreased to pantoprazole 40 mg twice daily. We plan to repeat an upper endoscopy to monitor the mucosal response to acid suppression and exclude Barrett esophagus.
Discussion
ZES was first described in 1955 and affects approximately 1% of patients with peptic ulcer disease. Classically, the syndrome is characterized by primary ulcerations in atypical locations such as the second or third portions of the duodenum or jejunum; severe gastric acid hypersecretion; and the presence of a non-beta islet cell tumor of the pancreas or duodenum. However, ulcers in patients with ZES are more commonly normal in size and location (typically less than 1 cm in size and located in the duodenal bulb).1 Diarrhea in patients with gastrinomas is common and results from a variety of mechanisms, including gastric acid hypersecretion; inactivation of pancreatic enzymes (leading to steatorrhea); epithelial cell damage; and inhibition of sodium and water absorption, leading to both malabsorptive and secretory states.1 Diagnosis of a gastrinoma requires a high level of suspicion, as the presenting symptoms (diarrhea, heartburn, dyspepsia) are so common. The average time between initial presentation and diagnosis of ZES is 6–9 years.1 A markedly elevated serum gastrin level of greater than 1,000 pg/mL in the absence of achlorhydria is virtually diagnostic of a gastrinoma. Exclusion of achlorhydric conditions such as atrophic gastritis and pernicious anemia (which are much more common than gastrinomas) is essential, as severe hypergastrinemia to this degree can occur in these diseases.
If nonachlorhydric hypergastrinemia is confirmed, a secretin stimulation test is performed. The paradoxical rise of serum gastrin level in response to a secretin level of greater than 120 pg/mL is 94% sensitive and nearly 100% specific for gastrinoma (again, in the absence of achlorhy-dria).1 Although a greater than 200 pg/mL rise in gastrin has been widely considered to be a positive test, this value may offer slightly lower sensitivity.1,2 Controversial issues include whether (and if so, when) acid suppression should be stopped prior to secretin stimulation testing. Many experts believe that continuing acid suppression therapy does not alter the results of secretin provocation testing, and in some patients (particularly those with a history of complicated or perforated peptic ulcer disease), discontinuing acid suppression may be dangerous.1
A negative secretin stimulation test is extremely rare in patients with ZES. If there is a high index of suspicion for ZES and the secretin test is negative, the test can either be repeated or a calcium stimulation test can be performed. This test is used less commonly, is less sensitive (63% vs 94%), and has the potential for serious side effects from the intravenous infusion of calcium.2 However, reports of patients with ZES who test negative to secretin stimulation and positive to calcium stimulation exist. Therefore, the test is considered highly specific for gastrinoma.
When biochemical studies suggest that a gastrinoma is present, its location must be identified. A number of tests are used to localize gastrinomas, including ultrasonography, computed tomography, magnetic resonance imaging, selective arterial secretin or calcium stimulation studies, and endoscopic ultrasound (EUS). In general, a combination of these tests allows for pre-operative localization of gastrinomas in approximately 80% of cases.1,3 With the advent of EUS, the sensitivity for detecting sporadic gastrinomas prior to surgical exploration has increased to approximately 85%.4 In general, the noninvasive imaging modalities tend to have slightly higher sensitivities in patients with MEN 1.3
Although somatostatin-receptor scintigraphy (octreotide scan) is touted for its high sensitivity in localizing gastrinomas, the use of this imaging modality is highly dependent on the size of the gastrinoma, ranging from 30% for gastrinomas smaller than 1.1 cm to 96% for gastrinomas larger than 2 cm.5 In cases where noninvasive imaging is negative, EUS becomes highly valuable with the ability for real-time cytologic evaluation of primary tumors and suspicious lymph nodes. The sensitivity of EUS depends upon gastrinoma location as well, ranging from 43% for duodenal gastrinomas to 85% for pancreatic gastrinomas.4,6,7
Still, some cases require surgical exploration to locate the gastrinoma. The surgical tenets of exploration for gastrinoma include a Kocher maneuver to allow careful examination of the head of the pancreas and uncinate process, bimanual palpation of the body and tail of the pancreas, intraoperative ultrasonography, duodenotomy and exploration of the duodenal mucosa, and sampling of lymph nodes in the gastrinoma triangle.1 The definition of a biochemical cure following surgery for ZES is a normal fasting and secretin stimulated gastrin level postoperatively. The initial postoperative cure rate is approximately 60% for sporadic gastrinomas, but this figure decreases significantly to 34% at 10-year follow-up.3 In patients with gastrinomas associated with MEN 1 syndrome, disease-free survival rates are much lower and surgery remains controversial.3 Therefore, it is essential to exclude MEN 1 in patients with gastrinoma.
Approximately one third of patients with MEN 1 present with ZES initially, followed by other manifestations of MEN 1 later, usually primary hyperparathyroidism. Indeed, the first surviving ZES patient was diagnosed with hyperparathyroidism some 40 years after the initial diagnosis of ZES.8,9 Gene mutation analysis for the MEN gene is available but costly, and there are no guidelines for genetic testing in these patients. It is generally recommended that all patients with gastrinomas are screened for MEN 1 by measuring serum calcium, phosphorous, intact-parathyroid hormone, and prolactin levels. These markers should be followed after surgical resection at regular intervals to monitor for recurrence.
Medical therapy for ZES consists primarily of acid suppression therapy with high-dose proton pump inhibitors. Although the somatostatin analogue octreotide has been used with success to treat other neuroendocrine tumors, its success in treating gastrinomas has not been consistent. At present, octreotide remains a second-line therapy in ZES for treating extreme hypersecretory states leading to voluminous diarrhea and dehydration.1
Prior to the widespread use of proton pump inhibitors, most of the morbidity in ZES resulted from severe and recurrent peptic ulcerations. Partial and total gastrectomy were commonly performed, and patients frequently required multiple operations. In the post?proton pump inhibitor era, the natural history of the disease appears to have changed and studies have shown that the number of surgical procedures in these patients has dropped dramatically.8
Although proton pump inhibitors effectively treat the acid hypersecretion in patients with ZES, they may delay the diagnosis. One study showed that in the pre?proton pump inhibitor era (prior to 1985), the incidence of patients presenting with metastatic disease was 19%, with a 5-year survival of 29%, whereas in the post?proton pump inhibitor era (from 1985 to 1995), the incidence of patients presenting with metastatic gastrinomas was 55%, with a 5-year survival rate of 5%.10 This provides even more impetus for the clinician to have a high index of suspicion when evaluating patients with heartburn, abdominal pain, and diarrhea, particularly if there is a history of peptic ulcer disease.
Even with total resection of the gastrinoma, patients may continue to have gastric acid hypersecretion due to an excess of gastric parietal cells resulting from the trophic effect of gastrin preceding the resection. Approximately 40% of patients require acid suppression up to 4 years postoperatively.1 The dose of proton pump inhibitor therapy should be gradually reduced postoperatively, according to symptoms and endoscopic healing. Alternatively, the proton pump inhibitor may be dose-adjusted by measuring the basal acid output, with the goal of a basal acid output of less than 10 mEq/hr in men and less than 5 mEq/hr in women.1
Summary
This unusual case emphasizes the need for a high index of clinical suspicion in evaluating patients who present with symptoms compatible with ZES. In retrospect, our patient eluded the diagnosis of ZES for many years. Measurement of the serum gastrin level earlier would have allowed timely diagnosis and prevented significant morbidity. We plan to measure the fasting serum gastrin level at regular intervals postoperatively in this patient. The possibility of occult lymph node or other primary locations missed by EUS and surgical exploration still exists, and recurrence is possible. It is noted that a duodenotomy was not performed during the operation, and the possibility of a tiny duodenal gastrinoma was not definitively excluded. However, the rapid fall in serum gastrin level following resection of the hepatic gastrinoma argues against this.
References
- 1.Ellison EC, Johnson JA. The Zollinger-Ellison syndrome: a comprehensive review of historical, scientific, and clinical considerations. Curr Probl Surg. 2009;46:13–106. doi: 10.1067/j.cpsurg.2008.09.001. [DOI] [PubMed] [Google Scholar]
- 2.Berna MJ, Hoffmann KM, Long SH, Serrano J, Gibril F, Jensen RT. Serum gastrin in Zollinger-Ellison syndrome: II. Prospective study of gastrin provocative testing in 293 patients from the National Institutes of Health and comparison with 537 cases from the literature. Evaluation of diagnostic criteria, proposal of new criteria, and correlations with clinical and tumoral features. Medicine (Baltimore) 2006;85:331–364. doi: 10.1097/MD.0b013e31802b518c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wells SA. Surgery for Zollinger-Ellison syndrome. N Engl J Med. 1999;341:688–690. doi: 10.1056/NEJM199908263410911. [DOI] [PubMed] [Google Scholar]
- 4.Norton JA, McLean AM, Fairclogh PD. Endoscopic ultrasound in the localization of pancreatic islet cell tumors. Best Pract Res Clin Endocrinol Metab. 2004;19:177–193. doi: 10.1016/j.beem.2004.11.012. [DOI] [PubMed] [Google Scholar]
- 5.Alexander HR, Fraker DL, Norton JA, Bartlett DL, Tio L, et al. Prospective study of somatostatin receptor scintigraphy and its effect on operative outcome in patients with Zollinger-Ellison syndrome. Ann Surg. 1998;228:228–238. doi: 10.1097/00000658-199808000-00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Norton A, Jensen RT. Resolved and unresolved controversies in the surgical management of patients with Zollinger-Ellison syndrome. Ann Surg. 2004;240:757–773. doi: 10.1097/01.sla.0000143252.02142.3e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Anderson MA, Carpenter S, Thompson NW, Nostrant TT, Elta GH, Scheiman JM. Endoscopic ultrasound is highly accurate and directs management in patients with neuroendocrine tumors of the pancreas. Am J Gastroenterol. 2000;95:2271–2277. doi: 10.1111/j.1572-0241.2000.02480.x. [DOI] [PubMed] [Google Scholar]
- 8.Ellison EC. Zollinger-Ellison syndrome: a personal perspective. Am Surg. 2008;74:563–571. [PubMed] [Google Scholar]
- 9.Melvin WS, Johnson JA, Sparks J, Innes JT, Ellison EC. Long-term prognosis of Zollinger-Ellison syndrome in multiple endocrine neoplasia. Surgery. 1993;114:1183–1188. [PubMed] [Google Scholar]
- 10.Corleto VD, Annibale B, Gibril F, Angeletti S, Serrano J, et al. Does the widespread use of proton pump inhibitors mask, complicate and/or delay the diagnosis of Zollinger-Ellison syndrome? Aliment Pharmacol Ther. 2001;15:1555–1561. doi: 10.1046/j.1365-2036.2001.01085.x. [DOI] [PubMed] [Google Scholar]


