INTRODUCTION
Lumbar degenerative spondylolisthesis (DS) and spinal stenosis (SPS) were originally described as separate pathoanatomic entities, though both cause narrowing of the spinal canal, compression of the nerve roots, and can lead to neurogenic claudication.1,2 Given these commonalities, DS was originally classified as a subgroup among other degenerative causes of stenosis.3 Because listhetic deformities were thought to be inherently unstable, it was debated if fusion in addition to decompression improved outcomes in DS patients. The most definitive answer to that question was provided by Herkowitz and Kurz, who demonstrated significantly improved outcomes when fusion was combined with decompression in a cohort of DS patients.4 As a result, fusion is performed routinely for most DS patients. Less debated has been the role of fusion in SPS. Although there has been no definitive study, two meta-analyses suggested that fusion in addition to decompression did not improve outcomes in SPS.5,6 Most clinicians continue to treat their SPS patients with decompression alone.
Despite the fact that DS and SPS patients typically undergo different surgical treatments, investigators have traditionally combined DS and SPS patients in clinical studies.5,7-12 Prior studies that included both DS and SPS patients have analyzed small subgroups to evaluate the relationship between listhesis and outcomes, and most found that listhesis was not associated with surgical outcomes.12-15 However, a meta-analysis reported that studies including only DS patients had better surgical results than those that combined DS and SPS patients,5 and a recent trial including DS and SPS patients found better outcomes among patients who underwent fusion, 90% of whom had DS.10 Given the lack of consensus about whether DS and SPS patients actually differ clinically, a formal comparison of these two diagnostic groups is needed.
Because DS patients and SPS patients are generally treated with different surgical techniques, the Spine Patient Outcomes Research Trial (SPORT) evaluated and reported results for these two patient groups separately.16,17 This allows us to address two important questions: “Apart from the listhetic deformity, are there clinically relevant differences between patients presenting with DS and SPS ?” and “Are there significant differences between the clinical outcomes of patients with these two conditions?”
METHODS
Study Design
The initial design of SPORT consisted of a randomized controlled trial with a concurrent observational cohort study conducted in 11 states at 13 institutions with multidisciplinary spine practices.18 The human subject committees at each participating institution approved a standardized protocol for the study.
Patient Population
Patients were considered for inclusion in the DS or SPS cohort of SPORT if they were over 18 years old (mean age 65.3 years, range 21-93 years), considered surgical candidates by their treating physicians, and had neurogenic claudication or radicular pain with associated neurologic signs for at least 12 weeks and spinal stenosis on cross-sectional imaging.16,18 Patients with listhesis on the lateral x-ray were assigned to the DS cohort, while patients without listhesis were assigned to the SPS cohort. Exclusion criteria for both diagnoses included: cauda equina syndrome; malignancy; significant deformity; prior back surgery; and other established medical contra-indications to elective surgery.18 In addition, patients with greater than 4 mm of anterior-posterior translation or 10 degrees of intervertebral rotation on lateral flexion-extension x-rays were excluded from the SPS group, and patients with spondylolysis were excluded from the DS group.
Study Interventions
All surgically treated patients in both diagnostic cohorts had a decompressive laminectomy. If fusion was performed, it consisted of bone grafting with or without instrumentation based on the surgeon’s preferences.18 The non-operative treatment group received “usual care”, recommended to include at least physical therapy, education and counseling with home exercise instruction, and non-steroidal anti-inflammatory drugs if tolerated. Details are reported elsewhere.16,17
Study Measures
Data utilized in this study were obtained from patient questionnaires completed at baseline, one and two years after enrollment or surgery that included the SF-36,19 ODI, 20 Stenosis Bothersomeness Index (SBI),21,22 and the Low Back Pain Bothersomeness Scale (LBP).7 The SF-36 scales and the ODI range from 0-100, the Stenosis Bothersomeness Index from 0-24, and the Low Back Pain Bothersomeness Scale from 0-6. Higher scores indicated more severe symptoms on the ODI, Stenosis Bothersomenss Index, and Low Back Pain Bothersomeness Scale, while higher scores indicated less severe symptoms on the SF-36.
Imaging
All patients underwent standing lateral x-rays and cross-sectional imaging. The treating physician determined if listhesis was present on the lateral x-ray. In addition, the cross-sectional imaging was evaluated to determine which levels were stenotic and the severity of the stenosis (mild, moderate or severe).23 The kappa scores for intra-rater reliability of the severity classification have been reported to range from 0.75 to 0.82, while inter-rater reliability ranged from 0.49 to 0.73.23
Statistical Considerations
The initial design of SPORT included both a randomized and an observational cohort. In the first two years of surveillance of the DS randomized trial, 36% of patients assigned to surgery did not have that intervention, and 49% of patients assigned to non-operative treatment underwent surgery.16 A similar trend was observed in the SPS randomized trial, where 33% of patients assigned to surgery did not have that intervention, and 43% of patients assigned to non-operative treatment did have surgery.17 We previously reported comparisons of the baseline characteristics between the randomized and observational cohorts for DS and SPS.16,17 The only significant differences between the DS cohorts were a lower frequency of L3-4 involvement and lateral recess stenosis in the observational group. Among SPS patients, the only significant baseline differences between the randomized and observational cohorts were a higher proportion of patients with a positive nerve tension sign and a lower proportion of patients with lateral recess stenosis among the observational cohort. Importantly, the as-treated analyses revealed no significant differences in the treatment effects of surgery between the randomized and observational patients for either of the diagnostic groups (DS or SPS). Given the high rate of protocol non-adherence (crossover between treatment groups) and the consistency of the baseline characteristics between the randomized and the observational cohorts for both diagnostic groups, the data from the randomized and observational trials (DS and SPS) were combined in an as-treated analysis. The detailed statistical rationale for this strategy has been published elsewhere.24
Differences in baseline characteristics between the DS and SPS cohorts were compared using chi square tests for categorical data and t-tests for continuous data. These baseline comparisons were made between the overall DS and SPS cohorts (surgery and non-operative patients combined), between the surgical cohorts, and between the non-operative cohorts. The primary analyses compared changes in the clinical outcome measures from baseline between the two diagnostic cohorts, within each treatment group (i.e. DS surgery vs. SPS surgery; DS non-operative vs. SPS non-operative). In addition, the treatment effect of surgery was also compared between the two diagnostic cohorts (i.e. DS treatment effect vs. SPS treatment effect). The treatment effect of surgery was defined as:
Positive treatment effects for SF-36 scores and negative treatment effects for ODI, Stenosis Bothersomeness Index, and Low Back Pain Bothersomeness Score indicated that surgery was more effective than non-operative treatment. In these analyses, the treatment indicator (surgery or non-operative) was assigned according to the actual treatment received at each time point. For surgery patients, all changes from baseline prior to surgery were included in the estimates of the effect of non-operative treatment. Following surgery, follow-up times were measured from the date of surgery.24
Longitudinal regression models were created for both diagnostic groups. To adjust for potential confounding, baseline variables associated with missing data or treatment received (baseline outcome score, age, gender, medical center, body mass index, baseline Stenosis Bothersomeness Index, presence of joint or stomach problems, self-rated health trend, insurance status, number of moderate or severe levels, stenosis severity, income, smoking status, and diabetes) were included as adjusting covariates in longitudinal regression models.25 A random effect was specified to account for the repeated measurements of individual patients. Statistical analysis was performed on SAS Software (SAS Institute Inc, Cary, NC) using PROC MIXED for continuous data with normal random effects (BP, PF, ODI, Sciatica Bothersomeness) and PROC GENMOD for non-normal outcomes (Low Back Pain Bothersomeness). At each time point, adjusted mean scores were estimated, and differences between the two diagnostic groups were compared using a Wald test. Statistical significance was defined as p<0.05 on the basis of a two-sided hypothesis test.
RESULTS
Patients
The DS cohort enrolled 607 of 892 eligible patients.16 Of those enrolled, 601 patients completed at least one follow-up visit and were included in the analysis. Sixty one percent (n=369) of patients underwent surgery within two years of enrollment, while the other 39% (n=232) were treated non-operatively. Ninety one percent of enrolled patients completed their one year follow-up, and 86% completed two year follow-up. Of 1,696 patients screened for inclusion in the SPS cohort, 1,091 were eligible, and 654 were enrolled.17 Six hundred thirty four patients completed at least one follow-up visit within the first two years and were included in the study. Three hundred ninety four (62%) underwent surgery within two years, while the remaining 240 received exclusively non-operative care. Eighty-nine percent of enrolled patients completed their one year follow-up, and 83% completed two year follow-up.
Comparison of Baseline Characteristics
Comparison of the baseline characteristics between the overall (surgery and non-operative patients combined) DS and SPS cohorts revealed few significant differences (Table 1). The DS group included a higher proportion of women (69% vs. 39%, p<0.001) and was about a year and a half older (66.1 vs. 64.6 years, p=0.021) than the SPS group. Fewer DS patients reported heart (20% vs. 26%, p=0.021) or bowel (7% vs. 14%, p<0.001) problems, while more reported depression (16% vs. 11%, p=0.009). There were no significant differences on any of the primary (SF-36 BP, PF or ODI) or secondary (SBI or LBP) outcome measures at baseline between the two diagnostic groups. Comparison of the two diagnostic groups stratified by treatment received showed similar trends.
Table 1.
Patient characteristics for the overall, surgery, and non-operative groups.
| Overall | Surgery | Non-operative | |||||||
|---|---|---|---|---|---|---|---|---|---|
| SPS (n=634) |
DS (n=601) |
p-value | SPS (n=394) |
DS (n=369) |
p-value | SPS (n=240) |
DS (n=232) |
p-value | |
| Mean Age (stdev) | 64.6 (11.7) | 66.1 (10.3) | 0.021 | 63.6 (12.2) | 64.7 (10.1) | 0.17 | 66.3 (10.5) | 68.2 (10.3) | 0.045 |
| Female | 249 (39%) | 412 (69%) | <0.001 | 152 (39%) | 256 (69%) | <0.001 | 97 (40%) | 156 (67%) | <0.001 |
| Education - At least some college | 401 (63%) | 400 (67%) | 0.25 | 245 (62%) | 248 (67%) | 0.17 | 156 (65%) | 152 (66%) | 0.98 |
| Work Status | 0.28 | 0.87 | 0.078 | ||||||
| Full or part time | 216 (34%) | 218 (36%) | 144 (37%) | 133 (36%) | 72 (30%) | 85 (37%) | |||
| Disabled | 60 (9%) | 51 (8%) | 40 (10%) | 33 (9%) | 20 (8%) | 18 (8%) | |||
| Retired | 296 (47%) | 257 (43%) | 167 (42%) | 157 (43%) | 129 (54%) | 100 (43%) | |||
| Other | 62 (10%) | 75 (12%) | 43 (11%) | 46 (12%) | 19 (8%) | 29 (12%) | |||
| Compensation - Any | 48 (8%) | 41 (7%) | 0.69 | 30 (8%) | 34 (9%) | 0.51 | 18 (8%) | 7 (3%) | 0.049 |
| Mean Body Mass Index (BMI), (stdev) | 29.5 (5.6) | 29.2 (6.2) | 0.27 | 29.3 (5.3) | 29.4 (6.5) | 0.89 | 29.9 (6.1) | 28.8 (5.7) | 0.053 |
| Smoker | 62 (10%) | 51 (8%) | 0.49 | 36 (9%) | 34 (9%) | 0.93 | 26 (11%) | 17 (7%) | 0.24 |
| Comorbidities | |||||||||
| Hypertension | 288 (45%) | 275 (46%) | 0.95 | 168 (43%) | 164 (44%) | 0.67 | 120 (50%) | 111 (48%) | 0.71 |
| Diabetes | 96 (15%) | 80 (13%) | 0.40 | 53 (13%) | 48 (13%) | 0.94 | 43 (18%) | 32 (14%) | 0.27 |
| Osteoporosis | 60 (9%) | 69 (11%) | 0.29 | 30 (8%) | 41 (11%) | 0.12 | 30 (12%) | 28 (12%) | 1 |
| Heart Problem | 165 (26%) | 122 (20%) | 0.021 | 95 (24%) | 66 (18%) | 0.044 | 70 (29%) | 56 (24%) | 0.26 |
| Stomach Problem | 139 (22%) | 133 (22%) | 0.99 | 82 (21%) | 79 (21%) | 0.91 | 57 (24%) | 54 (23%) | 0.99 |
| Bowel or Intestinal Problem | 86 (14%) | 43 (7%) | <0.001 | 49 (12%) | 30 (8%) | 0.067 | 37 (15%) | 13 (6%) | <0.001 |
| Depression | 70 (11%) | 98 (16%) | 0.009 | 41 (10%) | 64 (17%) | 0.007 | 29 (12%) | 34 (15%) | 0.49 |
| Joint Problem | 346 (55%) | 344 (57%) | 0.38 | 210 (53%) | 202 (55%) | 0.74 | 136 (57%) | 142 (61%) | 0.36 |
| Other | 220 (35%) | 234 (39%) | 0.14 | 136 (35%) | 147 (40%) | 0.15 | 84 (35%) | 87 (38%) | 0.64 |
| Bodily Pain (BP) Score | 31.6 (17.4) | 31.2 (16.9) | 0.69 | 28.6 (16.2) | 29.2 (16.8) | 0.61 | 36.6 (18.4) | 34.4 (16.7) | 0.19 |
| Physical Functioning (PF) Score | 34.8 (23.3) | 34.3 (22.4) | 0.71 | 31.7 (21.9) | 30.7 (20.6) | 0.49 | 39.9 (24.5) | 40.2 (23.9) | 0.90 |
| Mental Component Summary (MCS) Score | 49.4 (11.9) | 50.2 (11.5) | 0.25 | 48.5 (12) | 49.5 (11.6) | 0.26 | 50.9 (11.7) | 51.3 (11.3) | 0.72 |
| Oswestry (ODI) | 42.4 (18.5) | 41.6 (17.8) | 0.43 | 46 (17.9) | 44.9 (16.6) | 0.37 | 36.4 (17.9) | 36.3 (18.5) | 0.95 |
| Stenosis Frequency Index (0-24) | 13.9 (5.8) | 14 (5.6) | 0.76 | 15.2 (5.6) | 14.8 (5.5) | 0.38 | 11.8 (5.6) | 12.6 (5.4) | 0.094 |
| Stenosis Bothersome Index (0-24) | 14.3 (5.7) | 14.7 (5.6) | 0.28 | 15.6 (5.4) | 15.6 (5.5) | 0.98 | 12.3 (5.7) | 13.3 (5.4) | 0.068 |
| Back Pain Bothersomeness | 4.1 (1.8) | 4.3 (1.8) | 0.062 | 4.3 (1.8) | 4.4 (1.8) | 0.23 | 3.8 (1.8) | 4 (1.9) | 0.13 |
| Leg Pain Bothersomeness | 4.3 (1.7) | 4.5 (1.7) | 0.019 | 4.6 (1.6) | 4.7 (1.6) | 0.34 | 3.9 (1.8) | 4.3 (1.8) | 0.012 |
Comparison of Imaging Findings
Cross-sectional imaging revealed substantial patho-anatomic differences between the groups (Table 2). The majority of DS patients (62%) had only one level with moderate or severe stenosis, while 61% of SPS patients had multilevel involvement. Over 90% of patients in both groups had stenosis at L4-5, though DS patients were significantly less likely to have stenosis at any other level compared to the SPS patients (p<0.001). In general, DS was associated with more severe localized stenosis at the listhetic L4-5 level, while SPS patients tended to have more moderate, multilevel stenosis.
Table 2.
Imaging findings for the overall, surgery, and non-operative groups.
| Overall | Surgery | Non-operative | |||||||
|---|---|---|---|---|---|---|---|---|---|
| SPS (n=634) |
DS (n=601) |
p-value | SPS (n=394) |
DS (n=369) |
p-value | SPS (n=240) |
DS (n=232) |
p-value | |
| Stenosis Levels | |||||||||
| L2-L3 | 179 (28%) | 53 (9%) | <0.001 | 121 (31%) | 33 (9%) | <0.001 | 58 (24%) | 20 (9%) | <0.001 |
| L3-L4 | 420 (66%) | 236 (39%) | <0.001 | 266 (68%) | 145 (39%) | <0.001 | 154 (64%) | 91 (39%) | <0.001 |
| L4-L5 | 579 (91%) | 580 (97%) | <0.001 | 362 (92%) | 358 (97%) | 0.003 | 217 (90%) | 222 (96%) | 0.039 |
| L5-S1 | 173 (27%) | 57 (9%) | <0.001 | 100 (25%) | 29 (8%) | <0.001 | 73 (30%) | 28 (12%) | <0.001 |
| Stenotic Levels (Mod/Severe) | <0.001 | <0.001 | <0.001 | ||||||
| None | 15 (2%) | 23 (4%) | 6 (2%) | 9 (2%) | 9 (4%) | 14 (6%) | |||
| One | 234 (37%) | 370 (62%) | 140 (36%) | 232 (63%) | 94 (39%) | 138 (59%) | |||
| Two | 241 (38%) | 172 (29%) | 153 (39%) | 104 (28%) | 88 (37%) | 68 (29%) | |||
| Three+ | 144 (23%) | 36 (6%) | 95 (24%) | 24 (7%) | 49 (20%) | 12 (5%) | |||
| Stenosis Severity (of most severe level) | 0.004 | 0.24 | 0.007 | ||||||
| Mild | 15 (2%) | 23 (4%) | 6 (2%) | 9 (2%) | 9 (4%) | 14 (6%) | |||
| Moderate | 282 (44%) | 215 (36%) | 161 (41%) | 131 (36%) | 121 (50%) | 84 (36%) | |||
| Severe | 337 (53%) | 363 (60%) | 227 (58%) | 229 (62%) | 110 (46%) | 134 (58%) | |||
Comparison of Treatment Received
The surgical procedures performed on the two groups were markedly different. Ninety four percent (N=347) of DS patients underwent fusion compared to 11% (N=43) of SPS patients (p<0.001). Among those who underwent fusion, DS patients were more likely to undergo instrumented fusion (78% vs. 53%, p<0.001). No significant differences were seen in the type of non-operative care received between the two diagnostic groups.
Comparison of Outcomes
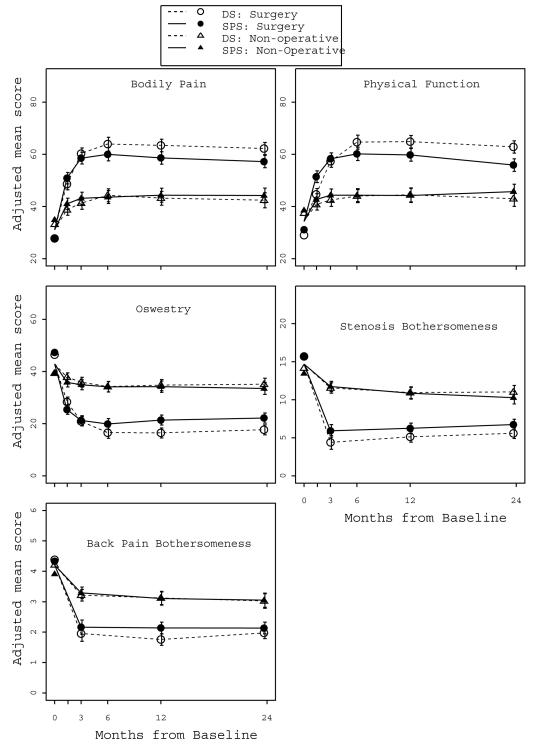
Both DS and SPS patients improved more with surgery than with non-operative treatment on all outcome measures at both one and two years. Among patients treated surgically, DS patients improved significantly more than SPS patients on all three primary outcome measures (SF-36 BP, PF, and ODI) at both one and two years (Figure 1). At one year, DS patients improved 32.3 points on the SF-36 BP score vs. 27.5 points for SPS patients (p=0.006), and the difference persisted at two years (31.1 vs. 26.1, p=0.003, Table 3). Similar differences were observed on the SF-36 PF score and ODI, with the most marked difference observed on PF at 2 years (DS 28.3 vs. SPS 21.4, p<0.001). Similar but less substantial differences were observed on the secondary outcome measures (SBI, LBP). Among surgical patients, the DS group improved about 1 point more than the SPS group on the SBI at one and two years (DS −9.5 vs. SPS −8.4, p=0.027 at 1 year; DS −9.0 vs. SPS −7.9, p=0.016 at two years). The difference in improvement on LBP was marginal and no longer significant at 2 years (DS −2.2 vs. SPS −2.0, p=0.26).
Figure 1.
Table 3.
Comparisons of change from baseline scores and treatment effects, adjusted* as-treated analysis.
| 1Y | 2Y | ||||||
|---|---|---|---|---|---|---|---|
| Surgery | Nono- perative |
Treatment Effect | Surgery | Nono- perative |
Treatment Effect | ||
| BP | |||||||
| DS | 32.3 (1.2) | 12 (1.4) | 20.3 (17, 23.5) | 31.1 (1.2) | 11.2 (1.5) | 19.9 (16.4, 23.3) | |
| SPS | 27.5 (1.2) | 13.2 (1.4) | 14.3 (10.9, 17.6) | 26.1 (1.2) | 13.1 (1.4) | 13 (9.5, 16.5) | |
| p-value** | 0.006 | 0.55 | 0.011 | 0.003 | 0.37 | 0.005 | |
|
| |||||||
| PF | |||||||
| DS | 30.4 (1.2) | 10 (1.4) | 20.4 (17.1, 23.7) | 28.3 (1.2) | 8.5 (1.5) | 19.9 (16.4, 23.3) | |
| SPS | 25.3 (1.2) | 9.7 (1.4) | 15.6 (12.2, 18.9) | 21.4 (1.2) | 11.2 (1.5) | 10.2 (6.7, 13.6) | |
| p-value** | 0.004 | 0.92 | 0.04 | <0.001 | 0.19 | <0.001 | |
|
| |||||||
| ODI | |||||||
| DS | −25.9 (1) | −7.6 (1.1) | −18.3 (−20.9, −15.7) | −24.7 (1) | −7.3 (1.2) | −17.4 (−20.2, −14.7) | |
| SPS | −21 (1) | −8.2 (1.1) | −12.8 (−15.5, −10.1) | −20.2 (1) | −8.9 (1.2) | −11.4 (−14.1, −8.6) | |
| p-value** | <0.001 | 0.70 | 0.003 | <0.001 | 0.35 | 0.002 | |
|
| |||||||
| Stenosis Bothersomeness | |||||||
| DS | −9.5 (0.4) | −3.7 (0.4) | −5.8 (−6.8, −4.8) | −9 (0.3) | −3.6 (0.4) | −5.4 (−6.5, −4.4) | |
| SPS | −8.4 (0.4) | −3.8 (0.4) | −4.6 (−5.6, −3.6) | −7.9 (0.4) | −4.3 (0.4) | −3.5 (−4.6, −2.5) | |
| p-value** | 0.027 | 0.88 | 0.084 | 0.016 | 0.22 | 0.008 | |
|
| |||||||
| Back pain bothersomeness | |||||||
| DS | −2.4 (0.1) | −1 (0.1) | −1.4 (−1.7, −1.1) | −2.2 (0.1) | −1.1 (0.1) | −1 (−1.3, −0.7) | |
| SPS | −2 (0.1) | −1.1 (0.1) | −1 (−1.3, −0.7) | −2 (0.1) | −1.1 (0.1) | −0.9 (−1.2, −0.6) | |
| p-value** | 0.012 | 0.90 | 0.054 | 0.26 | 0.87 | 0.52 | |
Adjusted for age, gender, site, baseline score, bmi, baseline Sciatica Bothersomeness, joint comorbidities, self-rated health trend, insurance coverage, number of moderate/severe levels, stenosis severity, stomach comorbidities, income, smoking status, diabetes
p-values are based on contrasts
There were no significant outcome differences between DS and SPS patients treated non-operatively on any outcome measure at one or two years. This resulted in the DS patients experiencing a greater treatment effect of surgery than the SPS patients on all three primary outcome measures at 1 and 2 years. The largest difference in treatment effect was observed for the PF score at two years (DS 19.9 vs. SPS 10.2, p<0.001). The treatment effect was slightly greater for DS compared to SPS at two years on the SBI (−5.4 vs. −3.5, p=0.008), while there was no significant difference in treatment effect on LBP at one (DS −1.4 vs. SPS −1.0, p= 0.054) or two years (DS −1.0 vs. SPS −0.9, p=0.52).
DISCUSSION
Degenerative spondylolisthesis has traditionally been viewed as a diagnostic subcategory within the broader diagnosis of spinal stenosis,3 and no formal comparison from baseline through treatment has been performed between the two diagnostic groups. The current study suggests that while DS and SPS patients may present with similar clinical findings, they have different demographic characteristics and radiographic findings, are treated with different surgical techniques, and have different surgical outcomes. As has been shown in prior epidemiologic studies, women were more likely to present with DS than men.26 Otherwise, the baseline clinical characteristics, including leg pain, back pain, and global health measures, were very similar for the two groups. This is in contrast to anecdotal evidence that has suggested DS patients more frequently report back pain that some authors have attributed to “instability”, whereas SPS patients are more likely to present with neurogenic claudication.27-31 The findings of the current study support a recent analysis of the SPORT DS cohort that reported no relationship between baseline back pain and the grade of slip or the presence of hypermobility on flexion-extension radiographs, suggesting that radiographic indicators of “instability” may not be associated with clinical symptoms.32 In the current study, DS patients tended to have single level, severe stenosis at L4-L5, while SPS patients more frequently had moderate, multilevel involvement. In accordance with current trends, most SPS patients (89%) were treated with decompression alone, while the vast majority (94%) of DS patients underwent decompression and fusion. The DS patients improved significantly more with surgical treatment than the SPS group, though the magnitude of these outcome differences was modest.33-35
The current investigation is the first large short-term cohort study to directly compare clinical outcomes between patients with DS and SPS. Herron et al. followed 140 surgically treated stenosis patients, some of whom had DS. They found that the presence of listhesis was not associated with the degree of improvement of leg or back pain.13 Katz et al. studied 199 stenosis patients, 33% of whom had > 5mm of forward displacement. After surgical intervention, there were no differences in walking capacity, symptom severity or satisfaction between those with or without DS.12 However, some of the DS patients were treated with decompression alone. While no prior study has clearly delineated better surgical outcomes in DS patients, there has been indirect evidence suggestive of this. In Malmivaara’s recent RCT comparing surgery to non-operative treatment of lumbar stenosis, the 10 patients who underwent decompression and fusion—9 of whom had DS--improved more than those who underwent decompression alone.10 In addition, Turner et al.’s meta-analysis of lumbar stenosis demonstrated better outcomes in the four studies that included only DS patients.5 However, it is unclear if this represented a real clinical difference or was the result of the DS studies’ exclusion of patients with prior lumbar surgery and those receiving worker’s compensation (i.e. excluding these patients who are known to have worse outcomes from the DS studies but not the SPS studies would bias the results towards better outcomes in DS patients). The current study offers the first sufficiently powered, direct comparison of outcomes in DS and SPS and confirms that DS patients improve more with surgery than those with SPS.
The current findings raise the question “Why are surgical outcomes better in DS than SPS?” A simplistic analysis might conclude fusion was the determining factor, yet this seems unlikely because back pain, the symptom fusion was designed to relieve, improved to a similar degree for the fused DS patients and the unfused SPS patients at two years. Direct comparison of the outcomes for the fused and unfused SPS patients was limited by the small number of SPS patients who were fused, but there were no significant outcomes differences between these groups at one or two years (data not shown). The inability to detect a difference between the two groups may have been due to similar outcomes between the two groups or an underpowered comparison (Type II error). The current study offers no evidence to support or refute the use of fusion in SPS patients without listhesis. It should be noted that the indications for fusion and fusion technique were not specified, and individual surgeons determined the need for fusion and the specific fusion technique on a case by case basis. The results of different fusion techniques in the SPORT DS cohort have been reported elsewhere.36
Prior studies have suggested that multilevel involvement and less severe stenosis were associated with worse surgical outcomes, though these findings are controversial.5,13,37,38 Separate SPORT subgroup analyses have shown that surgical outcomes were similar between SPS patients with single and multilevel involvement, suggesting that the higher rate of multilevel disease in SPS was not the driving factor behind the outcome differences observed in the current study.39 Future studies should explore what underlies the outcome differences between DS and SPS patients.
Another question that arises is “Why were non-operative outcomes no different in DS and SPS?” The degree of improvement observed with non-operative treatment was quite low for both diagnostic groups and probably not clinically meaningful. Unlike disk herniations that can often be treated successfully with non-operative treatment,40,41 DS and SPS may represent relatively static conditions that tend not to improve substantially with time and non-operative treatment.42 Given that neither non-operative group demonstrated clinically meaningful improvement, it is not surprising that no subtle outcome differences were detected.
This study does have certain limitations. Because of the high rate of protocol non-adherence, the data were analyzed on an as-treated basis, with loss of the benefits of randomization. As such, the surgery and non-operative groups had significant baseline differences. Longitudinal regression models were used to control for these differences, however, the potential for confounding by unmeasured variables exists. We have detailed the rationale behind these analyses elsewhere.24 In addition, SPORT was not initially designed to make the comparison between diagnostic groups.18 However, with over 600 patients in each diagnostic group, the current study was certainly not underpowered. The follow-up period of this study was limited to two years, and the Maine Lumbar Spine Study demonstrated that the surgical outcomes for spinal stenosis tended to deteriorate slightly from two to ten years.9 As such, the results of the current study may change with longer follow-up.
The current study demonstrated that DS and SPS patients are clinically similar at baseline but have different surgical outcomes. Given that the presence or absence of listhesis is not a modifiable factor, the results of this study will probably not affect the treatment of individual patients. Both diagnostic groups fared far better with surgical treatment compared to non-operative care, and the differences in surgical outcomes between the two diagnostic groups, though significant, were relatively modest.35 However, the differences in radiographic findings, surgical treatment, and outcomes indicate that these are two distinct patient populations that should probably not be combined in future studies.
Acknowledgement
The authors would like to acknowledge funding from the following sources: the National Institute of Arthritis and Musculoskeletal and Skin Diseases (U01-AR45444) and the Office of Research on Women’s Health, the National Institutes of Health, and the National Institute of Occupational Safety and Health, the Centers for Disease Control and Prevention.
Footnotes
This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Junghanns H. Spondylolisthesen ohne Spalt in Zwischengelenkstueck. Archiv fur Orthopadische Unfallchirurgie. 1930;29:118–27. [Google Scholar]
- 2.Verbeist H. A radicular syndrome from developing narrowing of the lumbar vertebral canal. J Bone Joint Surg [Br] 1954;37-B:230–7. doi: 10.1302/0301-620X.36B2.230. [DOI] [PubMed] [Google Scholar]
- 3.Arnoldi CC, Brodsky AE, Cauchoix J, et al. Lumbar spinal stenosis and nerve root entrapment syndromes. Definition and classification. Clin Orthop Relat Res. 1976:4–5. [PubMed] [Google Scholar]
- 4.Herkowitz HN, Kurz LT. Degenerative lumbar spondylolisthesis with spinal stenosis. A prospective study comparing decompression with decompression and intertransverse process arthrodesis. J Bone Joint Surg Am. 1991;73:802–8. [PubMed] [Google Scholar]
- 5.Turner JA, Ersek M, Herron L, et al. Surgery for lumbar spinal stenosis. Attempted meta-analysis of the literature. Spine. 1992;17:1–8. doi: 10.1097/00007632-199201000-00001. [DOI] [PubMed] [Google Scholar]
- 6.van Tulder MW, Koes B, Seitsalo S, et al. Outcome of invasive treatment modalities on back pain and sciatica: an evidence-based review. Eur Spine J. 2006;15(Suppl 1):S82–92. doi: 10.1007/s00586-005-1049-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Atlas SJ, Deyo RA, Keller RB, et al. The Maine Lumbar Spine Study, Part III. 1-year outcomes of surgical and nonsurgical management of lumbar spinal stenosis. Spine. 1996;21:1787–94. doi: 10.1097/00007632-199608010-00012. discussion 94-5. [DOI] [PubMed] [Google Scholar]
- 8.Atlas SJ, Keller RB, Robson D, et al. Surgical and nonsurgical management of lumbar spinal stenosis: four-year outcomes from the maine lumbar spine study. Spine. 2000;25:556–62. doi: 10.1097/00007632-200003010-00005. [DOI] [PubMed] [Google Scholar]
- 9.Atlas SJ, Keller RB, Wu YA, et al. Long-term outcomes of surgical and nonsurgical management of lumbar spinal stenosis: 8 to 10 year results from the maine lumbar spine study. Spine. 2005;30:936–43. doi: 10.1097/01.brs.0000158953.57966.c0. [DOI] [PubMed] [Google Scholar]
- 10.Malmivaara A, Slatis P, Heliovaara M, et al. Surgical or nonoperative treatment for lumbar spinal stenosis? A randomized controlled trial. Spine. 2007;32:1–8. doi: 10.1097/01.brs.0000251014.81875.6d. [DOI] [PubMed] [Google Scholar]
- 11.Katz JN, Lipson SJ, Brick GW, et al. Clinical correlates of patient satisfaction after laminectomy for degenerative lumbar spinal stenosis. Spine. 1995;20:1155–60. doi: 10.1097/00007632-199505150-00008. [DOI] [PubMed] [Google Scholar]
- 12.Katz JN, Stucki G, Lipson SJ, et al. Predictors of surgical outcome in degenerative lumbar spinal stenosis. Spine. 1999;24:2229–33. doi: 10.1097/00007632-199911010-00010. [DOI] [PubMed] [Google Scholar]
- 13.Herron LD, Trippi AC. L4-5 degenerative spondylolisthesis. The results of treatment by decompressive laminectomy without fusion. Spine. 1989;14:534–8. [PubMed] [Google Scholar]
- 14.Jonsson B, Annertz M, Sjoberg C, et al. A prospective and consecutive study of surgically treated lumbar spinal stenosis. Part II: Five-year follow-up by an independent observer. Spine. 1997;22:2938–44. doi: 10.1097/00007632-199712150-00017. [DOI] [PubMed] [Google Scholar]
- 15.Mariconda M, Fava R, Gatto A, et al. Unilateral laminectomy for bilateral decompression of lumbar spinal stenosis: a prospective comparative study with conservatively treated patients. J Spinal Disord Tech. 2002;15:39–46. doi: 10.1097/00024720-200202000-00006. [DOI] [PubMed] [Google Scholar]
- 16.Weinstein JN, Lurie JD, Tosteson TD, et al. Surgical versus nonsurgical treatment for lumbar degenerative spondylolisthesis. N Engl J Med. 2007;356:2257–70. doi: 10.1056/NEJMoa070302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Weinstein JN, Tosteson TD, Lurie JD, et al. Surgical versus nonsurgical therapy for lumbar spinal stenosis. N Engl J Med. 2008;358:794–810. doi: 10.1056/NEJMoa0707136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Birkmeyer NJ, Weinstein JN, Tosteson AN, et al. Design of the Spine Patient outcomes Research Trial (SPORT) Spine. 2002;27:1361–72. doi: 10.1097/00007632-200206150-00020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ware JE, Jr., Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–83. [PubMed] [Google Scholar]
- 20.Daltroy LH, Cats-Baril WL, Katz JN, et al. The North American spine society lumbar spine outcome assessment Instrument: reliability and validity tests. Spine. 1996;21:741–9. doi: 10.1097/00007632-199603150-00017. [DOI] [PubMed] [Google Scholar]
- 21.Atlas SJ, Deyo RA, Patrick DL, et al. The Quebec Task Force classification for Spinal Disorders and the severity, treatment, and outcomes of sciatica and lumbar spinal stenosis. Spine. 1996;21:2885–92. doi: 10.1097/00007632-199612150-00020. [DOI] [PubMed] [Google Scholar]
- 22.Patrick DL, Deyo RA, Atlas SJ, et al. Assessing health-related quality of life in patients with sciatica. Spine. 1995;20:1899–908. doi: 10.1097/00007632-199509000-00011. discussion 909. [DOI] [PubMed] [Google Scholar]
- 23.Lurie JD, Tosteson AN, Tosteson TD, et al. Reliability of readings of magnetic resonance imaging features of lumbar spinal stenosis. Spine. 2008;33:1605–10. doi: 10.1097/BRS.0b013e3181791af3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tosteson TD, Hanscom B, Blood EA, et al. Statistical methods for cross-over in the SPORT lumbar disc herniation trial. International Society for the Study of the Lumbar Spine Annual Meeting; Hong Kong. 2007. [Google Scholar]
- 25.Fitzmaurice G, Laird N, Ware J. Applied Longitudinal Analysised. John Wiley & Sons; Philadelphia, PA: 2004. [Google Scholar]
- 26.Rosenberg NJ. Degenerative spondylolisthesis. Predisposing factors. J Bone Joint Surg Am. 1975;57:467–74. [PubMed] [Google Scholar]
- 27.Hai Y. Spinal Stenosis: Classification, Natural History and Clinical Evaluation. In: Herkowitz H, Dvorak J, Bell G, et al., editors. The Lumbar Spine. 3 ed Lippincott Williams & Wilkins; Philadelphia: 2004. pp. 464–71. [Google Scholar]
- 28.Mossaad MM. Degenerative Lumbar Spondlyolisthesis with Spinal Stenosis: Natural History, Diagnosis, Clinical Presentation, and Nonoperative Treatment. In: Herkowitz H, Dvorak J, Bell G, et al., editors. The Lumbar Spine. 3 ed Lippincott Williams & Wilkins; Philadelphia: 2004. pp. 514–23. [Google Scholar]
- 29.Sengupta DK, Herkowitz HN. Degenerative spondylolisthesis: review of current trends and controversies. Spine. 2005;30:S71–81. doi: 10.1097/01.brs.0000155579.88537.8e. [DOI] [PubMed] [Google Scholar]
- 30.Nachemson A. Lumbar spine instability. A critical update and symposium summary. Spine. 1985;10:290–1. [PubMed] [Google Scholar]
- 31.Nizard RS, Wybier M, Laredo JD. Radiologic assessment of lumbar intervertebral instability and degenerative spondylolisthesis. Radiol Clin North Am. 2001;39:55–71. v–vi. doi: 10.1016/s0033-8389(05)70263-3. [DOI] [PubMed] [Google Scholar]
- 32.Pearson AM, Lurie JD, Blood EA, et al. Spine patient outcomes research trial: radiographic predictors of clinical outcomes after operative or nonoperative treatment of degenerative spondylolisthesis. Spine. 2008;33:2759–66. doi: 10.1097/BRS.0b013e31818e2d8b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zanoli G. Outcome assessment in lumbar spine surgery. Acta Orthop Suppl. 2005;76:5–47. [PubMed] [Google Scholar]
- 34.Hagg O, Fritzell P, Nordwall A. The clinical importance of changes in outcome scores after treatment for chronic low back pain. Eur Spine J. 2003;12:12–20. doi: 10.1007/s00586-002-0464-0. [DOI] [PubMed] [Google Scholar]
- 35.Glassman SD, Copay AG, Berven SH, et al. Defining substantial clinical benefit following lumbar spine arthrodesis. J Bone Joint Surg Am. 2008;90:1839–47. doi: 10.2106/JBJS.G.01095. [DOI] [PubMed] [Google Scholar]
- 36.Abdu WA, Lurie JD, Spratt KF, et al. Degenerative Spondylolisthesis: Does Fusion Method Influence Outcome? Four-Year Results of the Spine Patient Outcomes Research Trial (SPORT) Spine. 2009 doi: 10.1097/BRS.0b013e3181b8a829. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Iguchi T, Kurihara A, Nakayama J, et al. Minimum 10-year outcome of decompressive laminectomy for degenerative lumbar spinal stenosis. Spine. 2000;25:1754–9. doi: 10.1097/00007632-200007150-00003. [DOI] [PubMed] [Google Scholar]
- 38.Mariconda M, Zanforlino G, Celestino GA, et al. Factors influencing the outcome of degenerative lumbar spinal stenosis. J Spinal Disord. 2000;13:131–7. doi: 10.1097/00002517-200004000-00007. [DOI] [PubMed] [Google Scholar]
- 39.Park DK, An HS, Lurie JD, et al. Does multilevel stenosis lead to poorer outcomes? A subanalysis of the SPORT lumbar stenosis study. Spine. 2009 doi: 10.1097/BRS.0b013e3181bdafb9. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Weinstein JN, Lurie JD, Tosteson TD, et al. Surgical vs nonoperative treatment for lumbar disk herniation. The Spine Patient Outcomes Research Trial (SPORT) observational cohort. JAMA. 2006;296:2451–9. doi: 10.1001/jama.296.20.2451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Weinstein JN, Tosteson TD, Lurie JD, et al. Surgical vs nonoperative treatment for lumbar disc herniation. The Spine Patient Outcomes Research Trial (SPORT): a randomized trial. JAMA. 2006;296:2441–45. doi: 10.1001/jama.296.20.2441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Johnsson KE, Rosen I, Uden A. The natural course of lumbar spinal stenosis. Clin Orthop Relat Res. 1992:82–6. [PubMed] [Google Scholar]