Abstract
This article is one of ten reviews selected from the Yearbook of Intensive Care and Emergency Medicine 2010 (Springer Verlag) and co-published as a series in Critical Care. Other articles in the series can be found online at http://ccforum.com/series/yearbook. Further information about the Yearbook of Intensive Care and Emergency Medicine is available from http://www.springer.com/series/2855.
Introduction
Venous oxygen saturation is a clinical tool which integrates the whole body oxygen uptake-to-delivery (VO2-DO2) relationship. In the clinical setting, in the absence of pulmonary artery catheter (PAC)-derived mixed venous oxygen saturation (SvO2), the central venous oxygen saturation (ScvO2) is increasingly being used as a reasonably accurate surrogate [1]. Central venous catheters (CVCs) are simpler to insert, and generally safer and cheaper than PACs. The CVC allows sampling of blood for measurement of ScvO2 or even continuous monitoring if an oximetry catheter is being used. The normal range for SvO2 is 68 to 77% and ScvO2 is considered to be 5% above these values [2].
A decrease in hemoglobin (Hb, g/dl) is likely to be associated with a decrease in DO2 when cardiac output (CO) remains unchanged, since DO2 = CO × CaO2, where CaO2 is arterial oxygen content and is ≈ Hb × SaO2 × 1.34 (where SaO2 is the arterial oxygen saturation in%; and 1.34 is the oxygen-carrying capacity of Hb in mlO2/g Hb), when one ignores the negligible oxygen not bound to Hb [1]. A decrease in Hb is one of the four determinants responsible for a decrease in SvO2 (or ScvO2), alone or in combination with hypoxemia (decrease in SaO2), an increase in VO2 without a concomitant increase in DO2, or a fall in cardiac output.
When DO2 decreases, VO2 is maintained (at least initially) by an increase in oxygen extraction (O2ER) since O2ER = VO2/DO2. As VO2 ≈ (SaO2 - SvO2) × (Hb × 1.34 × CO) and DO2 ≈ SaO2 × Hb × 1.34 × CO, O2ER and SvO2 are thus linked by a simple equation: O2ER ≈ (SaO2 - SvO2)/SaO2 or even simpler: O2ER ≈ 1 - SvO2. Assuming SaO2 = 1 [3], if SvO2 is 40%, then O2ER is 60%.
Because it integrates Hb, cardiac output, VO2 and SaO2, the venous oxygen saturation therefore helps to assess the VO2-DO2 relationship and tolerance to anemia during blood loss.
Venous oxygen saturation as a physiologic transfusion trigger
When DO2 decreases beyond a certain threshold, it induces a decrease in VO2. This point is known as the critical DO2 (DO2crit), below which there is a state of VO2-DO2 dependency also called tissue dysoxia. In humans, dysoxia is usually present when SvO2 falls below a critical 40-50% (SvO2crit); this may, however, also occur at higher levels of SvO2 when O2ER is impaired. Usually efforts in correcting cardiac output (by fluids or inotropes), and/or Hb and/or SaO2 and/or VO2 must target a return of SvO2 (ScvO2) from 50 to 65-70% [4]. In sedated critically ill patients in whom life support was discontinued, the DO2crit was found to be approximately 3.8 to 4.5 mlO2/kg/min for a VO2 of about 2.4 mlO2/g/min; O2ER reached an O2ERcrit of 60% [5] with SvO2crit being ≈ 40%.
In a landmark study by Rivers et al. [6], patients admitted to an emergency department with severe sepsis and septic shock were randomized to standard therapy (aiming for a central venous pressure [CVP] of 8-12 mmHg, mean arterial pressure (MAP) ≥ 65 mmHg, and urine output ≥ 0.5 ml/kg/h) or to early goal-directed therapy where, in addition to the previous parameters, an ScvO2 of at least 70% was targeted by optimizing fluid administration, keeping hematocrit ≥ 30%, and/or giving dobutamine to a maximum of 20 μg/kg/min. The initial ScvO2 in both groups was low (49 ± 12%), suggesting a hypodynamic condition before resuscitation was started. From the 1st to the 7th hour, the amount of fluid received was significantly larger in the early goal-directed therapy patients (≈ 5,000 ml vs 3,500 ml, p < 0.001), fewer patients in the early goal-directed therapy group received vasopressors (27.4 vs 30.3%, p = NS), and significantly more patients were treated with dobutamine (13.7 vs 0.8%, p < 0.001). It is noticeable that the number of patients receiving red blood cells (RBCs) was significantly larger in the early goal-directed therapy group than in the control group (64.1 vs 18.5%) suggesting that the strategy of targeting a ScvO2 of at least 70% was associated with more decisions to transfuse once fluid, vasopressors, and dobutamine had been titrated to improve tissue oxygenation. In the follow-up period between the 7th and the 72nd hour, mean ScvO2 was higher, mean arterial pH was higher, and plasma lactate levels and base excess were lower in patients who received early goal-directed therapy. Organ failure score and mortality were significantly different in patients receiving standard therapy compared to early goal-directed therapy patients. This was the first study to demonstrate that initiation of early goal-directed therapy to achieve an adequate level of tissue oxygenation by DO2 (as judged by ScvO2 monitoring) could significantly reduce mortality.
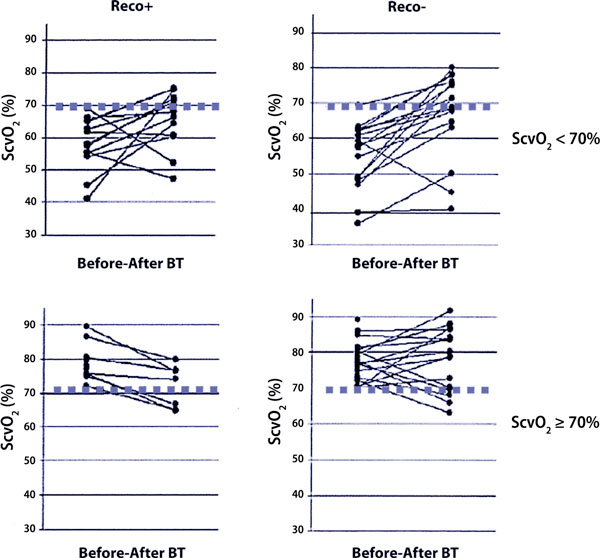
In a prospective observational study [7], we tested how well the ScvO2 corresponded to the French recommendations for blood transfusion and to the anesthesiologist's decision to transfuse. The French recommendations for blood transfusion were presented during a consensus conference organized in 2003 by the French Society of Intensive Care Medicine (Société de Réanimation de Langue Française, SRLF) [8]. These recommendations are based on plasma Hb concentration and associated clinical state (Table 1), and apart from in cardiac and septic patients, the threshold Hb value for blood transfusion is 7 g/dl. Sixty high risk surgical patients in whom the need for a blood transfusion was discussed postoperatively were included in the study [7]. They were eligible for study inclusion if they were hemodynamically stable and equipped with a CVC. The decision to transfuse was taken by the anesthesiologist in charge of the patient. The anesthesiologist was aware of the SRLF recommendations; if requested, he/she was provided with the ScvO2 value that was obtained at the same time as the blood was sampled for the Hb concentration. The following parameters were registered: Age, a history of cardiovascular disease, presence of sepsis, number of blood units transfused, agreement with the SRLF recommendations. A decision to transfuse was made in 53 of the 60 general and urologic surgical patients. ScvO2 and Hb were measured before and after blood transfusion, together with hemodynamic parameters (heart rate, systolic arterial pressure). Patients were retrospectively divided into two groups according to the ScvO2 before blood transfusion (< or = 70%); each of these groups was further divided into two groups according to agreement or not with the SRLF recommendations for blood transfusion. The ScvO2 threshold value of 69.5% (sensitivity 82%; specificity 76%) was validated with a receiver operator characteristic (ROC) curve analysis (Figure 1).
Table 1.
The French recommendations for blood transfusion in critically ill patients are based on a recent consensus by the French Society of Intensive Care Medicine (Société de Réanimation de Langue Française; SRLF) using threshold values for hemoglobin (Hb) together with the clinical context to indicate blood transfusion [8].
| Threshold value of Hb (g/dl) | Clinical context |
|---|---|
| 10 | • Acute coronary syndrome |
| 9 | • Ischemic heart disease |
| • Stable heart failure | |
| 8 | • Age > 75 |
| • Severe sepsis | |
| 7 | • Others |
Figure 1.
ROC curve analysis illustrating the usefulness of ScvO2 measurement before blood transfusion in order to predict a minimal 5% increase in ScvO2 after BT. The threshold value for ScvO2 with the best sensitivity and best specificity was 69.5% (*sensitivity: 82%, specificity: 76%; area under the curve: 0.831 ± 0.059). Adapted from [7] with permission.
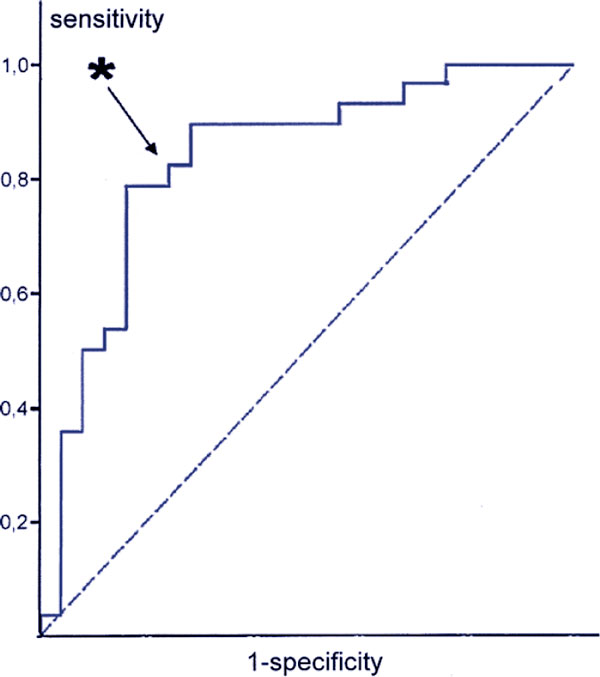
Overall, demographic characteristics were similar (age, weight, number of blood units transfused) among the groups. Blood transfusion provided a significant and approximately similar increase in hemoglobin concentration for all patients in the four groups but the ScvO2 value increased significantly only in patients with ScvO2 < 70% before blood transfusion (Figure 2 and Table 2). The heart rate and systolic arterial pressure did not help in the decision to transfuse.
Figure 2.
Individual evolutions in ScvO2 before and after blood transfusion (BT) according to agreement (Reco+) or not (Reco-) with the SRLF recommendations for transfusion and according to the ScvO2 before transfusion (< or ≥ 70%). Adapted from [7] with permission.
Table 2.
Central venous O2 saturation (ScvO2), hemoglobin (Hb), heart rate (HR) and systolic arterial pressure (SAP) values (median [CI 95%]) in 53 hemodynamically stable postoperative patients who received blood transfusion (BT), divided into two groups according to their ScvO2 before blood transfusion (< or ≥ 70%); and then into four groups according to agreement or not with the SRLF recommendations for transfusion.
| ScvO2 < 70% | ScvO2 ≥ 70% | ||||
|---|---|---|---|---|---|
| SRLF recommendations | Yes (n = 15) | No (n = 13) | Yes (n = 18) | No (n = 7) | Kruskal-Wallis test (p < .05) |
| ScvO2 preBT | 57.4 [48.2-62.0] | 58.0 [55.3-65.0] | 76.9 [72.0-80.8] | 75.7 [75.0-86.4] | p < 0.001 |
| ScvO2 postBT | 68.7* [63.0-75.6] | 67.8* [60.7-72.0] | 78.7 [70.0-84.2] | 74,0* [65.0-76.7] | p < 0.01 |
| Hb preBT | 7.4 [7.1-7.9] | 7.8 [7.4-8.7] | 7.5 [7.3-8.1] | 8.1 [7.5-8.2] | Ns |
| Hb postBT | 9.4** [8.7-9.7] | 10.0** [9.4-10.6] | 10.1** [9.3-10.6] | 9.8* [9.4-10.7] | Ns |
| HR preBT | 88 [78-90] | 96 [93-120] | 92 [85-105] | 95 [81-112] | Ns |
| HR postBT | 92 [84-97] | 95 [89-100] | 89 [78-104] | 96 [78-100] | Ns |
| SAP preBT | 118 [101-141] | 130 [120-150] | 128 [114-150] | 130 [124-151] | Ns |
| SAP postBT | 133 [119-140] | 120 [106-140] | 141* [128-161] | 140* [133-175] | p = 0.047 |
Ns: non-significant; * p < 0.05; **p < 0.01; Wilcoxon test for values before (preBT) vs after transfusion (postBT). Adapted from [7]
The conclusions of this observational study were as follows: 1) Twenty of the 53 patients (37.7%) received a blood transfusion against SRLF recommendations; 2) thirteen of these 20 patients (65%) had an ScvO2 < 70% and nevertheless seemed to benefit from the blood transfusion (according to the VO2/DO2 relationship), and one may speculate that the fact that they did not comply with the SRLF recommendations for blood transfusion could have contributed to a "lack of blood transfusion" in these patients; indeed, according to the ScvO2 (which remained largely below 70%) blood transfusion may even have been insufficient (n = 2 blood units) in this subgroup; 4) 54.5% of the patients (18/33) met the SRLF recommendation had an ScvO2 = 70% and received a blood transfusion although VO2/DO2 may have been adequate; one may speculate that transfusion in these patients could have contributed to an "excess of blood transfusion".
Following the study by Rivers et al. [6] and our own observations [7] we can conclude that ScvO2 appears to be an interesting parameter to help with transfusion decisions in hemodynamically unstable patients with severe sepsis or in stable high-risk surgical patients equipped with a CVC. ScvO2 can be proposed as a simple and universal physiologic transfusion trigger. This suggestion merits a controlled randomized study in which patients would be separated into two treatment groups: 1) A control group in which the decision to transfuse would be made according to Hb threshold values (similar to those presented by the SRLF); 2) an ScvO2 goal-directed group in which the decision to transfuse would be made according to an ScvO2 value < 70% as soon as the Hb value was less than 10 g/dl (hematocrit < 30%) providing that the CVP was 8 to 12 mmHg.
The concept of physiologic transfusion trigger
In an 84-year-old male Jehovah's Witness undergoing profound hemodilution, the DO2crit was 4.9 mlO2/kg/min for a VO2 of about 2.4 mlO2/kg/min; the Hb value at the DO2crit was 3.9 g/dl [9]. This Hb value can be defined as the critical Hb value. Consistent with these results, in young, healthy, and conscious (which means higher VO2) volunteers undergoing acute hemodilution with 5% albumin and autologous plasma, DO2crit was found to be less than 7.3 mlO2/kg/min for a VO2 of 3.4 mlO2/kg/min [10] and an Hb value of 4.8 g/dl. The same investigators studied healthy resting humans to test whether acute isovolemic reduction of blood hemoglobin concentration to 5 g/dl would produce an imbalance in myocardial oxygen supply and demand, resulting in myocardial ischemia [11]. Heart rate increased from 63 ± 11 (baseline measured before hemodilution began) to 94 ± 14 beats/min (a mean increase of 51 ± 27%; p < 0.0001), whereas MAP decreased from 87 ± 10 to 76 ± 11 mmHg (a mean decrease of 12 ± 13%; p < 0.0001), mean diastolic blood pressure decreased from 67 ± 10 to 56 ± 10 mmHg (a mean decrease of 15 ± 16%; p < 0.0001), and mean systolic blood pressure decreased from 131 ± 15 to 121 ± 16 mmHg (a mean decrease of 7 ± 11%; p = 0.0001). Electrocardiographic (EKG) changes were monitored continuously using a Holter EKG recorder for detection of myocardial ischemia. During hemodilution, transient, reversible ST-segment depression developed in three asymptomatic subjects at hemoglobin concentrations of 5 g/dl. The subjects who had EKG ST-segment changes had significantly higher maximum heart rates (110 to 140 beats/min) than those without EKG changes, despite having similar baseline values. The higher heart rates that developed during hemodilution may have contributed to the development of an imbalance between myocardial oxygen supply and demand resulting in EKG evidence of myocardial ischemia. An approach to the myocardial oxygen balance is offered by the product systolic arterial pressure × heart rate which should remain below 12,000. For heart rate = 110 beats/min, if systolic arterial pressure is 120 mmHg, systolic arterial pressure × heart rate = 13,200 and may be considered too high for the myocardial VO2.
In 20 patients older than 65 years and free from known cardiovascular disease, Hb was decreased from 11.6 ± 0.4 to 8.8 ± 0.3 g/dl [12]. With stable filling pressures, cardiac output increased from 2.02 ± 0.11 to 2.19 ± 0.10 l/min/m2 (p < 0.05) while systemic vascular resistance (SVR) decreased from 1796 ± 136 to 1568 ± 126 dynes/s/cm5 (p < 0.05) and O2ER increased from 28.0 ± 0.9 to 33.0 ± 0.8% (p < 0.05) resulting in stable VO2 during hemodilution. While no alterations in ST segments were observed in lead II, ST segment deviation became slightly less negative in lead V5 during hemodilution, from -0.03 ± 0.01 to -0.02 ± 0.01 mV (p < 0.05). The authors concluded that isovolemic hemodilution to a hemoglobin value of about 8.8 g/dl was the limit that could be tolerated in these patients [12].
In 60 patients with coronary artery disease receiving chronic beta-adrenergic blocker treatment and scheduled for coronary artery bypass graft (CABG) surgery, Hb was decreased from 12.6 ± 0.2 to 9.9 ± 0.2 g/dl (p < 0.05) [13]. With stable filling pressures, cardiac output increased from 2.05 ± 0.05 to 2.27 ± 0.05 l/min/m2 (p < 0.05) and O2ER from 27.4 ± 0.6 to 31.2 ± 0.7% (p < 0.05), resulting in stable VO2. No alterations in ST segments were observed in leads II and V5 during hemodilution. Individual increases in cardiac index and O2ER were not linearly related to age or left ventricular ejection fraction [13].
Healthy young volunteers were also tested with verbal memory and standard computerized neuropsychologic tests before and twice after acute isovolemic reduction of their Hb concentration to 5.7 ± 0.3 g/dl [14]. Heart rate, MAP, and self-assessed sense of energy were recorded at the time of each test. Reaction time for Digit-Symbol Substitution Test (DSST) increased, delayed memory was degraded, MAP and energy level decreased, and heart rate increased (all p < 0.05). Increasing PaO2 to 406 ± 47 mmHg reversed the DSST result and the delayed memory changes to values not different from those at the baseline Hb concentration of 12.7 ± 1.0 g/dl, and decreased heart rate (p < 0.05) although MAP and energy level changes were not altered with increased PaO2 during acute anemia. In that study, the authors confirmed that acute isovolemic anemia subtly slows human reaction time, degrades memory, increases heart rate, and decreases energy levels [14].
Subsequent studies identified the cause of the observed cognitive function deficits in impaired central processing as quantified by measurement of the P300 latency. The P300 response was significantly prolonged when unmedicated healthy volunteers were hemodiluted from hemoglobin concentrations of 12.4 ± 1.3 to 5.1 ± 0.2 g/dl [15]. The increased P300 latencies could be reversed to values not significantly different from baseline when inspired oxygen concentration was increased from 21 (room air) to 100%. These results suggest that P300 latency is a variable that is sensitive enough to predict subtle changes in cognitive function. Accordingly, increase in the P300 latency above a certain threshold may serve as a monitor of inadequate cerebral oxygenation and as an organ-specific transfusion trigger in the future. Spahn and Madjdpour recently commented [16] that Weiskopf et al. [15,17] have opened a "window to the brain" with respect to monitoring the adequacy of cerebral oxygenation during acute anemia.
These observations and results clearly indicate that there is no 'universal' Hb threshold that could serve as a reliable transfusion trigger and that transfusion guide lines should take into account the patient's individual ability to tolerate and to compensate for the acute decrease in Hb concentration. Useful transfusion triggers should rather consider signs of inadequate tissue oxygenation that may occur at various hemoglobin concentrations depending on the patient's underlying disease(s) [18].
Conclusion
Physiologic transfusion triggers should progressively replace arbitrary Hb-based transfusion triggers [19]. The same conclusions were drawn by Orlov et al. in a recent trial using a global oxygenation parameter for guiding RBC transfusion in cardiac surgery [20]. The use of goal-directed erythrocyte transfusions should render the management of allogeneic red cell use more efficient and should help: 1) in saving blood and avoiding unwanted adverse effects; and 2) in promoting and optimizing the adequacy of this life-saving treatment [16]. These 'physiologic' transfusion triggers can be based on signs and symptoms of impaired global (lactate, SvO2 or ScvO2) or, even better, regional tissue (EKG ST-segment, DSST or P300 latency) oxygenation; they do, however, have to include two important simple hemodynamic targets: heart rate and MAP or systolic arterial pressure.
Abbreviations
BT: blood transfusion; CO: cardiac output; CVC: central venous catheter; CVP: central venous pressure; EKG: electrocardiographic; Hb: hemoglobin; O2ER: oxygen extraction; MAP: mean arterial pressure; PAC: pulmonary artery catheter; RBC: red blood cell; ROC: receiver operator characteristic; SaO2: arterial oxygen saturation; ScvO2: central venous oxygen saturation; SvO2: mixed venous oxygen saturation; VO2-DO2: whole body oxygen uptake-to-delivery.
Competing interests
BV is a consultant for Edwards Lifesciences. ER and GL declare that they have no competing interests
References
- Dueck MH, Klimek M, Appenrodt S, Weigand C, Boerner U. Trends but not individual values of central venous oxygen saturation agree with mixed venous oxygen saturation during varying hemodynamic conditions. Anesthesiology. 2005;103:249–257. doi: 10.1097/00000542-200508000-00007. [DOI] [PubMed] [Google Scholar]
- Reinhart K, Kuhn HJ, Hartog C, Bredle DL. Continuous central venous and pulmonary artery oxygen saturation monitoring in the critically ill. Intensive Care Med. 2004;30:1572–1578. doi: 10.1007/s00134-004-2337-y. [DOI] [PubMed] [Google Scholar]
- Räsänen J. Mixed venous oximetry may detect critical oxygen delivery. Anesth Analg. 1990;71:567–568. doi: 10.1213/00000539-199011000-00028. [DOI] [PubMed] [Google Scholar]
- Vallet B, Singer M. In: Patient-Centred Acute Care Training. First. Ramsay G, editor. European Society of Intensive Care Medicine, Brussels; 2006. Hypotension. [Google Scholar]
- Ronco JJ, Fenwick JC, Tweeddale MG. Identification of the critical oxygen delivery for anaerobic metabolism in critically ill septic and nonseptic humans. JAMA. 1993;270:1724–1730. doi: 10.1001/jama.270.14.1724. [DOI] [PubMed] [Google Scholar]
- Rivers E, Nguyen B, Havstad S. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345:1368–1377. doi: 10.1056/NEJMoa010307. [DOI] [PubMed] [Google Scholar]
- Adamczyk S, Robin E, Barreau O. [Contribution of central venous oxygen saturation in postoperative blood transfusion decision] Ann Fr Anesth Reanim. 2009;28:522–530. doi: 10.1016/j.annfar.2009.03.013. [DOI] [PubMed] [Google Scholar]
- Conférence de consensus (2003) Société de réanimation de langue française - XXIIIe Conférence de consensus en réanimation et en médecine d'urgence - jeudi 23 octobre 2003. Transfusion érythrocytaire en réanimation (nouveau-né exclu) Réanimation. 2003;12:531–537. doi: 10.1016/j.reaurg.2003.11.001. [DOI] [PubMed] [Google Scholar]
- van Woerkens EC, Trouwborst A, van Lanschot JJ. Profound hemodilution: what is the critical level of hemodilution at which oxygen delivery-dependent oxygen consumption starts in an anesthetized human? Anesth Analg. 1992;75:818–821. doi: 10.1213/00000539-199211000-00029. [DOI] [PubMed] [Google Scholar]
- Lieberman JA, Weiskopf RB, Kelley SD. Critical oxygen delivery in conscious humans is less than 7.3 mLO2.kg-1.min-1. Anesthesiology. 2000;92:407–413. doi: 10.1097/00000542-200002000-00022. [DOI] [PubMed] [Google Scholar]
- Leung JM, Weiskopf RB, Feiner J. Electrocardiographic ST-segment changes during acute, severe isovolemic hemodilution in humans. Anesthesiology. 2000;93:1004–1010. doi: 10.1097/00000542-200010000-00023. [DOI] [PubMed] [Google Scholar]
- Spahn DR, Zollinger A, Schlumpf RB. Hemodilution tolerance in elderly patients without known cardiac disease. Anesth Analg. 1996;82:681–686. doi: 10.1097/00000539-199604000-00002. [DOI] [PubMed] [Google Scholar]
- Spahn DR, Schmid ER, Seifert B, Pasch T. Hemodilution tolerance in patients with coronary artery disease who are receiving chronic beta-adrenergic blocker therapy. Anesth Analg. 1996;82:687–694. doi: 10.1097/00000539-199604000-00003. [DOI] [PubMed] [Google Scholar]
- Weiskopf RB, Feiner J, Hopf HW. Oxygen reverses deficits of cognitive function and memory and increased heart rate induced by acute severe isovolemic anemia. Anesthesiology. 2002;96:871–877. doi: 10.1097/00000542-200204000-00014. [DOI] [PubMed] [Google Scholar]
- Weiskopf RB, Toy P, Hopf HW. Acute isovolemic anemia impairs central processing as determined by P300 latency. Clin Neurophysiol. 2005;116:1028–1032. doi: 10.1016/j.clinph.2004.12.009. [DOI] [PubMed] [Google Scholar]
- Spahn DR, Madjdpour C. Physiologic transfusion triggers: do we have to use (our) brain? Anesthesiology. 2006;104:905–906. doi: 10.1097/00000542-200605000-00002. [DOI] [PubMed] [Google Scholar]
- Weiskopf RB, Feiner J, Hopf H. Fresh blood and aged stored blood are equally efficacious in immediately reversing anemia-induced brain oxygenation deficits in humans. Anesthesiology. 2006;104:911–920. doi: 10.1097/00000542-200605000-00005. [DOI] [PubMed] [Google Scholar]
- Madjdpour C, Spahn DR, Weiskopf RB. Anemia and perioperative red blood cell transfusion: a matter of tolerance. Crit Care Med. 2006;34:S102–108. doi: 10.1097/01.CCM.0000214317.26717.73. [DOI] [PubMed] [Google Scholar]
- Vallet B, Adamczyk S, Barreau O, Lebuffe G. Physiologic transfusion triggers. Best Pract Res Clin Anaesthesiol. 2007;21:173–181. doi: 10.1016/j.bpa.2007.02.003. [DOI] [PubMed] [Google Scholar]
- Orlov D, O'Farrell R, McCluskey SA. The clinical utility of an index of global oxygenation for guiding red blood cell transfusion in cardiac surgery. Transfusion. 2009;49:682–688. doi: 10.1111/j.1537-2995.2008.02022.x. [DOI] [PubMed] [Google Scholar]