Abstract
The purpose of this prospective, randomized, double-blind crossover study was to evaluate the anesthetic efficacy of 2% lidocaine with 1 : 100,000 epinephrine, 4% prilocaine with 1 : 200,000 epinephrine, and 4% prilocaine in maxillary lateral incisors and first molars. Sixty subjects randomly received, in a double-blind manner, maxillary lateral incisor and first molar infiltrations of 1.8 mL of 2% lidocaine with 1 : 100,000 epinephrine, 1.8 mL of 4% prilocaine with 1 : 200,000 epinephrine, and 1.8 mL of 4% prilocaine, at 3 separate appointments spaced at least 1 week apart. The teeth were pulp-tested in 3-minute cycles for a total of 60 minutes. Anesthetic success (ie, obtaining 2 consecutive 80 readings with the electric pulp tester) and onset of pulpal anesthesia were not significantly different between 2% lidocaine with 1 : 100,000 epinephrine, 4% prilocaine with 1 : 200,000 epinephrine, and 4% prilocaine for the lateral incisor and first molar. For both lateral incisor and first molar, 4% prilocaine with 1 : 200,000 epinephrine and 2% lidocaine with 1 : 100,000 epinephrine were equivalent for incidence of pulpal anesthesia. However, neither anesthetic agent provided an hour of pulpal anesthesia. For both lateral incisor and first molar, 4% prilocaine provided a significantly shorter duration of pulpal anesthesia compared with 2% lidocaine with 1 : 100,000 epinephrine and 4% prilocaine with 1 : 200,000 epinephrine.
Keywords: Lidocaine, Epinephrine, Prilocaine, Infiltration, Maxillary
Maxillary infiltration anesthesia is a common method of anesthetizing maxillary teeth. Previous studies1–18 have evaluated the success of maxillary infiltrations using the electric pulp tester. With a volume of ≤1.8 mL and various anesthetic formulations, pulpal anesthetic success (ie, obtaining maximum output with an electric pulp tester) ranged from 62–100%.
Four percent prilocaine with 1 : 200,000 epinephrine has been found to be equivalent to 2% lidocaine with 1 : 100,000 epinephrine for inferior alveolar nerve blocks.19 Haas and coauthors4,5 compared infiltrations of 4% articaine and 4% prilocaine formulations with epinephrine in maxillary canines and second molars. They found no statistical differences between the 2 anesthetic formulations. Further investigation of 4% prilocaine with 1 : 200,000 epinephrine is needed to ensure its appropriate clinical use.
Four percent prilocaine plain has been found to be equivalent to 2% lidocaine with 1 : 100,000 epinephrine for inferior alveolar nerve blocks.20 However, Brown and Ward21 compared 4% prilocaine versus 2% lidocaine with 1 : 100,000 epinephrine for maxillary infiltrations and found that 4% prilocaine had a shorter duration of anesthesia. Although numerous studies have evaluated infiltration injections in the posterior maxilla,4,5,9,12–15,18 none have compared 4% prilocaine to 4% prilocaine with 1 : 200,000 epinephrine. Because anesthesia may vary between anterior and posterior maxilla, it would be of interest to study first molar infiltration anesthesia.
The efficacy of 2% lidocaine with 1 : 100,000, 4% prilocaine with 1 : 200,000 epinephrine, and 4% prilocaine in providing pulpal anesthesia when administered to human maxillary teeth should be further investigated to ensure their appropriate clinical use. The purpose of this prospective, randomized, double-blind crossover study was to evaluate the anesthetic efficacy of 2% lidocaine with 1 : 100,000 epinephrine, 4% prilocaine with 1 : 200,000 epinephrine, and 4% prilocaine in maxillary lateral incisors and first molars.
MATERIALS AND METHODS
Sixty adult subjects participated in this study. All subjects were in good health and were not taking any medication that would alter pain perception, as determined by a written health history and oral questioning. Exclusion criteria were as follows: younger than 18 or older than 65 years of age, allergies to local anesthetics or sulfites, pregnancy, history of significant medical conditions (American Society of Anesthesiology [ASA] II or higher), taking any medications that may affect anesthetic assessment (over-the-counter pain-relieving medications, narcotics, sedatives, antianxiety or antidepressant medications), active sites of pathosis in area of injection, and inability to give informed consent. The Ohio State University Review Committee approved the study, and written informed consent was obtained from each subject.
Using a crossover design, 30 subjects received 3 maxillary lateral incisor infiltrations, and 30 subjects received 3 maxillary first molar infiltrations, at 3 separate appointments spaced at least 1 week apart. For each lateral incisor or first molar, the 3 infiltrations consisted of 1.8 mL of 2% lidocaine with 1 : 100,000 epinephrine, 1.8 mL of 4% prilocaine with 1 : 200,000 epinephrine, and 1.8 mL of 4% prilocaine.
With the crossover design, 90 infiltrations were administered for the lateral incisor and 90 infiltrations for the first molar, and each subject served as his or her own control. Fifteen maxillary right lateral incisors and 15 maxillary left lateral incisors were used. Fifteen maxillary right first molars and 15 maxillary left first molars were used. The same side chosen for the first infiltration was used again for the second and third infiltrations. The same tooth was used at the 3 visits for each anesthetic solution. The contralateral canine was used as the control to ensure that the pulp tester was operating properly, and that the subject was responding appropriately. A visual and clinical examination was conducted to ensure that all teeth were free of caries, large restorations, crowns, and periodontal disease, and that none had a history of trauma or sensitivity.
Before injections were given at all appointments, the experimental tooth and the contralateral canine (control) were tested 3 times with the electric pulp tester (Analytic Technology Corp, Redmond, Wash) to obtain baseline information. The teeth were isolated with cotton rolls and dried with an air syringe. Toothpaste was applied to the probe tip, which was placed in the middle third of the facial or buccal surface of the tooth being tested. The value at the initial sensation was recorded. The current rate was set at 25 seconds to increase from no output (0) to maximum output (80). Trained personnel, who were blinded to the anesthetic solutions, administered all preinjection and postinjection tests.
Before the experiment was begun, the 3 anesthetic solutions were randomly assigned 4-digit numbers from a random number table generated by Microsoft Office Excel (Microsoft Corporation, Redmond, Wash). The random numbers were assigned to a subject to designate which anesthetic solution was to be administered at each appointment.
Under sterile conditions, the 2% lidocaine cartridges with 1 : 100,000 epinephrine (Xylocaine, Astra Pharmaceuticals Products Inc, Worcester, Mass), the 4% prilocaine cartridges with 1 : 200,000 epinephrine (Citanest Forte, Astra), and the 4% prilocaine cartridges (Citanest, Astra) were masked with opaque labels, and the cartridge caps and plungers were masked with a black felt tip marker. Corresponding 4-digit codes were written on each cartridge label. All anesthetic solutions were checked to ensure that the anesthetic solution had not expired.
A standard maxillary infiltration injection was administered with an aspirating syringe and a 27-gauge 1-inch needle (Sherwood Medical Co, St Louis, Mo). The target site was centered over the root apex of the maxillary lateral incisor or between the mesiobuccal and distobuccal root apices of the maxillary first molar. The needle was gently placed into the alveolar mucosa with the bevel toward bone and was advanced until the needle was estimated to be at or just superior to the apex of the lateral incisor or the apices of the first molar. The anesthetic formulation was deposited over a period of 1 minute. All infiltrations were given by the senior author (S.K.).
Depth of anesthesia was monitored with the electric pulp tester. At 1 minute after the infiltration injection, pulp test readings were obtained for the experimental tooth (first molar or lateral incisor) and the contralateral maxillary canine. Testing continued in 3-minute cycles for a total of 60 minutes. At every third cycle, the control tooth—the contralateral canine—was tested by an inactivated electric pulp tester to test the reliability of the subject, that is, if subjects responded positively to an inactivated pulp tester, then they were not reliable and could not be used in the study.
No response from the subject at the maximum output (80 reading) of the pulp tester was used as the criterion for pulpal anesthesia. Anesthesia was considered successful when 2 consecutive 80 readings with the pulp tester were obtained within 10 minutes after the infiltration. With a nondirectional alpha risk of 0.05 and a power of 80%, and assuming an anesthetic success rate of 75%, a sample size of 30 subjects per tooth group was required to demonstrate a difference in anesthetic success of ±25 percentage points. Onset of anesthesia was defined as the first of 2 consecutive 80 readings. Anesthesia was of short duration if the subject achieved 2 consecutive 80 readings, lost the 80 reading, and never regained it within the 60-minute period.
The data were analyzed statistically. Group comparisons among the lidocaine formulation and the prilocaine formulations for anesthetic success, incidence of pulpal anesthesia, and short duration of anesthesia were analyzed with the use of multiple McNemar tests, with P values adjusted by means of the step-down method of Holm. Onset of anesthesia was assessed by a 1-way repeated measures analysis of variance and Tukey-Kramer procedure. Comparisons were considered significant at P < .05.
RESULTS
For the lateral incisor, 25 men and 5 women ranging in age from 22–31 years, with an average age of 25 years, participated in this study. For the first molar, 20 men and 10 women ranging in age from 22–33 years, with an average age of 25 years, participated.
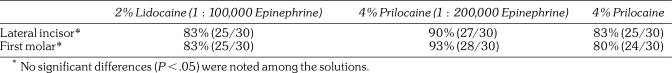
Table 1 demonstrates the percentages of successful pulpal anesthesia. Success rates ranged from 80–93%. No significant differences were noted among the anesthetic formulations.
Table 1.
Percentages and Number of Subjects Who Experienced Anesthetic Success
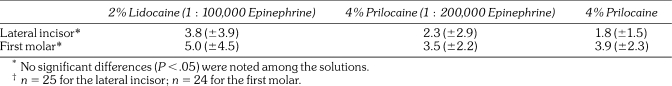
The onset of pulpal anesthesia is provided in Table 2. No significant differences were noted among the anesthetic formulations.
Table 2.
Onset of Pulpal Anesthesia (minutes ± standard deviation)†
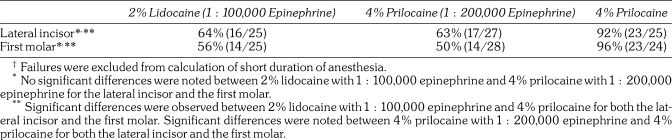
Anesthesia of short duration is presented in Table 3. No significant differences were noted between 2% lidocaine with 1 : 100,000 epinephrine and 4% prilocaine with 1 : 200,000 epinephrine for the lateral incisor and first molar. The 4% prilocaine formulation had a significantly increased incidence of anesthesia of short duration when compared with the lidocaine and prilocaine formulations with epinephrine.
Table 3.
Percentages and Numbers of Subjects Who Experienced Short Duration of Anesthesia†
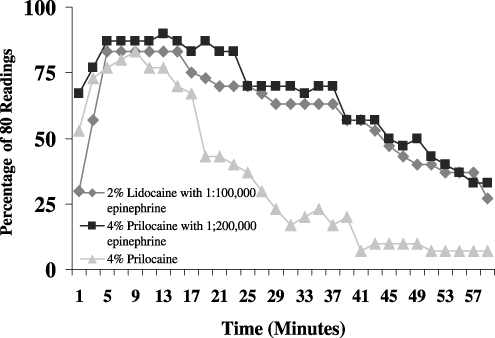
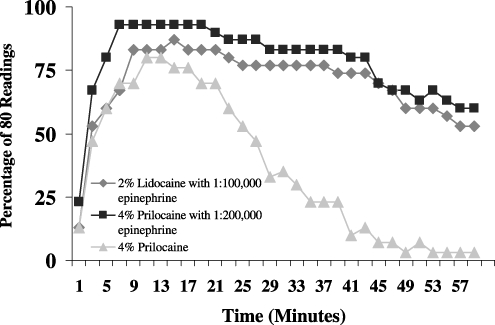
The incidence of pulpal anesthesia (80 readings across time) for the 3 anesthetic solutions is presented in Figures 1 and 2.
Figure 1.
Incidence of maxillary lateral incisor pulpal anesthesia as determined by lack of response to electric pulp testing at the maximum setting (percentage of 80 readings), at each postinjection time interval, for the 3 anesthetic solutions.
Figure 2.
Incidence of maxillary first molar pulpal anesthesia as determined by lack of response to electric pulp testing at the maximum setting (percentage of 80 readings), at each postinjection time interval, for the 3 anesthetic solutions.
DISCUSSION
We based our use of the pulp test reading of 80—signaling maximum output—as a criterion for pulpal anesthesia on the studies of Dreven and colleagues22 and Certosimo and Archer.23 These studies22,23 showed that no patient response to an 80 reading ensured pulpal anesthesia in vital, asymptomatic teeth. Additionally, Certosimo and Archer23 demonstrated that electric pulp test readings of less than 80 resulted in pain during operative procedures in asymptomatic teeth. Therefore, using the electric pulp tester before beginning dental procedures on asymptomatic, vital teeth will provide the clinician with a reliable indicator of pulpal anesthesia.
The success of the infiltration of 2% lidocaine with 1 : 100,000 epinephrine was 83% in the lateral incisor (Table 1). Various authors1–18 have evaluated the success of maxillary infiltrations using the electric pulp tester. Generally, results of these studies have demonstrated successful anesthesia ranging from 62–100%. It is very difficult to compare the results of previous studies with those of the current study because the authors used different dosages of anesthetic agents and vasoconstrictors and evaluated different teeth. Nusstein et al,11 Gross et al,13 Mikesell et al,14 Evans et al,15 Scott et al,17 and Mason et al18 used similar methods to those used in the current study and reported 85, 97, 97, 62, 95–100, and 100% success rates, respectively, for the lateral incisor with an infiltration of 1.8 mL of 2% lidocaine with 1 : 100,000 epinephrine. Regarding the first molar, the success rate was 83% with 2% lidocaine with 1 : 100,000 epinephrine (Table 2). Gross et al,13 Mikesell et al,14 Evans et al,15 and Mason et al18 used a similar method to that used in the current study and demonstrated 82, 100, 72, and 97% success rates, respectively, for the first molar with an infiltration of 1.8 mL of 2% lidocaine with 1 : 100,00 epinephrine. The success rates for both lateral incisor and first molar in these studies11,13–15,17,18 show some variation, which may be related to population or operator differences. In general, the infiltration injection of 1.8 mL of 2% lidocaine with 1 : 100,000 epinephrine may not always be 100% successful because of individual variations in response to the drug administered, operator differences, and variations in anatomy as well as tooth position.
The success rate of the infiltration of 4% prilocaine with 1 : 200,000 epinephrine was 90% in the lateral incisor and 93% in the first molar (Table 1). No significant differences were observed between the lidocaine and prilocaine formulations with epinephrine. Therefore, the 2 anesthetic formulations were equivalent for pulpal anesthesia in the lateral incisor and first molar. Haas and coauthors4,5 compared infiltrations of 4% articaine and 4% prilocaine formulations with 1 : 200,000 epinephrine in maxillary canines and second molars. They found no statistical differences between the 2 anesthetic formulations. The success rate (80 readings on the pulp tester) of the articaine solution was 65% for the canine infiltration and 95% for the second molar infiltration. The success rate for the canine (65%) was lower than the success rate of 90% for the lateral incisor in the current study, and the success rate of 93% for the first molar was similar to that recorded by Haas et al.4,5 Differences in the subject population, use of different teeth, use of a smaller number of subjects, or use of 1.5 mL of anesthetic solution in Haas' studies4,5 may account for the differences in success rates. Because we studied a young adult population, the results of this study may not apply to children or the elderly.
The success of the infiltration of 4% prilocaine was 83% in the lateral incisor and 80% in the first molar (Table 1). Because the definition of success did not include the duration of pulpal anesthesia, no significant difference was noted among the anesthetic solutions. However, as will be discussed, 4% prilocaine provided a shorter duration of pulpal anesthesia.
In the lateral incisor, mean onset times ranged from 1.8–3.8 minutes with no statistical differences among the 3 solutions (Table 2). Gross et al,13 Mikesell et al,14 Nusstein et al,11 Evans et al,15 Scott et al,17 and Mason et al,18 using 1.8 mL of 2% lidocaine with 1 : 100,000 epinephrine, reported onset times for the lateral incisor of 2.5, 2.9, 5.1, 3.0, 4.7, and 2.7–3.9 minutes, respectively. Except for Nusstein et al11 and Scott et al,17 the results are similar for the current study. In the first molar, mean onset times ranged from 3.5–5.0 minutes with no statistical differences among the 3 solutions (Table 2). Gross et al,13 Mikesell et al,14 Evans et al,15 and Mason et al,18 using 1.8 mL of 2% lidocaine with 1 : 100,000 epinephrine, reported onset times for the first molar of 4.3, 4.7, 3.7, and 3.9–5.1 minutes, respectively. Other authors1–10 have reported onset times of 2–5 minutes for maxillary infiltrations using lidocaine solutions. Decreasing the epinephrine concentration to 1 : 200,000 in a 4% prilocaine formulation or using a plain solution of 4% prilocaine did not increase the onset of pulpal anesthesia. Therefore, in general, onset times for maxillary infiltrations with these solutions would range from 2–5 minutes.1–10,13–15,17,18 Pulp testing of the tooth with an electric pulp tester or a cold refrigerant will give the clinician a reliable indicator of onset of pulpal anesthesia.
Figure 1 demonstrates the decline of pulpal anesthesia over 60 minutes for the lateral incisor. For the 2% lidocaine with 1 : 100,000 epinephrine formulation, approximately 63% of subjects had pulpal anesthesia at 30 minutes, 47% at 45 minutes, and only 27% at 60 minutes. Nusstein et al,11 Gross et al,13 Mikesell et al,14 Evans et al,15 Scott et al,17 and Mason et al18 also showed similar declining rates of pulpal anesthesia when using 1.8 mL of 2% lidocaine with 1 : 100,000 epinephrine. The 4% prilocaine with 1:200,000 epinephrine showed a pattern of pulpal anesthesia similar to that of the lidocaine formulation—with approximately 70% of subjects having pulpal anesthesia at 30 minutes, 50% at 45 minutes, and only 33% at 60 minutes (Figure 1). Anesthesia of short duration was not significantly different between the lidocaine and prilocaine formulations with epinephrine. Therefore, the 2 formulations were equivalent for pulpal anesthesia in the lateral incisor. Mikesell et al14 demonstrated a statistically slower decline of pulpal anesthesia with a 3.6-mL volume of 2% lidocaine with 1 : 100,000 epinephrine over 60 minutes for the lateral incisor when compared with the 1.8-mL volume—with 72% of subjects having pulpal anesthesia at 45 minutes and 50% at 60 minutes. Therefore, using a 3.6-mL volume of 2% lidocaine with 1 : 100,000 epinephrine will increase the duration of pulpal anesthesia but will not provide complete pulpal anesthesia for an hour. Mason et al18 found that 1.8 mL of 2% lidocaine with 1 : 50,000 epinephrine maintained a significantly higher percentage of pulpal anesthesia, from minute 37 through minute 60, than did 1.8 mL of 2% lidocaine with 1 : 100,000 epinephrine. Approximately 97% of subjects had pulpal anesthesia at 45 minutes and almost 80% at 60 minutes. Scott et al17 found repeated infiltration of 1.8 mL of 2% lidocaine with 1 : 100,000 epinephrine 30 minutes after an initial infiltration of the same dose of anesthetic significantly improved the duration of pulpal anesthesia, from 37 minutes through 90 minutes, in the maxillary lateral incisor. They found that 90% of subjects had pulpal anesthesia at 60 minutes for the repeated infiltration. Therefore, if pulpal anesthesia is required for 60 minutes in the lateral incisor, an initial dose of 1.8 mL of 2% lidocaine with 1 : 50,000 epinephrine or repeated infiltration at 30 minutes using 1.8 mL of 2% lidocaine with 1 : 100,000 epinephrine should be reasonably effective. A future study could determine whether duration would be prolonged when an initial infiltration of 3.6 mL volume of 4% prilocaine with 1 : 200,000 epinephrine is given, or when 1.8 mL of 4% prilocaine with 1 : 200,000 epinephrine is administered at 30 minutes.
Figure 1 demonstrates a significant decline in pulpal anesthesia with the 4% prilocaine formulation in the lateral incisor. Approximately 43% of subjects had pulpal anesthesia at 20 minutes, 23% at 30 minutes, and 7% at 60 minutes. Anesthesia of short duration was significantly higher with the 4% prilocaine formulation than with the lidocaine and prilocaine formulations with epinephrine (Table 3). Brown and Ward21 also demonstrated a shorter duration of pulpal anesthesia with 4% prilocaine in maxillary infiltrations.
In the first molar, a slower decline of pulpal anesthesia was demonstrated for both 2% lidocaine with 1 : 100,000 and 4% prilocaine with 1 : 200,000 epinephrine than in the lateral incisor (Figure 2). Gross et al,13 Mikesell et al,14 Evans et al,15 and Mason et al18 also showed a similar pattern of pulpal anesthesia of the first molar when using 1.8 mL of 2% lidocaine with 1 : 100,000 epinephrine. No significant difference in incidence of pulpal anesthesia or anesthesia of short duration was noted between the lidocaine and prilocaine formulations with epinephrine (Figure 2, Table 3). Therefore, the 2 formulations are equivalent for pulpal anesthesia in the first molar. Recently, Mikesell et al14 demonstrated that increasing the amount of lidocaine from 1.8 mL to 3.6 mL provided a longer duration of pulpal anesthesia after about 49 minutes for the first molar. However, complete pulpal anesthesia was not obtained for 60 minutes. In the current study, pulpal anesthesia started to decline for the lidocaine and prilocaine formulations with epinephrine after about 45 minutes (Figure 2). It is important to realize that if an hour of pulpal anesthesia is required for the first molar, 1.8 mL of 2% lidocaine with 1 : 100,000 or 4% prilocaine with 1 : 200,000 epinephrine may not provide the necessary duration of pulpal anesthesia.
Figure 2 demonstrates a significant decline in pulpal anesthesia with the 4% prilocaine formulation in the first molar. Approximately 70% of subjects had pulpal anesthesia at 20 minutes, 35% at 30 minutes, and only 7% at 47 minutes. Anesthesia of short duration was significantly higher with the 4% prilocaine formulation than with the lidocaine and prilocaine formulations with epinephrine (Table 3).
CONCLUSIONS
Onset of pulpal anesthesia was not significantly different between 2% lidocaine with 1 : 100,000 epinephrine, 4% prilocaine with 1 : 200,000 epinephrine, and 4% prilocaine for the maxillary lateral incisor and first molar.
Anesthetic success was not significantly different between 2% lidocaine with 1 : 100,000 epinephrine, 4% prilocaine with 1 : 200,000 epinephrine, and 4% prilocaine for the maxillary lateral incisor and first molar.
For both maxillary lateral incisor and first molar, 4% prilocaine with 1 : 200,000 epinephrine and 2% lidocaine with 1 : 100,000 epinephrine were equivalent for incidence of pulpal anesthesia. However, neither anesthetic agent provided an hour of pulpal anesthesia.
For both maxillary lateral incisor and first molar, 4% prilocaine provided a significantly shorter duration of pulpal anesthesia compared with 2% lidocaine with 1 : 100,000 epinephrine or 4% prilocaine with 1 : 200,000 epinephrine.
REFERENCES
- 1.Bjorn H., Huldt S. The efficiency of Xylocaine as a dental terminal anesthetic as compared to that of procaine. Svensk Tandl Tidskr. 1947;40:831–852. [Google Scholar]
- 2.Petersen J. K., Luck H., Kristensen F. A comparison of four commonly used local analgesics. Int J Oral Surg. 1977;6:51–59. doi: 10.1016/s0300-9785(77)80059-8. [DOI] [PubMed] [Google Scholar]
- 3.Nordenram A., Danielsson K. Local anesthesia in elderly patients: an experimental study of oral infiltration anaesthesia. Swed Dent J. 1990;14:19–24. [PubMed] [Google Scholar]
- 4.Haas D. A., Harper D. G., Saso M. A., Young E. R. Lack of differential effect by Ultracaine (articaine) and Citanest (prilocaine) in infiltration anesthesia. J Can Dent Assoc. 1991;57:217–223. [PubMed] [Google Scholar]
- 5.Haas D. A., Harper D. G., Saso M. A., Young E. R. Comparison of articaine and prilocaine anesthesia by infiltration in maxillary and mandibular arches. Anesth Prog. 1990;37:230–237. [PMC free article] [PubMed] [Google Scholar]
- 6.Knöll-Kohler E., Förtsch G. Pulpal anesthesia dependent on epinephrine dose in 2% lidocaine: a randomized controlled double-blind crossover study. Oral Surg Oral Med Oral Pathol. 1992;73:537–540. doi: 10.1016/0030-4220(92)90091-4. [DOI] [PubMed] [Google Scholar]
- 7.Vahatalo K., Antila H., Lehtinen R. Articaine and lidocaine for maxillary infiltration anesthesia. Anesth Prog. 1993;40:114–116. [PMC free article] [PubMed] [Google Scholar]
- 8.Pitt Ford T. R., Seare M. A., McDonald F. Action of adrenaline on the effect of dental local anaesthetic solutions. Endod Dent Traumatol. 1993;9:31–35. doi: 10.1111/j.1600-9657.1993.tb00457.x. [DOI] [PubMed] [Google Scholar]
- 9.Premdas C. E., Pitt Ford T. R. Effect of palatal injections on pulpal blood flow in premolars. Endod Dent Traumatol. 1995;11:274–278. doi: 10.1111/j.1600-9657.1995.tb00503.x. [DOI] [PubMed] [Google Scholar]
- 10.Chng H. S., Pitt Ford T. R., McDonald F. Effects of prilocaine local anesthetic solutions on pulpal blood flow in maxillary canines. Endod Dent Traumatol. 1996;12:89–95. doi: 10.1111/j.1600-9657.1996.tb00103.x. [DOI] [PubMed] [Google Scholar]
- 11.Nusstein J., Wood M., Reader A., Beck M., Weaver J. Comparison of the degree of pulpal anesthesia achieved with the intraosseous injection and infiltration injection using 2% lidocaine with 1:100,000 epinephrine. Gen Dent. 2005;53:50–53. [PubMed] [Google Scholar]
- 12.Costa C. G., Tortamano I. P., Rocha R. G., Francishone C. E., Tortamano N. Onset and duration periods of articaine and lidocaine on maxillary infiltration. Quintessence Int. 2005;36:197–201. [PubMed] [Google Scholar]
- 13.Gross R., McCartney M., Reader A., Beck M. A prospective, randomized, double-blind comparison of bupivacaine and lidocaine for maxillary infiltrations. J Endod. 2007;33:1021–1024. doi: 10.1016/j.joen.2007.06.003. [DOI] [PubMed] [Google Scholar]
- 14.Mikesell A., Drum M., Reader A., Beck M. Anesthetic efficacy of 1.8 mL and 3.6 mL of 2% lidocaine with 1 : 100,000 epinephrine for maxillary infiltrations. J Endod. 2008;34:121–125. doi: 10.1016/j.joen.2007.11.001. [DOI] [PubMed] [Google Scholar]
- 15.Evans G., Nusstein J., Drum M., Reader A., Beck M. A prospective, randomized double-blind comparison of articaine and lidocaine for maxillary infiltrations. J Endod. 2008;34:389–393. doi: 10.1016/j.joen.2008.01.004. [DOI] [PubMed] [Google Scholar]
- 16.Brunetto P. C., Ranali J., Ambrosano G. M. B., et al. Anesthetic efficacy of 3 volumes of lidocaine with epinephrine in maxillary infiltration anesthesia. Anesth Prog. 2008;55:29–34. doi: 10.2344/0003-3006(2008)55[29:AEOVOL]2.0.CO;2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Scott J., Drum M., Reader A., Nusstein J., Beck M. The efficacy of a repeated infiltration in prolonging duration of pulpal anesthesia in maxillary lateral incisors. J Am Dent Assoc. 2009;140:318–324. doi: 10.14219/jada.archive.2009.0161. [DOI] [PubMed] [Google Scholar]
- 18.Mason R., Drum M., Reader A., Nusstein J., Beck M. A prospective, randomized, double-blind comparison of 2% lidocaine with 1 : 100,000 and 1 : 50,000 epinephrine and 3% mepivacaine for maxillary infiltrations. J Endod. 2009;35:1173–1177. doi: 10.1016/j.joen.2009.06.016. [DOI] [PubMed] [Google Scholar]
- 19.Hinkley S., Reader A., Beck M., Meyers W. An evaluation of 4% prilocaine with 1 : 200,000 epinephrine and 2% mepivacaine with levonordefrin compared to 2% lidocaine with 1 : 100,000 epinephrine for inferior alveolar nerve block. Anesth Prog. 1991;38:84–89. [PMC free article] [PubMed] [Google Scholar]
- 20.McLean C., Reader A., Beck M., Meyers W. J. An evaluation of 4% prilocaine and 3% mepivacaine compared to 2% lidocaine (1 : 100,000 epinephrine) for inferior alveolar nerve block. J Endod. 1993;19:146–150. doi: 10.1016/s0099-2399(06)80510-8. [DOI] [PubMed] [Google Scholar]
- 21.Brown G., Ward N. L. Prilocaine and lignocaine plus adrenaline. Brit Dent J. 1969;126:557–562. [PubMed] [Google Scholar]
- 22.Dreven L., Reader A., Beck M., Meyers W., Weaver J. An evaluation of the electric pulp tester as a measure of analgesia in human vital teeth. J Endod. 1987;13:233–238. doi: 10.1016/s0099-2399(87)80097-3. [DOI] [PubMed] [Google Scholar]
- 23.Certosimo A., Archer R. A clinical evaluation of the electric pulp tester as an indicator of local anesthesia. Oper Dent. 1996;21:25–30. [PubMed] [Google Scholar]