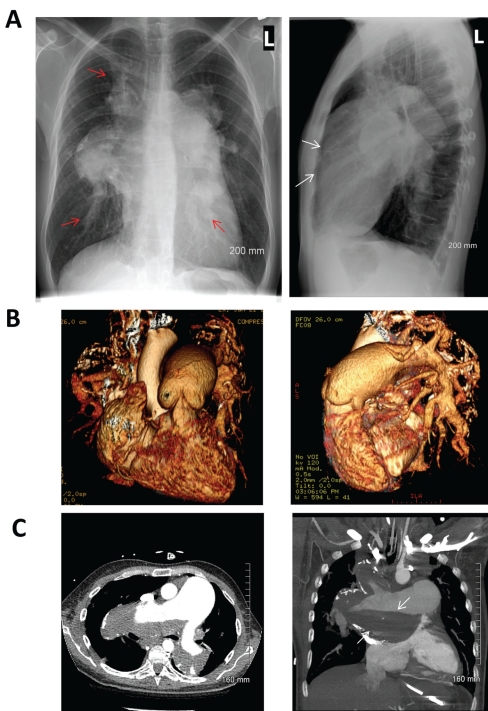
A 47-year-old man was referred for assessment of refractory hypoxia. Oxygen saturations measured by pulse oximetry remained between 70% and 80% despite 100% oxygen administration. Cardiac examination was significant for an elevated jugular venous pressure, a parasternal heave, a right-sided S4, a loud P2 and a holosystolic murmur loudest at the left lower sternal border. Respiratory examination was unremarkable. Posteroanterior and lateral radiographs of the chest (Figure 1A) demonstrated classic findings of pulmonary hypertension. Note the dilation of the central pulmonary arteries (PAs, red arrows) with rapid tapering and right ventricular enlargement (white arrows). Volume-rendered three-dimensional reconstructions (Figure 1B) demonstrated the relationship of cardiac anatomy and great vessels to the radiographic findings. A contrast-enhanced computed tomography scan of the chest (Figure 1C) demonstrated gross enlargement of the PAs relative to the aorta, and secondary development of a mural thrombus (white arrows) and PA wall calcification. The patient was temporized with inhaled nitric oxide therapy and subsequently treated with high-dose sildenafil and anticoagulated with coumadin. The patient showed dramatic improvement in oxygenation and was eventually discharged home with minimal oxygen requirements.
. 2010 May;26(5):e176. doi: 10.1016/s0828-282x(10)70387-1
Pulmonary hypertension
Benjamin Hibbert
1, Rebecca Hibbert
2, Trevor Simard
1, Carole Dennie
2, Edward R O’Brien
1,✉
Benjamin Hibbert, MD
1Division of Cardiology, University of Ottawa Heart Institute;
Find articles by Benjamin Hibbert
Rebecca Hibbert, MD
2Department of Diagnostic Imaging, University of Ottawa, Ottawa, Ontario
Find articles by Rebecca Hibbert
Trevor Simard, BSc
1Division of Cardiology, University of Ottawa Heart Institute;
Find articles by Trevor Simard
Carole Dennie, MD
2Department of Diagnostic Imaging, University of Ottawa, Ottawa, Ontario
Find articles by Carole Dennie
Edward R O’Brien, MD
1Division of Cardiology, University of Ottawa Heart Institute;
Find articles by Edward R O’Brien
1Division of Cardiology, University of Ottawa Heart Institute;
2Department of Diagnostic Imaging, University of Ottawa, Ottawa, Ontario
✉
Correspondence: Dr Edward R O’Brien, Division of Cardiology, University of Ottawa Heart Institute, 40 Ruskin Street, Ottawa, Ontario K1Y 4W7. Telephone 613-761-5030, fax 613-761-4237, e-mail eobrien@ottawaheart.ca
Received 2009 Sep 8; Accepted 2009 Oct 12.
© 2010, Pulsus Group Inc. All rights reserved
PMCID: PMC2886564 PMID: 20485698