ABSTRACT
The treatment of hand and upper-extremity injuries is complex. The treatment goals are to restore maximal hand function and, if possible, preinjury form. Several complications are frequently encountered while treating hand and upper-extremity injuries. Complications such as edema, direct structural destruction, and nerve palsies are the result of the inflicting injury. Skin graft contraction, fascial adhesions causing restricted tendon motion, and diminution of muscle function with time during staged reconstructions are treatment-related complications. The nature of these complications as well as means for their prevention and treatment are reviewed.
Keywords: Upper-extremity trauma, avoiding unfavorable results
The human hand is a specialized organ composed of a complex arrangement of bones, muscles, tendons, and skin permitting integrated and coordinated movements. The basic hand function comprises a thumb ray opposing with the adjacent functional fingers to achieve a prehensile task. The fundamental goal of mutilated hand reconstruction is to achieve a basic hand function, or better yet, a restoration of the hand as closely as possible to its pretraumatized state in both function and form. However, unfavorable results of the reconstructive process are not uncommon. Unfavorable results even after surgical efforts to reconstruct the hand can be trauma-related or surgery-related.
TRAUMA-RELATED UNFAVORABLE RESULTS
Edema Control
In trauma-related injuries, the initial management plays an important and essential role in the ultimate outcome. In the initial 2 to 3 days, the inflammatory cascade sets in, with histamine and cytokine release, capillary leakage, and resultant edema in the area of injury as well as in the adjacent noninjured areas. Progressively, the migration of fibroblasts and other inflammatory cells, as well as the extravasation of plasma proteins such as fibrin, albumin, and globulin infiltrate the interstitial tissue, synovial sheath, and joint space, turning the intra-articular inflammatory fluid volume and hematoma into subsequent cemented fibrosis of the joint space. The edematous fluid fills up the joint capsule, and as the process ensues, the synovial space becomes distended, positioning the collateral ligaments in an undesirable position. As a result, joint motion is restricted. Additionally, intrinsic muscles such as thenar muscles, dorsal and volar interosseous muscles, and lumbrical muscles become shortened and contracted. The edematous hand typically presents with (1) loss of normal skin wrinkles, (2) tautness of dorsal finger joint creases, (3) loss of metacarpal head definition, and (4) obscurity of digital extensor tendon outline over the dorsum of the hand. Tendon adhesion also occurs as a consequence of being bathed within the protein-rich edematous fluid leading to fibrosis (Fig. 1).
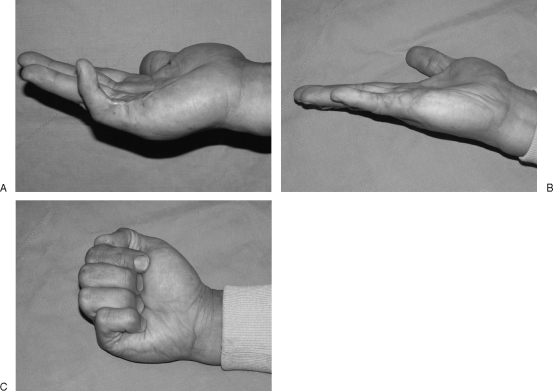
Figure 1.
Edematous hand presents with (1) loss of normal skin wrinkles, (2) tautness of dorsal finger joint creases, (3) loss of metacarpal head definitions, and (4) obscurity of digital extensor tendon outline.
Under the infliction of the edematous process, the hand presents as a negative hand, consisting of thumb adduction, proximal interphalangeal (PIP) joint flexion, metacarpophalangeal (MCP) joint extension, and wrist flexion (Fig. 2).
Figure 2.
Negative hand consists of thumb abduction, PIP joint flexion, MCP joint extension, and wrist flexion.
In cases with a negative hand manifestation, the patient often requires surgical intervention for contracture release.
To prevent and minimize edema formation in the posttraumatic hand, compressive treatments and splinting of the joints in the safe position are essential immediately after trauma, with elastic bandage (Coban or Jobst) and limb elevation, and avoidance of excessive salt intake highly recommended. Prevention of contracture secondary to a prolonged inflammatory and edematous state is the first priority in the management of hand trauma. Once contracture is established and the negative hand develops, multiple and often complex surgical procedures may be needed for functional improvement. The patient may be initially referred to a hand therapist. If the condition is not reversed with an aggressive rehabilitation program, surgical correction is then indicated.
PIP JOINT
A stiff PIP joint causes more disability than a stiff wrist or distal interphalangeal (DIP) joint and can be very difficult to restore to full range of motion once contracture is established. A traumatized hand tends to have a resting position in MCP joint extension and PIP joint flexion. With time, the PIP joint will be stiff with a flexion contracture deformity. In contrast with the collapsible volar plate of the MP joint, the PIP joint is composed of a rigid cartilaginous volar plate that glides with joint motion. This armor-like plate is fixed at its proximal border by checkrein ligaments, which merge with volar ligamentous structures such as the flexor sheath, Cleland and Grayson ligaments, and the oblique retinacular ligaments of Landsmeer. When the PIP joint is stiffened by fibrosis in the flexed position, the volar plate will slide proximally and be fixed by the checkrein ligament with resultant PIP joint flexion contracture. The neighboring flexor tendons in zone II will have formed adhesions because of tissue edema, especially after an episode of tendon injury or phalangeal fracture. The skin will have contracted and lost its elasticity for passive PIP joint extension after the PIP joint flexion contracture. This situation is worsened by scar contracture at the skin level after injury to the integument.
Some surgeons favor PIP joint contracture release through the midlateral approach, which is reported to have less soft tissue violation and less pain.1 The trauma patient with PIP joint contracture often has involvement of more than one tissue level, such as skin, tendon, and volar plate. As such, the volar approach is our preferred approach. First, it affords good access and improved visualization of all contractured structures. Second, its excellent exposure allows treatment of the affected structures concurrently: (1) Z-plasty for skin tension release, (2) flexor tendinolysis and/or removal of the contractured flexor digitorum superficialis (FDS), (3) checkrein ligament release for volar plate contracture, or (4) volar plate for interpositional arthroplasty for PIP joint degenerative change. Lastly, the volar approach can also permit synchronous neurolysis and/or nerve grafting if needed (Fig. 3).
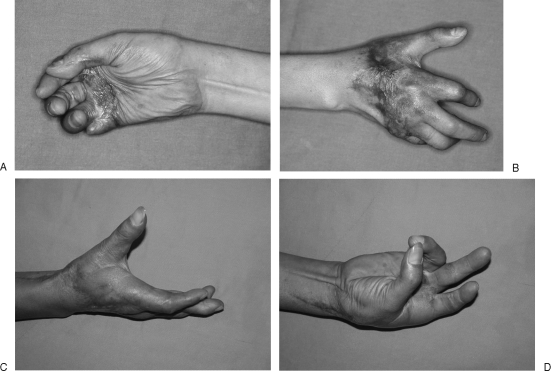
Figure 3.
(A) Little finger posttraumatic flexion contracture with extension lag. (B) Full active extension after skin Z-plasty, volar plate released by checkrein ligament cutoff, and lysis of flexors. (C) Full active flexion postoperatively.
Prolonged PIP joint contracture may also cause loosening of the extensor lateral bands and central slip. As a result, there is an extension lag after PIP joint release. The release will yield a better outcome if the volar skin is adequate or when the soft tissue contracture can be adequately addressed with Z-plasty lengthening.
MCP JOINT
The negative hand will have MCP joint extension. Due to the unique cam shape of the metacarpal head, the collateral ligament of MCP joint is tight in flexion and loose in extension. According to the normal anatomic configuration, when the intracapsular volume is increased such as from edema, the progressive joint space distension will drive the MCP joint into an extended position. The loose collateral ligament in the edematous, extended MCP joint configuration eventually shortens. In addition, the extravasated fluid in the synovial space can accumulate and cause more fibrosis if left unresolved or untreated over time. With this knowledge, it is prudent to keep the edematous hand in a splinted safe-position during the acute treatment stage, with the MCP joint in flexion, and the PIP and DIP joints in extension to prevent the negative hand formation. If MCP joint extension contracture occurs, the joint will require a dorsal capsulectomy and a collateral ligament releasing procedure to allow MCP joint flexion, with optional extensor tendon adhesion release.
In the resting position or particularly with a swollen hand, the thumb ray has a tendency toward an adduction posture. With this arrangement, the intrinsic thenar muscles and overlying fascia in the first web space shorten and contract over time. The contractured thumb ray prevents the thumb from circumduction—a crucial function of the hand—and the thumb cannot accomplish adequate opposition to the adjacent fingers. The natural opposition of the thumb to the ring or little finger requires a minimal intermetacarpal angle of 60 degrees between the 1st and 2nd metacarpals. If opposition is inadequate, a systematic analysis of the intermetacarpal angle may suggest an appropriate treatment solution. When the external thenar muscles (abductor pollicis brevis, flexor pollicis brevis) are functioning, and the maximum intermetacarpal angle is more than 60 degrees, the oppositional insufficiency is not a direct deficit or dysfunction of the radial aspect of the hand. Instead, it may be due to ulnar nerve palsy with hypothenar muscle dysfunction, resulting in MCP joint flexion deficit or failure of radial rotation or supination of the 4th and 5th metacarpal rays. Rehabilitation or tendon transfer for ulnar-innervated MCP joint flexion is recommended. When the maximum intermetacarpal angle is between 30 and 60 degrees, some form of Z-plasty with release of the internal thenar muscles and fascia is used to address the contracture. When the maximum intermetacarpal angle is less than 30 degrees, the contracture requires a more aggressive intrinsic thenar muscle release, and the web space defect can be resurfaced with either a rotational flap, a pedicled regional flap, or a free flap. The ipsilateral lateral arm flap is the author's preferred choice for the required width and length of the defect on the first web space. Our other soft tissue alternatives include a free groin flap, an anterolateral thigh flap, or a medial sural artery perforator flap (Fig. 4).
Figure 4.
(A) A posttraumatic palmar contracture with flexion insufficiency by skin graft. (B) First web space contracture and angle of separation less than 30 degrees. (C) Free lateral arm flap for first web space release. (D) Good opposition after contracture release.
The splinted safe position of the hand coupled with aggressive edema control can prevent or at least minimize the negative hand deformity. Programmed rehabilitation can achieve fingers flexion after splint removal. However, extensor intrinsic tightness can occur if the intrinsic muscle length was not maintained in the safe position in the acute stage or if there is intrinsic muscle length shortening secondary to a fracture process with adhesion formation. Clinically, intrinsic tightness presents with an inability of the PIP and DIP joints to flex completely in MPJ extension. If the interosseous muscles are fibrotic and tight but with some remnant contractility, a subperiosteal interosseous muscle release off the metacarpals may improve the intrinsic tightness.
Structural Destruction
It is not uncommon that the traumatized hand involves several components, including bone, musculotendinous unit, nerve, and skin. A strong bony platform is a prerequisite for subsequent functional reconstruction of the upper extremity. The musculotendinous unit must have a fixed bone distance for its origin and insertion to maintain its length. Additionally, the bone foundation has to be stable for the musculotendinous unit to carry out its vectorial contractility across the joints. Disruption of this bony framework through fractures or frank bone loss leads to significant functional deficits on many levels. Whatever the bony deficit, a stable osteosynthesis through various fixation methods and/or bone grafting (vascularized as well as nonvascularized) can accomplish successful bony union in appropriate cases. For smaller defects such as a scaphoid nonunion or a single metacarpal defect, the dorsal distal radius can be used as a pedicled bone transfer.2 For segmental ulnar or radius defects, extensive or multiple metacarpal defects, immediate reconstruction with a free vascularized bone transfer is of paramount importance for maintaining length. Our choices for vascularized bone transfer to the upper extremity include a free fibula flap as well as an iliac crest bone flap.3
A sophisticated strategy for soft tissue envelope and tendon repair will maximize the functional restoration. In milder cases, most of the disrupted tendons can be repaired primarily or with a small tendon graft. Subsequently, an aggressive rehabilitation program combined with a cooperative patient can achieve a satisfactory functional outcome. In more severe cases where there are multiple tendon and muscle avulsions, primary tendon or muscle repair will not be feasible, but if left alone for delayed or secondary repair, the disrupted muscle will shorten. An acute open traumatic wound allows for the most exposure of the injured, involved structures. This scenario presents with the best time and opportunity to evaluate the amount of damage present.
Regardless of the injury location (proximally based or distally based avulsion), it is possible that some residual or disrupted musculotendinous unit can be rearranged to have a synergistic tendon transfer to restore the functional deficit. If not, the tendon defect can be reconstructed with a normal expendable tendon from the remaining flexor or extensor group in the forearm. When there is extensive soft tissue defect requiring a free flap, a free functioning muscle transfer (such as the gracilis myocutaneous flap) can be another option for providing a simultaneous skin component for soft tissue coverage and muscle for functional restoration. Theoretically, a tendon transfer can afford a more reliable and predictable result than a free functioning muscle transfer, with a much shorter convalescence period. The tendon transfer strategy should be given a higher priority in the treatment option list than the free muscle transfer (Fig. 5).
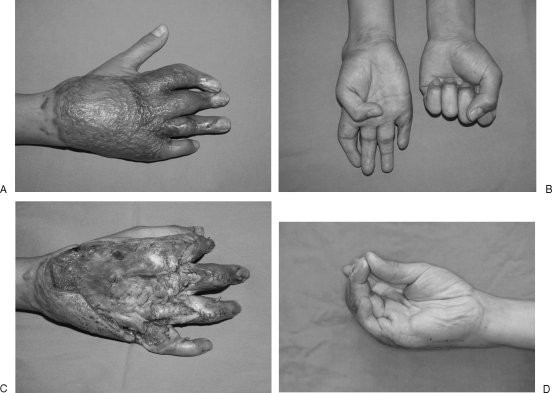
Figure 5.
(A) Left dorsal wrist crush injury with soft tissue defect and multiple extensor defect. (B) After simultaneous free groin flap and tendon transfer for thumb, and extensor carpi radialis brevis repair. (C) Good flexion and extension.
Distal Nerve Palsy
Nerve injuries are not uncommon in upper-extremity trauma. In distal median and ulnar nerve injuries, sensory restoration should be among the initial priorities. However, any motor function deficit will be observed until a clear determination of the deficit is made. When there is segmental median or ulnar nerve defect requiring nerve graft, or direct damage to the intrinsic muscles, the hand will present with a temporal course of unpredictable, evolving intrinsic functional deficit. Immediate tendon transfer will shorten the disability time and provide early functional reconstruction. In the case of external thenar muscle avulsion or unrepairable motor branch injury of the median nerve, an immediate tendon transfer of flexor digitorum superficialis (FDS), extensor indicis proprius (EIP), or palmaris longus (PL) transfer to APB or thumb MPJ can achieve opposition replacement.4 In addition, such an opponensplasty can function as an internal splinting to prevent the first web space contracture, especially in the cases of associated intrinsic thenar muscle damage.
Usually the disrupted ulnar nerve has poor motor function recovery after repair, in comparison with the repaired median nerve. When the ulnar nerve undergoes nerve grafting or when there is interosseous muscle destruction, a concurrent tendon transfer is preferred. The extensor carpi radialis longus (ECRL) tendon can be used with an intercalary tendon graft for the reconstruction of the avulsed lateral bands.
The immediate tendon transfer providing a functional reconstruction in the acute stage with either a disrupted donor tendon or a healthy donor tendon can be controversial in regard to the timing and indication. However, in our experience, it can provide not only internal splinting support but also a functional support augmenting for the unpredictable neurapraxia damage.
In scenarios where the damage involves nerve injury at or above the elbow level, the functional reconstruction of the forearm will be delayed until the full extent of nerve regeneration is determined over time. The one exception is the consideration of the optional Brand intrinsic tendon transfer for palsy support in the acute setting, as mentioned earlier.
SURGERY-RELATED UNFAVORABLE RESULTS
Skin Graft or Skin-Grafted Muscle Flap
Early wound coverage is always a cornerstone principle of posttraumatic defect management for the preservation of vital structures and the minimization of wound infection. An initial and radical debridement followed by early wound coverage is the most important management for lower-extremity open fracture salvage. In contrast, the upper extremity has relatively higher functional demands. As a result, the radical debridement should be tempered with preservation of essential vital structures such as disrupted tendons and nerve stumps to allow secondary reconstruction.
One option for soft tissue coverage is skin grafting. Skin grafts can take over paratenon, granulation tissue, or muscle to accomplish their purpose for wound coverage. But the recipient site may have the possibility of fibrosis, and it may present with flexor tendon adhesion or extensor extrinsic tightness. If the skin graft is placed over the repaired tendon, the healing of that tendon is doomed to failure, and the poor soft tissue coverage makes tendon adhesions difficult to treat with rehabilitation and secondary surgical intervention. In addition, the skin graft is prone to scar contracture. The grafted skin is less supple and elastic and will likely restrict joint movement. It is not uncommon that the mutilated upper limb will require secondary reconstructive procedures on the skin-grafted area, necessitating the replacement of grafted skin with a more flexible and elastic skin envelope (Fig. 6).
Figure 6.
(A) Distal forearm contractured skin graft with restriction of flexion and extension. (B) Tenolysis after removal of skin graft. (C) Hand extension after resurfacing with free groin flap. (D) Good opposition after resurfacing.
Skin-grafted fascial flaps, such as temporoparietal fascial flap, and skin-grafted muscle flaps are often reported to provide a flexible, expandable soft tissue coverage for underlying tendon gliding. However, these flaps may experience soft tissue contracture at the recipient site. Contracture of the skin graft or skin-grafted flap will require repeated release surgeries on the recipient site, but the absent subdermal plexus may jeopardize the graft or flap for elevation and tendon healing, leading to a newly created problem of tendon exposure at a nonhealing site (Fig. 7).
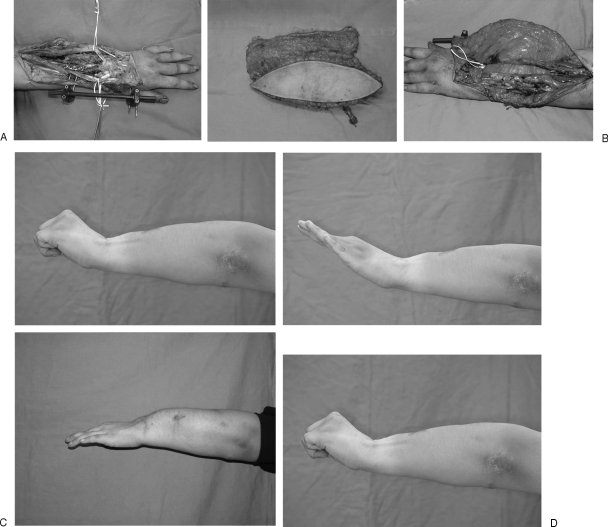
Figure 7.
(A) Dorsal hand defect after skin graft on latissimus dorsi muscle flap. (B) Restriction of flexion, and MPJ stiff. (C) MPJ interposition arthroplasty. (D) Good opposition after ALT flap resurfacing.
As a result, a supple and expandable skin flap is superior to the other options for the advantages of a reliable skin paddle for elevation to execute various tendon, bone, or joint procedures, as well as flap revision (i.e., local flap or Z-plasty). The anterolateral thigh (ALT) flap possesses numerous advantages including a wide skin paddle, composite tissue, thin or ultrathin flap, long and sizable pedicle, and less donor-site morbidity For these reasons, the ALT flap is becoming the workhorse for most defect reconstructions. Free skin flaps have a unique advantage in that they can be tailored to meet the needs of the defect, matching texture, color, bulk, and thickness as closely as possible to the tissue that was lost.
The skin flaps can be harvested from local sources or from more distant areas. Local flap coverage is indicated for small defect and is an easy method for neighboring defect reconstruction. Keeping in mind that the traumatized upper limb might require secondary revision surgery, with additional work done in adjacent noninjured areas, such as exploration for and execution of tendon transfer, extensive dissection with local flaps in the acute stage (e.g., reversed posterior interosseous flap) with skin grafting on the donor site (e.g., forearm flap) can result in forearm tissue fibrosis and tendon adhesion. If local reversed arterial flaps such as the posterior interosseus artery and radial forearm flaps are entertained for hand defect coverage, this must be a carefully thought-out decision because the arterial network at the wrist area is sometimes involved in the primary trauma, and the full extent of the vascular injury may be underappreciated in the acute setting. For that reason, use of local flaps should be highly selective to prevent tissue violation and fibrosis restricting secondary exploration and reconstruction.
Gliding Fascia
Both the flexor and extensor tendons in the forearm have a close relationship in their alignment with the bony structures. Forearm fractures have a higher incidence of tendon injuries. On the other hand, the mutilating soft tissue and tendon injuries may have accompanying forearm fractures. The callous formation of the bony component of replants is often coupled with adhesion to the overlying tendon with resultant tendon excursion restriction.
Skin graft and muscle flap coverage of the exposed tendon will have the problem of direct adhesion to the underlying tendons. Fascial flaps have been reported to provide an effective gliding plane immediately superficial to the tendon, which is beneficial for tendon excursion. However, the adhesion in this situation is more likely to be present on the deep contact surface between the tendon and the bone, especially in the cases of comminuted fractures. This is why some cases of fascial or fasciocutaneous flaps require tenolysis to release adhesions between the fracture site and with the implant fixator. If a fascial flap is considered, the required tendon gliding is best maintained or restored by also placing some of the fascial coverage deep to the tendon between the tendon-bone interface to separate the tendons from the fractured site. Additionally, it is not uncommon that the open fracture or comminuted fracture will require a secondary bone graft because of bone nonunion. The vascularized fascial separation of the tendon component from the fracture site will greatly facilitate secondary bone graft placement without tendon violation and subsequent sequelae of adhesion requiring tenolysis. A good option to consider is the ALT flap, which can be harvested with a wide and long vascularized fascia lata extension. The fascia lata can be placed above or beneath the tendon or completely wrapped around the repaired tendon (Fig. 8).
Figure 8.
(A) Distal forearm open fracture with soft tissue defect. (B) ALT flap with fascia lata for separation of the tendon from the fracture site. (C) Finger extension 3 months postoperatively. (D) After one lysis and debulking, good wrist and fingers extension.
Staged Reconstruction
Disrupted muscles contract progressively, with eventual loss of its tensile strength and length, negating its availability and usefulness as a potential musculo-tendon transfer unit in secondary stages for functional restoration. If the muscle disruption is much more proximal to the musculotendinous junction, the innervating motor nerve may be involved, and the remained muscle belly is too short to have adequate muscle power. In this case, the functional deficit of the involved muscle requires other suitable muscle units for functional substitution. If the muscle disruption is distal to the musculotendinous junction, the muscle can be either repaired directly or with a tendon graft or be transferred for more important synergistic function restoration, such as disrupted ECRL transfer for ECRB (wrist extension), thumb extension (extensor pollicis longus; EPL), or MPJ extension (extensor digitorum communis; EDC).
Radical debridement and early flap coverage is beneficial for improved surgical results and for infection prophylaxis or control, and one-stage reconstruction is better than staged reconstruction with tendon graft or bone graft at a later stage. This approach is well accepted by most reconstructive surgeons.
In a one-stage “functional” reconstructive approach, the reconstruction is not simply for defect coverage, bone or tendon repair, but may also include tendon transfer for nerve palsy and tendon defect and functional muscle or myocutaneous transfer for composite functioning muscle and soft tissue defect with optional tendon transfer (e.g., opponensplasty). For example, because of thin skin coverage on the dorsal hand, the metacarpal crush injury may present with skin, metacarpal, and extensor tendon defects and possible accompanying interosseous muscle destruction. Multiple bony metacarpal defects as well as soft tissue coverage can be adequately addressed simultaneously with a free fibula osteocutaneous flap osteotomized into two or three struts (Fig. 9). The extensor tendon disruption should be repaired, and the missing or nonfunctional interossei can be reconstructed using splitted palmaris longus extension graft from the ECRL to the lateral bands (Brand method) to achieve PIP and DIP joint extension. In the case of forearm avulsion with loss of the flexor muscle group and median nerve damage, a one-stage strategy may include defect reconstruction with a gracilis functioning muscle flap for finger flexion, remnant flexor muscle utilization or uninjured extensor tendon transfer for thumb flexion, and opponensplasty for thumb ray opposition.
Figure 9.
(A) Third to fifth metacarpal bone defect involving MPJ. (B) Fibular flap for 3rd, 4th metacarpal defect reconstruction and bone graft for 5th MPJ defect. (C) Finger extension after MPJ fusion and bone reconstruction. (D) Good opposition.
To accomplish the goal of one-stage functional reconstruction, a free composite flap inclusive of different components can be custom-made to fulfill every defect in the recipient site. Our preferred options include the fibula, ALT, and forearm flaps. The fibular flap is a composite flap comprising bone and skin paddle. The ALT can be a chimeric flap inclusive of skin, muscle, bone, and nerve. A forearm venous flap with accompanying palmaris longus tendon can be used for finger extensor tendon defect reconstruction.
As the functional reconstruction has to immobilize the wrist and hand in one position and one position only—either flexion or extension—but not both after surgery, a one-stage reconstruction may not be an optimal approach in injuries simultaneously involving the flexor and extensor side. In addition, if the reconstruction requires multiple tendon transfers from both the flexor and the extensor groups even though the defect is on one side, such as the volar aspect, the surgeon has to prioritize the order of tendon harvest and choose from one of the two muscle groups but not both concurrently. Effective splinting in either the flexion or extensive position exclusively will be impossible with the concurrent transfer of both donor extensor and flexor tendon units. The reconstructive strategy should be adaptable enough to give consideration to a staged approach when necessary.
One-stage early reconstruction is preferable to shorten the disability time and to allow for earlier rehabilitation to have better recovery and improved outcomes. In some situations, staged reconstruction is inevitable. However, all upper-limb reconstructions should have a well-thought-out strategic road map consisting of an optimal plan A and a back-up plan B, or even a plan C, to achieve an effective functional restoration.
REFERENCES
- Brüser P, Poss T, Larkin G. Results of proximal interphalangeal joint release for flexion contractures: midlateral versus palmar incision. J Hand Surg [Am] 1999;24:288–294. doi: 10.1053/jhsu.1999.0288. [DOI] [PubMed] [Google Scholar]
- Sheetz K K, Bishop A T, Berger R A. The arterial blood supply of the distal radius and ulna and its potential use in vascularized pedicled bone grafts. J Hand Surg [Am] 1995;20:902–914. doi: 10.1016/S0363-5023(05)80136-4. [DOI] [PubMed] [Google Scholar]
- Lin C H, Wei F C, Rodriguez E D, Lin Y T, Chen C T. Functional reconstruction of traumatic composite metacarpal defects with fibular osteoseptocutaneous free flap. Plast Reconstr Surg. 2005;116:605–612. doi: 10.1097/01.prs.0000173554.46455.5a. [DOI] [PubMed] [Google Scholar]
- Lin C H, Wei F C. Immediate Camitz opponensplasty in acute thenar muscle injury. Ann Plast Surg. 2000;44:270–276. doi: 10.1097/00000637-200044030-00004. [DOI] [PubMed] [Google Scholar]