Herpes simplex virus (HSV) is recognized as a cause of gastrointestinal infection in patients with underlying immunodeficiency. The esophagus, perineum, and rectum are the most common sites of involvement, though diffuse colitis is rare. We present the case of a patient with Crohn's disease as well as hepatitis B virus (HBV) and hepatitis D virus (HDV) cirrhosis who presented with a refractory Crohn's disease flare that was found to be secondary to HSV colitis.
Case Report
A 50-year-old white man with a past medical history significant for Crohn's disease and HBV and HDV cirrhosis presented with a complaint of bloody stools. The patient was enrolled in the National Institutes of Health trial of pegylated interferon (IFN) for HDV. His Crohn's disease maintenance therapy had consisted of mesalamine with intermittent acute flares previously treated with antibiotics with resultant symptom resolution and induction of remission. IFN and mesalamine were discontinued 6 months prior to presentation due to a foot abscess, which was treated conservatively. The patient was subsequently treated for a presumed Crohn's disease flare with antibiotics 2 months prior to this presentation, and IFN was restarted at that time. The patient subsequently developed progressive weakness, weight loss, abdominal pain, and rectal bleeding. He was then admitted to an outside hospital where he was again treated for a presumed Crohn's disease flare with steroids and antibiotics prior to transfer to our facility.
On admission to our facility, the patient's vital signs were within the normal range and he was noted to be afebrile. Physical examination was negative for encephalopathy. The patient exhibited temporal wasting, and the abdominal examination was notable for distention as well as right upper quadrant tenderness to palpation. Laboratory evaluation was notable for a serum sodium level of 134 mmol/L, aspartate aminotransferase of 50 IU/L, alanine aminotransferase of 38 IU/L, alkaline phosphatase of 291 IU/L, serum albumin of 2.0 g/dL, white blood cell count of 11,000/μL with 91% neutrophils, hemoglobin of 11.0 g/dL, platelet count of 70,000/μL, and international normalized ratio of 1.5. Serum cytomegalovirus (CMV) polymerase chain reaction (PCR) testing was negative. The patient was initially placed on bowel rest and started on total parenteral nutrition. Intravenous antibiotics and steroids, as well as oral mesalamine, were continued. Stool cultures were obtained and found to be negative for routine bacterial and parasitic pathogens. An abdominal computed tomography scan demonstrated diffuse contiguous bowel-wall thickening extending from the ascending colon to the rectum. There was also a large amount of generalized ascites. No lymphadenopathy, hepatic masses, or mesenteric abnormalities were noted. The patient was referred for endoscopic evaluation. On colonoscopic examination, the colon was diffusely erythematous, friable, and ulcerated with purulent exudate visible throughout the examined colon (Figure 1). Biopsy specimens obtained from the colonic mucosa showed ulcerated mucosa with fibrinous necrosis. Herpes simplex viral inclusions, confirmed by immunofluorescent staining, were noted within the surface epithelium and ulcer bed (Figure 2–4). CMV and adenovirus immunostaining were negative. Colonic tissue viral culture was positive for HSV type 2. Steroid therapy was then discontinued, and the patient was treated with antiviral therapy for HSV with subsequent rapid cessation of abdominal pain and bloody stools. However, he developed progressive hepatic decompensation and subsequently expired. The patient was not evaluated for liver transplantation in the acute setting due to the presence of infection and the rapidly progressive decline in clinical status.
Figure 1.
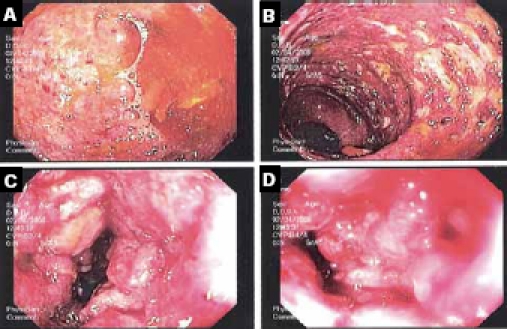
Endoscopic views of the colon.
Figure 2.
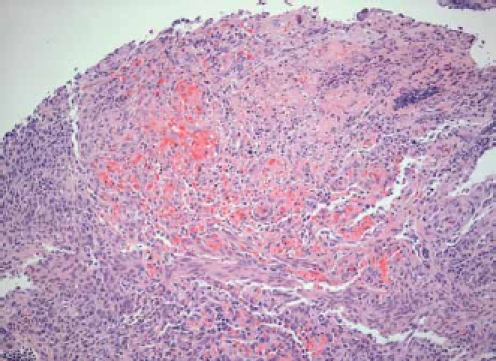
Granulating ulcer with necrotic exudate(hematoxylin and eosin stain).
Figure 4.
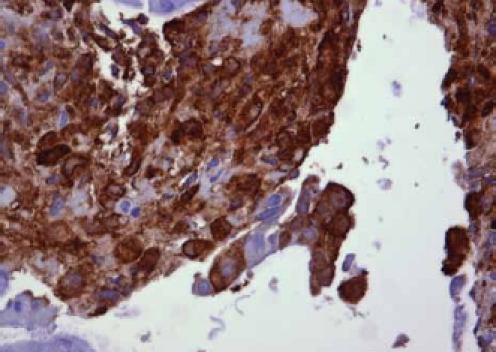
Infected cells display nuclear and cytoplasmic immunoreactivity for herpes simplex virus (SIGNET polyclonal Ab SIG-3435).
Figure 3.
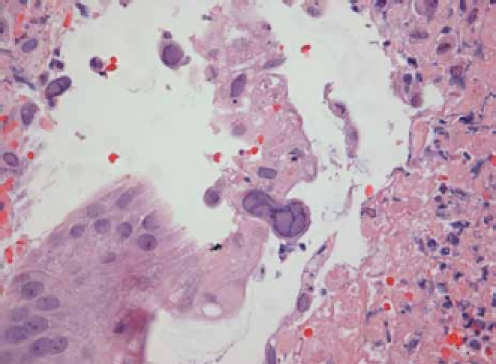
Cowdry type A intranuclear inclusions of herpes simplex virus forming the characteristic “eggs-in-a-basket” syncytia (hematoxylin and eosin stain).
Discussion
Evaluation and treatment of an acute exacerbation of Crohn's disease begins with the identification of exacerbating factors and exclusion of acute infection. Factors known to exacerbate an acute flare include cigarette smoking, nonsteroidal anti-inflammatory drug usage, and infections, including both upper respiratory and enteric infections such as Clostridium difficile.1 Diarrheal relapses in patients with ulcerative colitis have also been shown to be associated with enteric infections, and timely diagnosis may lessen avoidable exposure to corticosteroids and immunosuppressants.2 However, atypical etiologies should also be considered in those patients who fail to respond to therapy, particularly those who are immunosuppressed.
HSV proctitis has frequently been reported in immunocompromised patients presenting with anorectal pain, discharge, tenesmus, or hematochezia3; in contrast, diffuse colonic involvement with HSV is very rare and has been reported previously in 1 patient with Crohn's disease,4 but not in any patients with HBV and HDV cirrhosis. The majority of reported cases have occurred in patients who were immunosuppressed, had a defect in cellular immunity, or had a malignancy (eg, a bone marrow transplant recipient who also had intercurrent CMV, C. difficile infection, and graft-versus-host disease,5 a patient with common variable immunodeficiency syndrome presenting with HSV-1,6 a patient with HSV-1 who had undergone surgical treatment for adenocarcinoma of the transverse colon,7 and a child who had received a combined liver and small bowel transplant8). There has also been a case report of a neonate with congenital HSV infection with hematochezia and late sigmoid perforation.9
Endoscopic evaluation with biopsies was necessary in this patient to establish an etiology for his refractory flare in order to initiate appropriate treatment. With regard to pathologic evaluation for HSV, studies have been performed to determine the optimal methods for diagnosis in patients with HSV esophagitis, given its higher prevalence than HSV colitis. McBane and Gross, Jr. reported that the culture test for HSV was slightly more sensitive than microscopic examination (Cowdry type A inclusions) for the diagnosis of herpes simplex esophagitis (HSE) and that both tests should be employed in any immunosuppressed patients with esophagitis or esophageal ulcers.10 More rapid detection methods as well as microscopic investigation are necessary in practice, due to the length of time it can take for culture results to be finalized. The application of in situ hybridization or PCR assay in addition to immunohistochemical techniques with esophageal specimens may improve the diagnostic sensitivity for HSE. The immunoperoxidase method revealed diffuse positive staining in the nucleus and cytoplasm, whereas in situ hybridization revealed fibrillar positive staining in the nucleus only. Thus, the immunoperoxidase method using rabbit anti-human HSV can detect the presence of HSV protein with a greater sensitivity than that of in situ hybridization, most likely due to the greater quantity of HSV protein than HSV DNA in infected cells.11
Conclusion
HSV is a known pathogen in the gastrointestinal tract, primarily in the esophagus and rectum, in patients who are immunosuppressed. This case report is not only an example of HSV colitis, which is very rare, but of a patient with both Crohn's disease and cirrhosis. This case also demonstrates the need to consider HSV in the diagnosis of refractory colitis in order to reduce the morbidity and mortality of this disease entity. This is particularly important given the fact that patients with Crohn's disease flares are treated with steroids as first-line therapy, which can be detrimental (and fatal) to a patient with an active herpes viral infection of the colon, particularly those with cirrhosis.
References
- 1.Hanauer SB, Meyers S. Management of Crohn's disease in adults. Am J Gastro-enterol. 1997;92:559–566. [PubMed] [Google Scholar]
- 2.Banerjee D, Deb R, Dar L, Mirdha BR, Pati SK, et al. High frequency of parasitic and viral stool pathogens in patients with active ulcerative colitis: report from a tropical country. Scand J Gastroenterol. 2009;44:325–331. doi: 10.1080/00365520802556809. [DOI] [PubMed] [Google Scholar]
- 3.Goodell SE, Quinn TC, Mkrtichian E, Schuffler MD, Holmes KK, Corey L. Herpes simplex virus proctitis in homosexual men. Clinical, sigmoidoscopic, and histopathological features. N Engl J Med. 1983;308:868–871. doi: 10.1056/NEJM198304143081503. [DOI] [PubMed] [Google Scholar]
- 4.el-Serag HB, Zwas FR, Cirillo NW, Eisen RN. Fulminant herpes colitis in a patient with Crohn's disease. J Clin Gastroenterol. 1996;22:220–223. doi: 10.1097/00004836-199604000-00015. [DOI] [PubMed] [Google Scholar]
- 5.Naik HR, Chandrasekar PH. Herpes simplex virus (HSV) colitis in a bone marrow transplant recipient. Bone Marrow Transplant. 1996;17:285–286. [PubMed] [Google Scholar]
- 6.Dray X, Treton X, Mazeron MC, Lavergne-Slove A, Joly F. Herpes sim-plex virus type 1 colitis in a patient with common variable immunodeficiency syndrome. Eur J Gastroenterol Hepatol. 2006;18:541–544. doi: 10.1097/00042737-200605000-00015. [DOI] [PubMed] [Google Scholar]
- 7.Colemont LJ, Pen JH, Pelckmans PA, Degryse HR, Pattyn SR, Van Maercke YM. Herpes simplex virus type 1 colitis: an unusual cause of diarrhea. Am J Gas-troenterol. 1990;85:1182–1185. [PubMed] [Google Scholar]
- 8.Delis S, Kato T, Ruiz P, Mittal N, Babinski L, Tzakis A. Herpes simplex colitis in a child with combined liver and small bowel transplant. Pediatr Transplant. 2001;5:374–377. doi: 10.1034/j.1399-3046.2001.00014.x. [DOI] [PubMed] [Google Scholar]
- 9.Daley AJ, Craven P, Holland AJ, Jones CA, Badawi N, Isaacs D. Herpes sim-plex virus colitis in a neonate. Pediatr Infect Dis J. 2002;21:887–888. doi: 10.1097/00006454-200209000-00025. [DOI] [PubMed] [Google Scholar]
- 10.McBane RD, Gross JB Jr. Herpes esophagitis: clinical syndrome, endoscopic appearance, and diagnosis in 23 patients. Gastrointest Endosc. 1991;37:600–603. doi: 10.1016/s0016-5107(91)70862-6. [DOI] [PubMed] [Google Scholar]
- 11.Tomita T, Chiga M, Lenahan M, Balachandran N. Identification of herpes simplex virus infection by immunoperoxidase and in situ hybridization methods. Virchows Arch A Pathol Aanat Histopathol. 1991;419:99–105. doi: 10.1007/BF01600223. [DOI] [PubMed] [Google Scholar]


