Abstract
Purpose
To determine if reduced astigmatism-corrected acuity for vertical (V) and/or horizontal (H) gratings and/or meridional amblyopia (MA) are present prior to age three years in children who have with-the-rule astigmatism.
Methods
Subjects were 448 children, 6 months through 2 years of age with no known ocular abnormalities other than with-the-rule astigmatism, who were recruited through Women, Infants and Children clinics on the Tohono O’odham reservation. Children were classified as non-astigmats (≤ 2.00 D) or astigmats (> 2.00 D) based on right eye (RE) non-cycloplegic autorefraction measurements (Welch Allyn SureSight). RE astigmatism-corrected grating acuity for V and H stimuli was measured using the Teller Acuity Card procedure while children wore cross-cylinder lenses to correct their astigmatism or plano lenses if they had no astigmatism.
Results
Astigmatism-corrected acuity for both V and H gratings was significantly poorer in the astigmats than in the non-astigmats, and the reduction in acuity for astigmats was present for children in all three age groups examined (6 months to <1 year, 1 to <2 years, 2 to <3 years). There was no significant difference in V-H grating acuity (no evidence of MA) for the astigmatic group as a whole, or when data were analyzed for each age group.
Conclusions
Even in the youngest age group, astigmats tested with astigmatism correction showed reduced acuity for both V and H gratings, which suggests that astigmatism is having a negative influence on visual development. We found no evidence of orientation-related differences in astigmatism-corrected grating acuity, indicating either that MA does not develop prior to age 3 years, or that most of the astigmatic children had a type of astigmatism, i.e., hyperopic, that has proven to be less likely than myopic or mixed astigmatism to result in MA.
Keywords: astigmatism, amblyopia, meridional amblyopia, Native American, infants, toddlers
The presence of uncorrected astigmatism in early childhood can lead to reduced resolution (grating) acuity for stimuli of certain orientations that persists despite optical correction of the astigmatism-induced blur1-11 or emmetropization of the astigmatism.12 This pattern of deficits is referred to as meridional amblyopia (MA). A number of studies have indicated that the orientation for which subjects demonstrate reduced acuity is consistent with the stimulus orientation for which they experienced the greatest visual degradation when their astigmatism was uncorrected.3,5,7,9,12 However, astigmats do not always show the typical pattern of meridional deficits. In studies of astigmatic preschool and school-aged children, myopic and mixed with-the-rule (WTR) astigmats showed the traditional pattern of MA, with better best-corrected acuity for vertical (V) than for horizontal (H) gratings. However, hyperopic WTR astigmats showed below normal best-corrected acuity for both V and H stimuli, without MA.3,6,8
Research to date suggests that the age range for the period of susceptibility to the effects of uncorrected astigmatism on visual development begins after the first year of life.13-16 Teller et al.16 found no significant difference in V versus H best-corrected acuity in a six-month-old astigmatic infant, and Held15 and Gwiazda et al.13,14 reported that astigmatic infants did not show a preference for V or H gratings when wearing their best correction. However, these studies did not examine best-corrected acuity in comparison to a non-astigmatic control group, with the exception of one astigmatic infant for whom best-corrected acuity did not differ from non-astigmatic norms when tested between nine and twelve months of age.14
Although the lower age limit of the period of susceptibility to the effects of uncorrected astigmatism on visual development is not clear, previous research is consistent in indicating that it begins prior to age three years. Gwiazda et al.12 found meridional differences in vernier acuity in five- to eleven-year-old children who had astigmatism early in life that had emmetropized by the time the children were tested. The meridional differences in acuity were correlated most highly with the amount of astigmatism present late in the first year up to age two years, and were least correlated with the amount of astigmatism early in the first year of life, and between age two years and their age at the time of test (five to eleven years).12 These results suggest that uncorrected astigmatism begins to influence visual development by age two years. Consistent with these data are the results of several studies that have documented MA in three- to five-year-old astigmatic children.1,3,11
The purpose of the present study was to compare astigmatism-corrected acuity for V and H grating stimuli in WTR astigmatic versus low/non-astigmatic infants and toddlers. The goal was to determine if reduced acuity for V and/or H gratings and/or MA is present prior to age three years, and to determine if astigmats younger than three years of age show evidence of MA.
METHODS
Subjects
Subjects were children, six months through two years of age, who were recruited through Women, Infants and Children (WIC) clinics on the Tohono O’odham reservation from September 2005 through December 2008. Children in the study are followed longitudinally; however, the present report is based only on data from each child’s first test session.
This research followed the tenets of the Declaration of Helsinki and was approved by the Tohono O’odham Nation and by the Institutional Review Board of the University of Arizona. Parents provided written informed consent prior to testing.
Apparatus
The apparatus for grating acuity testing consisted of a Teller acuity card stage (Vistech Consultants, Inc., Dayton, OH) and two sets of 15 acuity cards, one set containing 14 V grating stimuli and a blank card, and one set containing 14 H grating stimuli and a blank card. V and H stimulus orientations were selected because nearly all astigmatic Tohono O’odham preschool children have WTR astigmatism (plus cylinder axis near 90°),3,17 and therefore V and H gratings would be parallel to the astigmatic axes in nearly all astigmatic children in this population. Each card was constructed of gray cardboard, 25.5 by 56 cm in size, and contained two 12-cm diameter circular openings located with the innermost edge 9 cm to the left and right, respectively, of a central 4 mm peephole. Behind one opening was a black-and-white square- wave grating and behind the other opening was a luminance-matched gray field, both of which were cut from a single unmounted Teller acuity card (Stereo Optical, Co., Inc, Chicago, IL). Grating spatial frequencies in each card set ranged from 0.32 to 38 cycles/cm in approximately half-octave steps. Ambient illumination was supplemented with a clip lamp attached to the stage, to provide uniform illumination of the stage and cards that was >10 cd/m2 in luminance.
A standard set of astigmatism-correcting Jackson Cross Cylinder spectacles (spherical equivalent = 0), with right eye (RE) cylinder power between 0 and 8.25 D in 0.75 D steps, and with axis at 30°, 60°, 75°, 90°, 105°, 120°, 150°, and 180°, was available at each test session. An example would be spectacles that are −1.50 + 3.00 × 90, which correct 3.00 D of astigmatism but have spherical equivalent of 0. The frames (Solo Bambini, Burlingame, CA) are specially designed for infants and young children, are made of soft plastic, and have straight temples connected by an elastic strap that can be adjusted to fit the child. We chose to measure grating acuity with eyeglasses that correct cylinder only, because previous studies of infants indicate that most infants and toddlers are hyperopes,18 and can accommodate to focus at near, and because at the test distance of 50 cm, only myopia >2.00 D, which is rare in this age group,19 would affect acuity. Data from subjects for whom SureSight measurements indicated myopia >2.00 D in the most positive/least negative RE sphere measurement were excluded from analyses. The most positive/least negative measurement was used to estimate myopia because, without cycloplegia, measurements are likely to over-estimate myopia due to accommodation.
Procedure
Prior to acuity testing, each child had refractive error assessed with the Welch Allyn SureSight autorefractor (software versions 2.16 and 2.20, Welch Allyn Medical Products, Skaneateles Falls, NY). The purpose of SureSight testing was to measure the magnitude and axis of any astigmatism the child had, in order to determine the appropriate spectacles to use to correct the astigmatism during assessment of grating acuity. SureSight testing was conducted in a dimly-lit room, away from direct sunlight. Subjects sat on the parent’s lap facing the tester, who attempted to take three measurements of the child’s RE and three measurements of the child’s left eye (LE).
Following SureSight measurements, a pair of astigmatism-correcting spectacles was selected that had a cylinder power and axis closest to the median cylinder power and axis measured by the SureSight for the RE. If no astigmatism was present, spectacles containing a plano lens were selected. If the SureSight displayed a value of 9.99 (indicating that the cylinder measurement was beyond the instrument’s measurement range of 3.00 D), spectacles were selected that corrected 3.75 D of astigmatism, with axis determined by the SureSight reading. If the SureSight would not take a reading in a cooperative child (which has been shown to indicate a cylinder value likely to be >3.00 D20), and therefore no estimate of axis was available, we excluded these children from further testing. For all other children, an over-refraction through the spectacles was then performed to verify the accuracy of the correction. For the over-refraction, the left lens in the spectacles was occluded, the sp ectacles were placed on the child, and the tester attempted to make three more SureSight measurements of the RE through the spectacles. If the median of the measurements of cylinder through the spectacles was <1.00 D, the spectacles were judged to be appropriate and the child wore these spectacles during assessment of grating acuity. If the median of the measurements showed ≥ 1.00 D of cylinder, the median value was used to select a pair of spectacles that left the child with <1.00 D of residual astigmatism, and these spectacles were worn during acuity testing. If the child would not cooperate for over-refraction, acuity testing was attempted using the spectacles chosen based on the initial SureSight measurements.
Immediately after the spectacles were selected and placed on the child’s face, RE grating acuity for V and H gratings was measured with the Teller acuity card (TAC) procedure21,22 at a distance of 50 cm. The grating orientation (V or H) tested first was determined according to a counterbalanced order. The acuity cards in each orientation set were presented in order from lower (coarser) to higher (finer) spatial frequencies, beginning with the card containing a 1.3 cy/cm (1.2 cy/deg) grating. The tester, who was masked to the location of the grating on each card, used the child’s eye and head movements to repeated presentations of each card to decide whether the child could discriminate the location of the grating on the card.21,22 Based on the child’s responses to repeated presentations of each card, the tester determined the highest spatial frequency (finest grating) that the child could resolve for each grating orientation. Threshold grating acuity scores (cy/deg) were transformed to log values for data analyses.
Parents of the subset of children whose results met any of the criteria summarized in Table 1 were offered a follow-up eye exam, with cycloplegic refraction, conducted by a pediatric ophthalmologist (JMM) who was masked to the results of the SureSight screening. The purpose of the follow-up examination was to determine if any ocular abnormality or significant refractive error requiring further follow-up or spectacle correction was present. In a given area of the reservation, exams were offered approximately six times per year, and parents were notified whenever an exam date was scheduled in their area.
Table 1.
Parents of children who met any of the following criteria were offered the opportunity to have the child examined, with cycloplegic refraction, by a pediatric ophthalmologist
| Reason for Referral for Examination |
Age | Criterion (in one or both eyes) |
|---|---|---|
| Astigmatisma | 6 to <12 months | ≥ 3.00 D |
| 12 to < 24 months | ≥ 2.50 D | |
| 24 to < 36 months | ≥ 2.00 D | |
|
| ||
| Anisometropiab | 6 to <36 months | > 1.50 D SE |
| Hyperopiac | 6 to <36 months | ≥ 4.00 D in the most hyperopic meridian |
| Myopiad | 6 to <36 months | ≥ 5.00 D in the most myopic meridian |
| High Refractive Error | 6 to <36 months | “Out of range” results on all SS measurements |
| Strabismus or Cataract | 6 to <36 months | Cover test, red reflex |
D = diopters; SE = spherical equivalent; SS = SureSight
Based on median SS cylinder measurement for each eye
Based on SE for each eye calculated using most hyperopic sphere measurement across all SS measures and median cylinder measurement across all SS measurements for each eye.
Based on most hyperopic sphere measurement and median cylinder measurement across all SS measures for each eye.
Based on most myopic sphere measurement for each eye.
Data Analysis
Data were excluded from children with known ocular abnormalities or developmental disabilities, and from children who did not provide both SureSight measurements and grating acuity data for the RE. In addition, data were excluded from children who completed grating acuity testing but in whom the most positive/least negative SureSight RE sphere measurement indicated more than 2.00 D of myopia, or who had RE astigmatism (> 0.00 D) that was not WTR (plus cylinder axis 90° ± 15°), based on the SureSight median axis.
For each eye, the estimate of cylinder magnitude and axis was obtained by converting measurements to vector notation,23 calculating the median J0 and J45, and then converting the medians back into clinical notation. In cases where the SureSight did not provide cylinder magnitude (due to out of range cylinder measurement indicated by a value of 9.99) but did provide axis measurements, axis used was the simple median of all measurements of axis obtained. Data were excluded in cases where the SureSight did not provide axis measurement (instrument turned off without making a measurement in a cooperative child, indicating a high likelihood of astigmatism >3.00 D20).
A previous comparison of SureSight cylinder values with cylinder values obtained with the Retinomax K-Plus autorefractor indicated that SureSight cylinder values ≤ 3.00 D correspond to true cylinder values of ≤ 2.00 D in 97% of cases, and SureSight cylinder values of 9.99 or failure to provide a cylinder correspond to true cylinder values of >2.00 D in 88% of cases.20 Therefore, in the present study, we used the median SureSight cylinder value for the RE to classify children in the present study as low/non-astigmatic (≤ 2.00 D of astigmatism) or highly astigmatic (>2.00 D of astigmatism). Children with SureSight values ≤ 3.00 D were classified as having low/no astigmatism, and those in whom the SureSight gave a value of 9.99 were classified as high astigmats. Those in whom the SureSight turned off without providing a reading were excluded from the data analysis, since axis of astigmatism was not known.
RESULTS
Subjects
The final sample included 448 children: 238 at 6 months to <1 year, 121 at 1 to <2 years, and 89 at 2 to <3 years of age. Although 786 children were initially recruited, data from 338 were excluded for the reasons summarized in Table 2. This included 8 children in whom the initial SureSight readings indicated out-of-range astigmatism by turning itself off after measurement in a cooperative child.
Table 2.
Summary of reasons for exclusion of 338 (43%) of the 786 children 6 months to <3 years of age who were enrolled in the study
| Reason for exclusion | Age (years) |
TOTAL | ||
|---|---|---|---|---|
| 0.5 to <1 | 1 to <2 | 2 to <3 | ||
| Ocular abnormalities or developmental disabilities | 7 | 3 | 3 | 13 |
| Unable to obtain grating acuity data | 60 | 94 | 38 | 192 |
| Unable to obtain grating acuity data and axis not WTR or unable to determine axis of astigmatism |
13 | 9 | 3 | 25 |
| Unable to obtain grating acuity data and Suspected myopia > 2.00 Da | 1 | 0 | 1 | 2 |
| Unable to obtain SureSight measurement | 1 | 0 | 0 | 1 |
| Unable to obtain SureSight measurement and grating acuity data |
0 | 5 | 4 | 9 |
| Suspected myopia > 2.00 Da | 4 | 2 | 0 | 6 |
| Astigmatism > 0.00 D present, but axis not WTR | 33 | 29 | 19 | 81 |
| Unable to determine axis of astigmatism | 4 | 0 | 5 | 9 |
D = diopters; WTR = with-the-rule
Suspected myopia: the most hyperopic/least myopic SureSight sphere reading indicated myopia >2.00 D
Based on the median SureSight reading for the RE (calculated using vector methods23), 112 children (25.0%) had >2.00 D of astigmatism; this included 29.8% (71/238) of the 6 month to <1 year age group, 14.9% (18/121) of the 1 to <2 year age group, and 25.8% (23/89) of the 2 to <3 year age group.
In 417 of the 448 children (93.1%) (93.3% [222/238] of the 6 month to <1 year age group, 91.7% [111/121] of the 1 to <2 year age group, and 94.4% [84/89] of the 2 to <3 year age group), the spectacles worn during acuity testing corrected astigmatism to within 1.00 D, based on the SureSight over-refraction. The remaining 31 children did not cooperate for over-refraction with the SureSight, and a X2 test indicated that the percentage of uncooperative children did not differ across the three age groups.
There were 192 children (24.4%) who were excluded solely for inability to cooperate for grating acuity testing. A X2 test showed no difference in the prevalence of high astigmatism in this group of children (39/192 (20.3%)) versus the prevalence of high astigmatism in the group of children who completed acuity testing and were included in the final analysis (112/448 (25.0%).
Cycloplegic retinoscopy data were available for 152 (33.9%) of the 448 children: 88 at 6 months to <1 year, 39 at 1 to <2 years, and 25 at 2 to <3 years. On average, the data were obtained 6.7 months (SD 6.8) after acuity testing. Among the 152 children who had a cycloplegic refraction, 28 (18.4%) had astigmatism >2.00 D in the RE based on cycloplegic retinoscopy. Analysis of agreement between SureSight classification and classification based on cycloplegic retinoscopy indicated that 58% (72/124) of children classified as low astigmats based on cycloplegic retinoscopy were also classified as low astigmats based on SureSight readings and 68% (19/28) of children classified as high astigmats based on cycloplegic retinoscopy were also classified as high astigmats based on SureSight readings. In 7 of the 28 children classified as high astigmats based on cycloplegic retinoscopy, the astigmatism was simple or compound myopic or mixed, and in 21 it was simple or compound hyperopic.
Grating Acuity
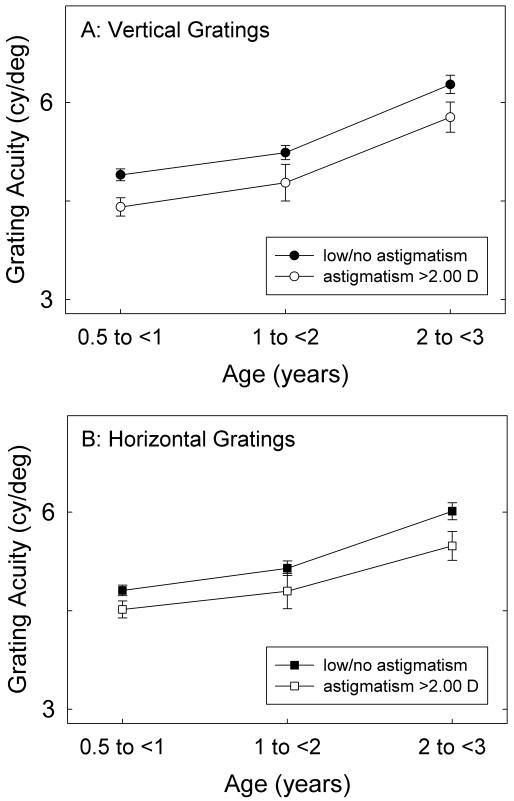
Figure 1 shows mean acuity for (A) V and (B) H gratings for the astigmatic and the low/non-astigmatic groups. Analysis of variance (ANOVA) indicated significant effects of age (F(2,448)=32.09, p<0.001 for V stimuli; F(2,448)=26.66, p<0.001 for H stimuli) and astigmatism group (F(1,448)=11.67, p<0.002 for V stimuli; F(2,448)=5.27, p<0.03 for H stimuli), and no interaction between age and astigmatism group. Post hoc comparisons (with Bonferroni correction) indicated that all pairwise comparisons of age for both V and H stimuli were significant (all ps < 0.004).
Figure 1.
Mean right eye acuity for (A) vertical and (B) horizontal gratings obtained with the child wearing astigmatism-correcting spectacles, or plano spectacles if no astigmatism was present. The low/no astigmatism group includes 186 children at 6 months to <1 year of age, 116 at 1 to < 2 years, and 75 at 2 to <3 years who had no astigmatism or with-the-rule (WTR) astigmatism ≤ 2.00 diopters (D). The astigmatism >2.00 D group includes 76 children at 6 months to <1 year of age, 18 at 1 to < 2 years, and 27 at 2 to <3 years, all of whom had WTR astigmatism. Bars indicate ± 1 standard error of the mean.
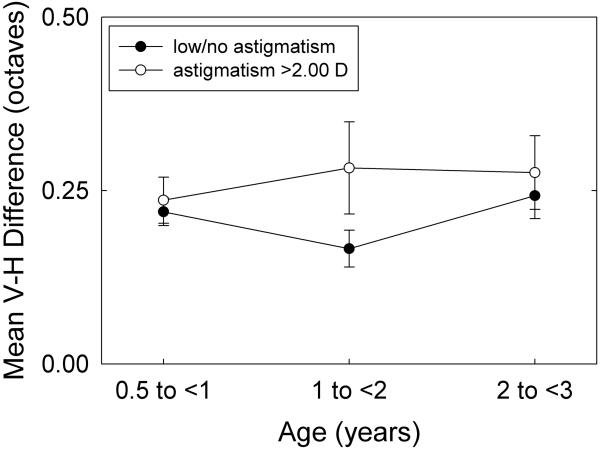
Figure 2 plots the difference in acuity for V versus H gratings, to determine whether MA is present in the astigmatic group. The values plotted are based on the absolute value of the difference between V and H acuities for each child, because in the absence of cycloplegic refraction data for sphere, it was not possible to know whether a child was a myopic, mixed, or hyperopic astigmat, and therefore to predict whether V or H gratings would be expected to yield better acuity if MA were present (i.e., in myopic/mixed, we would predict acuity for V would be better, and in hyperopic we would predict acuity for H would be better). ANOVA indicated no significant effect of age or of astigmatism group (astigmatic vs low/non-astigmatic), indicating no evidence of MA for the astigmatic group. Mean difference between acuity for V and H gratings was 0.26 octave (95% CI 0.20 to 0.32) for the astigmatic group and 0.21 octave (95% CI 0.18 to 0.24) for the low/non-astigmatic group.
Figure 2.
Mean of the absolute value of difference in octaves in astigmatism-corrected acuity for vertical and horizontal gratings shown for children in the low/no astigmatism group and children with astigmatism >2.00 D. The low/no astigmatism group includes 186 children at 6 months to <1 year of age, 116 at 1 to < 2 years, and 75 at 2 to <3 years who had no astigmatism or with-the-rule (WTR) astigmatism ≤ 2.00 diopters (D). The astigmatism >2.00 D group includes 76 children at 6 months to <1 year of age, 18 at 1 to < 2 years, and 27 at to <3 years, all of whom had WTR astigmatism. Bars indicate ± 1 standard error of the mean.
Grating acuity in the subset of 152 children who underwent cycloplegic retinoscopy
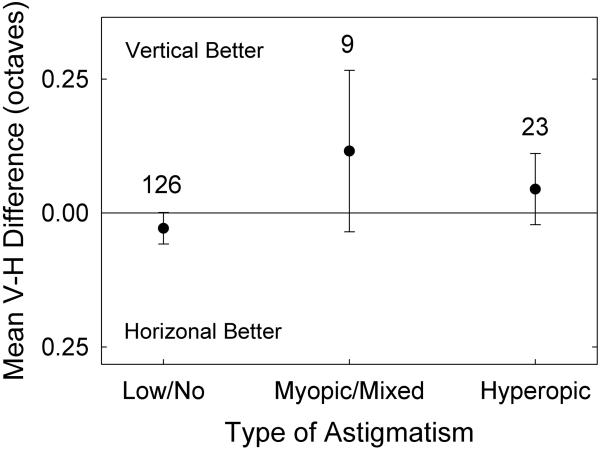
ANOVA indicated no difference in acuity for either V or H gratings across three groups of children: 124 with low/no astigmatism (≤ 2.00 D); 7 with myopic or mixed astigmatism >2.00 D, and 21 with hyperopic astigmatism >2.00 D. Mean acuity for V gratings was 4.36 cy/deg (SD 0.44 octave) for the low/no astigmatism group, 4.90 cy/deg (SD 0.59 octave) for the myopic/mixed astigmatism group, and 4.55 cy/deg (SD 0.34 octave) for the hyperopic astigmatism group. Mean acuity for H gratings was 4.45 cy/deg (SD 0.37 octave) for the low/no astigmatism group, 4.90 cy/deg (SD 0.39 octave) for the myopic/mixed astigmatism group, and 4.32 cy/deg (SD 0.35 octave) for the hyperopic astigmatism group. Figure 3 plots the difference in acuity for V versus H gratings for the three groups of children. An ANOVA indicated no significant difference among groups. Mean difference in acuity (V-H results) was close to 0 in all three groups.
Figure 3.
Mean difference between acuity for vertical and horizontal gratings for 152 children 6 months to <3 years of age who underwent cycloplegic retinoscopy. Children with astigmatism >2.00 diopters (D) based on the cycloplegic retinoscopy were categorized as having simple or compound, mixed, or simple or compound hyperopic astigmatism.
DISCUSSION
The results of the present study of 448 children 6 months to <3 years of age, 121 (24.3%) of whom had astigmatism >2.00 D, indicated that astigmatism-corrected acuity for both V and H gratings in children with high astigmatism was worse than that of children with astigmatism ≤ 2.00 D, and that the reduction in acuity was present for children in all three age groups examined (6 months to <1 year, 1 to <2 years, and 2 to <3 years). These data suggest that amblyopia is present. However, no evidence of MA was found for the high astigmatism group as a whole, or when data were analyzed for each age group.
The reduction in grating acuity for both V and H gratings in astigmatism-corrected infants and toddlers in comparison to low/non-astigmatic children of the same age is a new finding, as previous studies of children in this age range have not included a non-astigmatic comparison group. However, if most of the infants and toddlers in the astigmatic group had hyperopic astigmatism, which is suggested by cycloplegic refraction of a subset of the children, then the finding of reduced acuity for both V and H gratings is consistent with data from hyperopic astigmatic children three years of age and older in this population.3,8 Preliminary data from these older children suggest that, when uncorrected, young hyperopic astigmats may accommodate between the two astigmatic focal planes,24 rendering both orientations out of focus during development.
Our failure to find evidence of MA in infants and toddlers is in agreement with the results of previous studies of astigmats in this age group.13-16 One explanation for the failure to find MA in infants and toddlers is that MA does not develop at these young ages. Another explanation, however, is that most astigmatic children in our sample were probably hyperopic astigmats, a condition that is not likely to result in MA in children in this population.3,8 It is also possible that, while MA is not found in children younger than three years of age, astigmatism during this age range may lead to later development of MA. This would be consistent with the finding of Gwiazda et al.12 who tested non-astigmatic five- to eleven-year-old children whose refractive error development had been followed longitudinally and found meridional differences in vernier acuity in that were correlated most highly with the amount of astigmatism present late in the first year up to age two years. The meridional differences were least correlated with the amount of astigmatism early in the first year of life, and between age two years and their age at the time of test (five to eleven years).12
The design of the present study did not include cycloplegic refraction of all subjects, so we do not know what proportion of the overall sample of astigmats was hyperopic. However, a subset of the study population did receive a complete eye examination, including cycloplegic retinoscopy. This was not a random sample; instead, parents were offered an eye examination for their child on a different date if there was evidence of ocular abnormalities on cover testing, or evidence of high refractive error based on SureSight measurements. Among the 152 children whose parents took them for the eye examination, 28 (18.4%) had astigmatism >2.00 D based on the cycloplegic retinoscopy, and 75.0% of these had simple or compound hyperopic astigmatism. Grating acuity results showed no evidence of MA in the group of 21 hyperopic astigmats nor in the 7 myopic/mixed astigmats (Figure 3). Because the cycloplegic retinoscopy was a clinical exam for safety purposes and referral for further care if indicated, rather than gold-standard measurement of refractive error, it is possible that there were additional children with astigmatism ≥ 2.00 D who were not identified and who could have provided additional information concerning grating acuity in hyperopic, myopic, and mixed astigmats. Data from a larger number of myopic and/or mixed astigmats and more precise cycloplegic measures of refractive error would help to determine whether MA does occur in children younger than three years of age. However, data from the relatively small number of hyperopic astigmats identified do support the hypothesis that the reason data in the present study show reduced acuity for both V and H gratings, without evidence for MA, is likely due to a high proportion of the astigmatic infants and toddlers being hyperopic, rather than myopic or mixed, astigmats.
One noticeable finding of the grating acuity results for both astigmatic and non-astigmatic subjects is that they are at the low end of the normal range for monocular acuity results for children of the same age.25,26 It is likely that this result is due to several sources of distraction to the child (wearing spectacles during testing, having siblings nearby during testing, and other activity going on at the WIC clinic). It could also reflect under-correction or over-correction of astigmatism in children who did not cooperate for over-refraction with the SureSight when the spectacles were worn. However, the percentage of subjects who failed to cooperate for the over-refraction was small, only 6.9%.
The present study has both strengths and limitations. Strengths include a large number of subjects, assessment of subjects who were younger than three years of age, and the fact that all subjects, including non-astigmats, wore spectacles during testing. Limitations include the possibility that the astigmatism-correcting lenses under- or over-corrected the astigmatism in the small percentage (6.9%) of children in whom over-refraction when the spectacles were worn was not possible, the absence of cycloplegic refraction data with which to classify all children as hyperopic, myopic, or mixed astigmats, and the fact that one-fourth of the children failed to cooperate for grating acuity testing: 20% (74/361) at 6 months to <1 year, 41% (108/263) at 1 to <2 years, and 28% (46/162) at 2 to <3 years. If the relatively high proportion of children who failed to cooperate for acuity testing had included a substantial number of high astigmats, it would suggest that the acuity results obtained from the cooperative group might have under-estimated the true reduction in acuity that would have been found if all high astigmats could have been tested. However, comparison of in the uncooperative and the cooperative groups indicated no difference in the proportion with high astigmatism (20.3% vs 25.0%), suggesting that the grating acuity results obtained were probably representative of results from the entire group of children.
In conclusion, the results of the present study failed to find evidence of orientation-related differences in astigmatism-corrected grating acuity in astigmatic infants and toddlers less than three years of age who were tested with spectacle correction of astigmatism. However, even in the youngest age group tested (age 6 months to <1 year), astigmats tested with spectacle correction showed reduced acuity for both V and H gratings, suggesting that astigmatism is having a negative influence on visual development.
ACKNOWLEDGMENTS
This study was supported by National Institutes of Health/National Eye Institute (NIH/NEI) grants EY13153 (EMH) and by Research to Prevent Blindness (a Career Development Award (EMH), a Walt and Lilly Disney Award for Amblyopia Research (JMM), and unrestricted funds to the Department of Ophthalmology and Vision Science (JMM)). Velma Dobson, PhD, has received royalties from the sale of the Teller acuity cards II.
We thank the Tohono O’odham Nation, Donna Juan and the staff of the WIC program, the parents and children who participated in the study, and our NIH/NEI Data Monitoring and Oversight Committee [Robert Hardy, PhD (chair), Morgan Ashley, Donald Everett, MA, Jonathan Holmes, MD, Andrew Lorentine, and Karla Zadnik, OD, PhD].
Footnotes
Preliminary results of the study were presented at The Third Annual Berkeley Conference on Translational Research, Berkeley, CA, June 6–7, 2009.
This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Atkinson J, Braddick O, Robier B, Anker S, Ehrlich D, King J, Watson P, Moore A. Two infant vision screening programmes: prediction and prevention of strabismus and amblyopia from photo- and videorefractive screening. Eye. 1996;10(Pt 2):189–98. doi: 10.1038/eye.1996.46. [DOI] [PubMed] [Google Scholar]
- 2.Cobb SR, MacDonald CF. Resolution acuity in astigmats: evidence for a critical period in the human visual system. Br J Physiol Opt. 1978;32:38–49. [PubMed] [Google Scholar]
- 3.Dobson V, Miller JM, Harvey EM, Mohan KM. Amblyopia in astigmatic preschool children. Vision Res. 2003;43:1081–90. doi: 10.1016/s0042-6989(03)00014-2. [DOI] [PubMed] [Google Scholar]
- 4.Freeman RD. Contrast sensitivity in meridional amblyopia. Invest Ophthalmol. 1975;14:78–81. [PubMed] [Google Scholar]
- 5.Freeman RD, Mitchell DE, Millodot M. A neural effect of partial visual deprivation in humans. Science. 1972;175:1384–6. doi: 10.1126/science.175.4028.1384. [DOI] [PubMed] [Google Scholar]
- 6.Freedman RD, Thibos LN. Contrast sensitivity in humans with abnormal visual experience. J Physiol. 1975;247:687–710. doi: 10.1113/jphysiol.1975.sp010952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Harvey EM, Dobson V, Miller JM, Clifford-Donaldson CE. Amblyopia in astigmatic children: patterns of deficits. Vision Res. 2007;47:315–26. doi: 10.1016/j.visres.2006.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Harvey EM, Dobson V, Miller JM, Clifford-Donaldson CE. Changes in visual function following optical treatment of astigmatism-related amblyopia. Vision Res. 2008;48:773–87. doi: 10.1016/j.visres.2007.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mitchell DE, Freeman RD, Millodot M, Haegerstrom G. Meridional amblyopia: evidence for modification of the human visual system by early visual experience. Vision Res. 1973;13:535–58. doi: 10.1016/0042-6989(73)90023-0. [DOI] [PubMed] [Google Scholar]
- 10.Mithcell DE, Wilkinson F. The effect of early astigmatism on the visual resolution of gratings. J Physiol. 1974;243:739–56. doi: 10.1113/jphysiol.1974.sp010774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mohindra I, Jacobson SG, Held R. Binocular visual form deprivation in human infants. Doc Ophthalmol. 1983;55:237–49. doi: 10.1007/BF00140811. [DOI] [PubMed] [Google Scholar]
- 12.Gwiazda J, Bauer J, Thorn F, Held R. Meridional amblyopia does result from astigmatism in early childhood. Clin Vision Sci. 1986;1:145–52. [Google Scholar]
- 13.Gwiazda J, Mohindra I, Brill S, Held R. Infant astigmatism and meridional amblyopia. Vision Res. 1985;25:1269–76. doi: 10.1016/0042-6989(85)90042-2. [DOI] [PubMed] [Google Scholar]
- 14.Gwiazda J, Mohindra I, Brill S, Held R. The development of visual acuity in infant astigmats. Invest Ophthalmol Vis Sci. 1985;26:1717–23. [PubMed] [Google Scholar]
- 15.Held R. In: Cool SJ, Smith EL, editors. Development of visual acuity in normal and astigmatic infants; Frontiers in Visual Science: Proceedings of the University of Houston College of Optometry Dedication Symposium, Houston, Texas, U.S.A., March, 1977; New York: Springer-Verlag. 1978.pp. 712–79. [Google Scholar]
- 16.Teller DY, Allen JL, Regal DM, Mayer DL. Astigmatism and acuity in two primate infants. Invest Ophthalmol Vis Sci. 1978;17:344–9. [PubMed] [Google Scholar]
- 17.Dobson V, Miller JM, Harvey EM. Corneal and refractive astigmatism in a sample of 3- to 5-year-old children with a high prevalence of astigmatism. Optom Vis Sci. 1999;76:855–60. doi: 10.1097/00006324-199912000-00022. [DOI] [PubMed] [Google Scholar]
- 18.Sorsby A, Leary G. A longitudinal study of refraction and its components during growth. Medical Research Council. Her Majesty’s Stationery Office; London: 1969. p. 1. Special Report Series No. 309. [PubMed] [Google Scholar]
- 19.Baldwin WR. Refractive status of infants and children. In: Rosenbloom AA, Morgan MW, editors. Principles and Practice of Pediatric Optometry. Lippincott; Philadelphia: 1990. pp. 104–52. [Google Scholar]
- 20.Harvey EM, Dobson V, Miller JM, Clifford-Donaldson CE, Green TK, Messer DH, Garvey KA. Accuracy of the Welch Allyn SureSight for measurement of magnitude of astigmatism in 3- to 7-year-old children. J AAPOS. 2009;13:466–71. doi: 10.1016/j.jaapos.2009.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McDonald MA, Dobson V, Sebris SL, Baitch L, Varner D, Teller DY. The acuity card procedure: a rapid test of infant acuity. Invest Ophthalmol Vis Sci. 1985;26:1158–62. [PubMed] [Google Scholar]
- 22.Teller DY, McDonald MA, Preston K, Sebris SL, Dobson V. Assessment of visual acuity in infants and children: the acuity card procedure. Dev Med Child Neurol. 1986;28:779–89. doi: 10.1111/j.1469-8749.1986.tb03932.x. [DOI] [PubMed] [Google Scholar]
- 23.Harvey EM, Miller JM, Dobson V, Tyszko R, Davis AL. Measurement of refractive error in Native American preschoolers: validity and reproducibility of autorefraction. Optom Vis Sci. 2000;77:140–9. doi: 10.1097/00006324-200003000-00013. [DOI] [PubMed] [Google Scholar]
- 24.Harvey EM, Dobson V, Miller JM, Clifford CE. Accommodation in uncorrected astigmatic children. Invest Ophthalmol Vis Sci. 2003;44 E-Abstract 2727. [Google Scholar]
- 25.Mayer DL, Beiser AS, Warner AF, Pratt EM, Raye KN, Lang JM. Monocular acuity norms for the Teller Acuity Cards between ages one month and four years. Invest Ophthalmol Vis Sci. 1995;36:671–85. [PubMed] [Google Scholar]
- 26.Salomao SR, Ventura DF. Large sample population age norms for visual acuities obtained with Vistech-Teller Acuity Cards. Invest Ophthalmol Vis Sci. 1995;36:657–70. [PubMed] [Google Scholar]