Abstract
Buerger's disease, or thromboangiitis obliterans, is a nonatherosclerotic inflammatory disease affecting the small- and medium-sized arteries and veins of the extremities (arms, hands, legs, and feet). It is most common in the Orient, Southeast Asia, India, and the Middle East, and usually affects men aged between 20 and 40 years, although it is becoming more common in women. It is well established that most such patients smoke heavily and experience an improvement in symptoms following smoking cessation. Mesenteric involvement in Buerger's disease is extremely rare; however, we describe herein two cases of colon ischemia in patients who were previously diagnosed with lower-extremity Buerger's disease. In one case, the patient developed colonic obstruction, and surgical resection was performed. Histopathologic findings were compatible with the chronic stage of Buerger's disease. In the other case, angiography revealed abrupt occlusion of the inferior mesenteric artery with numerous collateral vessels, just like the corkscrew appearance found in the extremities. If patients with established Buerger's disease of the extremities complain of gastrointestinal symptoms, early interventional diagnosis should be performed to prevent intestinal obstruction and gangrene.
Keywords: Thromboangiitis obliterans, Mesenteric involvement, Colon ischemia
INTRODUCTION
Buerger's disease or thromboangiitis obliterans is characterized by occlusive segmental and often multiple inflammatory lesions of arteries and superficial veins with thrombosis and recanalization of the affected vessels.1 It is once considered a variant of atherosclerosis, and now recognized as a distinct clinical and pathologic entity.2 It typically occurs in young smokers, and its remissions and relapses are correlated to smoking.3
It mainly affected medium and small arteries in the extremities, and visceral and cerebral arteries were rarely affected.4 Involvement of large arteries such as mesenteric vessels is extremely rare.5-7 Herein, we encountered two cases of colon ischemia in the patients diagnosed as low extremity Buerger's disease previously. Both cases presented with abdominal pain and bloody diarrhea. In one case, the patient developed colonic obstruction during the hospital day and was operated on because of bowel obstruction. The postoperative histopathological diagnosis was mesenteric involvement of Buerger's disease. In the other case, inferior mesenteric artery was obstructed and there were numerous venous collaterals in inferior mesenteric angiography.
CASE REPORT
1. Case 1
A 65-year-old man was admitted to our emergency room complaining of a periumbilical and right lower quadrant pain for 2 months. Two months ago, he experienced right lower quadrant pain and bloody diarrhea and was treated with ischemic colitis in local clinic. This abdominal pain had worsened as he developed constipation and abdominal distention in the last 3 days. Abdominal examination revealed mild distention, diffuse pain after palpation, and increased bowel sounds. He was diagnosed as Buerger's disease at the age of 49 years when he developed migratory thrombophlebitis. After 5 years he developed ischemic manifestation and underwent amputation on the right lower limb up to the mid-thigh level. He smoked one pack of cigarettes daily since he was 20 years of age and quit smoking for the last 3 years.
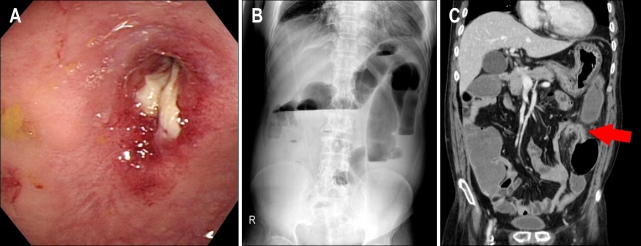
Laboratory values showed a white blood cell count of 12,600/L, hemoglobin of 11.3 g/dL, and a platelet count of 336,000/L. His liver function test showed aspartate transaminase of 33 IU/L, alanine transaminase of 26 IU/L, albumin of 3.5 g/dL and total bilirubin of 0.2 mg/dL. The other laboratory findings showed fast blood sugar of 99 mg/dL, blood urea nitrogen of 12.2 mg/dL, creatinine of 1.1 mg/dL, sodium of 139 mEq/L, and potassium of 3.8 mEq/L. Sigmoidoscopy showed marked luminal narrowing without any mass lesion (Fig. 1A). Computed tomography of the abdomen showed marked intestinal distension with segmental bowel wall thickening and pericolic hazziness in sigmoid colon (Fig. 1B). He underwent a laparotomy with bowel obstruction. Hartmann procedure (rectosigmoid resection with end colostomy and rectal stump) was performed. Histological examination of resected specimen revealed prominent vascularization of the media and infiltration of inflammatory cells with intact normal architecture (Fig. 2). After 6 months, successful end to end anastomosis was performed. Now, he stops smoking cigarette and has no further disease progression.
Fig. 1.
(A) Sigmoidoscopy reveales marked luminal narrowing without a mass lesion in the sigmoid colon. (B) Plain X-ray of the abdomen showing several dilated loops of the large bowel and multiple air-fluid levels. (C) Computed tomography revealing segmental luminal narrowing (red arrow) of the redundant sigmoid colon with a markedly distended proximal colon.
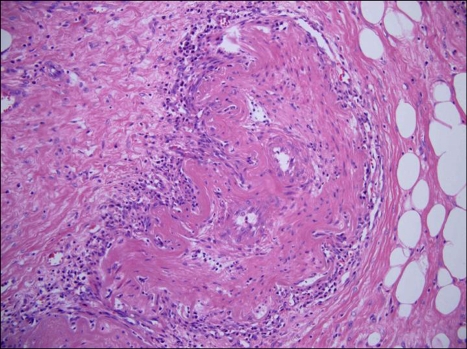
Fig. 2.
Histopathology of a surgical specimen, showing chronic-stage Buerger's disease. Focal lymphoproliferative cell infiltration and a recanalized thrombus are noted. The architecture of the vascular wall is well preserved (H&E stain, ×100.)
2. Case 2
A 39-year-old man was admitted to our emergency room complaining of a right lower quadrant pain and bloody stool for 5 days. He intermittently experienced abdominal pain for several months. Abdominal examination revealed diffuse pain after palpation, and decreased bowel sounds. He was diagnosed as Buerger's disease at the age of 34 years when he developed a gangrene formation in the right toe. Extremity angiography showed that right anterior, and posterior tibial, and popliteal artery were occluded with corkscrew appearance of collateral vessels which supplied plantar arch (Fig. 3). He underwent amputation on the right toe. He smoked one pack of cigarettes daily since he was 18 years of age and continued smoking.
Fig. 3.
Angiography of the lower extremities. The right anterior and posterior tibial arteries are occluded, the collateral vessels that supply the plantar arch have a corkscrew appearance.
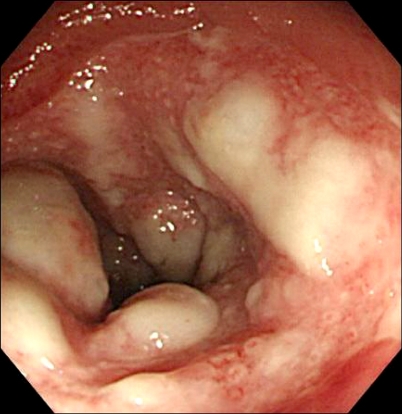
Laboratory values showed a white blood cell count of 9,280/L, hemoglobin of 12.3 g/dL, and a platelet count of 203,000/L. His liver function test showed aspartate transaminase of 41 IU/L, alanine transaminase of 38 IU/L, albumin of 3.8 g/dL and total bilirubin of 0.8 mg/dL. The other laboratory findings showed fast blood sugar of 85 mg/dL, blood urea nitrogen of 14.0 mg/dL, creatinine of 1.2 mg/dL, sodium of 140 mEq/L, and potassium of 3.8 mEq/L. Emergency sigmoidoscopy showed circumferential ulceration and hard coated exudates with mucosal edema, segmental involved and clear distinction between normal and lesion in the proximal sigmoid colon (Fig. 4). In computed tomography of the abdomen, we could not trace the inferior mesenteric artery. We performed a mesenteric angiography and it revealed abrupt occlusion of inferior mesenteric artery and numerous collaterals without evidence of atherosclerosis (Fig. 5). Conservative treatment of the colonic ischemia was successful, and a low residual diet was introduced without further complication. Now, he quits smoking and is in good condition at outpatient clinic.
Fig. 4.
Sigmoidoscopic findings. Circumferential ulceration with a hard-coated exudate is observed in the sigmoid colon that is segmental and denuded the affected mucosa.
Fig. 5.
Mesenteric angiography. The inferior mesenteric artery is completely occluded. The left colic artery is opacified through to the marginal artery of the middle colic artery.
DISCUSSION
Most of the patients with Buerger's disease are young male who are under 40 years old, and they are heavy cigarette smokers.8 However, a higher percentage of women and people over the age of 50 have been recognized to have this disease.9 The main symptom is pain in the affected areas. It is induced by insufficient blood flow during exercise. There is a progressive decrease in the blood flow to the affected areas that results in weak or undetectable pulse. The lack of blood flow can lead to gangrene. Most patients are heavy smokers, but some cases occur in patients who are smokeless.10 Smoking seems to be a synergistic factor rather than the cause of the disease. Diagnosis is usually made from the clinical symptoms. The traditional diagnosis of Buerger's disease is based on 5 criteria (smoking history, onset before the age of 50 years, infrapopliteal arterial occlusive disease, either upper limb involvement or phlebitis migrans, and absence of atherosclerotic risk factors other than smoking). As there is no specific laboratory test to aid in the diagnosis, clinical diagnosis should be made only when all these 5 criteria have been fulfilled. It is also clinically and pathologically distinguishable from atherosclerosis, endocarditis, severe Raynaud's phenomenon associated with connective tissue disorders and clotting disorders of the blood.11 In our report, we ascertained the previous diagnosis of these patients as Buerger's disease. It was supported by the patient's age, sex, the smoking history, angiographic findings, histopathologic examination and exclusion of other disease.
Biopsy and tissue sample are rarely required to establish the diagnosis. However, in a few cases with unusual onset of the disease, typical findings of pathology would be needed.12 In acute phase, there is acute inflammation involving all layers of the vessel wall in association with occlusive cellular thrombosis. In the subacute phase, there is progressive organization of the occlusive thrombus in the arteries and veins, and the chronic phase is characterized by complete organization of the occlusive thrombus with extensive recanalization, prominent vascularization of the media and adventitial and perivascular fibrosis. In all three stages, the normal architecture of the vessel wall including the internal elastic lamina remains intact and these findings distinguish from atherosclerosis and other systemic vasculitis.13,14 In the first case, histopathological examination revealed prominent vascularization of the media and inflammatory cell infiltration without fibrinoid necrosis and other evidence of atherosclerosis. Intact normal architecture was maintained. These histological features were compatible of chronic stage of Buerger's disease. We also differentiated other conditions by checking autoimmune disease and anticardiolipin antibodies.
Extensive arterial occlusion accompanied by the development of corkscrew collateral vessels is characteristic angiographic finding, but not pathognomonic. The disease is confined most often to the distal circulation and is almost always infra-popliteal in the lower extremities and distal to the brachial artery in the upper extremities. It may be seen in patients with connective tissue disease such as lupus, mixed connective tissue disease and scleroderma.5,15,16 In our case, there were no evidence of atherosclerosis, aneurysm or other source of proximal emboli in angiographic findings. Mesenteric involvement of Buerger's disease is extremely rare; therefore findings of mesenteric angiography are not established yet. In previous report, selective superior mesenteric artery angiogram revealed the corkscrew collaterals in addition to tapering of arterial segments in the intestinal arterial circulation that would be standard criteria for establishing the chronic angiographic course of Buerger's disease.17 In another report, mesenteric arteriography might appear normal or reveal no specific features which were always similar to those of peripheral Buerger's disease, but it can be useful to rule out other more common vascular disorders.7 In our case, we showed typical findings of Buerger's disease in previous angiography of low extremity and also the obstruction of IMA and numerous collateral vessels without atherosclerotic evidence in mesenteric angiography. These features were in favor of diagnosis as the mesenteric involvement of Buerger's disease. Further study on the standard criteria of mesenteric angiography in Buerger's disease would be needed.
Gastrointestinal symptom in Buerger's disease has rarely been reported, representing about 2% in the previous study result.12 Until now, twenty nine case reports were published in the world.6,12,18,19 It may occur at any time during the course of the disease, but mostly it happens years after the onset of the disease.6,16 However, most reported cases had significant peripheral vascular manifestations before developing mesenteric involvement. The occurrence of female was in only three cases (10.3%, 3/29). The gastric, colonic, celiac, and mesenteric arteries were affected, seeming to have a preference for branches smaller than the main stem. The small bowel was the most frequently involved site of Buerger's disease. Especially like our case, colonic involvement of Buerger's disease was extremely rare and six cases (20.7%, 6/29) were reported. Diagnostic or emergency laparotomy was performed in most cases and preoperative motality was 30% despite emergency surgery.6 In only three cases reported (10.3%, 3/29), conservative treatment was successful.
In general, it is known that the gastrointestinal involvement of Buerger's disease is difficult in early diagnosis and has poor prognosis. If the patients with established or suspicious clinical manifestation of extremity Buerger's disease complain of gastrointestinal symptoms, early interventional diagnosis is recommended for the prevention of intestinal obstruction and gangrene formation.
References
- 1.Olin JW. Thromboangiitis obliterans (Buerger's disease) N Engl J Med. 2000;343:864–869. doi: 10.1056/NEJM200009213431207. [DOI] [PubMed] [Google Scholar]
- 2.Adar R, Papa MZ, Schneiderman J. Thromboangiitis obliterans: an old disease in need of a new look. Int J Cardiol. 2000;75(Suppl 1):S167–S170. doi: 10.1016/s0167-5273(00)00185-6. [DOI] [PubMed] [Google Scholar]
- 3.Papa MZ, Adar R. A critical look at thromboangiitis obliterans (Buerger's disease) Perspect Vasc Surg. 1992;5:1–21. [Google Scholar]
- 4.Kempczinski RF, Clark SM, Blebea J, Koelliker DD, Fenoglio-Preiser C. Intestinal ischemia secondary to thromboangiitis obliterans. Ann Vasc Surg. 1993;7:354–358. doi: 10.1007/BF02002889. [DOI] [PubMed] [Google Scholar]
- 5.Hassoun Z, Lacrosse M, De Ronde T. Intestinal involvement in Buerger's disease. J Clin Gastroenterol. 2001;32:85–89. doi: 10.1097/00004836-200101000-00020. [DOI] [PubMed] [Google Scholar]
- 6.Kobayashi M, Kurose K, Kobata T, Hida K, Sakamoto S, Matsubara J. Ischemic intestinal involvement in a patient with Buerger disease: case report and literature review. J Vasc Surg. 2003;38:170–174. doi: 10.1016/s0741-5214(02)75469-4. [DOI] [PubMed] [Google Scholar]
- 7.Sauvaget F, Debray M, Herve de Sigalony JP, et al. Colonic ischemia reveals thromboangiitis obliterans (Buerger's disease) Gastroenterology. 1996;110:900–903. doi: 10.1053/gast.1996.v110.pm8608901. [DOI] [PubMed] [Google Scholar]
- 8.Lazarides MK, Georgiadis GS, Papas TT, Nikolopoulos ES. Diagnostic criteria and treatment of Buerger's disease: a review. Int J Low Extrem Wounds. 2006;5:89–95. doi: 10.1177/1534734606288817. [DOI] [PubMed] [Google Scholar]
- 9.Stvrtinova V, Ambrozy E, Stvrtina S, Lesny P. 90 years of Buerger's disease-what has changed? Bratisl Lek Listy. 1999;100:123–128. [PubMed] [Google Scholar]
- 10.Lie JT. Thromboangiitis obliterans (Buerger's disease) and smokeless tobacco. Arthritis Rheum. 1988;31:812–813. doi: 10.1002/art.1780310620. [DOI] [PubMed] [Google Scholar]
- 11.Shionoya S. Diagnostic criteria of Buerger's disease. Int J Cardiol. 1998;66(Suppl 1):S243–S245. doi: 10.1016/s0167-5273(98)00175-2. [DOI] [PubMed] [Google Scholar]
- 12.Magalhaes Ede P, Trevisan M, Mochizuki M, Sachetto Z, Samara AM, Fernandes SR. Intestinal ischemia as a single manifestation of thromboangiitis obliterans: a case report. Angiology. 2005;56:789–792. doi: 10.1177/000331970505600619. [DOI] [PubMed] [Google Scholar]
- 13.Kurata A, Franke FE, Machinami R, Schulz A. Thromboangiitis obliterans: classic and new morphological features. Virchows Arch. 2000;436:59–67. doi: 10.1007/pl00008199. [DOI] [PubMed] [Google Scholar]
- 14.Kobayashi M, Nishikimi N, Komori K. Current pathological and clinical aspects of Buerger's disease in Japan. Ann Vasc Surg. 2006;20:148–156. doi: 10.1007/s10016-005-9436-2. [DOI] [PubMed] [Google Scholar]
- 15.Raat H, Stockx L, Broeckaert L, et al. Mesenteric involvement of thromboangiitis obliterans (Buerger's disease) in a woman. J Belge Radiol. 1993;76:245–246. [PubMed] [Google Scholar]
- 16.Krupski WC, Selzman CH, Whitehill TA. Unusual causes of mesenteric ischemia. Surg Clin North Am. 1997;77:471–502. doi: 10.1016/s0039-6109(05)70562-4. [DOI] [PubMed] [Google Scholar]
- 17.Michail PO, Filis KA, Delladetsima JK, Koronarchis DN, Bastounis EA. Thromboangiitis obliterans (Buerger's disease) in visceral vessels confirmed by angiographic and histological findings. Eur J Vasc Endovasc Surg. 1998;16:445–448. doi: 10.1016/s1078-5884(98)80016-6. [DOI] [PubMed] [Google Scholar]
- 18.Cordobès Gual J, Riera Vázquez R, Merino Mairal O, Manuel-Rimbau Muñoz E, Lozano Vilardell P, Company Campins M. Buerger's disease with intestinal ischemic involvement. An Med Interna. 2005;22:235–237. doi: 10.4321/s0212-71992005000500008. [DOI] [PubMed] [Google Scholar]
- 19.Cho YP, Kwon YM, Kwon TW, Kim GE. Mesenteric Buerger's disease. Ann Vasc Surg. 2003;17:221–223. doi: 10.1007/s10016-001-0220-7. [DOI] [PubMed] [Google Scholar]