Abstract
OBJECTIVES
This study used high-resolution impedance manometry (HRIM) to determine pressure topography thresholds of peristaltic integrity predictive of incomplete esophageal bolus clearance.
METHODS
A total of 16 normal controls and 8 patients with dysphagia were studied using a solid-state HRIM assembly incorporating 36 manometric sensors and 12 impedance segments. Each of the 10 saline swallows in each study was dichotomously scored as either complete or incomplete bolus clearance by impedance criteria, and peristaltic integrity was evaluated using pressure topography isobaric contours ranging from 10 to 30 mm Hg in 5-mm Hg increments. Each isobaric contour plot was characterized by the location and length of breaks in the isobaric contour.
RESULTS
All subjects had normal esophagogastric junction (EGJ) relaxation and none met the pressure topography criteria of hiatus hernia. In all, 70 (29%) of the 240 individual swallows had incomplete bolus clearance. In every case, an intact ≥20 mm Hg isobaric contour was associated with complete bolus clearance. The largest defect in the 20 and 30 mm Hg isobaric contours associated with complete bolus clearance measured 1.7 and 3.0 cm, respectively, in length, whereas the smallest defect predictive of incomplete bolus clearance measured 2.1 and 3.2 cm, respectively.
CONCLUSIONS
In individuals with normal EGJ relaxation and morphology, peristaltic contractions with breaks <2 cm in the 20 mm Hg isobaric contour or <3 cm in the 30 mm Hg isobaric contour are associated with complete bolus clearance, and longer breaks predict incomplete bolus clearance.
INTRODUCTION
A major objective of clinical esophageal manometry studies is to ascertain whether esophageal peristaltic function is sufficient enough to facilitate bolus transport to the stomach. Kahrilas et al. (1) used conventional manometry and concurrent videofluoroscopy to determine that a mean peristaltic amplitude of ≥30 mm Hg was conducive to liquid bolus transit and esophageal emptying. Five years later, Ren et al. (2) used similar techniques to show that a peristaltic amplitude of 20 mm Hg greater than the intrabolus pressure (~10 mm Hg) was associated with effective bolus transit. On the basis of these studies, a peristaltic amplitude of 30 mm Hg has come to be accepted as the lower limit of normal in current manometry classification schemes (3,4).
Although peristaltic amplitudes <30 mm Hg have been shown to be adequate for bolus transit, amplitudes <30 mm Hg are not necessarily inadequate. In 2003, Tutuian and Castell (5) used a combined multichannel intraluminal impedance and esophageal manometry system to reassess the 30 mm Hg amplitude threshold. They found that a peristaltic amplitude ≥30 mm Hg predicted complete bolus transit in 95% of instances, whereas amplitudes <30 mm Hg were associated with incomplete bolus transit 52% of the time. In other words, 48% of swallows still achieved complete bolus transit despite having peristaltic amplitudes less than the 30 mm Hg threshold. Using similar methodology, but defining normal contraction pressures as ≥12 mm Hg in the proximal esophagus and ≥30 mm Hg in the distal esophagus, Conchillo et al. (6) similarly noted that 35% of patients with “normal motility” had abnormal transit. Taken together, these studies highlighted that manometry alone has limitations in predicting bolus transit. However, the manometric technique and interpretation paradigms used in these two studies were relatively basic by current standards, lacking the resolution to define small peristaltic defects and ignoring subtle physiological abnormalities of the esophagogastric junction (EGJ) that could potentially be associated with incomplete bolus clearance (7,8).
Using concurrent high-resolution manometry (HRM) and videofluoroscopy, Fox et al. (9) recently showed that HRM that is displayed in pressure topography plots predicts bolus transit more accurately than does conventional manometry. Fox et al. noted that the increased spatial resolution of HRM frequently showed segmental hypotensive foci that would have been missed with conventional manometry. However, the threshold dimensions of defects in pressure topography plots likely associated with incomplete bolus transit remain to be defined. Thus, the aim of this study was to determine the pressure topography characteristics of peristalsis predictive of complete and incomplete bolus clearance. The simultaneous evaluation of esophageal pressure topography and associated bolus clearance was made possible by the recent development of a catheter combining HRM with high-resolution multichannel intraluminal impedance.
METHODS
Patients
High-resolution impedance manometry (HRIM) studies were conducted on both control subjects and patients. The control group consisted of volunteers without gastrointestinal symptoms, history of upper gastrointestinal tract surgery, or any significant medical condition. The patients were recruited from the clinical practices of J.E.P. and P.J.K. at the Northwestern Medical Faculty Foundation. The study protocol was approved by the Northwestern University Institutional Review Board, and informed consent was obtained from each subject before the study.
High-resolution impedance manometry
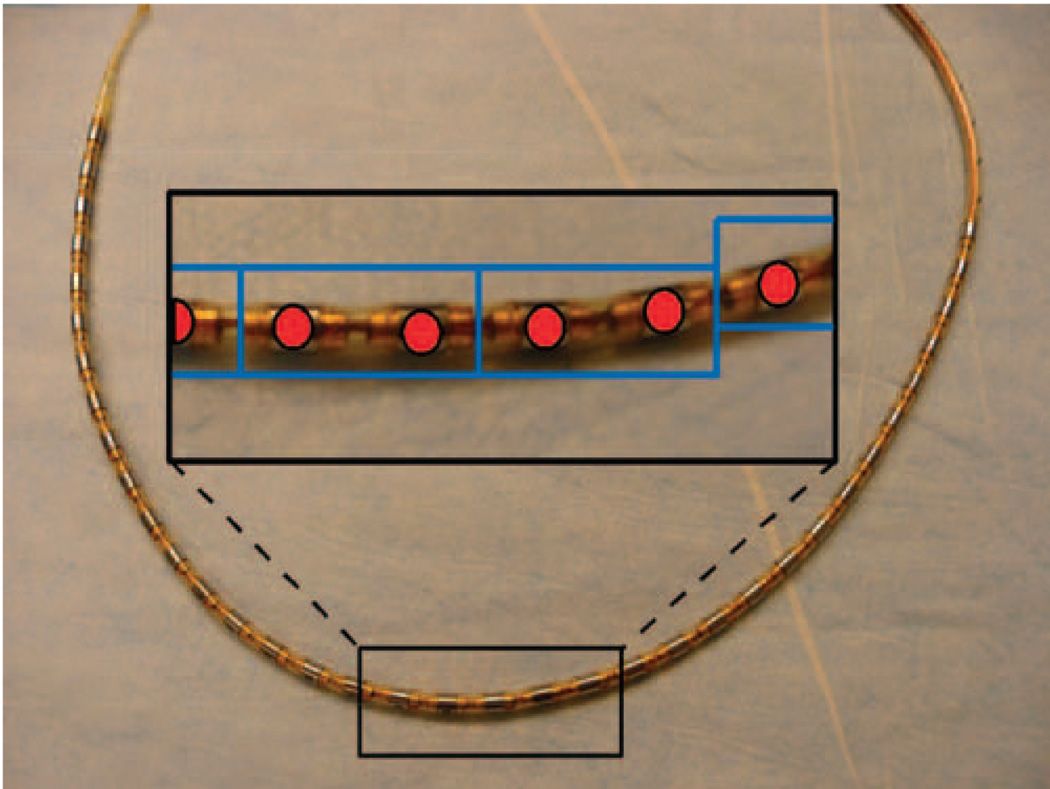
A solid-state combined manometry and impedance recording assembly incorporating 36 unidirectional strain gauge pressure sensors spaced at 1-cm intervals and 14 impedance-recording rings (12 impedance segments) spaced at 2-cm intervals spanning the distal 26 cm of the assembly (Figure 1) was used (Medical Measurement Systems, Enschede, The Netherlands). The response characteristics of the pressure sensors were such that they could record pressures ranging from −100 to 300 mm Hg at a sampling rate of 50 Hz with accuracy to within 2 mm Hg. After calibration in a water bath and correction for body temperature, the drift over the course of the study was <3 mm Hg. The impedance-sensing elements could record impedance transients up to 10,000 ohms at a sampling rate of 50 Hz with accuracy to within 30 ohms.
Figure 1.
High-resolution impedance manometry (HRIM) recording assembly. The device integrated 36 strain gauge pressure sensors (red dots) spaced 1 cm apart with 14 impedance-recording rings (12 impedance-recording segments) spaced at 2-cm intervals (except one 4-cm gap in the proximal segment) traversing the distal 26 cm of the assembly.
Subjects fasted for at least 6 h before a brief interview, examination, and transnasal placement of the HRIM assembly. Studies were conducted with the subjects in a supine position, and the HRIM assembly was positioned to record from the hypopharynx to the proximal stomach with approximately five intragastric pressure sensors. The impedance sensors were thus positioned to record from the termination of the proximal esophageal segment through the distal esophagus and into the proximal stomach with approximately two intragastric impedance measurements. The assembly was fixed in place by taping it the nose. The manometric protocol included 30 s without swallows to assess basal EGJ pressure and morphology followed by 10 5-ml swallows of 0.3% saline solution. Saline solution was chosen because its conductivity allowed it to be easily distinguished from esophageal mucosa during impedance monitoring.
Data analysis
Data were analyzed using MMS Database software (Medical Measurement Systems, version 8.11a). Color isobaric contour plots were overlaid with impedance line tracings, providing concurrent visualization of pressure and impedance data at each of the 12 impedance-recording sites. The integrity of esophageal peristalsis was assessed using the isobaric contour tool provided by the MMS Database, which allowed delineation of the anatomical and temporal boundaries of user-designated pressure thresholds. Breaks in the isobaric contours were measured using the smart mouse function of the MMS Database and characterized by the vertical length of the break (Figure 2). EGJ pressure was referenced to gastric pressure; all other esophageal pressures were referenced to atmospheric pressure.
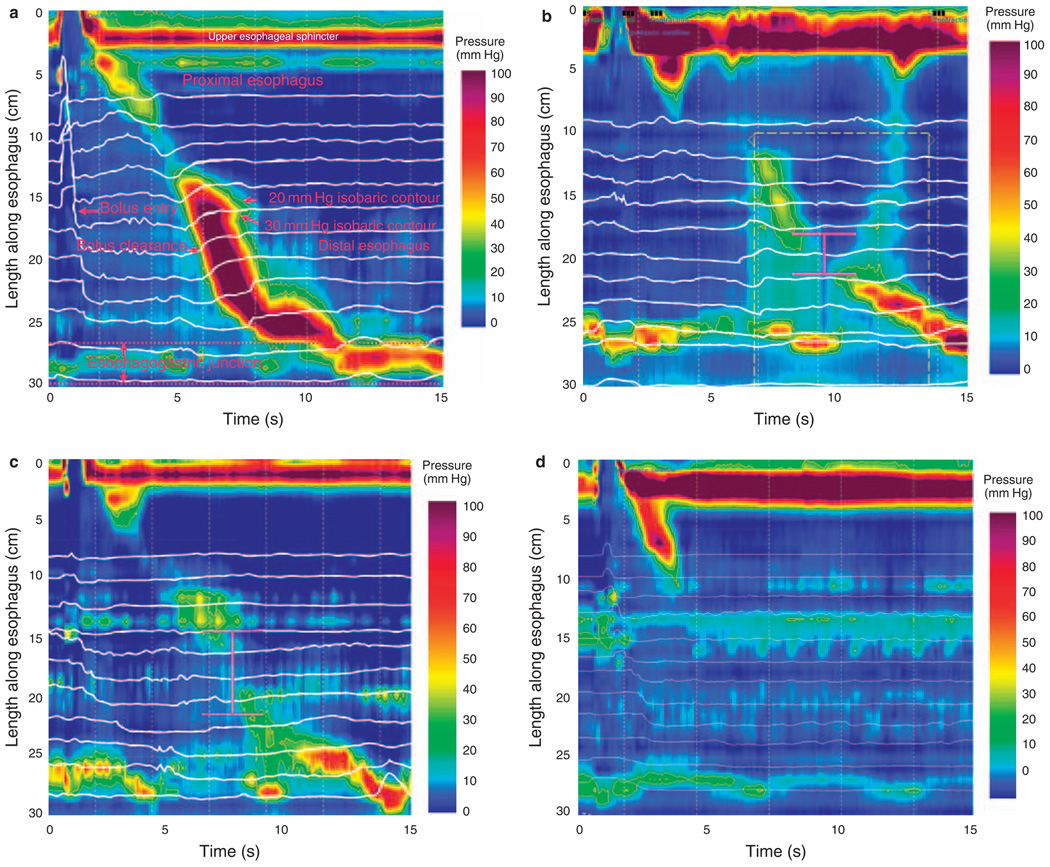
Figure 2.
Methodology for identifying and measuring isobaric contour breaks as a means of classifying peristaltic hypotension. In this example, the isobaric contour of 20 mm Hg is analyzed. The smart mouse tool of DataBase software is used to delineate the margins of the break, and it is then scored according to the vertical separation between the proximal and distal margins. In this particular example, the two areas of separation are illustrated using the bracket line (pink). The first defect is 4 cm in vertical separation, whereas the more distal second defect is ~2 cm in length.
Esophageal pressure topography analysis
Pressure topography studies were first evaluated for deglutitive EGJ relaxation. This was done by determining the nadir pressure across the 6-cm array of pressure sensors traversing the EGJ during the post-deglutitive period and using 10 mm Hg as the upper limit of normal. Each patient was also evaluated for hiatus hernia using previously established pressure topography criteria (10). For inclusion in the study, subjects were required to have normal EGJ anatomy (no hernia) and normal EGJ relaxation, as abnormalities of either can cause impaired bolus clearance even in the context of normal peristalsis (7,8).
Peristaltic integrity was then evaluated for each swallow on isobaric contour plots ranging from 10 to 30 mm Hg in 5-mm Hg increments. Each plot was characterized dichotomously as intact (no break in the isobaric contour) or disrupted (breaks of any length in the isobaric contour). On the basis of the presence and length of breaks observed, swallows were then further characterized using a modification of our previously published scheme: (i) normal (no break ≥2.0 cm, Figure 3a); (ii) focal peristaltic hypotension (longest break ≥2.0 and < 5.0 cm, Figure 3b); (iii) diffuse peristaltic hypotension (longest break ≥5.0 cm, Figure 3c); or (iv) absent peristalsis (no pressure domain >30 mm Hg, Figure 3d) (11). The 2.0 and 5.0 cm length cut points were chosen on the basis of observations made during concurrent manometry and fluoroscopy that breaks of < 2 cm in the 30 mm Hg isobaric contour rarely, if ever, compromised bolus clearance and breaks of ≥5 cm were invariably associated with incomplete clearance (8,12). Although not yet subject to systematic analysis, complete bolus clearance may or may not occur with intermediate size breaks (2.0–5.0 cm). The categorization for each swallow was performed for 20, 25, and 30 mm Hg isobaric contours.
Figure 3.
Classification of peristaltic integrity or hypotension. (a) Illustration of normal peristalsis through the smooth muscle segments (segments 2 and 3) with no breaks in the 20 or 30 mm Hg isobaric contour. (b) Illustration of an example of focal peristaltic hypotension analyzed at the 30 mm Hg isobaric contour with a 3.5-cm break (pink bracket line). (c) Illustration of diffuse peristaltic hypotension and (d) an example of absent peristalsis, both also analyzed at the 30 mm Hg isobaric contour.
Impedance assessment of bolus transit
Impedance line tracings for each swallow were analyzed for bolus clearance. At each impedance sensor, bolus entry was identified by a decrease in impedance of at least 50% relative to baseline and bolus clearance as a subsequent, sustained (≥5 s), ≥50% increase in impedance toward the original baseline (13). Complete bolus clearance was defined as bolus entry followed by sequential bolus clearance at all impedance-recording sites. Conversely, incomplete bolus clearance was defined as bolus entry without bolus clearance at one or more esophageal impedance-recording sites. Using these definitions, each swallow was characterized dichotomously as either complete or incomplete bolus clearance. In cases of incomplete bolus clearance, the locus of failure was characterized by anatomical location (transition zone, distal contractile segment, or both) and by the presence and length of breaks in the corresponding isobaric contour plots at that locus. In cases in which the boundary between the transition zone and the smooth muscle was not clear, such as with a hypotensive distal segment, we designated the lower boundary of the transition zone as occurring 2.0 cm distal to the distal margin of the 20 mm Hg isobaric contour of the proximal segment. That convention was based on 2.0 cm being the upper limit of normal (95th percentile) for transition zone length (14). To further delineate predictors of bolus clearance, we determined the maximal length of breaks in the 20 and 30 mm Hg isobaric contours that still facilitated complete bolus clearance. Similarly, in swallows with incomplete bolus clearance, we identified the shortest break associated with incomplete bolus clearance at each pressure threshold.
Patient categorization
After each patient’s 10 swallows were analyzed and categorized, we applied previously established manometric and impedance criteria to define their general swallow pattern (15,16). For an individual patient, abnormal bolus transit was defined as ≥30% liquid swallows with incomplete bolus clearance. In terms of pressure topography, patients with absent peristalsis on all manometry swallows were classified as absent peristalsis. Patients with focal peristaltic hypotension, diffuse peristaltic hypotension, or absent peristalsis in ≥30% but < 70% of test swallows were labeled as intermittent peristaltic hypotension, whereas those with ≥70% of swallows with these patterns had frequent peristaltic hypotension.
Statistical analysis
SPSS statistical software (SPSS, Chicago, IL, version 16.0.2) was used throughout. Given that single swallows are not independent observations, the statistical analysis of each subject’s 10 swallows was considered a single observation. Evaluation of the individual swallows in terms of defining upper limits of normal is presented as descriptive data and no comparisons were made.
RESULTS
A total of 16 asymptomatic controls (6 men, age: 24–37 year) and 8 patients (2 men, age: 19–59 years) were studied. All the eight patients had a chief complaint of dysphagia, one in the setting of previous fundoplication surgery. All subjects tolerated the study well and had normal deglutitive EGJ relaxation. Among the patient group, the mean EGJ nadir was 5.5 mm Hg (s.d. 3.5 mm Hg) with a maximum of 9.9 mm Hg. Among the control group, the mean EGJ nadir was 6.5 mm Hg (s.d. 2.3 mm Hg) with a maximum of 9.2 mm Hg. No subject had a hiatal hernia by pressure topography criteria. Hence, no subject was excluded from analysis because of abnormal EGJ morphology or function. Using the 30 mm Hg isobaric contour pressure to classify swallows as normal, focal hypotension, diffuse hypotension, or absent peristalsis, there were 3 control subjects with frequent peristaltic hypotension and 1 with intermittent peristaltic hypotension; the remaining 12 had normal peristalsis. In contrast, four patients had frequent peristaltic hypotension, one had intermittent peristaltic hypotension, and three had normal peristalsis. No subject in either group had absent peristalsis.
Concordance between bolus clearance and peristaltic function
Table 1 defines the concordance between the patient category on the basis of HRM definitions and impedance criteria for bolus transit (abnormal, ≥30% liquid swallows with incomplete bolus clearance). Of the 15 subjects with an intact 30 mm Hg isobaric contour (12 controls and 3 patients), all 15 had normal bolus transit. Of the seven subjects with frequent peristaltic hypotension (three controls and four patients), all seven had abnormal bolus transit (≥30% liquid swallows with incomplete bolus clearance). Of the two subjects with intermittent peristaltic hypotension, the patient had abnormal bolus transit, whereas the control subject had normal bolus transit. Thus, using these criteria we found 95.8% concordance (23 of 24) between manometric and impedance classification.
Table 1.
Concordance between HRM patient classification and impedance criteria for defining abnormal bolus transit
| Cutoff values isobaric contour |
Patient classification peristaltic function |
Normal bolus transit |
Abnormal bolus transit |
|---|---|---|---|
| 30 mm Hg 2-cm break |
Normal | 15 | 0 |
| Intermittent hypotension |
1 | 1 | |
| Frequent hypotension | 0 | 7 | |
| 20 mm Hg 2-cm break |
Normal | 16 | 0 |
| Intermittent hypotension |
0 | 2 | |
| Frequent hypotension | 0 | 5 | |
| 30 mm Hg 3-cm break |
Normal | 16 | 0 |
| Intermittent hypotension |
0 | 2 | |
| Frequent hypotension | 0 | 5 |
HRM, high-resolution manometry.
Applying the same classification criteria, but using the 20 mm Hg isobaric contour to assess peristalsis, one patient and one control were reclassified as intermittent rather than frequent peristaltic hypotension. One control subject (the one who had normal bolus transit in the setting of intermittent peristaltic hypotension using the 30 mm Hg threshold pressure) was also reclassified as normal rather than intermittent peristaltic hypotension. Consequently, using a 20 mm Hg isobaric contour to assess peristaltic integrity, 16 subjects had normal peristalsis (13 control subjects and 3 patients), 3 had intermittent peristaltic hypotension (1 control and 2 patients), and 5 had frequent peristaltic hypotension (2 controls and 3 patients) with 100% concordance (24 of 24) between manometric and impedance classification.
Modifying the defining criterion for focal hypotension with the 30 mm Hg isobaric contour plots to require a 3.0-cm break (vs. 2.0 cm) in the isobaric contour resulted in identical classification for all patients as occurred using the 2-cm break criterion with the 20 mm Hg isobaric contour plots. Hence, using the 3-cm break criterion with the 30 mm Hg isobaric contour also yielded 100% concordance (24 of 24) between manometric and impedance categorization.
Pressure topography predictors of bolus clearance in individual swallows
A total of 70 (29%) of the 240 swallows that were analyzed had incomplete bolus clearance; all of these exhibited breaks in the 30, 25, and 20 mm Hg isobaric contours of the peristaltic contraction. The 70 swallows with incomplete bolus clearance occurred among 6 patients and 8 controls. In all, 3 patients had 10 of 10 swallows associated with abnormal bolus transit, whereas 1 control patient also had 10 of 10 swallows associated with abnormal bolus transit.
With isobaric contour values < 20 mm Hg, incomplete bolus clearance was observed without breaks in the isobaric contour of the peristaltic contraction (Table 2); 11 instances of incomplete bolus clearance were observed with an intact 15 mm Hg isobaric contour and 21 instances of incomplete clearance occurred with an intact 10 mm Hg isobaric contour. It was also noted that among the 70 swallows with incomplete bolus clearance, there were no instances that had been classified as normal peristalsis because in all instances there was a break of ≥2-cm length in the isobaric contour. This remained true regardless of whether the 20, 25, or 30 mm Hg isobaric contour was used for classification, effectively verifying that a break of < 2.0 cm in the isobaric contour is still conducive to complete bolus clearance.
Table 2.
Breaks in the isobaric contour of the deglutitive peristaltic contraction as a predictor of complete bolus clearance for threshold amplitudes ranging from 10 to 30 mm Hg
| Isobaric contour pressure value (mm Hg) |
Breaks in isobaric contour? |
Complete bolus clearance (n = 170) |
Incomplete bolus clearance (n = 70) |
|---|---|---|---|
| 10 | No | 170 | 21 |
| Yes | 0 | 49 | |
| 15 | No | 170 | 11 |
| Yes | 0 | 59 | |
| 20 | No | 153 | 0 |
| Yes | 17 | 70 | |
| 25 | No | 142 | 0 |
| Yes | 28 | 70 | |
| 30 | No | 126 | 0 |
| Yes | 44 | 70 |
Breaks of any length were counted.
Swallow classification was somewhat dependent on the isobaric contour pressure value used to identify and measure breaks. Table 3 illustrates the effect this had on the distribution of the 240 swallows among classifications as well as the correspondence between those classifications and the completeness of bolus clearance. It is noteworthy that swallows classified as normal were uniformly associated with complete bolus clearance, whereas those classified as diffuse hypotension or absent peristalsis were uniformly associated with incomplete bolus clearance regardless of which isobaric contour value was used. Discrepancies between peristaltic integrity and the completeness of clearance were observed only with the focal hypotension classification: 13 swallows were associated with complete clearance despite classification as focal hypotension using 30 mm Hg as the isobaric contour threshold pressure as were 3 using the 25 mm Hg value. Only the 20 mm Hg isobaric contour threshold pressure exhibited complete agreement between a diagnosis of some degree of peristaltic weakness and complete bolus clearance, thus implying that a break of ≥2.0 cm in the 20 mm Hg isobaric esophageal contraction is not conducive to complete bolus clearance.
Table 3.
Integrity of esophageal peristalsis classified using 20, 25, or 30 mm Hg isobaric contour thresholds as a predictor of complete bolus clearance
| Isobaric contour threshold (mm Hg) |
Swallow classification | Complete bolus clearance (n = 170) |
Incomplete bolus clearance (n = 70) |
|---|---|---|---|
| 20 | Normal | 170 | 0 |
| Focal hypotension | 0 | 14 | |
| Diffuse hypotension | 0 | 30 | |
| Absent peristalsis | 0 | 26 | |
| 25 | Normal | 167 | 0 |
| Focal hypotension | 3 | 10 | |
| Diffuse hypotension | 0 | 34 | |
| Absent peristalsis | 0 | 26 | |
| 30 | Normal | 157 | 0 |
| Focal hypotension | 13 | 9 | |
| Diffuse hypotension | 0 | 35 | |
| Absent peristalsis | 0 | 26 |
Breaks in the isobaric contour <2 cm in length were classified as normal, 2 to 5 cm as focal hypotension, and 5 cm as diffuse hypotension.
Isobaric contour breaks associated with normal and abnormal bolus transit
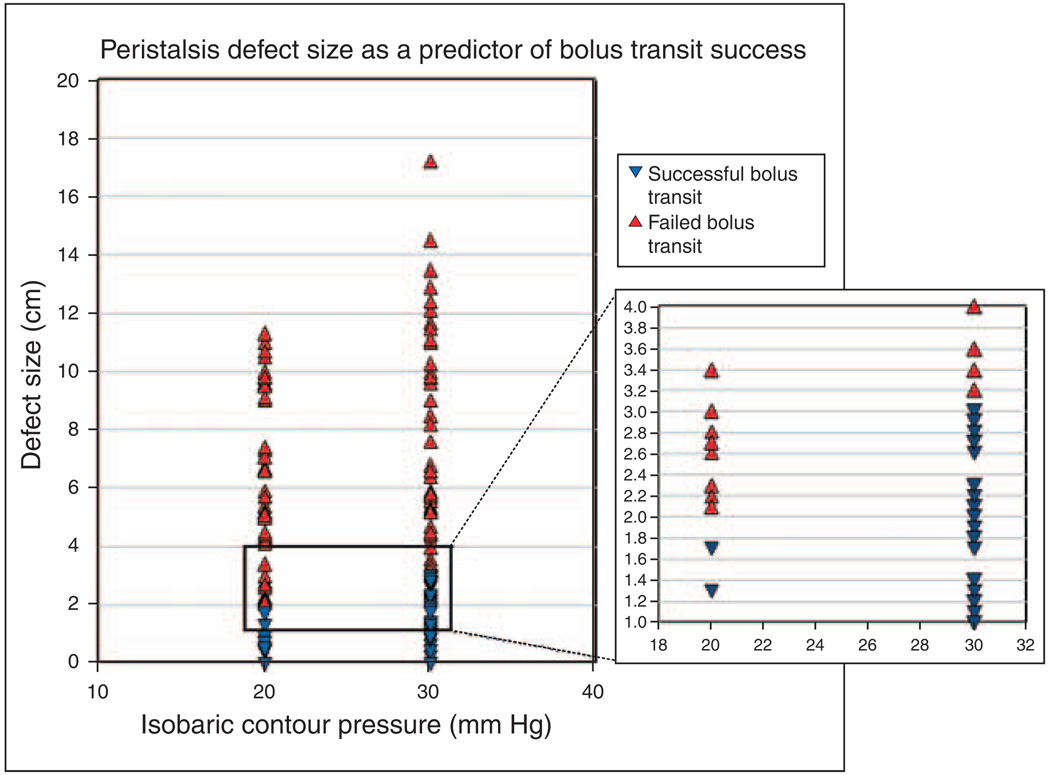
To further delineate the minimal pressure topography criteria necessary for achieving complete bolus clearance, swallows with complete bolus clearance were analyzed for the longest isobaric contour break observed, whereas those with incomplete clearance were analyzed for the shortest isobaric contour break observed (Figure 4). Using the 20 mm Hg isobaric contour threshold, the longest break associated with complete clearance was 1.7 cm and using the 30 mm Hg isobaric contour the longest break measured was 3.0 cm. Among the 70 cases of incomplete bolus clearance, there were 26 instances of absent peristalsis that could not be analyzed in this manner. The remaining 44 cases were analyzed for the shortest defect in the peristaltic wave front that was spatially associated with incomplete bolus clearance. Using the 20 mm Hg isobaric contour threshold, the shortest defect measured 2.1 cm in length, and using a 30 mm Hg isobaric contour threshold it was 3.2 cm. As demonstrated in Figure 4, there were no instances of overlap between the maximum defect predictive of complete bolus clearance and the minimum defect predictive of incomplete bolus clearance using pressure thresholds of either 20 or 30 mm Hg.
Figure 4.
Length of break in the 20 and 30 mm Hg isobaric contours vs. completeness of bolus clearance. Red triangles indicate complete clearance, whereas blue triangles denote incomplete clearance. A clear cutoff exists at 2 cm for the 20 mm Hg isobaric contour and at 3 cm for the 30 mm Hg isobaric contour above which there was uniform failure of clearance.
One consideration is that the four subjects (three patients and one control) with uniformly incomplete bolus clearance account for 40 of the 70 swallows with incomplete transit, and therefore could be driving the data. If those four subjects are removed from the analysis, a repeat analysis shows the shortest defect to be unchanged; 2.1 cm in the 20 mm Hg isobaric contour and 3.2 cm in the 30 mm Hg isobaric contour. The smallest defect found among the 40 swallows in the excluded group was 2.7 and 4.0 cm, respectively. Thus, the minimal manometric defect size associated with abnormal bolus transit does not seem to be altered by the type of subject or the frequency of abnormal bolus transit.
DISCUSSION
This study used combined multichannel intraluminal impedance and HRM to define the pressure topography characteristics of esophageal peristalsis necessary to affect complete clearance of a liquid bolus. The major findings were that in the context of normal EGJ morphology and deglutitive relaxation, peristalsis with an intact isobaric contour of ≥20 mm Hg was uniformly associated with complete bolus clearance. In cases in which there were breaks in the isobaric contour, a defect size of < 2 cm in the 20 mm Hg isobaric contour or 3 cm in the 30 mm Hg isobaric contour were also uniformly associated with complete bolus clearance. Breaks >2 cm (20 mm Hg isobaric contour) or 3 cm in length (30 mm Hg isobaric contour) were associated with incomplete bolus clearance. A break size >5 cm in length (20 or 30 mm Hg isobaric contour) was uniformly associated with incomplete bolus clearance.
The recent introduction and widespread adoption of esophageal pressure topography has led to the formulation of diagnostic criteria for esophageal motility disorders on the basis of pressure topography characteristics (16). In the initial iteration of this pressure topography classification, peristalsis was judged to be “hypotensive” on the basis of having a break of ≥2 cm length in the 30 mm Hg isobaric contour (16). That criterion was not established on the basis of a functional assessment, but rather on a best guess of what would be equivalent to hypotensive peristalsis diagnosed with conventional manometry. On the basis of the current findings, these criteria should be slightly revised such that a 2-cm break in the 20 mm Hg isobaric contour or a 3-cm break in the 30 mm Hg isobaric contour should be the requisite criteria for defining “focal peristaltic hypotension.”
Although impedance data were scored dichotomously in this study (complete or incomplete clearance), observations made in the course of conducting concurrent manometry and fluoroscopy make it very clear that incomplete bolus clearance does not necessarily equate to “failed transit” (1). Even a small fraction of residual swallowed bolus in the esophagus will result in that contraction being scored as associated with incomplete clearance. This would be especially true with the multitude of impedance segments used in this study (17). It was to emphasize this distinction that we proposed a two-tiered scoring of peristaltic weakness. Data from this study established that breaks in the 20, 25, or 30 mm Hg isobaric contour of the peristaltic contraction >5 cm in length were uniformly associated with incomplete bolus clearance, and observations from fluoroscopy suggested that defects of that length resulted in most if not all of the swallowed bolus being retained in the esophagus (1). Hence, in revising the classification of peristaltic hypotension, we propose that defects >5 cm in the isobaric contour of the peristaltic contraction (20 or 30 mm Hg) be classified as “diffuse peristaltic hypotension.” Finally, at the extreme end, “absent peristalsis” deserves a unique classification as this may not only imply poor performance in bolus clearance but may also serve as a defining criteria for the diagnosis of a major motor disorder, such as achalasia (18).
In summary, this study was facilitated by the recent development of a single recording device integrating multichannel intraluminal impedance and HRM technologies, thereby allowing their direct comparison. On the basis of our results, HRM data analyzed in terms of pressure topography can be used to accurately predict complete bolus clearance with peristalsis provided that EGJ morphology and relaxation are normal. The current findings are not applicable to instances of abnormal EGJ relaxation, morphological separation of the EGJ into distinct crural diaphragm and lower esophageal components indicative of hiatus hernia, or any condition associated with elevated esophageal intrabolus pressure. In those instances, concomitant intraluminal impedance monitoring or appropriate alternative pressure topography paradigms would need to be used to assess the completeness of bolus clearance (7,8,12). However, that would be the focus of future studies along with studies focused on the upright position and solid swallows. Similarly, further studies using the robust analysis possible with combined HRM and impedance monitoring will hopefully shed light on the determinants of esophageal symptoms, primarily dysphagia or pain, in patients with abnormalities of both peristalsis and the EGJ.
Study Highlights.
WHAT IS CURRENT KNOWLEDGE
Conventional manometry has significant limitations in defining bolus clearance.
Intraluminal impedance is a validated surrogate marker for bolus clearance that does not require radiation.
High-resolution manometry provides more detail in assessing esophageal contractile activity by increasing the number of pressure sensors while reducing axial separation of the recording sites.
WHAT IS NEW HERE
Defining peristaltic function using high-resolution manometry and an isobaric contour analysis will allow an accurate assessment of bolus clearance.
Peristaltic contractions with breaks <2 cm in the 20 mm Hg isobaric contour or <3 cm in the 30 mm Hg isobaric contour are associated with complete bolus clearance, whereas longer breaks predict incomplete bolus clearance.
High-resolution impedance manometry provides a complementary methodology for the assessment of esophageal function.
ACKNOWLEDGMENTS
We want to disclose a clerical protocol violation. A number of completed consent forms of study participants were inadvertently discarded during an office move, and this error was reported to the Northwestern University investigational review board.
Footnotes
CONFLICT OF INTEREST
Guarantor of the article: John E. Pandolfino, MD.
Specific author contributions: Study design, data analysis, writing, and performance of experiments: William J. Bulsiewicz; data analysis and writing: Peter J. Kahrilas; data analysis and performance of experiments: Monika A. Kwiatek; performance of experiments: Sudip K. Ghosh; hardware consultation and troubleshooting: Albert Meek; study design, primary data analysis, and writing: John E. Pandolfino. Albert Meek is employed by MMS, however, his input on the paper was confined to providing the hardware/catheter and troubleshooting software issues with the new HRIM analysis program.
Financial support: This work was supported by R01 DC00646 (PJK and JEP) from the Public Health Service.
Potential competing interests: None.
REFERENCES
- 1.Kahrilas PJ, Dodds WJ, Hogan WJ. Effect of peristaltic dysfunction on esophageal volume clearance. Gastroenterology. 1988;94:73–80. doi: 10.1016/0016-5085(88)90612-9. [DOI] [PubMed] [Google Scholar]
- 2.Ren J, Massey BT, Dodds WJ, et al. Determinants of intrabolus pressure during esophageal peristaltic bolus transport. Am J Physiol. 1993;264(3 Pt 1):G407–G413. doi: 10.1152/ajpgi.1993.264.3.G407. [DOI] [PubMed] [Google Scholar]
- 3.Leite LP, Johnston BT, Barrett J, et al. Ineffective esophageal motility (IEM): the primary finding in patients with nonspecific esophageal motility disorder. Dig Dis Sci. 1997;42:1859–1865. doi: 10.1023/a:1018802908358. [DOI] [PubMed] [Google Scholar]
- 4.Spechler SJ, Castell DO. Classification of oesophageal motility abnormalities. Gut. 2001;49:145–151. doi: 10.1136/gut.49.1.145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tutuian R, Castell DO. Clarification of the esophageal function defect in patients with manometric ineffective esophageal motility: studies using combined impedance-manometry. Clin Gastroenterol Hepatol. 2004;2:230–236. doi: 10.1016/s1542-3565(04)00010-2. [DOI] [PubMed] [Google Scholar]
- 6.Conchillo JM, Nguyen NQ, Samsom M, et al. Multichannel intraluminal impedance monitoring in the evaluation of patients with non-obstructive dysphagia. Am J Gastroenterol. 2005;100:2624–2632. doi: 10.1111/j.1572-0241.2005.00303.x. [DOI] [PubMed] [Google Scholar]
- 7.Sloan S, Kahrilas PJ. Impairment of esophageal emptying with hiatal hernia. Gastroenterology. 1991;100:596–605. doi: 10.1016/0016-5085(91)80003-r. [DOI] [PubMed] [Google Scholar]
- 8.Pandolfino JE, Ghosh SK, Lodhia N, et al. Utilizing intraluminal pressure gradients to predict esophageal clearance: a validation study. Am J Gastroenterol. 2008;103:1898–1905. doi: 10.1111/j.1572-0241.2008.01913.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fox M, Hebbard G, Janiak P, et al. High-resolution manometry predicts the success of oesophageal bolus transport and identifies clinically important abnormalities not detected by conventional manometry. Neurogastroenterol Motil. 2004;16:533–542. doi: 10.1111/j.1365-2982.2004.00539.x. [DOI] [PubMed] [Google Scholar]
- 10.Kahrilas PJ, Kim HC, Pandolfino JE. Approaches to the diagnosis and grading of hiatal hernia. Clin Gastroenterol. 2008;22:601–616. doi: 10.1016/j.bpg.2007.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kahrilas PJ, Ghosh SK, Pandolfino JE. Esophageal motility disorders in terms of pressure topography: the Chicago Classification. J Clin Gastroenterol. 2008;42:627–635. doi: 10.1097/MCG.0b013e31815ea291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ghosh SK, Kahrilas PJ, Lodhia N, et al. Utilizing intraluminal pressure differences to predict esophageal bolus flow dynamics. Am J Physiol Gastrointest Liver Physiol. 2007;293:G1023–G1028. doi: 10.1152/ajpgi.00384.2007. [DOI] [PubMed] [Google Scholar]
- 13.Sifrim D, Castell D, Dent J, et al. Gastro-oesophageal reflux monitoring: review and consensus report on detection and definitions of acid, non-acid, and gas reflux. Gut. 2004;53:1024–1031. doi: 10.1136/gut.2003.033290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ghosh SK, Pandolfino JE, Kwiatek MA, et al. Oesophageal peristaltic transition zone defects: real but few and far between. Neurogastroenterol Motil. 2008;20:1283–1290. doi: 10.1111/j.1365-2982.2008.01169.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Simren M, Silny J, Holloway R, et al. Relevance of ineffective oesophageal motility during oesophageal acid clearance. Gut. 2003;52:784–790. doi: 10.1136/gut.52.6.784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pandolfino JE, Ghosh SK, Rice J, et al. Classifying esophageal motility by pressure topography characteristics: a study of 400 patients and 75 controls. Am J Gastroenterol. 2008;103:27–37. doi: 10.1111/j.1572-0241.2007.01532.x. [DOI] [PubMed] [Google Scholar]
- 17.Blom D, Mason R, Balaji N, et al. Esophageal bolus transport measured by simultaneous multichannel intraluminal impedance and manometry (abstract) Gastroenterology. 2001;120:a–220. [Google Scholar]
- 18.Pandolfino JE, Kwiatek MA, Nealis T, et al. Achalasia: anew clinically relevant classification by high-resolution manometry. Gastroenterology. 2008;135:1526–1533. doi: 10.1053/j.gastro.2008.07.022. [DOI] [PMC free article] [PubMed] [Google Scholar]