Abstract
Introduction
Since mid 1990s, Uganda has had an estimated 1.6 million internally displaced persons (IDPs) in the northern and eastern districts. A major cause of morbidity and mortality amongst children in displaced settings is protein energy malnutrition.
Objective
To estimate the prevalence of and describe the risk factors for protein energy malnutrition among under five years old children living in internally displaced persons camps in Omoro county Gulu district.
Methods
This was a cross sectional study undertaken among internally displaced people's in Omoro county, Gulu district during 13 – 23rd September 2006. Anthropometric measurements of 672 children aged 3 – 59 months were undertaken and all their caretakers interviewed. The anthropometric measurements were analyzed using z-scores of height-for-age (H/A) and weight-for-height (W/H) indices. Qualitative data were collected through 6 focus group discussions, key informant interviews and observation. Data were captured using Epi Data version 3.0 and analyzed using EPI-INFO version 3.3.2 and SPSS version 12.0 computer packages respectively. ResultsThe prevalence of global stunting was found to be 52.4% and of global acute malnutrition 6.0%. Male children are at risk of being stunted Adjusted OR 1.57 95% CI 1.15–2.13; p value=0.004. Children in the age group 3 – 24 months were at risk of acute malnutrition Adjusted OR 2.78 95% CI 1.26–6.15; p value=0.012 while de-worming was protective Adjusted OR 0.44 95% CI 0.22–0.88; p value=0.018. The main sources of foodstuff for IDPs include food rations distributed by WFP, cultivation and purchase.
Conclusion and Recommendations
There is high prevalence of protein energy malnutrition (stunting) among children in the internally displaced people's camps in Gulu district. Male children are at an increased risk of stunting while children aged between 3 – 24 months are at an increased risk of suffering from acute malnutrition. Stakeholders including local government and relief organizations should intensify efforts to improve the nutritional status of IDPs especially children in the camp settings. The quantity of and access to household food supplies, health education on infant and child feeding and integrated management of childhood illnesses (IMCI) activities in the camps should be strengthened.
Keywords: PEM, prevalence, risk factors, IDP, northern Uganda
Introduction
Since the mid 1990s, Uganda has had an estimated 1.6 million internally displaced persons in northern and eastern regions of the country. The massive population displacement has been due to a protracted 20 year old civil war between the Lord's Resistance Army (LRA) rebels and the government armed forces. The districts of the Acholi sub-region of Gulu, Kitgum, Pader and Amuru have been the most severely affected.
To date the majority of the population in the Acholi sub-region districts live in encampment.1, 2, 3 The health indices in the Acholi sub-region remains poor with high crude and under five mortality rates, estimated at 1.54 and 3.18 per 10,000/day respectively.2 The crude mortality rate (CMR) and the under five mortality rate (U5MR) in Gulu district IDP camps are high estimated at 1.22 and 2.31 per 10,000/day respectively. These mortality rates are both above the emergency thresholds of 1/10,000/day and 2/10,000/day respectively and the national estimates of 0.46/10,000/day and 0.98/10,000/day respectively.2
During emergency, women and children are extremely vulnerable owing to socio-cultural, economic and physiologic reasons.4, 5 Several factors including poverty, poor nutrition, inadequate water and sanitation, lack of adequate health services, insecurity displacement predispose displaced population to high levels of morbidity and mortality.4 Excess mortality in displaced population settings is often caused by the same disease that affect displaced populations including acute lower respiratory tract infection (ARI), malaria, measles, diarrheal diseases and malnutrition.4, 6
Protein energy malnutrition is a major cause of morbidity and mortality in children in sub-Saharan Africa. The prevalence of malnutrition is high in Africa, with 38.6% of the children under five years stunted, 28.4% underweight, and 7.2% wasted.7 Uganda has high rates of malnutrition. The prevalence rate of global stunting is estimated at 39.1%, underweight 22.8% and global wasting 4.1%.8
Malnutrition is the cellular imbalance between the supply of nutrients, energy and the body's demand for them to ensure growth, maintenance and specific functions. The causes of malnutrition are multi-factorial. Dietary and environmental factors contribute to the risks of malnutrition in children.9 The spectrum of the more severe forms of protein energy malnutrition of early childhood considered to form clinical and biochemical change include nutritional marasmus, marasmickwashiorkor and kwashiorkor.10 The objective of the study was to estimate the prevalence of and investigate the risk factors for malnutrition among the children aged 3–59 months in internally displaced persons camps, Omoro county, Gulu district.
Methods
Study Site
The study was carried out in IDP camps in Omoro county, Gulu District. Administratively the county comprises 6 sub counties.11 There are a total of 13 camps in the county situated in each sub county. The camps population range from 2,577 to 24,772, with a total of 129,048 inhabitants. The under five year comprise 20% of the total camp population. The camps are divided into zones, which are further subdivided into administrative blocks. There are 5–10 zones per camp. Omoro county has 2 supplementary feeding centers, located in Awere and Opit camps respectively. There are 2 health center level III in the county. Referrals of the severely sick persons from Omoro are usually made to Gulu regional referral hospital, Lacor hospital and occasionally to Gulu independent hospital.
Sampling procedure
This was a cross sectional study. The study populations comprised children aged 3–59 months and their caretakers. We used multistage sampling procedure to select sub counties, camps, zones and households for the household survey. There are 6 sub-counties in Omoro county. Four (67%) of the sub counties in the district were randomly selected. In each sub county a camp was randomly selected. Thus a total of four camps were randomly selected from the four sub counties. In each of the 4 camps selected, 2 zones were randomly selected. Hence a total of 8 zones were included in the study. A zone constituted the study cluster.
To select a household per camp, probability proportion to size was used. Thus the zone with a bigger number of households had more participants selected and interviewed. The modified WHO cluster sampling technique was used to select study households and participants.12 In the selected zones a borehole was considered as the center of the cluster/zone. To determine the direction of movement, the camp leader spun a pen. The direction pointed by the tip of the pen was followed. The households in the direction the pencil pointed (from the centre to the end of the cluster) were allocated numbers. To determine the starting point (household) random selection was made.
In each selected household, the parents/caretakers were interviewed to obtain information about their children aged 3 – 59 months. Anthropometric measurements (weight and height) were taken, and the children aged 3–59 months were also examined for edema. If more than one child between the age of 3 months to 59 months was found in the same household, then one of them was randomly selected. The child selected was referred to as an index child. If the index child was from a multiple birth (twin or triplet), then both or all the children of that birth were assessed in order to conform to the cultural practices. The next household chosen for the interview was the one whose door was nearest to the previous household in which the interview had been conducted. A household with no child under five years of age was skipped.
Anthropometric measurements
Anthropometric measurements of a total of 678 eligible children including weight and heights were taken. Weight was recorded in kilograms (kg) to the nearest 0.1kg. Children were weighed using electronic weighing scales and those who were unable to stand, had their weights obtained from the difference between weights of mother/caretaker as she/he holds the child and the weight of the mother/caretaker alone.
Heights/lengths measurements were carried out using measuring boards (stadiometers) and were recorded in centimeters (cm) to the nearest 0.1 cm. Children aged more than 24 months (more or equal to 85cm) heights were measured while standing, while those less than 24 months or less than 85cm, had theirs lengths measured while lying down.
Clinical evaluations of the malnourished children was undertaken to check for the presence of oedema. Oedema was recorded as present when a shallow imprint persisted on both feet when pressure was removed and absent when there was no pitting of the dorsum of both feet.
Qualitative data collection
Six focus group discussions were conducted. The FGDs consisted of 8 people each and comprised mothers, fathers and other caretakers who had not participated in the questionnaire interview. Each discussion took about one hour. The focus group discussions were taped recorded.
In-depth key informants' interviews (KIIs) were conducted. The key informants comprised camp leaders, zone leaders; community owned resource persons and health workers in charge of health centers serving the camps. The key informants provided information on causes of protein energy malnutrition, and utilization of nutrition and health services offered in the camp settings.
Quality control
The research assistants were trained for two days on how to take measurements including weights and lengths/heights. The questionnaires were translated into Luo/Acholi language and back translated into English. The selected research assistants were fluent in both English and Acholi languages. The questionnaires were pre-tested. The weighing scales and measuring boards (stadiometers) were standardized to the nearest 0.1kg and 0.1cm respectively. The weighing scale was recalibrated to zero after every child was weighed. Completed questionnaires were checked by the principal investigator daily for accuracy, completeness and consistency before leaving the IDP camps.
Data analysis
Quantitative data were checked for completeness, sorted, coded and entered into the computer using EpiData version 3.0. The data were analyzed using EPI INFO version 6.03 and SPSS version 11. Anthropometric measurement outcomes were defined in terms of wasting and stunting using weight for height and height for age indices respectively expressed in standard deviation (z-scores). Univariate and bivariate analyses were done to determine factors that were significantly associated with wasting and stunting. Chi square test was used to ascertain statistical significance of the variables at p value <0.05. All variables with a p value less than or equal to 0.2 were entered into logistic regression to determine the risk factors for protein energy malnutrition. Qualitative data were analyzed manually. Content analysis was based on condensation and abstraction of main themes focusing on causes of protein energy malnutrition.
Results
Socio-demographic characteristics of caretakers
Two thirds of the caretakers (67.7%) were peasant farmers. Most of the parents/caretakers 570 (84.8%) had stayed in the camps for less than four years.
Sources of foodstuff
The caretakers reported various ways of obtaining foodstuff. The majority 78% of households obtained foodstuff through WFP food distributions, purchase of food, cultivation and worked in exchange for foodstuff.
“The amount of food given to us is not enough and lasts for a maximum of only one week, yet food distribution is monthly. We are therefore involved in all kind of casual labour activities (leja — leja) so as to get money to buy food or sometimes work in exchange for food” (Koro Abili FGD Mothers)
Other sources of food include cultivation. However the men (FGD) reported difficulty in acquiring land for cultivation in the camp settings and in obtaining money for purchasing food stuff for their families.
“We are in this camp, but our home land is far from here. We do not have land to cultivate. Its expensive to hire land around here. We don't even have the money. We therefore have to depend on World Food Programme rations which are very little” (Koro Tetugu FGD Men)
“We go the whole day in search of casual work (leja — leja) to get some money for buying food. Our children are left home without food the whole day. Our children eat food in the morning and have to wait for their next meal in the evening when we return from doing leja- leja”. (FGD Women)
The caretakers reported that new comers to the camps were not immediately entitled to the World Food Programme food rations. They have to wait until their names are included in the registry for food distribution and this may take a minimum of one year.
“Sometimes the number of members in the households is being reduced to a smaller number in the registry at the WFP offices, reducing the amount of foodstuff given further and yet food is distributed only once a month.” (KII-Camp leader — Koro Abili)
The types of food distributed are not diverse and consists of maize seeds, beans and cooking oil, with no animal protein.
“We do not have a variety of foodstuff to feed on as before we came to the camps. Our children are now forced to feed on only one type of food for a long period of time.” (Koro-Abili FGD Men)
Complementary feeding practices
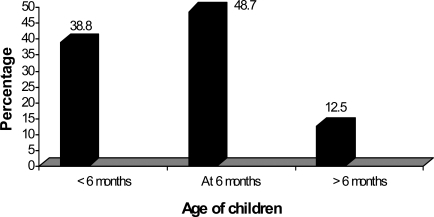
As shown in the figure below, nearly half 49% of the children had timely complementary feeding; however 39% of the children received complementary feeds before the age of 6 months and 13% after 6 months.
Figure.
Age at onset of complementary feeding
The most commonly provided complementary foods were cereals (mainly maize), vegetables and tubers (sweet potatoes and cassava). Animal based foods (meat/fish) were rarely given because of lack of affordability. The caretakers reported that breastfeeding children were given Soya maize flour for porridge by World Vision. However, the flour was unfortunately being sold off by the caretakers to obtain money for buying foodstuff for the whole household, as one caretaker stated;
“This porridge flour gives our children diarrhea, so we either sell the flour and use the money to buy other foodstuff for the whole household or we the adults take the porridge”. (FGD Men)
Mothers stated that
“We ourselves go hungry the whole day in search of food; hence we don't have enough breast milk for the babies. We are busy searching for food, fetching water, in addition to doing gardening. We leave the young children at home with their siblings”. (FGD Mothers)
The prevalence of global stunting was 52.4% and severe stunting 24.9%. The prevalence of both global acute malnutrition and stunting were higher in the age groups 6–12 months and 13–24 months compared to the rest of the age groups. The prevalence of global acute malnutrition (GAM) was 6.0%.
The most prevalent diseases that the children in the IDP camps had were fever (84.8%), cough (81.7%) and diarrhea 62%.
The presence of fever was significantly associated with global acute malnutrition OR 7.42 95% CI 1.01–54.61 (p value=0.021) and being a male child OR 1.52 95% CI 1.12–2.05 (p value=0.007) was significantly associated with chronic malnutrition.
Logistical regression analysis
Logistical regression analysis into the causes of malnutrition was performed. Variables with p value less or equal to 0.2 were selected. The selected variables for acute malnutrition included: household head, major age groups, gender of the child, evidence of deworming, diarrhea and fever. While for stunting, the variables selected were major age group, gender, diarrhea and cough.
On logistic regression, age group 3 – 24 months Adjusted OR 2.78 95% CI 1.26–6.15 (p value = 0.012) was significantly associated with acute malnutrition, while deworming in the previous 3 months Adjusted OR 0.55 95% CI 0.22–0.87 (p value = 0.018) was protective. A male child was nearly 2 times more likely to suffer chronic malnutrition compared to a female child Adjusted OR 1.56 95% CI 1.15–2.13 (p value = 0.004).
Discussion
This study has shown high prevalence of global stunting of 52.1%, and global acute malnutrition 6.0% respectively in the IDP settings in Gulu district, northern Uganda. Our findings indicate slight increment in the prevalence of malnutrition compared to those reported in previous studies in the settings.13, 14, 15 Although the studies were carried out during different seasons, the previous conducted during harvest and ours done during the planting season, nevertheless, both studies reveal high levels of both chronic and acute malnutrition, reflecting long standing food shortage experienced by the internally displaced populations in the camp settings. The lack of foodstuff for the internally displaced populations in encampment may be attributable to several reasons including inadequate and irregular food supply and limited productivity.
It was observed that the main sources of foodstuff for the IDPs included food rations distributed by WFP. The food rations supplied is supplemented by limited cultivation, food for work i.e “leja leja” and through purchase of foodstuff. However, several caretakers reported that the WFP food rations were inadequate in quantity and limited in variety. The ration comprises principally beans, posho and cooking oil. Furthermore, access to foodstuff by new camp IDPs was reported to be difficult. New IDPs often had to wait till their names were included in the registry. This process was reported to take very long - up to a year or more. The process of screening and registration of the beneficiary displaced population ought to be hastened in order to ensure quicker access to foodstuff by the affected populations.
The study revealed that the cultivation of foodstuff is grossly limited in the IDP camp settings. The reasons for this include insecurity and lack of land to cultivate. The IDPs in both peri-urban and rural areas have to hire land for cultivation. Many IDP couldn't afford hiring sizable land areas for cultivation because of financial difficulty. Moreover, the time for cultivation is also restricted. IDPs can only access their gardens during particular time of the day, usually between about 10.00am and have to return to the camps by about 4.00pm. Men on the other hand, were reported to spend most of the time drinking alcohol leaving the women to do most of the cultivation and to look for money to feed their families in the settings. Hence women tend to engage in a variety of casual labour activities to generate money to buy foodstuff to feed their families. Thus, most mothers tend to stay away from home for long duration compounding the problem of caring for and feeding their children in the camp settings.
The main nutritional interventions implemented in the settings include blanket food distribution, supplementary feeding of children with moderate malnutrition and therapeutic feeding centers children with severe malnutrition.16 During the study period, however, it was established that the amount of foodstuff supplied - the blanket food distributed had been reduced. The reduction was triggered by the prospects of IDPs return to their original homesteads. Although the implementing NGO-World Vision, reported that food distribution would continue during the period of camp decongestion, it's advisable that all the stakeholders (local government, NGOs/UN agencies) ensure a phase reduction in food supplementation during the decongestion and resettlement periods. The supply of foodstuff to returnees ought to continue until the time when the returnees have harvested their own foodstuff in order not to aggravate their already precarious nutritional status.
Our study showed that younger children aged 3 – 24 months had a higher risk of suffering from acute malnutrition and stunting compared to the older age group 25 – 59 months. The findings are consistent with those of non displaced populations.17, 18, 19 In camp situations, however, several factors including poor socioeconomic status, mother's absence from home (spend most of the time doing casual labour in order to get money buy foodstuff), poor weaning practices, leaving the infants with their siblings or their grandmothers may contribute to poor nutritional status of the younger children. Moreover, in the camp settings, it's notable that the most commonly provided complementary foods comprised maize, vegetables and tubers such as sweet potatoes and cassava. Animal based protein foods were rarely given as complementary feeds because the mothers/caretakers could not afford them. Furthermore, the communal feeding practices of the communities whereby the young children (less than 2 years) feed with the older children (persons) may predispose the younger siblings to under feeding as they may not be able to feed adequately alongside the older children on the meal provided.
This study has revealed that male children had nearly two fold increased risk of becoming stunted. Our findings are consistent with those of other studies.20, 21 The predisposition of the male children to increased risk of stunting may be due to several reasons. One of the explanations could be that the boys are rare at home. They tend to be active, running around in the neighbor hood as compared to the female children who probably eat whatever small feeds that their mothers got since they are always with them at home. Furthermore, a study byWamani et al. 2007 reported that low social economic status of the parents predisposes the boy child to stunting. Indeed in these IDP camps settings, the parents/caretakers have very poor social economic status; owing to several years of deprivation, homelessness, loss of their wealth, lack of farming and employment opportunities. Nation wide, the conflict affected region of northern Uganda has the lowest human development index (HDI) - a composite measure of longeivity, educational attainment and standards of living of 0.32 compared to central region with HDI of 0.49, western 0.37, eastern 0.36 and the national HDI of 0.4022.
The presence of co-morbidity — communicable disease infections such as fever (malaria) was associated with acute malnutrition in the settings. Studies amongst refugees in Sudan and Uganda showed that the risk of malnutrition increased with increasing communicable disease burden including malaria, diarrhea and pneumonia.23, 24 There are several mechanisms through which communicable diseases predispose to poor nutrition including poor appetite, malabsorption and chronic ill health. Our study revealed that most caretakers 7 in 10 preferred using the services of health workers within the camps. The caretakers further reported that they mainly go the community owned resource persons (CORPs) for treatment when their children fall ill at night, but they go to the health centers within the camps during daytime. These findings suggest the need to strengthen the capacity of CORPs to effectively manage the simple conditions (diseases) in the settings. Furthermore, there is need to strengthen the capacity of the formal health care system to provide effective clinical, preventive and promotive health services and referrals services. There is need to adequately equip and train available health facilities human resources to offer effective services in such settings.
Conclusions and Recommendations
Our study has shown high prevalence of malnutrition (stunting and acute malnutrition) among the under five children living in Omoro county IDP camps, Gulu district. Male children and those aged between 3 –24 months are at risk at of stunting and acute malnutrition. The high level of stunting reflects the longstanding displacement and poor availability of and access to food in the IDP settings.
The stake holders (local governments and relief organizations) involved in provision of care and support to the IDPs in the camps should intensify efforts to improve the nutritional status of the entire IDPs especially children. The process of decongestion of the camps should be hastened so as to enable IDPs (caretakers) access and cultivate their land to have adequate foodstuff. Furthermore, emphasis should be put on effective management of fever in the IDP camps and provision of insecticide treated mosquito nets to mothers/caretakers with children under five years old.
Table 1.
Social demographic characteristics of the Caretakers
| Character | Frequency (N=672) | Percentage (%) |
| Age (years) | ||
| <20 | 43 | 6.4 |
| 20 – 30 | 363 | 54.0 |
| 31 – 40 | 192 | 28.6 |
| >40 | 74 | 11.0 |
| Sex | ||
| Female | 664 | 98.8 |
| Male | 8 | 1.2 |
| Marital status | ||
| Married | 502 | 74.7 |
| Not married | 170 | 25.3 |
| Level of education | ||
| None | 177 | 26.3 |
| Primary | 432 | 64.3 |
| Secondary and above | 63 | 9.4 |
| Source of income | ||
| Peasant farmers | 455 | 67.7 |
| Housewives | 121 | 18 |
| Others | 97 | 14.2 |
| Duration of stay in camps (years) | ||
| <2 | 63 | 9.4 |
| 2–4 | 507 | 75.4 |
| >5 | 102 | 15.2 |
Table 2.
Prevalence of acute and chronic malnutrition by age groups
| Population | Frequency | Acute malnutrition (W/H) | Chronic malnutrition (H/A) | ||||
| Age group (months) |
N | Severe n (%) |
Moderate n (%) |
Global n (%) |
Severe n (%) |
Moderate n (%) |
Global n (%) |
| 3 – 5 | 30 | - | 1 (3.3) | 1 (3.3) | 2 (6.7) | 9 (30) | 11 (36.7) |
| 6 – 12 | 275 | 4 (1.5) | 18 (6.5) | 22 (8.0) | 73 (26.5) | 79 (28.7) | 152 (55.3) |
| 13 – 24 | 175 | 2 (1.1) | 9 (5.1) | 11 (6.3) | 52 (29.7) | 45 (25.7) | 97 (55.4) |
| 25 – 36 | 119 | 2 (1.7) | 2 (1.7) | 4 (3.4) | 26 (21.8) | 35 (29.4) | 61 (51.3) |
| 37 – 48 | 60 | - | 1 (1.7) | 1 (1.7) | 13 (21.7) | 15 (25.0) | 28 (46.7) |
| 49 – 59 | 13 | 1 (7.7) | - | 1 (7.7) | 1 (7.7) | 2 (15.4) | 3 (23.1) |
| Total | 672 | 9 (1.3) | 31 (4.6) | 40 (6.0) | 167 (24.9) | 185 (27.5) | 352 (52.4) |
Keys:
Severe refers to <-3SD and / or bilateral edema; Moderate refers to a range from <-2SD to <-3SD/ absence of edema. Global refers to <-2SD
Table 3.
Prevalence of communicable diseases in children by age group
| Age group (months) | Freq | Diarrhea | Cough (RTI) | Fever (Malaria) | |||
| N | n | % | n | % | n | % | |
| 3 – 5 | 30 | 18 | 60.0 | 24 | 80.0 | 25 | 83.3 |
| 6 – 12 | 275 | 182 | 66.2 | 222 | 80.7 | 229 | 83.3 |
| 13 – 24 | 175 | 100 | 57.1 | 147 | 84.0 | 155 | 88.6 |
| 25 – 36 | 119 | 67 | 56.3 | 96 | 80.7 | 96 | 80.7 |
| 37 – 48 | 60 | 41 | 68.3 | 52 | 86.7 | 53 | 88.3 |
| 49 – 59 | 13 | 8 | 61.5 | 8 | 61.5 | 12 | 92.3 |
| Total | 672 | 416 | 61.9 | 547 | 81.7 | 570 | 84.8 |
RTI=Respiratory tract infection
Table 4.
Factors associated with acute and chronic malnutrition
| Acute malnutrition | |||||
| Variable Age group |
N | n (%) | OR | 95% CI | P - Value |
| 3 – 24 months | 425 | 31 (7.3) | 2.08 | 0.97 – 4.45 | 0.054 |
| 25 – 59 months | 247 | 9 (3.6) | |||
| Sex | |||||
| Male | 343 | 26 (7.6) | 1.85 | 0.95 – 3.60 | 0.069 |
| Female | 329 | 14 (4.3) | |||
| Feeding practices | |||||
| Breastfeeding | 253 | 18 (7.1) | 0.94 | 0.45 – 1.97 | 0.863 |
| Not breastfeeding | 172 | 13 (7.6) | |||
|
Age at complementary Feeding |
|||||
| <6months | 256 | 18 (7.0) | 0.88 | 0.41 – 1.89 | 0.747 |
| ≥ 6months | 152 | 12 (7.9) | |||
| Deworming last 3months | |||||
| No | 305 | 14 (4.6) | 0.49 | 0.24 – 1.04 | 0.058 |
| Yes | 193 | 17 (8.8) | |||
| Diarrhea | |||||
| Yes | 416 | 29 (7.0) | 1.67 | 0.82 – 3.40 | 0.155 |
| No | 256 | 11 (4.3) | |||
| Fever | |||||
| Yes | 570 | 39 (6.8) | 7.42 | 1.01 – 54.61 | 0.021* |
| No | 102 | 1 (1.0) | |||
| Cough | |||||
| Yes | 549 | 35 (6.4) | 1.61 | 0.62 – 4.19 | 0.328 |
| No | 123 | 5 (4.1) | |||
|
Chronic malnutrition Age group |
|||||
| 3 – 24 months | 425 | 234 (55.1) | 1.34 | 0.98 – 1.83 | 0.068 |
| 25 – 59 months | 247 | 118 (47.8) | |||
| Sex | |||||
| Male | 343 | 197 (57.4) | 1.52 | 1.12 – 2.05 | 0.007* |
| Female | 329 | 155 (47.1) | |||
| Feeding practices | |||||
| Breastfeeding | 253 | 139 (54.9) | 0.99 | 0.67 – 1.46 | 0.953 |
| Not breastfeeding | 172 | 95 (55.2) | |||
| Age at complementary Feeding | |||||
| <6months | 256 | 140 (54.7) | 0.93 | 0.62 – 1.39 | 0.710 |
| ≥6months | 152 | 86 (56.6) | |||
| Deworming last 3months | |||||
| No | 305 | 163 (53.4) | 0.96 | 0.67 – 1.38 | 0.834 |
| Yes | 193 | 105 (54.4) | |||
| Diarrhea | |||||
| Yes | 416 | 209 (50.2) | 0.80 | 0.58 – 1.09 | 0.157 |
| No | 256 | 143 (55.9) | |||
| Fever | |||||
| Yes | 570 | 294 (51.6) | 0.81 | 0.53 – 1.23 | 0.325 |
| No | 102 | 58 (56.9) | |||
| Cough | |||||
| Yes | 549 | 280 (51.0) | 0.74 | 0.49 – 1.09 | 0.130 |
| No | 123 | 72 (58.5) |
P-value is significant at ≤ 0.05
Table 5.
Factors associated with acute and malnutrition on logistic regression analysis
| Acute malnutrition Variable |
Adjusted OR | 95% CI | P-Value |
| Age group | |||
| 3–24 months | 2.78 | 1.26 – 6.15 | 0.012* |
| 25–59 months | |||
| Sex | |||
| Male/Female | 1.94 | 0.98 – 3.84 | 0.058 |
| Household head | |||
| Mother, other/father | 1.82 | 0.81 – 4.08 | 0.148 |
| Relationship with child | |||
| Other/father, mother | 1.58 | 0.55 – 4.56 | 0.400 |
| Evidence of deworming | |||
| No/Yes | 0.44 | 0.22 – 0.87 | 0.018* |
| Diarrhea | |||
| Yes/No | 1.28 | 0.61 – 2.68 | 0.507 |
| Fever | |||
| Yes/No | 6.51 | 0.87 – 48.87 | 0.068 |
|
Chronic malnutrition Major age group |
|||
| 3 – 24 | 1.37 | 0.99 – 1.88 | 0.052 |
| 25 – 59 | |||
| Sex | |||
| Male | 1.56 | 1.15 – 2.13 | 0.004* |
| Female | |||
| Diarrhea | |||
| Yes | 0.81 | 0.58 – 1.12 | 0.193 |
| No | |||
| Cough | |||
| Yes | 0.78 | 0.52 – 1.18 | 0.239 |
| No |
Acknowledgements
We thank the Ministry of Health (MoH) Nutrition Division, Gulu District Directorate of Health Services and District local authorities for the support during the study. We thank the IDP Camp leaders for the support to the Research team. We thank the parents and caretakers of the children who participated in the study. Finally we are grateful to Kulika Charitable Trust for the financial support towards the study.
References
- 1.Office of the Prime Minister (OPM), author Northern Uganda internally displaced persons profiling study: Department of Disaster Preparedness and Refugees. 2005. [Google Scholar]
- 2.Ministry of Health (MoH), author Northern Uganda: MoH/WHO study report. 2005. Health and mortality survey among internally displaced persons in Gulu, Kitgum and Pader districts. [Google Scholar]
- 3.Norwegian Refugee Council, author. Global overview in trends and development in 2005: Internal displacement monitoring centre. 2006. Mar, [Google Scholar]
- 4.MSF, author. An Approach to Emergency Situations. London: London & Basingstoke: Macmillan Press; 1997. Refugee Health. [Google Scholar]
- 5.Tambiah Y. Sexuality and Women's right in Armed Conflicts in Sri lanka. Sexuality, rights and social justice. Reproductive Health Matters. 2004;12:78–87. doi: 10.1016/s0968-8080(04)23121-4. [DOI] [PubMed] [Google Scholar]
- 6.Toole MJ, Waldman RJ. Refugees and displaced persons. War, hunger and public health. JAMA. 1993;270:600–605. [PubMed] [Google Scholar]
- 7.Hendrickse RG, Barr DGD, Matthews TS. Paediatrics in the Tropics. Oxford Blackwell Scientific Publication; 1991. [Google Scholar]
- 8.Uganda Demographic and Health Survey (UDHS), author Preliminary Report 2006/2007. pp. 22–23. [Google Scholar]
- 9.Onis M, Monteiro C, Akre J, et al. The world wide magnitude of protein energy malnutrition; an overview from the WHO Global Database on Child Growth. Bulletin of the World Health Organization. 1993;71:703–712. [PMC free article] [PubMed] [Google Scholar]
- 10.NCHS, author. United States Vital Statistics. 1977. Growth curves for children less than 18 years. [PubMed] [Google Scholar]
- 11.Uganda Bureau of Statistics (UBOS), author Uganda population and housing census report. 2002. [Google Scholar]
- 12.World Health Organisation (WHO), author Training for Mid-level Managers 1988. Geneva: WHO; 1988. Coverage Survey. WHO Expanded Programme on Immunisation. (WHO/EPI/MLM/COV/88) [Google Scholar]
- 13.ACF-USA, author. Nutrition survey report in IDP camps Gulu district, Northern Uganda: Action Against Hunger (ACF-USA) 2004. [Google Scholar]
- 14.ACF-USA, author. Field Report of nutritional assessment in IDPs, Gulu district northern Uganda. 2005. [Google Scholar]
- 15.WFP/UNICEF, author. Health and nutritional assessment in internally displaced people living in camps, Gulu district. 2005a. [Google Scholar]
- 16.WFP/UNICEF. WFP/UNICEF, author. Health and nutritional assessment of internally displaced persons living in camps in Kitgum district. 2005b. [Google Scholar]
- 17.Jitta M, Mudusu J. Determinants of malnutrition in the under fives in Uganda. Ministry of Health and Child Health Development Centre, Makerere University; 1992. [Google Scholar]
- 18.Vella V, Tomkins A, Borghesi A, Migliori GB, Adriko BC, Crevatin E. Determinants of child nutrition and mortality in north-west Uganda. Bull World Health Organ. 1992;70:637–643. [PMC free article] [PubMed] [Google Scholar]
- 19.Owor M, Tumwine JK, Kikafunda JK. Socio-economic risk factors for severe protein energy malnutrition among children in Mulago Hospital, Kampala. East Afr Med J. 2000;77:471–475. doi: 10.4314/eamj.v77i9.46691. [DOI] [PubMed] [Google Scholar]
- 20.Wamani H, Thorkid T, Nordrehaug A, et al. Mothers' education but not father's education, household assets or land ownership is the predictor of child health inequalities in rural Uganda. International Journal for Equity in Health. 2004;3(9) doi: 10.1186/1475-9276-3-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wamani H, Nordiehaug A, Stefan P, et al. Boys are more stunted than girls in Sub-Saharan Africa: a mete-analysis of 16 demographic and health surveys. BMC Paediatrics. 2007;(17) doi: 10.1186/1471-2431-7-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.United Nations Development Programme (UNDP), author Poverty and Human Development: Kampala report. 1998. Uganda Human Development Report; pp. 7–26. [Google Scholar]
- 23.Shears P, Berry AM, Murphy R, Nabil MA. Epidemiological assessment of the health and nutrition of Ethiopina refugees in emergency camps in Sudan 1985. Br Med J (Clin Res Ed) 1987;295:314–318. doi: 10.1136/bmj.295.6593.314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Orach GC. Morbidity and mortality amongst southern Sudanese in Koboko refugee camps, Arua district, Uganda. East African Medical Journal. 1999;74:195–1999. [PubMed] [Google Scholar]