Abstract
We reviewed clinical and billing data from a university-based health system to assess HPV vaccine utilization among 9–18-year-old girls by individual, visit and medical specialty characteristics. Our sample included 10,082 adolescent patients with 27,928 visits to outpatient family medicine (FM), pediatric and gynecology clinics between January 2007 and March 2008. Vaccine series completion was low among eligible adolescents (15%), with important disparities in vaccine utilization by medical specialty, age, race and insurance status. Missed opportunities for vaccination were common. Our findings may help to target future interventions aimed at increasing adolescent HPV vaccine utilization.
Keywords: Human papillomavirus, Adolescent, Vaccine
1. Introduction
Human papillomavirus (HPV) is a common sexually transmitted virus that causes cervical cancer, and genital warts and is linked to other anogenital and head and neck cancers. In 2006 a quadrivalent HPV vaccine was licensed in the U.S. [1]. Because the vaccine is only useful if provided prior to HPV exposure, which generally occurs at the onset of sexual activity [2], adolescents are the preferred target age for vaccination. Catch-up vaccination programs are recommended through young adulthood [3].
Data are beginning to emerge regarding adolescent utilization of the HPV vaccine. National estimates indicate that uptake among females ages 13–17 in 2007 was 25% for the first dose and 6.9% for completion of the 3 dose series [4]. Studies of smaller U.S. populations have found wide variation in uptake, ranging between 0.2% and 58% for series completion [5–8]. These data have begun informing our understanding of adolescent HPV vaccine utilization patterns, but a deeper understanding is needed to ensure that future interventions to increase HPV vaccine uptake are optimally developed. Defining populations with low utilization, clinical or physician factors associated with uptake, and the characteristics of visits that are missed opportunities for HPV vaccination are important for understanding what types of interventions might be most effective. In this study, we describe these aspects of HPV vaccine utilization during the first year of vaccine availability among adolescent girls seen in pediatric, family medicine or gynecology clinics within a university-based health system.
2. Methods
2.1. Study design and population
We retrospectively reviewed clinical visit data (medical records and billing data) from the University of Michigan Health System to capture all outpatient visits for females ages 9–18 years that occurred within the family medicine (FM), pediatric and gynecology clinics between January 1 2007 and March 31 2008. These three medical specialties were chosen as they provide the vast majority of primary care services (where immunizations are preferentially provided) to adolescents. These outpatient visits occurred at 20 university-affiliated outpatient clinics interspersed throughout southeast Michigan. The study initiation date was selected to coincide with the beginning of Michigan Medicaid coverage for HPV vaccine. Providers within this health system were made aware of this coverage through staff and clinical emails and notices. Most private insurers in the area also covered the vaccine at this time. The institution's immunization committee instructed providers to offer the vaccine to all age-eligible females (in accordance with national vaccine recommendations) beginning in January 2007. Adolescents who initiated the HPV series at age 18 but whose subsequent doses within the study period occurred at age 19 were also included in the study population. For six months during the study period, the FM clinics, but not other specialties, had automated computerized prompts to remind providers about HPV vaccination for eligible patients. (The effect of this automated intervention is reported in a separate manuscript.) All study activities were approved by the institutional review board at the University of Michigan.
2.2. Inclusion criteria
Qualifying visits were identified using Current Procedural Terminology (CPT) codes. Visits coded as outpatient visits (99383-5, 99393-5, 99201-5, and 99211-5) and/or vaccine administration (90649, 90471) were included in the study. Visits with diagnostic codes indicating pregnancy at the time of the visit were excluded. Internal validation demonstrated that this search strategy captured 98% of the HPV vaccine doses administered in the three medical specialties to qualifying females during the study period.
2.3. Variables
2.3.1. Outcome measures
Outcomes were measured at the patient, vaccine dose and visit level. Patient level analyses assessed the proportion of adolescent females appropriately receiving first, second and third doses of HPV vaccine. Vaccine dose-level analyses assessed the proportion of the HPV vaccine doses administered that were attributable to different patient or clinical characteristics.
Visit-level analyses assessed the proportion of visits that were missed opportunities for providing HPV vaccine. Missed opportunities were defined as visits where an HPV vaccine dose could have been provided, based on timing from any previous HPV vaccine doses, when applicable. To account for potential variation in vaccination practices we explored the proportion of visits that were missed opportunities for vaccination under four different scenarios. We evaluated the impact of defining missed opportunities using either the routine vaccination schedule (0, 2 and 6 month) or the “minimal interval” schedule (0, 4, 16 weeks) that existed at the time of the study (but has subsequently been modified) [9], and combined these strategies with two different definitions of missed opportunity visits. One required the vaccine to be given on the same day as the qualifying appointment and the other allowed a two-week window from the qualifying appointment for vaccine administration. Because results differed minimally among these 4 scenarios, we present data only from analyses using the routine immunization schedule and a two-week window for vaccine administration.
2.3.2. Independent variables
CPT and diagnostic (ICD-9) codes were used to classify visits as either “preventive”, “problem-focused” or “immunization-only”. Preventive visits included visits coded as (a) a “comprehensive exam” (99383–99385, 99393–99395); or (b) a level 3 or 4 office visit (99203–99204, 99213–99214) plus a Pap smear (Q0091, G0101) but no diagnostic code for “history of abnormal pap” (ICD-9 codes V13.22 or 795.0X); or (c) a level 3 or 4 office visit plus a diagnostic code specifying “routine gynecological visit” (ICD-9 V72.31). Problem-focused visits had “office visit” procedural codes (99201–99205, 99211–99215) with or without an immunization code. Immunization-only visits had a procedural code for immunization (90649 or 90471) but no associated office visit code.
Race designations were based on parent-report and were condensed to generate three race categories (African American, White, and other/not specified). Insurance specification was based on billing data with “public” insurance defined as patients with Medicaid-only billing, “no insurance” patients as those billed as “self pay” and/or “collection agency” without another identified billing source and “private/other” as patients with private and/or military insurance. For patients with >1 visit during the study period, race, age and insurance were defined using data from the first visit where an HPV vaccine dose was provided, or the first visit during the study period when no doses were administered. Age stratification corresponded to early HPV vaccination (9–10 years), routine vaccination (11–12 years), early catch up vaccination (13–15 years) and late catch up vaccination (16+ years).
2.4. Statistical analyses
The proportion of appropriately vaccinated females was determined by dividing the number of girls having received first, second or third HPV vaccine doses by the number of girls who would have been eligible for those doses, taking into account timing from previous doses when applicable (i.e. the recommended time interval from a previous dose was required to be considered eligible for second or third doses). The proportion of vaccine doses attributable to different patient and clinical factors was determined by dividing the number doses with a given characteristic by the total number doses, with separate analyses performed for first, second and third doses in the series. The proportion of missed opportunity visits was determined by dividing the number of missed opportunity visits by the total number of visits where a vaccine dose could have been/was administered. For each of these outcomes, analyses were further stratified by various patient or clinic characteristics, and chi-square tests assessed for any associations. Logistic regression analysis determined factors independently associated with HPV vaccine series initiation and included patient age, insurance type, race, visit type (immunization-only category eliminated from the analysis because of small cell size) and medical specialty, as these were the variables hypothesized a priori to be predictors of this outcome. Analyses were performed using a combination of SAS®, version 9.1 and STATA®, version 10 (Stata Corporation, College Stations, TX). A p-value of ≤0.05 was considered significant.
3. Results
3.1. Sample characteristics
There were 10,082 adolescent female patients in our sample who participated in 27,928 outpatient visits for the three medical specialties during the study period. Less than 1% of the sample was uninsured. A majority of visits occurred in pediatric clinics. Sample characteristics are described in Table 1.
Table 1.
Characteristics of sample by patient- and visit-level factors.
| Characteristics | % |
|---|---|
| Characteristics of patients (n = 10,082) at time of first qualifying visit | |
| Age | |
| 9–10 years | 24 |
| 11–12 years | 20 |
| 13–15 years | 29 |
| 16+ | 27 |
| Race | |
| White | 73 |
| African American | 14 |
| Other/not specified | 13 |
| Insurance | |
| Private/other | 78 |
| Public | 21 |
| No insurance | 1 |
| Characteristics of qualifying visits (n = 27,928) | |
| Medical specialty | |
| Pediatrics | 76 |
| Family medicine | 21 |
| Ob/Gyn | 3 |
| Visit type | |
| Preventive care | 20 |
| Problem-focused | 66 |
| Immunization-only | 14 |
3.2. Vaccine utilization among eligible girls
While only a minority of girls (28%) initiated the HPV series, more than three quarters of those who were eligible for second and third doses received them (Table 2). Of those completing the series, only 28% did so within the recommended 6-month time frame; 69% completed the series within 1 year of their first dose.
Table 2.
Overall HPV vaccination and factors associated with receipt of first, second and third doses of HPV vaccine.
| Vaccination among cohort overall | |||||||
|---|---|---|---|---|---|---|---|
| Dose 1 | Dose 2 | Dose 3 | |||||
| # Girls eligible to receive dose | 10,082 | 2,625 | 1,515 | ||||
| % Eligible girls vaccinated | 28% | 78% | 75% | ||||
| Vaccination by patient characteristics | |||||||
| Characteristic | % eligible girls vaccinated (n) | p-Value | % Eligible girls vaccinated (n) | p-Value | % Eligible girls vaccinated (n) | p-Value | |
| Ageb | |||||||
| 9–10 years | 2% (38) | <0.0001 | 74% (25) | 0.35 | 72% (13) | 0.34 | |
| 11–12 years | 32% (647) | 77% (461) | 74% (249) | ||||
| 13–15 years | 38% (1130) | 79% (829) | 77% (483) | ||||
| 16+ | 39% (1040) | 77% (723) | 73% (389) | ||||
| Race | |||||||
| White | 28% (2069) | <0.0001 | 82% (1562) | <.0001 | 77% (911) | <0.0001 | |
| African American | 34% (463) | 60% (252) | 61% (102) | ||||
| Other/not specified | 25% (323) | 76% (224) | 71% (121) | ||||
| Insurancea | |||||||
| Private | 27% (2094) | <0.0001 | 81% (1578) | <0.0001 | 78% (933) | <0.0001 | |
| Public | 35% (739) | 67% (446) | 63% (198) | ||||
| No insurance | 24% (22) | 70% (14) | 30% (3) | ||||
| Concurrently received other adolescent vaccinesc with HPV dose | |||||||
| Yes | 50% (1765) | <0.0001 | 78% (1263) | 0.56 | 74% (694) | 0.24 | |
| No | 17% (1090) | 77% (775) | 77% (440) | ||||
Similar patterns of statistical significance were obtained when individuals with no insurance were removed from the analysis.
Similar patterns of statistical significance were obtained when 9–10 year olds were removed from the analysis.
Tetanus–diphtheria–pertussis vaccine [Tdap] and meningococcal conjugate vaccine [MCV4].
Because many girls in our cohort had insufficient time in the study period to have received all three doses, we evaluated vaccine utilization specifically among a sub-population of 4712 girls who had ≥12 months from the time of their first qualifying visit in the study (regardless of whether any vaccine doses were given) and the end of the study period. Though this cohort had ample opportunity to both initiate and complete the vaccination series, only 15% of these girls received all three vaccine doses.
Several patient characteristics were associated with series initiation and/or completion (Table 2). There was a significant association between series initiation and age, but utilization of second and third doses was similar among all age groups. It was also notable that series initiation was most common, but series completion least common, among African Americans when compared other race groups, and among those with public health insurance versus private or no insurance. We repeated our analyses excluding 9–10-year olds (for the age analysis) or those with no insurance (for the insurance analysis) and found a similar pattern of statistical association with vaccine utilization (data not shown).
3.3. Vaccine utilization by visit type
There were statistically significant differences in utilization of each vaccine dose and the type of outpatient visit (Fig. 1). Series initiation most commonly occurred at preventive care visits, while second and third doses were most commonly provided at immunization-only visits.
Fig. 1.
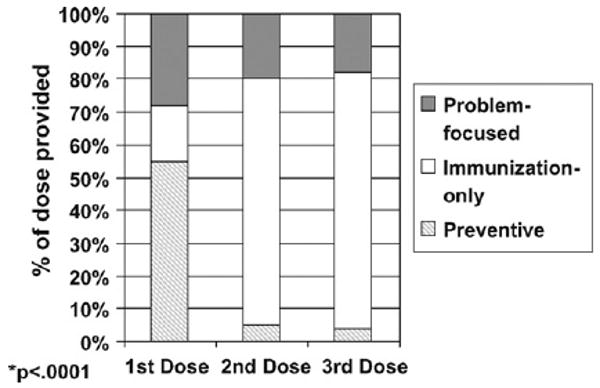
Comparison of first, second and third doses of HPV vaccine by visit type (*p < 0.0001).
There were additional associations when the visit-type analysis was further sub-divided by adolescent age (Fig. 2). Series initiation during preventive visits decreased, while series initiation at problem-focused visits increased, with increasing age. A similar pattern was seen for second and third HPV vaccine doses, except that the increases in problem-focused visit utilization with advancing age were accompanied by decreases in immunization-only, rather than preventive, visits (data not shown).
Fig. 2.
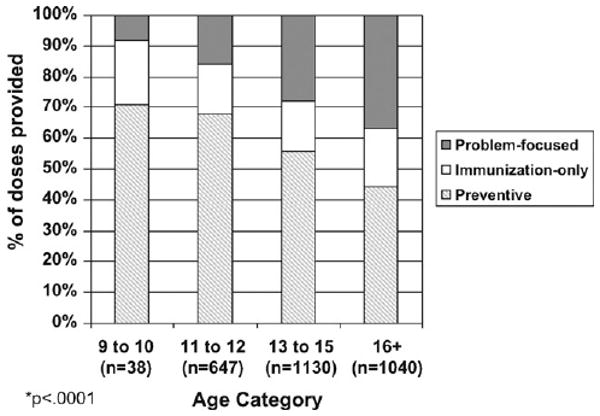
Types of visits for HPV vaccine series initiation, sub-divided by adolescent age group (*p < 0.0001).
Subdividing the visit-type analysis by race, we found that African American girls (66%) were more likely to initiate the vaccine series at preventive visits when compared to White (52%) or other/unknown race girls (58%, p < 0.0001). African American girls were also less likely than girls in the other race categories to use immunization-only appointments for subsequent doses, though this association was statistically significant only for the second dose (African American 64%, White 76% and other/unknown 77%, p = 0.04). Similarly, when the visit-type analysis was sub-divided by insurance status, we found that those with public insurance were significantly more likely to initiate the vaccine series at preventive care visits, and were significantly less likely to receive subsequent doses at immunization-only appointments, than those with private or no insurance (data not shown).
3.4. Vaccine utilization by medical specialty
Pediatricians and FM physicians initiated the vaccine series among eligible girls significantly more frequently (29% each) than gynecologists (17%, p < 0.0001). However, there were no statistically significant differences between the three medical specialties in administration of the second or third doses (data not shown).
When the medical specialty analysis was sub-divided by visit type, we found that pediatricians (59%) were significantly more likely than FM physicians (43%) or gynecologists (28%) to initiate the series at a preventive visit, and were the least likely to initiate the series at a problem-focused visit (24% pediatricians vs. 41% and 45% for FM and gynecologists, respectively, p < 0.0001). There were not statistically significant differences between the medical specialties when the analysis was sub-divided by visit type for second or third doses (data not shown).
We next evaluated vaccine utilization by medical specialty among each adolescent age strata. Pediatricians administered the majority of doses regardless of age, but there was a shift towards vaccination by gynecologists as adolescents aged. However, at most gynecologists administered only 2–6% of the vaccine provided (first dose, Table 3; other doses, data not shown).
Table 3.
Proportion of first doses of HPV vaccine attributable to each medical specialty, sub-divided by adolescent age*.
| Age category | Pediatrics (# doses) | Family medicine (# doses) | Gynecology (# doses) | Total # doses |
|---|---|---|---|---|
| 9–10 years | 74% (28) | 26% (10) | 0 (0) | 38 |
| 11–12 years | 85% (552) | 15% (94) | 0 (1) | 647 |
| 13–15 years | 77% (875) | 21% (235) | 2% (20) | 1130 |
| 16+ | 65% (677) | 29% (306) | 6% (57) | 1040 |
| Total # doses | 2,132 | 645 | 78 | 2855 |
p < 0.0001.
3.5. Independent predictors of HPV series initiation
In a multivariable model examining HPV series initiation (Table 4), we found that increasing age, having public insurance and attending a preventive visit were associated with a significantly increased odds of vaccine series initiation. Conversely, gynecology but not FM specialty was associated with a significantly decreased odds of initiating the vaccine series when compared to pediatrics.
Table 4.
Multivariable analysis of patient and clinic factors associated with HPV series initiationa.
| Variable | Odds ratio | 95% Confidence interval | p-Value |
|---|---|---|---|
| Race | |||
| White | Ref | – | – |
| Black | 1.06 | 0.91–1.24 | 0.4700 |
| Other/not specified | 0.78 | 0.66–0.93 | 0.0050 |
| Age | |||
| 9–10 | 0.03 | 0.02–0.05 | <0.0001 |
| 11–12 | Ref | – | – |
| 13–15 | 1.44 | 1.25–1.65 | <0.0001 |
| 16+ | 1.92 | 1.66–2.23 | <0.0001 |
| Insurance | |||
| Public | Ref | – | – |
| Private | 0.52 | 0.45–0.59 | <0.0001 |
| No insurance | 0.47 | 0.26–0.85 | 0.0124 |
| Medical specialty | |||
| Pediatrics | Ref. | – | – |
| Family medicine | 0.92 | 0.81–1.04 | 0.1981 |
| Gynecology | 0.24 | 0.18–0.33 | <0.0001 |
| Visit typeb | |||
| Problem-focused | Ref | – | – |
| Preventive | 5.18 | 4.64–5.79 | <0.0001 |
Adjusted for the factors listed in first column.
“Immunization-only” visits were eliminated from the analysis due to small cell sizes.
3.6. Missed opportunities for vaccination
Missed opportunities for vaccination were common, and were most prevalent among problem-focused visits, and for gynecologists (Table 5). However, gynecologists had significantly fewer missed opportunities at immunization-only appointments than the other medical specialties. Adolescents aged 11–12 years were significantly more likely to experience a missed opportunity visit than older adolescents, and this was particularly common at problem-focused visits. Receiving other adolescent vaccines concurrently with HPV was associated with decreased missed opportunities at problem-focused and preventive visits, but not at immunization-only appointments.
Table 5.
Factors associated with missed opportunities for HPV vaccination, overall and by visit type.
| % Qualifying visits that were missed opportunities for HPV vaccine administration | ||||
|---|---|---|---|---|
| Preventive | Problem-focused | Immunization-only | ||
| By visit type* | 62% | 89% | 18% | |
| Clinic/patient characteristic (total # visits)§ | All visit types combined | By visit type | ||
| Preventive | Problem-focused | Immunization-only | ||
| Specialty* | ||||
| Pediatrics (n = 15,915) | 71% | 60% | 89% | 17% |
| Family medicine (n = 5,040) | 73% | 66% | 87% | 24% |
| Gynecology (n = 879) | 81% | 84% | 93% | 2% |
| Race* | ||||
| White (n = 16,758) | 72% | 65% | 89% | 17% |
| African American (n = 2,610) | 68% | 50% | 86% | 15% |
| Other/not specified (n = 2,466) | 73% | 65% | 89% | 28% |
| Age at time of visita | ||||
| 11–12 (n = 5,560) | 77% | 66% | 93% | 28% |
| 13–15 (n = 5,809) | 70% | 61% | 88% | 16% |
| 16+ (n = 5,615) | 70% | 60% | 86% | 14% |
| Insurance at time of visit‡,† | ||||
| Private (n = 17,232) | 73% | 66% | 90% | 19% |
| Public (n = 3,034) | 68% | 48% | 84% | 14% |
| Concurrently received other adolescent vaccines at visit* | NS | |||
| Yes (n = 10,387) | 63% | 57% | 83% | 18% |
| No (n = 11,447) | 80% | 70% | 93% | 18% |
NS: not significant.
p < 0.0001.
p < 0.05.
Includes missed opportunity visits plus visits that were not missed opportunities.
9–10 year olds were eliminated from the analysis since routine HPV vaccination is recommended beginning at age 11 years.
Patients with no insurance were eliminated from the analysis due to small cell sizes.
4. Discussion
In this assessment of HPV vaccine utilization by adolescent girls during the first 15 months of vaccine availability within a university-based health system, we found that approximately one out of four girls had received at least one dose of the vaccine. Once the vaccination series was begun, there was a high likelihood that it would be completed, with more than 75% of girls eligible for second and third doses receiving them. However, the series completion rate for the adolescent cohort overall was quite low. Among a sub-population who had a full year to initiate and complete the vaccine series, only 15% received all three doses.
Two lines of evidence from our analysis suggested that series initiation was a critical step in the overall HPV vaccination process. First, we found that series initiation increased with age, but there were no age-related differences for second and third doses. Second, our analysis demonstrated that gynecologists were significantly less likely to initiate the series than other specialties, but that once the series was begun, they were similarly likely to deliver subsequent vaccine doses to their eligible patients. Our results suggest that focusing on increasing HPV series initiation may be an efficient target for future interventions to increase HPV vaccination overall among adolescents, particularly among 11–12 year olds, the preferred age for HPV vaccination, and in the gynecology setting, since vaccine initiation was substantially lower in these groups.
Many have hypothesized that a major barrier to high HPV vaccine uptake is convincing the adolescent to return for second and third doses [10]. This is a reasonable concern given that many teens will initiate the series during routine check-ups, as in our study, but may not be as willing to return to the medical setting solely for receiving second and third doses. However, the relatively high series completion rate among those initiating the series in our study suggests that, at least in some settings, returning to the office for subsequent doses may be less of a barrier than initially envisioned. Making use of immunization-only appointments, which we found to be the visit type associated with the majority of second and third doses, may be one way to facilitate completion of the series. In our institution, we encourage parents/patients make a follow-up “immunization” appointment for their daughter's next HPV dose at the time of the visit where the first (or second) dose was received. This practice may have contributed to the high utilization of “immunization-only” appointments for second and third doses in our study. Completing the series is obviously important, as there is no evidence that one or two doses confers protection against HPV infection. Given this, the financial implications for insurers and parents of initiating, but not completing, the costly HPV series are considerable.
Our results also highlight important disparities in HPV vaccine utilization. We found that African Americans and those on public health insurance were less likely than those of other races or those with private health insurance to complete the HPV series. Similar results were described in a smaller study that assessed HPV vaccination among 352 adolescents age <21 years [6]. These race- and insurance-based disparities are disturbing given that the risk of developing and dying from cervical cancer is highest among underserved minorities and those of low socioeconomic status [11,12]. If this utilization pattern were widespread, our results raise questions about whether the HPV vaccine is being delivered to populations most in need of this preventive intervention. Furthermore, modeling studies suggest that HPV vaccination may no longer be cost effective if there is preferential utilization of cervical cancer screening programs among those who were vaccinated against HPV [13]. Additional studies are needed to confirm whether the race- and insurance-based disparities in HPV series completion found in this study are prevalent over a wider geographic area. A limitation of our study was that vaccine doses provided in other settings (i.e. health departments) were not captured in our analyses; these types of alternative vaccination venues are likely differentially utilized by various socio-demographic groups.
As has been found for other adolescent vaccines [14], missed opportunities for providing HPV vaccine doses were common in our study. This was most apparent for problem-focused visits in our study, but there was also a high proportion (60%) of missed opportunity visits among preventive visits, which are the visit type most associated with vaccination [15–17]. Gynecologists had the highest proportion of missed opportunity visits overall, but had substantially fewer missed opportunity immunization-only appointments than the other medical specialties. This latter finding likely reflects the unique vaccination practices of gynecology clinics which tend to offer only select vaccines (e.g. HPV, Tdap and influenza) and have a more targeted approach to immunization (e.g. Tdap primarily for post-partum mothers) [18]. Adolescent patients presenting for immunization-only appointments in the gynecology setting would therefore be more likely to receive HPV vaccine than immunization-only appointments in pediatrics or FM, where other adolescent-targeted vaccines besides HPV could be provided. In addition, gynecologists within our health system see relatively few adolescent patients for routine gynecologic care. Because of this, gynecology clinics had less experience in administering vaccines to this age group, which likely contributed to the overall lower administration of adolescent HPV vaccine than other specialties in our study. However, regardless of the reasons behind differences in care patterns, the high level of missed opportunities across specialties, visit types and adolescent characteristics points to the need to find mechanisms to effectively reduce this occurrence. Suggested modalities include the use of standing orders, automated prompts and reminder/recall systems, which have been shown in clinical trials to be effective, but are not widely utilized in the U.S. [19].
4.1. Limitations
Our study findings should be interpreted in the context of several limitations. First, our study population was limited to one university-based health system located in Michigan, and therefore our results may not be generalizable to patients seen in other medical settings or geographic locations. This may be true especially for results from gynecology visits since only a small proportion of adolescents in our sample were seen by gynecologists, which is in contrast to national adolescent health care utilization patterns [20]. Second, our sample included very few adolescents categorized as being without health insurance, which does not reflect adolescent insurance coverage levels nationally [21], and could have resulted in higher than average vaccine utilization. Third, though we used well accepted methods to classify visit types and patient characteristics, it is possible that some of these characteristics were misclassified [22]. Fourth, our analysis did not evaluate HPV vaccine utilization among females >18 years, which are a important component of “catch up” HPV vaccination strategies and where there may be substantially different patterns of utilization than that found in our study. Fifth, our analysis captured only those vaccine doses provided within our University's health system. It is possible that some adolescents received HPV vaccine doses in other settings that could not be quantified in our study. However, internal audits of our patient population suggest that the majority of pediatric patients receive all of their primary care services (where immunizations tend to be provided) within our health setting. Finally, we were not able to ascertain from our study the reasons why vaccination did not occur at some visits. Although it was university policy at the time to offer the vaccine to all eligible females, it is unknown whether provider variability in these recommendations occurred, or how this might have impacted our results.
5. Conclusions
In one of the first studies to assess adolescent vaccine utilization patterns in depth, we found that overall uptake by the eligible cohort was low, but for girls who did initiate the vaccine series, there was a relatively high likelihood that they would receive all three doses. Younger adolescents and those seen by gynecologists had lower series initiation than their comparative groups. However, they had comparable series completion rates once they received the first dose, suggesting that series initiation was a critical step in the overall HPV vaccination process. We found disparities in series completion by race and insurance statues, raising questions about the degree to which HPV vaccination will impact cervical cancer rates in the U.S. Our results suggest that continued outreach to adolescents is needed in order to improve HPV vaccination, and that particular efforts to increase vaccination among underserved minorities, those who are socio-economically disadvantaged, and pre-adolescents (11–12-year olds) are needed.
Footnotes
Financial disclosures: Amanda F. Dempsey serves on an advisory board for Merck.
References
- 1.U.S. Food and Drug Administration. Product Approval Information—Licensing Action, Gardasil. 2006 [cited August 1, 2006]; Available from: http://www.fda.gov/cber/products/hpvmer060806qa.htm.
- 2.Winer RL, Feng Q, Hughes JP, O'Reilly S, Kiviat NB, Koutsky LA. Risk of female human papillomavirus acquisition associated with first male sex partner. J Infect Dis. 2008 January;197(2):279–82. doi: 10.1086/524875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Markowitz LE, Dunne EF, Saraiya M, Lawson HW, Chesson H, Unger ER. Quadrivalent human papillomavirus vaccine: recommendations of the Advisory Committee on Immunization Practices (ACIP) MMWR Recomm Rep. 2007 March;56(RR-2):1–24. [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. Vaccination coverage among adolescents aged 13–17 years—United States, 2007. Morb Mortal Wkly Rep. 2008 October;57(40):1100–3. [PubMed] [Google Scholar]
- 5.Chao C, Slezak JM, Coleman KJ, Jacobsen SJ. Papanicolaou screening behavior in mothers and human papillomavirus vaccine uptake in adolescent girls. Am J Public Health. 2009 June;99(6):1137–42. doi: 10.2105/AJPH.2008.147876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Neubrand TP, Breitkopf C Radecki, Rupp R, Brieitkopf D, Rosenthal SL. Factors associated with completion of the human papillomavirus vaccine series. Clin Pediatr (PL) 2009 doi: 10.1177/0009922809337534. Epub May 29. [DOI] [PubMed] [Google Scholar]
- 7.Kahn JA, Rosenthal SL, Jin Y, Huang B, Namakydoust A, Zimet GD. Rates of human papillomavirus vaccination, attitudes about vaccination, and human papillomavirus prevalence in young women. Obstet Gynecol. 2008 May;111(5):1103–10. doi: 10.1097/AOG.0b013e31817051fa. [DOI] [PubMed] [Google Scholar]
- 8.Rosenthal SL, Rupp R, Zimet GD, Meza HM, Loza ML, Short MB, et al. Uptake of HPV vaccine: demographics, sexual history and values, parenting style, and vaccine attitudes. J Adolesc Health. 2008 September;43(3):239–45. doi: 10.1016/j.jadohealth.2008.06.009. [DOI] [PubMed] [Google Scholar]
- 9.American Academy of Pediatrics Committee on Infectious Diseases. Prevention of human papillomavirus infection: provisional recommendations for immunization of females with quadrivalent human papillomavirus vaccine. Pediatrics. 2007;120(3):666–8. doi: 10.1542/peds.2007-1735. [DOI] [PubMed] [Google Scholar]
- 10.Dempsey AF, Davis MM. Overcoming barriers to adherence to HPV vaccination recommendations. Am J Manage Care. 2006 December;12(17 Suppl):S484–91. [PubMed] [Google Scholar]
- 11.Garner EI. Cervical cancer: disparities in screening, treatment, and survival. Cancer Epidemiol Biomarkers Prev. 2003 March;12(3):242s–7s. [PubMed] [Google Scholar]
- 12.Wang SS, Sherman ME, Hildesheim A, Lacey JV, Jr, Devesa S. Cervical adenocarcinoma and squamous cell carcinoma incidence trends among white women and black women in the United States for 1976–2000. Cancer. 2004 March;100(5):1035–44. doi: 10.1002/cncr.20064. [DOI] [PubMed] [Google Scholar]
- 13.Kim JJ, Goldie SJ. Health and economic implications of HPV vaccination in the United States. N Engl J Med. 2008 August;359(8):821–32. doi: 10.1056/NEJMsa0707052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lee GM, Lorick SA, Pfoh E, Kleinman K, Fishbein D. Adolescent immunizations: missed opportunities for prevention. Pediatrics. 2008 October;122(4):711–7. doi: 10.1542/peds.2007-2857. [DOI] [PubMed] [Google Scholar]
- 15.Halpern-Felsher BL, Ozer EM, Millstein SG, Wibbelsman CJ, Fuster CD, Elster AB, et al. Preventive services in a health maintenance organization: how well do pediatricians screen and educate adolescent patients? Arch Pediatr Adolesc Med. 2000 February;154(2):173–9. doi: 10.1001/archpedi.154.2.173. [DOI] [PubMed] [Google Scholar]
- 16.Kottke TE, Solberg LI, Brekke ML, Cabrera A, Marquez MA. Delivery rates for preventive services in 44 midwestern clinics. Mayo Clin Proc. 1997 June;72(6):515–23. doi: 10.4065/72.6.515. [DOI] [PubMed] [Google Scholar]
- 17.Schaffer SJ, Humiston SG, Shone LP, Averhoff FM, Szilagyi PG. Adolescent immunization practices: a national survey of US physicians. Arch Pediatr Adolesc Med. 2001 May;155(5):566–71. doi: 10.1001/archpedi.155.5.566. [DOI] [PubMed] [Google Scholar]
- 18.Gonik B, Fasano N, Foster S. The obstetrician–gynecologist's role in adult immunization. Am J Obstet Gynecol. 2002 October;187(4):984–8. doi: 10.1067/mob.2002.128027. [DOI] [PubMed] [Google Scholar]
- 19.Briss PA, Rodewald LE, Hinman AR, Shefer AM, Strikas RA, Bernier RR, et al. Reviews of evidence regarding interventions to improve vaccination coverage in children, adolescents, and adults. The Task Force on Community Preventive Services. Am J Prev Med. 2000 January;18(1 Suppl):97–140. doi: 10.1016/s0749-3797(99)00118-x. [DOI] [PubMed] [Google Scholar]
- 20.Rand CM, Shone LP, Albertin C, Auinger P, Klein JD, Szilagyi PG. National health care visit patterns of adolescents: implications for delivery of new adolescent vaccines. Arch Pediatr Adolesc Med. 2007 March;161(3):252–9. doi: 10.1001/archpedi.161.3.252. [DOI] [PubMed] [Google Scholar]
- 21.Newacheck PW, Park MJ, Brindis CD, Biehl M, Irwin CE., Jr Trends in private and public health insurance for adolescents. JAMA. 2004 March;291(10):1231–7. doi: 10.1001/jama.291.10.1231. [DOI] [PubMed] [Google Scholar]
- 22.HEDIS 2002 Guidelines. 2002 [cited November 4th, 2008]; Available from: http://www.ncqa.org/Programs/HEDIS.


