Abstract
Objectives
Hypothyroidism in utero leading to mental retardation is highly prevalent and recurrent in developing countries where iodine deficiency and thiocyanate overload are combined. So, to explore and identify human population's risks for developing iodine deficiency disorders and their endemicity in Western Cameroon, with the aim to prevent this deficiency and to fight again it, urinary iodine and thiocyanate levels were determined.
Methods
The district of Bamougoum in Western Cameroon was selected for closer study due to its geographic location predisposing for iodine deficiency disorders (IDD). A comprehensive sampling strategy included 24-h urine samples collected over three days from 120 school-aged children. Urinary iodine and thiocyanate levels were measured by colorimetric methods.
Results
Twenty one percent of boys between the ages 3 and 19 were classified as iodine deficient. The prevalence of thiocyanate overload in the same population was found to be 20%.
Conclusion
Presence of endemic iodine deficiency and excessive thiocyanate in the population indicates that the region is at risk of iodine deficiency disorder. A multifactorial approach that includes improvement of diet, increasing iodine and minimizing goitrogen substances intake, soil and crop improvement and an iodine supplementation program may help alleviate IDD in the affected area studied.
Keywords: human, iodine deficiency disorder, IDD, Cameroon, iodine, thiocyanate, food, urine
Running title: IDD in West Cameroon
Introduction
Several minerals and trace elements (iodine, iron, selenium, and zinc) are essential for normal thyroid hormone metabolism. Deficiencies of these minerals can impair thyroid function. Iodine is most commonly known for its effect on thyroid function. Production of thyroxin (T4) by the thyroid and later generation of its active metabolite triiodothyronine (T3) relies on iodine availability. Thus, low-levels of bioavailable iodine can cause low thyroxin levels. Goiter, a classic symptom of iodine deficiency is caused by an over-stimulation of the thyroid tissues by thyroid stimulating hormone (TSH) due to insufficient T3/T4 feedback inhibition.1
Low levels of thyroxin, especially during fetal development, cause damage collectively known as iodine deficiency disorders (IDD) such as mental retardation, brain damage, impaired physical development, spontaneous abortions, low birth weight, infant mortality, cretinism, dwarfism and endemic goiters.2, 3, 4 More than two billion people worldwide are at risk of developing IDD due to the inadequate dietary intake of iodine either from plant or animal sources.5, 6 The soils of the countries at high risk of IDD are often deficient in iodine. This leads to insufficient uptake of iodine by their food crops. Furthermore, they often lack access to iodine-rich sea foods, increasing the risk of IDD development.7
Iodine is not the only micronutrient that can impact thyroid function. Thiocyanate (SCN) is believed to be a goitrogenic compound. It is a competitive inhibitor of the human thyroid sodium/iodide symporter NIS.8, 9, 10 Thus, the adverse effects of thiocyanate overload are especially noticeable when iodine availability is low. Intake of goitrogenic substances causes an adaptive increase in T3's binding to brain nuclear receptors and in the activity of type II 5′-deiodinase, which generates T3 from T4. This altered function and availability of T3 is detrimental to the developing brain.11 Thiocyanate is also known to modulate activity of mammalian peroxidases although the biological impact of this mechanism is unknown.12 Cassava, grown and consumed widely in Africa, is a major source of thiocyanate. The digested cyanogenic glucosides of unprocessed cassava generate cyanides, which are metabolized to thiocyanate.11
Unfortunately, goiter is endemic in many of the distal inland regions of Cameroon. As such, the effects of IDD remain a drain on the economic and human potential of Cameroon. Estimates suggest that IDD afflicted children may forfeit 10–15 IQ points while the World Bank suggests that up to 5% of the world economic output is sacrificed due to micronutrient deficiency like iodine deficiency.13, 14, 15 In such a situation, it is crucial to assess the risk of developing IDD in children and youths of at least one of the distal inland regions of Cameroon using quantifiable indicators. Therefore, the present investigation was undertaken to explore the risk of IDD with the aim to prevent and to fight against them in Bamougoum, a mountain region of western Cameroon, by studying urinary iodine and thiocyanate excretion levels in children.
Methods
Study area
The study was conducted from August 2002 to September 2003 in Bamougoum, a large district comprised of 9 villages located on the leeward side of the mountain chains of western central Cameroon. The study was carried out after the informed consent of children's parents and approval by the University of Douala, Cameroon, for the use of human subjects.
Sample collection
Samples collections were undertaken especially at the period of August 2002, holiday's period in Cameroon, when all children are supposed to be at home. Selected subjects were visited in their homes by specially-trained nurseswho obtained subjects' demographic information by questionnaire. Dried bottle of two liters, decontaminated with concentrated nitric acid and rinsed with double distilled water, was given to the child the evening before. Under the supervision of his parent, each child was supposed to urinate into a bottle every time he needs to do. 24 h after, bottle with urine was collected, mixed and only 10 mL of that were aliquoted in small sterilized bottle (10 mL) contained HCl (0.5% V/V), to prevent oxidation16. The same operation has been done during three consecutives days (i.e. Monday, Tuesday and Wednesday) and Urine samples of 120 children (58 boys and 62 girls) aged 3 to 19 years were collected by group of 20 children each three days. All samples were stored at room temperature overnight until an analysis was performed in the laboratory the next day. Although the study did not directly attempt to follow the diet and provenance of foodstuffs consumed by youth subjects, iodine levels in common foodstuffs can still be linked to subjects' urinary iodine.
Quantification of thiocyanate and iodine
The iodine in urine samples is released after mineralization at 600°C in an alkaline medium. Released iodine catalyzes the reduction of yellow-orange ceric ions (Ce4+) to colorless cerous ions by arsenic ions (As3+).16, 17, 18 Potassium iodate (KIO3; 5mg/dL) was used as standard solution whereas distilled H2O was used as blank sample. Thiocyanate contained in urine was quantified colorimetrically following the method described by Ngogang.16 In this method, thiocyanate is allowed to react with ferric ions in a neutral or slightly alkaline medium, yielding a red color. Serial dilutions of ammonium thiocyanate (NH4SCN; 50, 100, 150, 200 mM) were used as standard curves whereas distilled H2O was used as blank sample.
Statistical analysis
The iodine status was based on the median values obtained from urinary iodine excretion. The data were analyzed using SigmaStat (version 2.03) statistical software, student's T tests and ANOVA 2 to compare medians and to identify significant differences in iodine contents between values and groups. Urinary excretion and the estimated iodine deficient (I<50µg/L) proportion of the population were calculated in accordance with the World Health Organization's (WHO) recommendations.19 Furthermore, median I/SCN ratios and estimated thiocyanate overloaded (I/SCN<3µg/mg) proportions were also calculated.
Results
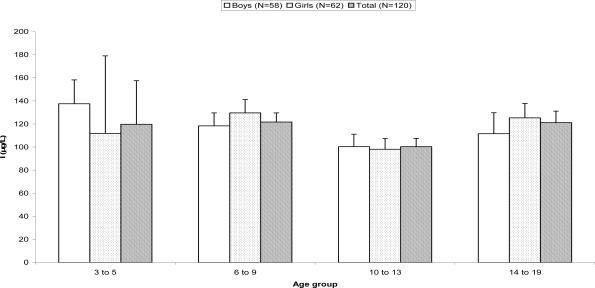
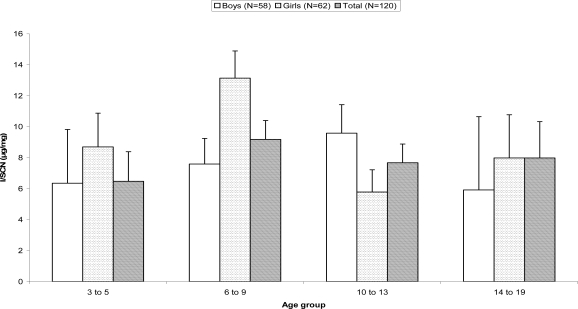
The median urinary iodine excretion of the studied population is shown in Figure 1. Median iodine excretions of all groupings were approximately 100µg/L. Similarly, Figure 2 shows median excreted thiocyanate contents of collected urine samples. Median values were estimated to be 15mg/L. No significant differences between medians of various age or sex groupings could be detected. Median I/SCN ratios of the children are shown in Figure 3. Again, the medians of the groupings were approximately 9µg/mg with large standard deviations. No significant differences were detected between the groupings. The youths with excreted iodine levels below 50µg/L were consideredas iodine deficient according to the World Health Organization's (WHO) recommendations.19 Results from analysis of youths' urine samples are shown in Table 1. The results indicate that 22% of boys between the ages of three and five years were iodine deficient. Further, 29% of boys age six to nine years and 17% of 14 to 19 year old boys were iodine deficient. The prevalence of iodine deficiency in girls was a bit smaller compared to that in boys. Among the results, 18% of girls between the ages of three to five were iodine deficient. Sixteen percent of girls aged six to nine years were iodine deficient while 21% of 14 to 19 year old girls had urinary excreted iodine levels below 50ug/L.
Fig. 1.
Median urinary iodine excretion in youths of district Bamougoum, Cameroon. The iodine contents were assayed by a method described by Moxon and Dixon16 with a modification that the mineralization was performed at 600°C in an alkaline medium. Error bars represent + standard error.
Fig. 2.
Median urinary thiocyanate excretion in youths of district Bamougoum, Cameroon. Thiocyanate contents were quantified following the method described by Ngogang18. Error bars represent + standard error.
Fig. 3.
Median urinary iodine/thiocyanate excretion ratio in youths of district Bamougoum, Cameroon. Error bars represent + standard error.
Table 1.
Percentage of iodine deficiency in human subjects by age group and gender. In accordance with the World Health Organization's (WHO) recommendations19, the urine samples with I<50µg/L and I/SCN< 3µg/mg represent iodine deficiency.
| Boys | Girls | |||||||||
| I<50µg/L | I/SCN<3µg/mg | I<50µg/L | I/SCN<3µg/mg | |||||||
| Age group (y.o.*) | n | # | % | # | % | n | # | % | # | % |
| 3–5 | 9 | 2 | 22 | 2 | 22 | 11 | 2 | 18 | 3 | 27 |
| 6–9 | 21 | 6 | 29 | 5 | 24 | 19 | 3 | 16 | 2 | 11 |
| 10–13 | 22 | 5 | 23 | 4 | 18 | 18 | 3 | 17 | 3 | 17 |
| 14–19 | 6 | 1 | 17 | 3 | 50 | 14 | 3 | 21 | 2 | 14 |
| Total | 58 | 14 | 24 | 14 | 24 | 62 | 11 | 18 | 10 | 16 |
y.o., years old
The data on the population with excreted thiocyanate overloaded is also presented in Table 1. I/SCN ratios below 3µg/mg were considered as indicative of thiocyanate overload, as per World Health Organization (WHO) recommendations.19 The data indicates that 22% of three to five year old boys were thiocyanate overloaded. Twenty four percent of boys aged six to nine years were thiocyanate overloaded. Even greater, half of samples from 14 to 19 years old boys had an I/SCN ratio above 3ug/mg. Again, the girls fared slightly better than boys since the percentage of girls with thiocyanate overload was less. Twenty seven percent of samples from three to five year old girls had a thiocyanate overload. Eleven percent of girls aged six to nine years were thiocyanate overloaded. Fourteen percent of the samples from last age group of 14 to 19 year old girls had I/SCN ratio above 3ug/mg.
When pooling data from both sexes, as in Table 2, the highest prevalence of iodine deficiency (23%) was found in children aged 6–9. The rest of the age groups studied had a 20% prevalence of iodine deficiency. Overall, twenty one percent of the total subject population was iodine deficient, which nears the 20% value characteristic of endemic goiter areas. Table 2 also shows the percentage of thiocyanate overloaded children. The highest prevalence of 23% of thiocyanate overload was found in children aged 3–5 and 14–19. The age groups 6–9 and 10–13 had a lower 18% prevalence of thiocyanate overload. Overall, twenty percent of the total subject population show thiocyanate overload.
Table 2.
Percentage of iodine deficiency and thiocyanate overloads in human subjects by age group. In accordance with the World Health Organization's (WHO) recommendations19, the urine samples with I<50µg/L and I/SCN< 3µg/mg represent iodine deficiency.
| I<50µg/L | I/SCN<3µg/mg | ||||||
| Age group (y.o.*) | n | # | % | # | % | ||
| 3–5 | 20 | 4 | 20 | 5 | 25 | ||
| 6–9 | 40 | 9 | 23 | 7 | 18 | ||
| 10–13 | 40 | 8 | 20 | 7 | 18 | ||
| 14–19 | 20 | 4 | 20 | 5 | 25 | ||
| Total | 120 | 25 | 21 | 24 | 20 | ||
y.o., years old
Discussion
Iodine is an essential element that enables the thyroid gland to produce thyroid hormones. This element is ingested and absorbed in the gut almost completely in different forms. In a healthy person, 90% of ingested iodine is excreted through urine. If iodine deficiency is present, the ingested iodine will be further retained by the body reducing the levels of excreted urinary iodine. Therefore, the level of urinary iodine is used as an indicator for the assessment of IDD. The WHO defines iodine deficiency as excreted urinary iodine content below 50µg/L. Furthermore, a population is classified at risk of IDD if 20% of the population falls below the 50µg/L threshold or if the median excreted iodine content is below 100µg/L.19
According to our study, 24% of boys had urinary iodine excretion levels lower than 50µg/L while 18% of girls were below this threshold (Table 1). When considering our whole study population, 21% of subjects had urinary iodine excretion levels lower than 50µg/L. Consequently, Bamougoum's youth should be considered at risk of IDD according to the WHO definition.19 This can be explained by the strong consumption of staple foods that are low in iodine such as fufu maize and vegetables like black nightshade by the habitants of the Bamougoum area.
Low urinary iodine excretion and low urinary ratio of I/SCN are the fundamental criteria for detection of IDD in any population. The former reflects iodine availability while the latter, the goitrogenic food consumption. It is known that a normally adequate intake of iodine may not ensure thyroid function in the presence of goitrogens.11 In fact, intake of a goitrogen-rich diet can induce goiter even when iodine supply is sufficient.20, 21, 22 In the present study, twenty percent of the total study population (24% for boys and 16% for girls) was suffering from thiocyanate overload. I/SCN ratios less than 3µg/mg suggest too little iodine and/or too much goitrogenic thiocyanate relative to each other. The food consumed by these children might contain goitrogenic substances such as thionamide-like compounds and thiocyanate which are known to affect thyroid function.23 A geochemical goitrogen cannot be ruled out as a possible contributing factor.24, 25 By applying similar WHO iodine deficiency criteria to the thiocyanate overload data, the prevalence of thiocyanate overload among the children studied suggests an endemic case throughout the general population. Table 1 shows the proportion of children in each group classified as either iodine deficient (I<50µg/) according to WHO or thiocyanate overloaded (I/SCN<3µg/mg). Except for the youngest age group (3–5 years of age), a smaller percentage of girls were classified as iodine deficient and thiocyanate overloaded compared to boys. Among the study subjects, the age distribution tended towards 6–13 year old children, especially among boys who were mostly 10–13 years old.
When pooling data from both sexes, as in Table 2, the prevalence of iodine deficiency in children was more evident. In fact, this was especially true for children aged 6-9, among whom approximately 23% were iodine deficient. Roughly 21% of the total subject population was iodine deficient, which nears the 20% value characteristic of endemic goiter areas. The low I/SCN ratio can be attributed to consumption of fufu maize and cassava, which during processing, are mixed together. Cassava tubers are low in iodine especially those growing in Mountains regions as Bamougoum, where downpours wash minerals from apex of the mountain to the dregs. They also contain goitrogenic substances such as cyanogenic glycosides.25 Thiocyanate (SCN) is a competitive inhibitor of the human thyroid sodium/iodide symporter NIS which can have adverse effects like developing IDD. Thus, a thiocyanate overload originating from consumption of poorly detoxified cassava can aggravate a mild or severe iodine deficiency.26 Additionally, another complement of fufu maize is black nightshade, which has low iodine and high goitrogen contents. So, the existing goiter prevalence in the region could possibly be due to adequate but variable iodine supply along with an aggravating thiocyanate overload.21, 22, 27, 28, 29,30
It is difficult to maintain a sufficient iodine intake in these villages as the individual foods are very low in this element and contain goitrogenic substances. Artificial iodine supplementation via iodized salt is one of the best strategies to ameliorate the incidence of IDD because of its efficacy.31, 32, 33 However such an approach has proven to be far from ‘universal’ because of inconsistent maintenance and storage throughout the edible salt chain, lack of political will, weak monitoring systems and lack of capacity for enforcing legislation in many developing countries.34, 35, 36, 37, 38
The consumption of seaweed, which is rich in iodine, could be an easy, non-toxic way to meet dietary iodine requirements but is not readily available to those living in poorly developed areas such as Bamougoum.39, 40 Changes in dietary habits could yield great improvements. By increasing consumption of high iodine foods such as the yam, kelen kelen or eggplant leaves would help prevent IDD. However, to successfully decrease the occurrence of IDD, SCN overload from other foods must be avoided especially among those with only adequate iodine contents.22 It is necessary to further analyze the goitrogen contents in order to determine which goitrogen-rich foods should be avoided. As resource-poor people tend to be most at risk to IDD and tend to be limited in their dietary choices, nutritional improvement may prove difficult.
Crop improvement strategies and improved soil management might be more efficacious in combating iodine deficiency and SCN overload. For example, development of low goitrogen Brassica cultivars, such as cabbage, would likely be more feasible than attempting to boost iodine levels. An effective iodine supplementation program, such as salt iodination, still holds great promise to help abate endemic goiter and IDD among the world's poor. Moreover, it is most encouraging to witness the advances being made in genetically engineered cassava for lowering cyanide content in the staple diet of these regions.41
Acknowledgments
This work was funded by grants from The Rockefeller Foundation, l'Agence Universitaire de la Francophonie and the Natural Sciences and Engineering Research Council of Canada to IA.
References
- 1.Papi G, Pearce EN, Braverman LE, Betterle C, Roti E. A clinical and therapeutic approach to thyrotoxicosis with thyroid-stimulating hormone suppression only. Am J Med. 2005;118:349–361. doi: 10.1016/j.amjmed.2005.01.004. [DOI] [PubMed] [Google Scholar]
- 2.Perring L, Basic-Doral M, Andrey D. Colorimetric determination of inorganic iodine in fortified culinary products. Analyst. 2001;126:985–988. doi: 10.1039/b102423j. [DOI] [PubMed] [Google Scholar]
- 3.Delange F, Burgi H, Chen ZP, Dunn JT. World status of monitoring of iodine deficiency disorders control programs. Thyroid. 2002;12:915–924. doi: 10.1089/105072502761016557. [DOI] [PubMed] [Google Scholar]
- 4.Hetzel BS. Iodine and neuropsychological development. J Nutr. 2000;130(Suppl):493S–495S. doi: 10.1093/jn/130.2.493S. [DOI] [PubMed] [Google Scholar]
- 5.Plantin-Carrenard E, Beaudeux JL. Physiopathologie de l'iode: intérêt actuel de son dosage en biologie clinique. Annales de Biologie Clinique. 2000;58:395–401. (Fre). In French. [PubMed] [Google Scholar]
- 6.Hetzel BS. Eliminating iodine deficiency disorders - the role of the International Council in the global partnership. Bull World Health Org. 2002;80:341. [PMC free article] [PubMed] [Google Scholar]
- 7.Krajcovicova-Kudlackova M, Buckova K, Klimes I, Sebokova E. Iodine deficiency in vegetarians and vegans. Ann Nutr Metab. 2003;47:183–185. doi: 10.1159/000070483. [DOI] [PubMed] [Google Scholar]
- 8.Tonacchera M, Pinchera A, Dimida A, Ferrarini E, Agretti P, Vitti P, Santini F, Crump K, Gibbs J. Relative potencies and additivity of perchlorate, thiocyanate, nitrate, and iodide on the inhibition of radioactive iodide uptake by the human sodium iodide symporter. Thyroid. 2004;14:1012–1019. doi: 10.1089/thy.2004.14.1012. [DOI] [PubMed] [Google Scholar]
- 9.Dohan O, De la Vieja A, Paroder V, Riedel C, Artani M, Reed M, Ginter CS, Carrasco N. The sodium/iodide Symporter (NIS): characterization, regulation, and medical significance. Endocrine Rev. 2003;24:48–77. doi: 10.1210/er.2001-0029. [DOI] [PubMed] [Google Scholar]
- 10.Spitzweg C, Heufelder AE, Morris JC. Thyroid iodine transport. Thyroid. 2000;10:321–330. doi: 10.1089/thy.2000.10.321. [DOI] [PubMed] [Google Scholar]
- 11.Rao PS, Lakshmy R. Role of goitrogens in iodine deficiency disorders & brain development. Ind J Med Res. 1995;102:223–226. [PubMed] [Google Scholar]
- 12.Tahboub YR, Galijasevic S, Diamond MP, Abu-Soud HM. Thiocyanate modulates the catalytic activity of mammalian peroxidases. J Biol Chem. 2005;280:26129–26136. doi: 10.1074/jbc.M503027200. [DOI] [PubMed] [Google Scholar]
- 13.Delange F. Iodine deficiency as a cause of brain damage. Postgrad Med J. 2001;77:217–220. doi: 10.1136/pmj.77.906.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.World Bank, author. Enriching lives: Overcoming vitamin and mineral malnutrition in developing countries. Washington DC: World Bank Publications; 1994. p. 9. [Google Scholar]
- 15.Santiago-Fernandez P. Intelligence quotient and iodine intake: a cross-sectional study in children. J Clinic Endocrin Metab. 2004;89:3851–3857. doi: 10.1210/jc.2003-031652. [DOI] [PubMed] [Google Scholar]
- 16.Ngogang YJ. Techniques biochimiques élémentaires pour le diagnostic des troubles dus à la carence en iode. Yaoundé: Éditions Sopecam; 1990. Dosage de l'iode dans l'eau et les urines; pp. 3–7. (Fre). In French. [Google Scholar]
- 17.Karmrakar MG, Pandav CS, Krishnamachari KBVR. Principle and procedure for iodine estimation and laboratory manual. New Delhi: Ind Counc Med Res; 1986. [Google Scholar]
- 18.Moxon RE, Dixon E. Semi-automatic method for the determination of total iodine in food. Analyst. 1980;105:344–352. doi: 10.1039/an9800500344. [DOI] [PubMed] [Google Scholar]
- 19.World Health Organisation, United Nations Children's Fund, International Council for Control of Iodine Deficiency Disorders, author. Assessment of the Iodine Deficiency Disorders and monitoring their elimination. 2nd ed. Geneva: WHO; 2001. pp. 1–107. [Google Scholar]
- 20.Chandrajith R, Dissanayake CB, Tobschall HJ. Geochemistry of trace elements in paddy (rice) soils of Sri Lanka—implications for iodine deficiency disorders (IDD) Environ Geochem Health. 2005;27:55–64. doi: 10.1007/s10653-004-2290-2. [DOI] [PubMed] [Google Scholar]
- 21.Gaitan E. Goitrogens in food and water. Annu Rev Nutr. 1990;10:21–39. doi: 10.1146/annurev.nu.10.070190.000321. [DOI] [PubMed] [Google Scholar]
- 22.Jooste PL, Weight MJ, Kriek JA, Louw AJ. Endemic goiter in the absence of iodine deficiency in schoolchildren of the Northern Cape Province of South Africa. Eur J Clin Nutr. 1999;53:8–12. doi: 10.1038/sj.ejcn.1600671. [DOI] [PubMed] [Google Scholar]
- 23.Erdogan G, Erdogan MF, Sav H, Güllü S, Kamel N. Endemic goiter, thiocyanate overload, and selenium status in school-age children. Biol Trace Elem Res. 2001;79:121–130. doi: 10.1385/BTER:79:2:121. [DOI] [PubMed] [Google Scholar]
- 24.Saikat SQ, Carter JE, Mehra A, Smith B, Stewart A. Goiter and environmental iodine deficiency in the UK—Derbyshire: A review. Environ Geochem Health. 2004;26:395–401. doi: 10.1007/s10653-005-7165-7. [DOI] [PubMed] [Google Scholar]
- 25.Conn EE. Cyanogenic glucosides. J Agric Food Chem. 1969;17:519–526. [Google Scholar]
- 26.Thilly CH, Vanderpas JB, Bebe N, Ntambue K, Contempre B, Swennen B, Moreno-Reyes R, Bourdoux P, Delange F. Iodine deficiency, other trace elements, and goitrogenic factors in the etiopathogeny of iodine deficiency disorders. Biol Trace Elem Res. 1992;32:229–243. doi: 10.1007/BF02784606. [DOI] [PubMed] [Google Scholar]
- 27.Aquaron R, Nguessi P, Ben Eno L, Riviere R. Endemic goiter in Cameroon. Revue française d'endocrinologie clinique, nutrition et métabolisme. 1985;26:537–546. (Fre). In French. [Google Scholar]
- 28.Merck manual of diagnosis and therapy. Rahway, N.J.: Merck, Sharp & Dohme Research Laboratories; 1999. Mineral Deficiency and Toxicity, Iodine; p. 51. [Google Scholar]
- 29.Taga I, Sameza ML, Kayo AV, Ngogang YJ. Évaluation de la teneur en iode des aliments et du sol de certaines régions du Cameroun. Santé. 2004;14:11–15. (Fre). In French. [PubMed] [Google Scholar]
- 30.Salpou D. Contribution à l'étude des troubles dus à la carence en iode (TDCI) et de l'hypothyroídie juvénile, dans l'arrondissement de Doukoula province de l'Extrême Nord Cameroun. Yaoundé: Université de Yaoundé; 1992. p. 35. (Fre). MD Thesis. In French. [Google Scholar]
- 31.Mackowiak CL, Grossl PR. Iodate and iodide effects on iodine uptake and partitioning in rice grown in solution culture. Plant Soil. 1999;212:135–143. doi: 10.1023/a:1004666607330. [DOI] [PubMed] [Google Scholar]
- 32.Szybinski Z, Delange F, Lewinski A, Podoba J, Rybakowa M, Wasik R, Szewczyk L, Huszno B, Golkowski F, Przybylik-Mazurek E, Karbownik M, Zak T, Pantoflinski J, Trofimiuk M, Kinalska I. A programme of iodine supplementation using only iodised household salt is efficient—the case of Poland. Eur J Endocrinol. 2001;144:331–337. doi: 10.1530/eje.0.1440331. [DOI] [PubMed] [Google Scholar]
- 33.Biswas AB, Chakraborty I, Das DK, Biswas S, Nandy S, Mitra J. Iodine deficiency disorders among school children of Malda, West Bengal, India. J Health Pop Nutr. 2002;20:180–183. [PubMed] [Google Scholar]
- 34.Dunn JT. Seven deadly sins in confronting endemic iodine deficiency, and how to avoid them. J Clin Endocrinol Metab. 1996;81:1332–1335. doi: 10.1210/jcem.81.4.8636328. [DOI] [PubMed] [Google Scholar]
- 35.Yamada C, Oyunchimeg D. Difference in goiter rates between regular and occasional users of iodized salt in Mongolia. Food Nutr Bull. 2002;23:89–93. doi: 10.1177/156482650202300112. [DOI] [PubMed] [Google Scholar]
- 36.Diosady LL, Alberti JO, Venkatesh Mannar MG, Fitzgerald S. Stability of iodine in iodized salt used for correction of iodine deficiency disorders II. Food Nutr Bull. 1998;19:239–249. [Google Scholar]
- 37.Remer T, Neubert A, Manz F. Increased risk of iodine deficiency with vegetarian nutrition. Br J Nutr. 1999;81:3–4. doi: 10.1017/s0007114599000136. [DOI] [PubMed] [Google Scholar]
- 38.Zimmermann MB. Assessing iodine status and monitoring progress of iodized salt programs. Nutri Res. 2004;134:1673–1677. doi: 10.1093/jn/134.7.fpage. [DOI] [PubMed] [Google Scholar]
- 39.Lee SM, Lewis J, Buss DH, Holcombe GD, Lawrance PR. Iodine in British foods and diets. Br J Nutr. 1994;72:435–446. doi: 10.1079/bjn19940045. [DOI] [PubMed] [Google Scholar]
- 40.Maberly GF, Trowbridge FL, Yip R, Sullivan KM, West CE. Programs against micronutrient malnutrition: ending hidden hunger. Annu Rev Publ Health. 1994;15:277–301. doi: 10.1146/annurev.pu.15.050194.001425. [DOI] [PubMed] [Google Scholar]
- 41.Siritunga D, Sayre R. Engineering cyanogen synthesis and turnover in cassava (Manihot esculenta) Plant Mol Biol. 2004;56:661–669. doi: 10.1007/s11103-004-3415-9. [DOI] [PubMed] [Google Scholar]