SUMMARY
Background
The status and determinants of health-related quality of life (HRQOL) in female veterans with and without irritable bowel syndrome (IBS) is unknown.
Aim
To compare HRQOL in female veterans with and without IBS symptoms and examine the contribution of post-traumatic stress disorder (PTSD), depression, and anxiety to HRQOL.
Methods
A cross-sectional study of 339 female veterans. Self-report questionnaires were used to evaluate IBS symptoms, PTSD, depression, anxiety, and HRQOL.
Results
Symptoms consistent with IBS were present in 33.5% of participants. Female veterans with IBS symptoms had significant reductions in physical component score (PCS) and 5 of 8 Health Related Quality of Life subscales, and on 7 of 8 Irritable Bowel Syndrome Quality Of Life subscales, than female veterans without IBS symptoms. Compared to the US general female population, female veterans had significantly lower Health Related Quality of Life PCS and mental component scores (MCS) irrespective of IBS symptom status. Differences in the MCS score was most explained by depression; while the PCS score was most explained anxiety.
Conclusions
IBS symptoms in female veterans are associated with considerable reduction in HRQOL. However, female veterans regardless of IBS symptom status have lower HRQOL compared to the general US female population.
Introduction
Irritable bowel syndrome (IBS) is a functional gut disorder that manifests in patients as chronic or recurring abdominal pain, accompanied with alteration of bowel habits (1, 2). Hayee and Forgacs (2007) have suggested that IBS is likely the result of several biological and psychosocial factors (3). Some of the biological factors include disordered gut motility, visceral hypersensitivity, intestinal inflammation, and genetics (4, 5). Psychologically, patients presenting with IBS show more depression, emotionality, and worry about their health than do patients without IBS (7), as well as more maladaptive coping strategies (8). Further, two recent community-based studies (9, 10) have shown an association between IBS and psychological factors as well as somatization; in one study, IBS was not found in cases with both low global severity index score and few somatic symptoms (9), and in the other study, there was strong association between IBS and generalized anxiety co-morbidity (10). Identifying and treating psychosocial factors have increasingly become a component of IBS management (11, 12).
There were nearly 1.6 million women veterans according to the 2000 U.S. Census, 11.4% of whom use the VA for part or all of their health care (13). Furthermore, women veterans were considered to be “among the fastest growing segments of new users” (13). Although there have been over 180 published articles as of 2008 examining different aspects of female veterans health, few have included IBS or general gastrointestinal symptoms (14–23). Psychological treatments have been recommended, but their effectiveness is still a matter of debate as psychological interventions may show slight superiority over usual care but the benefits have not yet been show to be sustained following treatment completion (24). A recent review by Ford et. al. (2009) has suggested pharmacotherapy with antidepressants is an effective IBS treatment with a number needed to treat of 4 both for selective serotonin reuptake inhibitors and for tricyclic antidepressants (25).
Prior investigations have shown that patients with IBS have a reduced health related quality of life (HRQOL) (26–29). Gralnek et al. (27) and Afendy et al. (29) have described a pronounced reduction in energy, role limitations due to physical problems, body pain, and in general health perceptions domains of HRQOL. Afendy et al. further noted that female patients had lower functioning on the following 6 of 8 Health Related Quality of Life (SF-36) subscales: physical functioning, role functioning, bodily pain, general health, vitality, and mental health (29). Previous studies in non-veterans have linked the presence and severity of IBS to the co-morbid presence of depression (30–33) and anxiety disorders (29,33–37), including PTSD (38). The sole published data on IBS in an all-female veteran’s sample, based upon the same but smaller sample as this project, reported that the presence of anxiety, depression, or PTSD was associated with more than a 3 fold increase in the odds of having IBS or dyspepsia (23).
Given that HRQOL is an important measure of IBS burden as well as a factor to be monitored in the treatment of IBS, and that this information in women veterans is notably lacking, the purpose of this study was to estimate the impact of IBS symptoms on the health-related quality of life for a sample of female veterans. The two questions we aimed to answer were: 1) How do female veterans with symptoms consistent with IBS compare in their HRQOL to female veterans without IBS symptoms, and to the standardized general US female population; and 2) How do IBS symptoms, PTSD, depression, or anxiety relate to HRQOL in female veterans?
Methods
This prospective cross-sectional study examined the burden of IBS symptoms in women veterans seeking care at a VA women’s clinic. This project was part of a larger study designed to examine the prevalence of functional gut disorders in women veterans (23). The sampling frame consisted of patients scheduled for non-urgent outpatient primary care at the Michael E. DeBakey Veterans Affairs Medical Center (MEDVAMC) Women’s Health Center. Only women veterans (not family members of veterans) 18 years of age and older were eligible to participate. Eligible women were introduced to the study at the time of their arrival to the clinic and asked to complete the study questionnaires provided by a research associate. Veterans who agreed to participate were handed a packet containing the study questionnaires to complete at the clinic or return completed questionnaires in a pre-paid envelope.
Self-administered questionnaires were used to collect demographic data, including age, body mass index (BMI) based on each participant’s height and weight at the time of survey, race (White, African American, Hispanic/Other), marital status (currently married, previously married, never married), education (High School or less, some College (1–3 years) or Technical School, College Graduate or Graduate School), and frequency of tobacco smoking (everyday, some days, never). Additional questionnaires described below were administered to ascertain IBS symptom status, quality of life, depression, anxiety and PTSD.
Bowel Disorder Questionnaire (BDQ)
IBS status was defined by the presence of compatible symptoms after clinical exclusion of other potential organic causes. The BDQ (39) consists of 59 questions that capture the presence, severity, and duration of several upper and lower GI symptoms. Questions #1,2,3,4,14, and one or more of #20–24,28,30,33 were used as the qualifying and diagnosis questions closely approximating the Rome II definition for IBS (40).
Irritable Bowel Syndrome Quality of Life Questionnaire (IBSQOL)
The IBSQOL (41) is a disease-specific quality of life measure for IBS consisting of 34 questions. It produces an overall score and 8 subscale scores, including dysphoria, interference with activity, body image, health worry, food avoidance, social reaction, sexual functioning, and interpersonal relationships. The scores are transformed as a percentage from 0% (low functioning) to 100% (high functioning). The IBS-QOL has demonstrated high internal consistency (Cronbach’s alpha = 0.95), and high reproducibility (Intraclass correlation = 0.86). Convergent validity for the IBSQOL showed that scores are more related to overall well-being than to function (compared to the SF-36) (41). The IBSQOL scores indicative of minimally clinically important difference (MCID) ranges in its different domains from a minimal response at 10 points to an optimal response at 14 points (42). We have chosen to use a MCID of ≥ 14.0.
Health Related Quality of Life (SF-36)
The SF-36 yields 8 sub-scales on physical functioning [PF], role–physical [RP], bodily pain [BP], general health [GH], vitality [VS], social functioning [SF], role–emotional [RE], mental health [MH], and 2 composite summary scores (the physical component score [PCS] and the mental component score [MCS]). Validity and reliability for the SF-36 were previously established (43, 44).
A version of the SF-36 (SF-36V) was designed to use with the Veterans Health Administration (VHA) ambulatory care populations (45), and was shown to have good discriminant validity for measuring disease burden in VHA populations (28). The VHA uses the SF-36V both to monitor patient self-reported health as well as an outcome measure for program evaluation, population health, health services, and for clinical interventions. Higher scores are associated with higher quality of life.
The SF-36 has been shown to have a MCID ranging from 2.8 (Physical Component Score) to 7.6 (Physical Functioning) (46). Hays et al. (47) concluded the MCID for SF-36 is typically between 3–5 points. We used a MCID cutoff value of 5.0 for guiding our interpretations.
Mississippi Scale for Combat Related PTSD
The Mississippi Scale for Combat Related PTSD (48) is a 35-item self report scale based on DSM-IV criteria, and has shown to be sensitive (.93), and specific (.89) in differentiating groups with and without PTSD. The scale is scored from 1 to 5 on each item, with 10 of the 35 items being reversed scored. The scoring range is from 35 to 175, with higher scores corresponding to more symptomatology. We used the previously validated cutoff score of 107 to define PTSD (48).
Beck Depression Inventory - Second Edition (BDI)
The 21-item BDI (49) was used to assess severity of depression. The BDI is a highly reliable and valid instrument with excellent internal consistency, and factorial and convergent validity (50). Total scores ranging from 0–13 are indicative of minimal depression, 14–19 of mild depression, 20–28 of moderate depression, and 29–63 of severe depression (49).
Beck Anxiety Inventory (BAI)
The BAI (51) is a 21-item, self-report measure of anxiety that was used to assess severity of anxiety. The BAI possesses strong psychometric properties related to internal consistency, test-retest reliability, and validity (52–54). A score of 0–7 indicates minimal anxiety; 8–15, mild anxiety; 16–25, moderate anxiety; and 26–63, severe anxiety (51).
Statistical Analysis
For the primary analyses, the sample of participants was categorized into two groups; with and without IBS symptoms based on BDQ responses (23). HRQOL was evaluated using the SF-36 (for comparison to the US general female population), the SF-36V (for comparison for our female veteran sample with and without IBS), and the IBSQOL overall score and its 8 subscales.
We compared using T-tests for the SF-36 and IBSQOL scales and summary scores between participants with and without IBS. In addition, SF-36 in the overall study sample is compared to the U.S. General Female Population (55). Levene’s Test for equality of variances was calculated for each comparison. If equal variance was not present, the final T-test was performed using Satterthwaite’s approximation for unequal variances.
We employed linear regression models to evaluate the potential contributions of IBS, demographic factors, and psychological factors toward HRQOL scores. The dependent variables for the two SF-36V regressions were the SF-36V physical component score and mental component score. The dependent variable for the IBSQOL was the overall score. The independent variables for each linear regression were entered as follows. In step 1: age, marital status, ethnicity, education, BMI, and smoking status were entered. In step 2: IBS symptom status, total BDI score, total BAI score, and total PTSD score were added to variables retained from step 1. Backwards stepwise elimination was employed in order to get the smallest list of potentially contributory variables.
We performed comparisons of SF-36 scores to the U.S. General Female Population using Stata version 8 (StataCorp LP, College Station, TX. http://www.stata.com). All other analyses were conducted using SPSS version 15.0 for Windows (SPSS, Inc., Chicago, IL),
Results
Between November 2005 and February 2006, we identified 393 consecutive women veterans scheduled for primary care appointments in the Women’s Health Center at Michael E. DeBakey Veterans Affairs Medical Center. Fifty-four of the identified potential participants were not included in the study as they declined offers for participation and as such no data was gathered on them. We recruited 339 women veterans for study participation for an overall participation rate of 84%. Two participants were missing information on IBS symptoms, and were excluded from the analysis.
Table 1 shows the sociodemographic features for the 337 participants in the final analysis dataset, and for a comparison between those with IBS symptoms compared to those without IBS symptoms. Symptoms compatible with IBS in the BDQ were reported in 33.5% (113 of 337) of the entire sample. There were significantly more white (46%) and African American (48.7%) than hispanic/other (5.3%) female veterans in the IBS symptom group (Chi-Square (df=2) = 7.84, p = 0.02). No significant differences were noted for age, marital status, education, smoking frequency, or BMI.
Table 1.
Sociodemographics for study participants overall, and when compared between those with and without Symptoms consistent with Irritable Bowel Syndrome (IBS), as mean scores (standard deviations) or percentages.
| Overall (n=337) | IBS (n=113) | No-IBS (n=224) | P-value | |
|---|---|---|---|---|
| Age, mean (SD) | 48.5 (12.1) | 46.9 (10.0) | 49.3 (12.9) | 0.08 |
| Ethnicity | 0.02 * | |||
| White | 39.9% | 46.0% | 36.8% | |
| African American | 48.2% | 48.7% | 48.0% | |
| Hispanic/Other | 11.9% | 5.3% | 15.2% | |
| Marital Status | 0.61 | |||
| Never Married | 18.5% | 16.8% | 19.3% | |
| Previously Married | 53.8% | 52.2% | 54.7% | |
| Currently Married | 27.7% | 31.0% | 26.0% | |
| Education | 0.07 | |||
| High School or Less | 14.1% | 8.0% | 17.2% | |
| Some College | 57.7% | 62.5% | 55.2% | |
| Completed College or More | 28.2% | 29.5% | 27.6% | |
| Smoking Frequency | 0.63 | |||
| Non-smoker | 71.2% | 67.9% | 72.9% | |
| Less than Daily | 7.8% | 8.9% | 7.2% | |
| Daily | 21.0% | 23.2% | 19.9% | |
| Body Mass Index, mean (SD) | 30.1 (6.2) | 30.2 (5.6) | 30.0 (6.4) | 0.75 |
IBS: Those with symptoms from the Bowel Disorder Questionnaire consistent with an Irritable Bowel Syndrome diagnosis.
No-IBS: Those without symptoms from the Bowel Disorder Questionnaire consistent with an Irritable Bowel Syndrome diagnosis.
Anxiety
the overall sample reported a mean BAI total score of 16.6 (sd=13.1) equating with mild severity. A larger proportion of participants with IBS symptoms reported anxiety than those without IBS (Chi-Square (df=3) = 28.5, p < .001). Please refer to Table 2 for details on the distribution of mild, moderate, and severe anxiety overall, and for the subset with IBS symptoms. The odds ratios and 95% confidence intervals are reported for the severity levels of the BAI, with the moderate and severe cases differing significantly from the reference no anxiety group.
Table 2.
The Beck Anxiety Inventory and Beck Depression Inventory total scores and the distribution of their severity ratings for the overall sample and for the subsamples with and without symptoms consistent with irritable bowel syndrome.
| Scale | Reference Score Range | N | % of Overall Sample | N | % of IBS Sample | N | % of No IBS Sample | OR, P-value (95% CI) |
|---|---|---|---|---|---|---|---|---|
| Total BAI Score | 0–63 | 332 | 103* | 219* | 1.06, <.001 (1.04–1.08) | |||
| None to Minimal | 0–7 | 103 | 31.0% | 18 | 15.9% | 85 | 38.8% | Reference group |
| Mild | 8–15 | 76 | 22.9% | 21 | 18.6% | 55 | 25.1% | 1.77, =.119 (0.86–3.65) |
| Moderate | 16–25 | 77 | 23.2% | 35 | 31.0% | 42 | 19.2% | 3.87, <.001 (1.95–7.68) |
| Severe | 26–63 | 76 | 22.9% | 39 | 34.5% | 37 | 16.9% | 5.32, <.001 (2.66–10.63) |
| Total BDI Score | 0–63 | 333 | 113** | 220** | 1.04, <.001 (1.02–1.06) | |||
| None to Minimal | 0–13 | 171 | 51.4% | 40 | 35.4% | 131 | 59.5% | Reference group |
| Mild | 14–19 | 46 | 13.8% | 23 | 20.4% | 23 | 10.5% | 3.11, =.001 (1.55–6.21) |
| Moderate | 20–28 | 45 | 13.5% | 17 | 15.0% | 28 | 21.7% | 1.75, =.126 (0.86–3.58) |
| Severe | 29–63 | 71 | 21.3% | 33 | 29.2% | 38 | 17.3% | 3.28, <.001 (1.78–6.03) |
IBS: Those with symptoms from the Bowel Disorder Questionnaire consistent with an Irritable Bowel Syndrome diagnosis.
No IBS: Those without symptoms from the Bowel Disorder Questionnaire consistent with an Irritable Bowel Syndrome diagnosis.
BAI: Beck Anxiety Inventory total score
BDI: Beck Depression Inventory total score
: Participants with IBS symptoms reported anxiety than those without IBS symptoms (Chi-Square (df=3) = 28.5, p < .001).
: Participants with IBS symptoms reported more depression that those without IBS symptoms (Chi-Square (df=3) = 19.1, p < .001).
OR: Odds Ratio
95% CI: the 95% Confidence Interval for the Odds Ratio
Reference Group: This is the group each severity level for the BAI and BDI were respectively compared to for determination of the Odds Ratios and 95% Confidence Intervals.
Depression
the overall sample reported a mean BDI total score of 16.5 (sd=14.0) equating with mild severity. Participants with IBS symptoms reported more depression that those without IBS (Chi-Square (df=3) = 19.1, p < .001). Please refer to Table 2 for details on the distribution of mild, moderate, and severe depression overall, and for the subset with IBS symptoms. The odds ratios and 95% confidence intervals are reported for the association between IBS and the severity levels of the BDI, with the mild and severe cases differing significantly from the reference no depression group.
PTSD
the overall sample reported a mean Mississippi Scale for Combat Related PTSD score of 71.1 (sd=25.6). Female veterans meeting criteria for PTSD represented 51.0% (25 of 49) of female veterans with IBS symptoms, but only represented 30.9% (87 of 282) of female veterans without IBS symptoms (Chi-Square (df=1) = 7.6, p = .006).
IBSQOL
Female veterans with IBS symptoms scored significantly lower for the overall total score, as well as on 7 of the 8 subscales than those without IBS. The differences were both statistically and clinically significant (MCID ≥14). The Relationship subscale showed a statistically significant difference between groups, but did not surpass the MCID of 14.0 for clinical significance (Table 3).
Table 3.
HRQOL in women Veterans: Comparison of normalized SF-36V and IBSQOL scores between participants with and without IBS symptoms.
| Scale/Sub-scale | n | Mean (SD) No IBS | n | Mean (SD) IBS | Mean Difference | P-value |
|---|---|---|---|---|---|---|
| SF -36V | ||||||
| Physical Functioning | 213 | 40.5 (13.3) | 106 | 38.0 (12.6) | − 2.5 | 0.11 |
| Role-Limitations: Physical | 213 | 29.8 (3.4) | 108 | 28.5 (2.9) | − 1.3 | 0.001 |
| Bodily Pain | 217 | 40.3 (12.9) | 109 | 33.3 (10.4) | − 7.0* | < 0.001 |
| General Health | 214 | 42.8 (12.7) | 109 | 37.8 (11.4) | − 5.0* | 0.001 |
| Vitality | 167 | 47.4 (12.8) | 72 | 39.6 (11.1) | − 7.8* | < 0.001 |
| Social Functioning | 213 | 39.6 (13.4) | 108 | 33.3 (13.3) | − 6.3* | < 0.001 |
| Role-Limitations: Emotional | 217 | 29.5 (3.5) | 109 | 28.0 (3.2) | − 1.5 | < 0.001 |
| Mental Health | 187 | 49.7 (14.3) | 95 | 43.7 (14.9) | − 6.0* | 0.001 |
| Physical Component Score | 149 | 41.2 (9.2) | 67 | 36.1 (9.7) | − 5.1* | < 0.001 |
| Mental Component Score | 149 | 44.4 (10.8) | 67 | 40.3 (10.2) | − 4.1 | 0.011 |
| IBSQOL | ||||||
| Dysphoria | 224 | 89.1 (15.2) | 113 | 71.0 (25.4) | −18.1* | < 0.001 |
| Interference with Activity | 224 | 87.3 (16.9) | 113 | 64.7 (27.4) | −22.6* | < 0.001 |
| Body Image | 224 | 80.4 (17.8) | 113 | 58.9 (25.1) | −21.5* | < 0.001 |
| Health Worries | 224 | 81.5 (16.9) | 113 | 63.4 (24.7) | −18.1* | < 0.001 |
| Food Avoidance | 224 | 78.4 (20.2) | 113 | 56.6 (29.5) | −21.8* | < 0.001 |
| Social Reaction | 224 | 86.8 (13.4) | 113 | 71.3 (24.7) | −15.5* | < 0.001 |
| Sexual | 224 | 82.8 (14.6) | 113 | 64.8 (28.0) | −18.0* | < 0.001 |
| Relationships | 224 | 85.0 (14.9) | 113 | 71.6 (24.9) | −13.4 | < 0.001 |
| Overall | 224 | 89.4 (14.9) | 113 | 69.7 (24.5) | −19.7* | < 0.001 |
IBS: Those with symptoms from the Bowel Disorder Questionnaire consistent with an Irritable Bowel Syndrome diagnosis.
No IBS: Those without symptoms from the Bowel Disorder Questionnaire consistent with an Irritable Bowel Syndrome diagnosis.
IBSQOL: Irritable Bowel Syndrome Quality of Life Questionnaire.
SF-36V: Medical Outcomes Study 36-Item Short-Form Health Survey-Veterans.
Difference: Calculated by subtracting the IBS negative mean score from the IBS positive mean score.
: The mean difference is greater than the MCID of at least 5.0 for the SF-36V or at least 14.0 for the IBSQOL signifying clinical significance.
SF-36V Comparison between IBS and no IBS symptoms
Female veterans with IBS symptoms scored significantly lower than female veterans without IBS symptoms on the physical component summary score and on 5 of 8 subscales: bodily pain, general health, vitality, social functioning, and mental health. The differences were also clinically meaningful by exceeding the MCID difference of at least 5.0 points (Table 3).
SF-36 Comparisons to US General Female Population
The study population had both statistically and clinically significant lower physical and mental component summary scores compared to the US general female population. These significantly reduced HRQOL scores were also maintained when the IBS symptom positive and IBS symptom negative subgroups were examined separately (Figure 1). Reference values for the US general female population are 49.12 for the PCS and 48.96 for the MCS. Our sample of female veterans with IBS symptoms had a SF-36 PCS score of 37.59 and a MCS score of 34.80, while those without IBS symptoms has a SF-36 PCS score of 42.55 and a MCS score of 39.21.
Figure 1. Comparison of HRQOL between female veterans in the study to the US General Female population using the SF-36*.
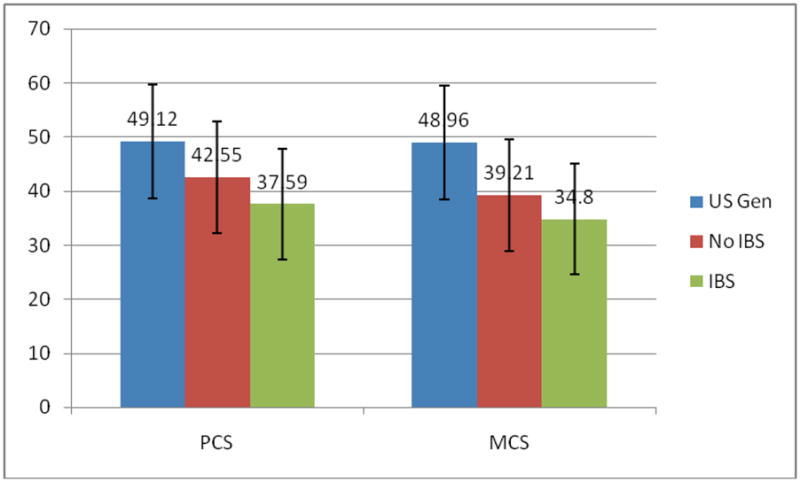
US Gen: The US General Female comparison population
SF-36: Medical Outcomes Study 36-Item Short-Form Health Survey
PCS: SF-36 Physical Component Summary Score, with an expected range of 20–58. MCS: SF-36 Mental Component Summary Score, with an expected range of 17–62. IBS: Those with symptoms from the Bowel Disorder Questionnaire consistent with an Irritable Bowel Syndrome diagnosis.
No IBS: Those without symptoms from the Bowel Disorder Questionnaire consistent with an Irritable Bowel Syndrome diagnosis.
*: The SF-36 is standardized differently than the SF-36V and will have different total scores than the SF-36V scores reported elsewhere in this manuscript.
Regression Analyses
We examined the relative contribution of several variables toward the SF-36V mental and physical component summary scores in two separate regression models. For the mental component score, the BDI total score was the predictor variable retained with the largest parameter estimate. However, the physical component score had several retained predictors (standardized betas between −0.139 and −0.199) including age, IBS, BAI total score, and total PTSD score. A third linear regression examining IBSQOL overall scores as an outcome variable found that the strongest predictor was the anxiety severity as measured by the BAI total score, closely followed by IBS symptom status. White race and older age were also associated with reduced IBSQOL scores (Table 4).
Table 4.
Results of linear regression models evaluating the potential determinants of HRQOL in a sample of female veterans, as measured by SF-36V summary scales (mental and physical), and the overall IBSQOL.
| SF-36V | P-Value | ||
|---|---|---|---|
| Mental Component Score | Adjusted R2 = 0.57 | F (3,206) = 92.38 | < 0.001 |
| Explanatory Variable | Parameter estimate | ||
| Age | 0.106 | 0.024 | |
| BAI | −0.191 | 0.010 | |
| BDI | −0.573 | < 0.001 | |
| SF-36V | P-Value | ||
| Physical Component Score | Adjusted R2 = 0.15 | F (4,205) = 10.52 | < 0.001 |
| Explanatory Variables | Parameter estimate | ||
| Age | −0.196 | 0.003 | |
| IBS Symptom Diagnosis Status | −0.139 | 0.043 | |
| BAI | −0.199 | 0.030 | |
| PTSD | −0.158 | 0.079 | |
| IBSQOL | P-Value | ||
| Overall Score | Adjusted R2 = 0.43 | F (4,315) = 60.79 | < 0.001 |
| Explanatory Variables | Parameter estimate | ||
| Age | −0.139 | 0.002 | |
| Ethnicity | 0.078 | 0.075 | |
| BAI | −0.488 | < 0.001 | |
| IBS Diagnosis | −0.304 | < 0.001 | |
IBS Symptom diagnosis Status: Irritable Bowel Syndrome status, positive or negative, based on symptoms from the Bowel Disorder Questionnaire consistent with an Irritable Bowel Syndrome diagnosis.
IBSQOL: Irritable Bowel Syndrome Quality of Life Questionnaire
SF-36V: Medical Outcomes Study 36-Item Short-Form Health Survey-Veteran
BAI: Beck Anxiety Inventory total score BDI: Beck Depression Inventory total score
PTSD: Posttraumatic Stress Disorder total score from the Mississippi Scale for Combat-Related PTSD
Ethnicity: This was coded as 0 = White, 1 = African American, 2 = Hispanic/Other. Education: This was coded as 0 = High School or less, 1 = Some College (1–3 years) or Technical School, 2 = College Graduate or Graduate School.
Finally, we evaluated potential explanatory variables for the 8 subscales scores of the IBSQOL (Table 5), and the 8 subscale scores of the SF-36V (Table 6). IBS symptom status was retained as a highly significant predictor variable for all 8 of the IBSQOL subscales, whereas it was retained for only the bodily pain and vitality subscales of SF-36V.
Table 5.
Potential explanatory factors for the eight IBSQOL subscales in a sample of female veterans. A separate linear regression was constructed for each subscale using backward elimination.
| Dysphoria | P-Value | ||
|---|---|---|---|
| Adjusted R2 = 0.39 | F (4,315) = 52.44 | < 0.001 | |
| Retained Explanatory Variables | Parameter estimate | ||
| Age | −0.207 | < 0.001 | |
| IBS Symptom Diagnosis Status | −0.280 | < 0.001 | |
| BAI | −0.403 | < 0.001 | |
| PTSD | −0.111 | = 0.065 | |
| Interference with Activity | P-Value | ||
| Adjusted R2 = 0.39 | F (3,316) = 69.87 | < 0.001 | |
| Retained Explanatory Variables | Parameter estimate | ||
| Age | −0.172 | < 0.001 | |
| IBS Symptom Diagnosis Status | −0.342 | < 0.001 | |
| BAI | −0.431 | < 0.001 | |
| Body Image | P-Value | ||
| Adjusted R2 = 0.38 | F (4,315) = 50.20 | < 0.001 | |
| Retained Explanatory Variables | Parameter estimate | ||
| Age | −0.079 | = 0.085 | |
| Ethnicity | +0.092 | = 0.044 | |
| IBS Symptom Diagnosis Status | −0.312 | < 0.001 | |
| BAI | −0.441 | < 0.001 | |
| Health Worry | P-Value | ||
| Adjusted R2 = 0.33 | F (3,316) = 53.89 | < 0.001 | |
| Retained Explanatory Variables | Parameter estimate | ||
| Age | −0.159 | = 0.001 | |
| IBS Symptom Diagnosis Status | −0.300 | < 0.001 | |
| BAI | −0.411 | < 0.001 | |
| Food Avoidance | P-Value | ||
| Adjusted R2 = 0.27 | F (4,315) = 30.99 | < 0.001 | |
| Retained Explanatory Variables | Parameter estimate | ||
| Age | −0.134 | = 0.007 | |
| IBS Symptom Diagnosis Status | −0.314 | < 0.001 | |
| BAI | −0.260 | < 0.001 | |
| PTSD | −0.115 | = 0.082 | |
| Social Reactions | P-Value | ||
| Adjusted R2 = 0.36 | F (3,316) = 59.41 | < 0.001 | |
| Retained Explanatory Variables | Parameter estimate | ||
| Age | −0.104 | = 0.023 | |
| IBS Symptom Diagnosis Status | −0.248 | < 0.001 | |
| BAI | −0.478 | < 0.001 | |
| Sexual | P-Value | ||
| Adjusted R2 = 0.30 | F (3,316) = 46.77 | < 0.001 | |
| Retained Explanatory Variables | Parameter estimate | ||
| Ethnicity | +0.097 | = 0.042 | |
| IBS Symptom Diagnosis Status | −0.276 | < 0.001 | |
| BAI | −0.386 | < 0.001 | |
| Relationships | P-Value | ||
| Adjusted R2 = 0.33 | F (4,315) = 40.46 | < 0.001 | |
| Retained Explanatory Variables | Parameter estimate | ||
| Age | −0.118 | = 0.013 | |
| Ethnicity | +0.114 | = 0.016 | |
| IBS Symptom Diagnosis Status | −0.116 | = 0.001 | |
| BAI | −0.493 | < 0.001 | |
IBS Symptom diagnosis Status: Irritable Bowel Syndrome status, positive or negative, based on symptoms from the Bowel Disorder Questionnaire consistent with an Irritable Bowel Syndrome diagnosis.
IBSQOL: Irritable Bowel Syndrome Quality of Life Questionnaire
BAI: Beck Anxiety Inventory total score
BDI: Beck Depression Inventory total score
PTSD: Posttraumatic Stress Disorder total score from the Mississippi Scale for Combat-Related PTSD
Ethnicity: This was coded as 0 = White, 1 = African American, 2 = Hispanic/Other.
Table 6.
The adjusted r-square, F-statistic, and the standardized betas for the retained explanatory factors for the final backwards stepwise linear regression models, investigating the eight SF-36V subscales in a sample of female veterans.
| Physical Functioning | P-Value | ||
|---|---|---|---|
| Adjusted R2 = 0.25 | F (4,300) = 26.72 | < 0.001 | |
| Retained Explanatory Variables | Parameter estimate | ||
| Age | −0.297 | < 0.001 | |
| Body Mass Index | −0.105 | = 0.037 | |
| BAI | −0.297 | < 0.001 | |
| BDI | −0.173 | = 0.026 | |
| Role Physical | P-Value | ||
| Adjusted R2 = 0.29 | F (3,304) = 42.97 | < 0.001 | |
| Retained Explanatory Variables | Parameter estimate | ||
| Age | −0.153 | = 0.002 | |
| BAI | −0.328 | < 0.001 | |
| BDI | −0.253 | = 0.001 | |
| Body Pain | P-Value | ||
| Adjusted R2 = 0.29 | F (4,307) = 33.13 | < 0.001 | |
| Retained Explanatory Variables | Parameter estimate | ||
| Age | −0.126 | = 0.010 | |
| IBS Symptom Diagnosis Status | −0.105 | = 0.039 | |
| BAI | −0.379 | < 0.001 | |
| BDI | −0.158 | = 0.037 | |
| General Health | P-Value | ||
| Adjusted R2 = 0.41 | F (5,304) = 43.09 | < 0.001 | |
| Retained Explanatory Variables | Parameter estimate | ||
| Age | −0.162 | = 0.001 | |
| Marital Status | +0.079 | = 0.080 | |
| BAI | −0.359 | < 0.001 | |
| BDI | −0.177 | = 0.017 | |
| PTSD | −0.165 | = 0.011 | |
| Vitality | P-Value | ||
| Adjusted R2 = 0.41 | F (3,227) = 54.56 | < 0.001 | |
| Retained Explanatory Variables | Parameter estimate | ||
| Body Mass Index | −0.144 | = 0.005 | |
| IBS Symptom Diagnosis Status | −0.096 | = 0.070 | |
| BDI | −0.598 | < 0.001 | |
| Social Functioning | P-Value | ||
| Adjusted R2 = 0.59 | F (3,307) = 152.17 | < 0.001 | |
| Retained Explanatory Variables | Parameter estimate | ||
| BAI | −0.202 | = 0.001 | |
| BDI | −0.530 | < 0.001 | |
| PTSD | −0.103 | = 0.050 | |
| Emotional | P-Value | ||
| Adjusted R2 = 0.44 | F (3,308) = 81.08 | < 0.001 | |
| Retained Explanatory Variables | Parameter estimate | ||
| Education | −0.078 | = 0.068 | |
| BAI | −0.242 | < 0.001 | |
| BDI | −0.456 | < 0.001 | |
| Mental Health | P-Value | ||
| Adjusted R2 = 0.59 | F (3,296) = 133.66 | < 0.001 | |
| Retained Explanatory Variables | Parameter estimate | ||
| How Often Smoke | +0.079 | = 0.046 | |
| BAI | −0.221 | < 0.001 | |
| BDI | −0.577 | < 0.001 | |
IBS Symptom diagnosis Status: Irritable Bowel Syndrome status, positive or negative, based on symptoms from the Bowel Disorder Questionnaire consistent with an Irritable Bowel Syndrome diagnosis.
SF-36V: Medical Outcomes Study 36-Item Short-Form Health Survey-Veteran
BAI: Beck Anxiety Inventory total score
BDI: Beck Depression Inventory total score
PTSD: Posttraumatic Stress Disorder total score from the Mississippi Scale for Combat-Related PTSD
Ethnicity: This was coded as 0 = White, 1 = African American, 2 = Hispanic/Other. Marital Status: This was coded as 0 = currently married, 1 = previously married, 2 = never married.
Education: This was coded as 0 = High School or less, 1 = Some College (1–3 years) or Technical School, 2 = College Graduate or Graduate School.
How often smoke: This was coded as 0 = everyday, 1 = some days, 2 = never smoke.
Discussion
We have previously demonstrated women veterans who use the VA for primary care are at increased risk of having IBS symptoms (23). This is the first study to examine general and disease specific HRQOL measures in women veterans with and without IBS symptoms. IBS symptoms were associated with a significantly impaired HRQOL in female veterans compared to female veterans without IBS symptoms, and to the general female veteran population. The reduced HRQOL scores in IBS symptom positives were both statistically significant and clinically meaningful (a difference equal to or greater than the MCID). This was seen across most domains of disease specific QOL measures (IBSQOL), and less so with general QOL measures (SF-36V). Female veterans with IBS symptoms had lower scores than non-IBS symptomatic females for the overall IBSQOL and 7 of its 8 subscales, with the lowest scores on the food avoidance and body image subscales. On the other hand, the SF-36V in women veterans with IBS symptoms had lower physical but not mental component scores, and 5 of the 8 subscales: bodily pain, general health, vitality, social functioning, and mental health. This differs slightly from Afendy et al. (29) who noted differences in physical functioning and role functioning but not in social functioning, whereas the rest of the findings with regards to bodily pain, general health, vitality, and mental health were similar to our study.
These results support prior findings on IBS and HRQOL, and extend them to the women veterans who use the VA healthcare system. Previous studies have shown that IBS patients have impaired HRQOL (26, 28, 29), as well as high burden of psychological factors (7–12, 23). The findings also support prior work showing a positive association between IBS symptoms and each of depression (7, 30–33), and anxiety (29, 33–37). This finding supports the underlying reason, the presence of anxiety or depression, why prior reports showing antidepressants and psychological treatments are beneficial in IBS (25). While PTSD has previously been noted to be associated with IBS (16), it was retained in only three of the ten SF-36 models and two of the eight IBSQOL models. Four of these five models all dealt with physical issues (SF-36 PCS and General Health, IBSQOL Dysphoria and Food Avoidance subscales), with one related to psychological issues (SF-36 Social Functioning. However, in all five instances PTSD had the third or fourth lowest parameter estimate in the model indicating, while explanatory, it was not the dominant two factors in the model. In all five of these cases the BAI total score was more explanatory than the PTSD total score, while in two cases both the BAI and BDI total scores were more explanatory. Colliniarity diagnostics showed that PTSD was not collinear with either the BAI or BDI (or IBS symptom diagnostic status when retained) for any of these 5 models suggesting that the BAI and BDI were in fact evaluating different conceptual factors than the PTSD questionnaire.
The study indicates that female veterans who utilize the VA healthcare system have lower physical and mental HRQOL scores than the US general female population, regardless of their IBS symptom status. While the reasons for these findings are not known, female veterans are exposed to several types of mental and physical trauma, including sexual trauma, which has been reported to occur at prevalence of 23–40% (56–59).
These results further highlight the importance of accounting for co-morbid mental health conditions, particularly anxiety and depression, when planning treatment for IBS. Irrespective of IBS symptom status, total depression score was the dominant contributing factor for SF-36V scores including the four mental component subscales and summary score with beta values in the regression model between −0.46 and −0.60. In contrast, total anxiety score was the major contributing factor for the SF-36V 4 sub-scales physical component scores. For IBSQOL, the dominant explanatory factors were presence of an IBS symptom diagnosis and a total anxiety score. In addition, older age was associated with four SF-36V physical subscales; these results are similar to those by Afendy et al. (29) except for the 4 mental subscales. This difference could be in part an artifact due to Afendy et al. not controlling for depression, or by our focus on IBS symptoms.
Our results highlight the importance of including disease-specific HRQOL measures, such as the IBSQOL when assessing HRQOL in IBS, rather than rely solely on general HRQOL measures such as the SF-36V. IBS symptom status was associated with significant reduction in only 2 of the 8 the subscale for the SF-36V, but in all 8 subscales of IBSQOL. IBS specific HRQOL measures are more sensitive in detecting small but important changes that might otherwise be missed by more general HRQOL measures.
A strength of this study is that we evaluated female veterans in a primary health care setting, rather than female veterans in gastrointestinal or mental health clinics. However, as few female veterans actually seek women’s health care in VA settings (4.3% of all veterans based on 2003 national data, 60), our findings may not be generalized to the broader population of women veterans.
Additional limitations include that IBS status was determined by self-report questionnaire, but not further confirmed by a normal endoscopy or by health care seeking behavior for IBS. Some participants with IBS symptoms may never clinically go on to develop IBS; as such we have refrained from directly labeling the symptomatic group IBS patients. The possibility exists of selection bias, as those not participating are unknown as to their IBS status and may have led to a tendency for those with IBS to participate, possibly skewing our observed rate of IBS. Further, our sample was mostly older females with an average age in their late 40’s, and as such may not be representative of younger or older populations. Additionally, as this was a cross-sectional sample of a woman’s health primary care clinic setting, there was limited capability to obtain full medical illness history and thus unknown medical co-morbidity. Finally, given the cross-sectional study design, no conclusions can be drawn as to direct causality between IBS symptom status, depression, or anxiety with the HRQOL scores.
In summary, female veterans with IBS symptoms had a lower mental and physical HRQOL when compared to those without IBS symptoms, and both groups had significantly lower scores than the general US female population, regardless of IBS symptom status. Depression and anxiety were important explanatory variables for HRQOL irrespective of IBS symptom status.
Acknowledgments
The research reported/outlined here was supported by the Department of Veterans Affairs, Veterans Health Administration, Health Services Research and Development Service, (project H-17978). This work was supported in part by the Houston VA HSR&D Center of Excellence (HFP90-020). This work was also supported in part by a grant from Novartis pharmaceuticals to Dr. El-Serag. The views expressed in this article are those of the author(s) and do not necessarily represent the views of the Department of Veterans Affairs. It was also supported by Public Health Service Grant DK56338, which funds the Texas Medical Center Digestive Disease Center.
References
- 1.Francis CY, Whorwell PH. The irritable bowel syndrome. Postgrad Med J. 1997;73:1–7. doi: 10.1136/pgmj.73.855.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Drossman DA, Whitehead WE, Camilleri M. Irritable bowel syndrome: a technical review for practice guideline development. Gastroenterology. 1997;112:2120–2137. doi: 10.1053/gast.1997.v112.agast972120. [DOI] [PubMed] [Google Scholar]
- 3.Hayee BH, Forgacs I. Psychological approach to managing irritable bowel syndrome. BMJ. 2007;334:1105–1109. doi: 10.1136/bmj.39199.679236.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gunnarsson J, Simren M. Peripheral factors in the pathophysiology of irritable bowel syndrome. Dig Liver Dis. 2009 Aug 7; doi: 10.1016/j.dld.2009.07.006. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 5.Camilleri M. Genetics and Irritable Bowel Syndrome: from genomics to intermediate phenotype and pharmacogenetics. Dig Dis Sci. 2009 Aug 5; doi: 10.1007/s10620-009-0903-4. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Herschbach P, Henrich G, von Rad M. Psychological factors in functional gastrointestinal disorders: characteristics of the disorder or of the illness behavior? Psychosom Med. 1999;61:148–153. doi: 10.1097/00006842-199903000-00005. [DOI] [PubMed] [Google Scholar]
- 8.Seres G, Kovacs Z, Kovacs A, Kerekgyarto O, et al. Different associations of health related quality of life with pain, psychological distress and coping strategies in patients with irritable bowel syndrome and inflammatory bowel disorder. J Clin Psychol Med Settings. 2008;15:287–295. doi: 10.1007/s10880-008-9132-9. [DOI] [PubMed] [Google Scholar]
- 9.Choung RS, Locke GR, 3rd, Zinsmeister AR, Schleck CD, Talley NJ. Psychosocial distress and somatic symptoms in community subjects with irritable bowel syndrome: a psychological component is the rule. Am J Gastroenterol. 2009;104:1772–1779. doi: 10.1038/ajg.2009.239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lee S, Wu J, Tsang A, Guo WJ, Sung J. Irritable bowel syndrome is strongly associated with generalized anxiety disorder: a community study. Aliment Pharmacol Ther. 2009;30:643–651. doi: 10.1111/j.1365-2036.2009.04074.x. [DOI] [PubMed] [Google Scholar]
- 11.Wilhlemson I. The role of psychosocial factors in gastrointestinal disorders. Gut. 2000;47(suppl IV):iv73–75. doi: 10.1136/gut.47.suppl_4.iv73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lea R, Whorwell PJ. Psychological influences on the irritable bowel syndrome. Minerva Med. 2004;95:443–450. [PubMed] [Google Scholar]
- 13.Goldzweig CL, Balekian TM, Rolon C, Yano EM, Shekelle PG. The state of women veterans’ health research. J Gen Intern Med. 2006;21:S82–S92. doi: 10.1111/j.1525-1497.2006.00380.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gardella C, Johnson KM, Dobie DJ, et al. Prevalence of hysterectomy and associated factors in women Veterans Affairs patients. J Reprod Med. 2005;50:166–172. [PubMed] [Google Scholar]
- 15.Johnson KM, Bradley KA, Bush K, Gardella C, et al. Frequency of mastalgia among women veterans: Association with psychiatric conditions and unexplained pain syndromes. J Gen Intern Med. 2006;21:S70–S75. doi: 10.1111/j.1525-1497.2006.00378.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dobie DC, Kivlahan DR, Maynard C, Bush KR, et al. Posttraumatic stress disorder in female veterans: Association with self-reported health problems and functional impairment. Arch Intern Med. 2004;164:394–400. doi: 10.1001/archinte.164.4.394. [DOI] [PubMed] [Google Scholar]
- 17.Gray GC, Reed RJ, Kaiser KS, Smith TC, Gastanaga VM. Self-reported symptoms and medical conditions among 11,868 Gulf War-era veterans. Am J Epidemiol. 2002;155:1033–1044. doi: 10.1093/aje/155.11.1033. [DOI] [PubMed] [Google Scholar]
- 18.Dunphy RC, Bridgewater L, Price DD, Robinson ME, et al. Visceral and cutaneous hypersensitivity in Person Gulf war veterans with chronic gastrointestinal symptoms. Pain. 2003;102:79–85. doi: 10.1016/s0304-3959(02)00342-1. [DOI] [PubMed] [Google Scholar]
- 19.Gray GC, Smith TC, Kang HK, Knoke JD. Are Gulf War veterans suffering war-related illnesses? Federal and civilian hospitalizations examined, June 1991 to December 1994. Am J Epidemiol. 2000;151:63–71. doi: 10.1093/oxfordjournals.aje.a010123. [DOI] [PubMed] [Google Scholar]
- 20.Sosteck MB, Jackson S, Linevsky JK, Schimmel EM, Fincke BG. High prevalence of chronic gastrointestinal symptoms in a National Guard Unit of Persian Gulf veterans. Am J Gastroenterol. 1996;91:2494–2497. [PubMed] [Google Scholar]
- 21.Hallman WK, Kipen HM, Diefenbach M, et al. Symptom patterns among Gulf War registry veterans. Am J Public Health. 2003;93:624–630. doi: 10.2105/ajph.93.4.624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ford JD, Campbell KA, Storzbach D, Binder LM, et al. Posttraumatic stress symptomotology is associated with unexplained illness attributed to Persian Gulf War military service. Psychosom Med. 2001;63:842–849. doi: 10.1097/00006842-200109000-00019. [DOI] [PubMed] [Google Scholar]
- 23.Savas LS, White DL, Wieman M, Dacis K, et al. Irritable bowel syndrome and dyspepsia among women veterans: prevalence and association with psychological distress. Ailment Pharmacol Ther. 2008;29:115–125. doi: 10.1111/j.1365-2036.2008.03847.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zijdenbos IL, de Wit NJ, van der Heijden GJ, Rubin G, Quartero AO. Psychological treatments for the management of irritable bowel syndrome. Cochrane Database Syst Rev. 2009;1:CD006442. doi: 10.1002/14651858.CD006442.pub2. [DOI] [PubMed] [Google Scholar]
- 25.Ford AC, Talley NJ, Schoenfeld PS, Quigley EM, Moayyedi P. Efficacy of antidepressants and psychological therapies in irritable bowel syndrome: systematic review and meta-analysis. Gut. 2009;58:367–378. doi: 10.1136/gut.2008.163162. [DOI] [PubMed] [Google Scholar]
- 26.Park JM, Choi MG, Kin YS, Choi CH, et al. Quality of life of patients with irritable bowel syndrome in Korea. Qual Life Res. 2009 Feb 27; doi: 10.1007/s11136-009-9461-7. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 27.Gralnek IM, Hays RD, Kilbourne A, Naliboff B, Mayer EA. The impact of irritable bowel syndrome on health-related quality of life. Gastroenterology. 2000;119:654–660. doi: 10.1053/gast.2000.16484. [DOI] [PubMed] [Google Scholar]
- 28.Halder SL, Locke GR, Talley NJ, Fett SL, et al. Impact of functional gastrointestinal disorders on health-related quality of life: a population-based case-control study. Aliment Pharmacol Ther. 2004;19:233–242. doi: 10.1111/j.0269-2813.2004.01807.x. [DOI] [PubMed] [Google Scholar]
- 29.Afendy A, Kallman JB, Stepanova M, et al. Predictors of health-related quality of life in patients with chronic liver disease. Aliment Pharmacol Ther. 2009;30:469–476. doi: 10.1111/j.1365-2036.2009.04061.x. [DOI] [PubMed] [Google Scholar]
- 30.Jones R, Latinovic R, Charlton J, Gulliford M. Physical and psychological co-morbidity in irritable bowel syndrome: a matched cohort study using the General Practice Research Database. Aliment Pharmacol Ther. 2006;24:879–886. doi: 10.1111/j.1365-2036.2006.03044.x. [DOI] [PubMed] [Google Scholar]
- 31.Cole JA, Rothman KJ, Cabral HJ, Zhang Y, Farraye FA. Migraine, fibromyalgia, and depression among people with IBS: a prevalence study. BMC Gastroenterology. 2006;6:26. doi: 10.1186/1471-230X-6-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lackner JM, Quigley BM, Blanchard EB. Depression and Abdominal Pain in IBS Patients: The Mediating Role of Catastrophizing. Psychosom Med. 2004;66:435–441. doi: 10.1097/01.psy.0000126195.82317.46. [DOI] [PubMed] [Google Scholar]
- 33.Walker EA, Gelfand AN, Gelfand MD, Katon WJ. Psychiatric Diagnoses, Sexual and Physical Victimization, and Disability in Patients with Irritable Bowel Syndrome or Inflammatory Bowel Disease. Psychol Med. 1995;25(6):1259–1268. doi: 10.1017/s0033291700033225. [DOI] [PubMed] [Google Scholar]
- 34.Schwarz SP, Blanchard EB, Berreman CF, et al. Psychological aspects of irritable bowel syndrome: comparisons with inflammatory bowel disease and nonpatient controls. Behav Res Ther. 1993;31:297–304. doi: 10.1016/0005-7967(93)90028-s. [DOI] [PubMed] [Google Scholar]
- 35.Drossman DA, Creed FH, Olden KW, Svedlund J, et al. Psychosocial aspects of the functional gastrointestinal disorders. Gut. 1999;45(Suppl 2):II25–II30. doi: 10.1136/gut.45.2008.ii25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kaplan DS, Masand PS, Gupta S. The relationship of irritable bowel syndrome (IBS) and panic disorder. Ann Clin Psychiatry. 1996;8(2):81–88. doi: 10.3109/10401239609148805. [DOI] [PubMed] [Google Scholar]
- 37.Culpepper L. Generalized anxiety disorder and medical illness. J Clin Psychiatry. 2009;70 (Suppl 2):20–24. doi: 10.4088/jcp.s.7002.04. [DOI] [PubMed] [Google Scholar]
- 38.Friedman MJ, Schnurr PP. The relationship between trauma, post-traumatic stress disorder, and physical health. In: Friedman MJ, Charney DS, Deutch AY, editors. Neurobiological and Clinical Consequences of Stress: From Normal Adaptation to PTSD. Philadelphia: Lippincott-Raven Publishers; 1995. pp. 507–524. [Google Scholar]
- 39.Talley NJ, Phillips SF, Wiltgen CM, Zinsmeister AR, Melton LJ., 3rd Assessment of functional gastrointestinal disease: the bowel disease questionnaire. Mayo Clin Proc. 1990 Nov;65(11):1456–79. doi: 10.1016/s0025-6196(12)62169-7. [DOI] [PubMed] [Google Scholar]
- 40.Longstreth GF, Thompson WG, Chey WD, Houghton LA, et al. Functional bowel disorders. Gastroenterology. 2006;130:1480–1491. doi: 10.1053/j.gastro.2005.11.061. [DOI] [PubMed] [Google Scholar]
- 41.Patrick DL, Drossman DA, Frederick IO. Users Manual, U.S. Version. University of Washington; Seattle, Washington: Jun, 1997. A Quality of Life measure for persons with Irritable Bowel Sydrome (IBS-QOL) [Google Scholar]
- 42.Drossman D, Morris CB, Hu Y, Toner BB, et al. Characterization of Health Related Quality of Life (HRQOL) for patients with functional bowel disorder (FBD) and its response to treatment. Am J Gastroenterology. 2007;102:1442–1453. doi: 10.1111/j.1572-0241.2007.01283.x. [DOI] [PubMed] [Google Scholar]
- 43.Ware JE, Jr, Sherbourne CD. The MOS 36-Item Short-Form Health Survey (SF-36): I. Conceptual framework and item selection. Med Care. 1992;30:473–483. [PubMed] [Google Scholar]
- 44.McHorney CA, Ware JE, Jr, Raczek AE. The MOS 36-Item Short-Form Health Survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med Care. 1993;31:247–263. doi: 10.1097/00005650-199303000-00006. [DOI] [PubMed] [Google Scholar]
- 45.Kazis LE, Miller DR, Clark J, et al. Health-related quality of life in patients served by the Department of Veterans Affairs: results from the Veterans Health Study. Arch Intern Med. 1998;158:626–32. doi: 10.1001/archinte.158.6.626. [DOI] [PubMed] [Google Scholar]
- 46.Angst F, Aeschlimann A, Stucki G. Smallest detectable and minimal clinically important differences of rehabilitation intervention with their implications for required sample sizes using WOMAC and SF-36 quality of life measurement instruments in patients with osteoarthritis of the lower extremities. Arthritis Care Res. 2001;45:384–391. doi: 10.1002/1529-0131(200108)45:4<384::AID-ART352>3.0.CO;2-0. [DOI] [PubMed] [Google Scholar]
- 47.Hays RD, Morales LS. The RAND-36 measure of health-related quality of life. Annals of Medicine. 2001;33:350–357. doi: 10.3109/07853890109002089. [DOI] [PubMed] [Google Scholar]
- 48.Keane TM, Caddell JM, Taylor KL. Mississippi Scale for Combat-Related Posttraumatic Stress Disorder: three studies in reliability and validity. J Consult Clin Psychol. 1988;56:85–90. doi: 10.1037//0022-006x.56.1.85. [DOI] [PubMed] [Google Scholar]
- 49.Beck AT, Steer RA, Brown GK. Manual for Beck Depression Inventory-II. San Antonio, TX: Psychological Corporation; 1996. [Google Scholar]
- 50.Arnau RC, Meagher MW, Norris MP, et al. Psychometric evaluation of the Beck Depression Inventory-II with primary care medical patients. Health Psychol. 2001;20:112–119. doi: 10.1037//0278-6133.20.2.112. [DOI] [PubMed] [Google Scholar]
- 51.Beck AT, Steer RA. Beck Anxiety Inventory: Manual. The Psychological Corporation; 1990. [Google Scholar]
- 52.Beck AT, Epstein N, Brown G, et al. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol. 1988;56:893–897. doi: 10.1037//0022-006x.56.6.893. [DOI] [PubMed] [Google Scholar]
- 53.Kabacoff RI, Segal DL, Hersen M, et al. Psychometric properties and diagnostic utility of the Beck Anxiety Inventory and the State-Trait Anxiety Inventory with older adult psychiatric outpatients. J Anxiety Disord. 1997;11:33–47. doi: 10.1016/s0887-6185(96)00033-3. [DOI] [PubMed] [Google Scholar]
- 54.Wetherell JL, Arean PA. Psychometric evaluation of the Beck Anxiety Inventory with older medical patients. Psychological Assessment. 1997;9:136–144. [Google Scholar]
- 55.Ware JE, Jr, Kosinski M, Dewey JE. How to Score Version 2 of the SF-36R Health Survey. Lincoln, RI: QualityMetric Incorporated; 2000. [Google Scholar]
- 56.Coyle BS, Wolan DL, Van Horn AS. The prevalence of physical and sexual abuse in women veterans seeking care at a Veterans Affairs Medical Center. Mil Med. 1996;161:588–593. [PubMed] [Google Scholar]
- 57.Hankin CS, Skinner KM, Sullivan LM, Miller DR, et al. Prevalence of depressive and alcohol abuse symptoms among women VA outpatients who report experiencing sexual assault while in the military. J Trauma Stress. 1999;12:601–612. doi: 10.1023/A:1024760900213. [DOI] [PubMed] [Google Scholar]
- 58.Sadler AG, Booth BM, Nielson D, Doebbeling BN. Health-related consequences of physical and sexual violence: women in the military. Obstet Gynecol. 2000;96:473–480. doi: 10.1016/s0029-7844(00)00919-4. [DOI] [PubMed] [Google Scholar]
- 59.Sadler AG, Booth BM, Cook BL, Doebbeling BN. Factors associated with women’s risk of rape in the military environment. Am J Ind Med. 2003;43:262–273. doi: 10.1002/ajim.10202. [DOI] [PubMed] [Google Scholar]
- 60.Kimmerling R, Gima K, Smith MW, Street A, Frayne S. The Veterans Health Administration and military sexual trauma. Am J Public Health. 2007;97:2160–2166. doi: 10.2105/AJPH.2006.092999. [DOI] [PMC free article] [PubMed] [Google Scholar]


