Abstract
The search for a ‘third’-generation smallpox vaccine has resulted in the development and characterization of several vaccine candidates. A significant barrier to acceptance is the absence of challenge models showing induction of correlates of protective immunity against variola virus. In this light, virus neutralization provides one of few experimental methods to show specific ‘in vitro’ activity of vaccines against variola virus. Here, we provide characterization of the ability of a modified vaccinia virus Ankara vaccine to induce variola virus-neutralizing antibodies, and we provide comparison with the neutralization elicited by standard Dryvax vaccination.
The current smallpox vaccine, which was used as a tool to eradicate smallpox by 1980, is a formulation of live, fully replicative vaccinia virus. Recent studies, using modern immunological and proteomic methods to evaluate the immune response, have characterized more fully the immune responses elicited by these historic smallpox vaccines that are believed to contribute to protection (Frey et al., 2002, 2003; Davies et al., 2005a, b, 2007, 2008; Pütz et al., 2005, 2006; Tscharke et al., 2005; Lawrence et al., 2007). These and other studies have shown that a combination of humoral and cellular (CD4 and CD8) factors are manifest in smallpox vaccine-provided protection. Successful vaccination correlates with laboratory demonstration of the development of a cytotoxic T-cell response, lymphocyte proliferation, vaccinia virus-specific gamma interferon production, neutralizing antibodies to both mature virus (MV) and additional enveloped infectious virus (EV) forms, and serological responses to whole virus, core virus and MV and EV surface proteins in ELISA (Viner & Isaacs, 2005; Davies et al., 2005a, b, 2007, 2008; Pütz et al., 2005, 2006). However, actual study data on the role of these vaccine-elicited responses in protection from challenge with human smallpox are not available. In animal-challenge models with surrogate (non-variola) orthopoxvirus species, a necessary factor is the humoral response (Panchanathan et al., 2008). This study examined the historic vaccine used in the USA (Dryvax) and evaluated the humoral neutralizing-antibody responses elicited against variola virus. Additionally, this study evaluated the immune response elicited by one of the more recently developed (Stickl et al., 1974; Meyer et al., 1991; Vollmar et al., 2006), replication-impaired, less reactogenic smallpox vaccines, modified vaccinia virus Ankara (MVA) (Antoine et al., 1998; Vollmar et al., 2006); in this study, IMVAMUNE was used. Less reactogenic smallpox vaccines are anticipated to have fewer overall adverse events, especially those associated with direct virus replication (such as eczema vaccinatum, contact transmission and secondary-site implantation), associated with their use (Lane & Goldstein, 2003). Analyses using variola virus as a substrate for in vitro viral immune response, or surrogate ‘efficacy’, provide additional information important for smallpox-vaccine evaluation (Fogg et al., 2007). This may be especially important in circumstances where the historic correlate of vaccination success, the ‘take’ or Jennerian pustule, is not elicited, as is observed with MVA.
In total, 124 sera from 55 of the 90 participants enrolled in a National Institutes of Health-funded smallpox-vaccine trial (DMID 02-017) were obtained and sent to the Centers for Disease Control and Prevention; 106 sera from 53 of these participants (Frey et al., 2007) were used to evaluate the dose and route of MVA (IMVAMUNE) compared with those of standard Dryvax. Experimentalists were blinded to the vaccination regimen, but unblinded to the time of collection of the sera, i.e. pre- or post-vaccination. Fourteen individuals received Dryvax vaccination, 26 received MVA by the subcutaneous route (MVA SC; 1×108 TCID50, two doses, 1 month apart) and 15 received MVA by the intramuscular route (MVA IM; 1×108 TCID50, two doses, 1 month apart). Paired sera collected prior to vaccine dose and at the times of ‘peak’ response, based on plaque reduction neutralization test (PRNT) data against either MVA or Dryvax (Frey et al., 2007), were evaluated by a variola (VAR) PRNT. Individuals' sera in the Dryvax arm were evaluated 28–30 days post-vaccination; individuals vaccinated with MVA were evaluated 14 days after the second SC or IM dose. Serological-response data from 18 sera were not included in the final analysis. Six of these sera were from two individuals who enrolled and were assigned randomly to receive Dryvax vaccination, but were excluded from receiving vaccination after the discovery of contraindications to vaccine. The remaining 12 sera, which were redundant pre-vaccination serum samples from individuals in the Dryvax arm of the trial, were also not included in the analysis.
VAR PRNT titres were evaluated by using a method adapted from that described previously (Newman et al., 2003). Briefly, duplicate twofold dilutions of sera were prepared in RPMI 1640 medium supplemented with 2 % fetal bovine serum and incubated at 35 °C overnight with variola virus strain Solaimen at final serum dilutions of 1 : 10–1 : 40 for pre-bleeds and 1 : 40–1 : 1280 for post-vaccination sera. Variola virus strain Solaimen, a Bangladesh isolate, was chosen as the assay strain because it is used frequently for virus analysis. As virus was diluted from a crude viral lysate stock, it was primarily an MV preparation and contained approximately six particles per p.f.u.; this ratio was calculated by using a quantitative PCR assay to evaluate genome number as a surrogate of particle number. Mock serum dilutions were used to quantify the ‘virus-only’ control. Positive (sera from previously vaccinated persons) and negative (Davies et al., 2007; Karem et al., 2005) serum controls were used to validate the assay. Vaccinia immune globulin (VIG), used as one of the positive controls, was used at dilutions of 1 : 1000–1 : 32 000 based on prior knowledge of vaccinia-neutralizing capacity. After overnight incubation, serum plus virus or control plus virus was added to BSC40 cell monolayers (derived from African green monkey kidney cells; ATCC) in a volume of 1 ml and, after a 1 h adsorption period, additional medium (1 ml) was applied. Plaques were allowed to develop over 72 h and were counted following crystal violet staining of cell monolayers.
Post-vaccination mean percentage plaque reductions for each of the vaccine treatment groups (Dryvax, MVA SC and MVA IM) were calculated at each serum dilution. Non-parametric statistics were used for comparisons between groups because the data were not distributed normally (Lehmann, 1975). The percentage plaque reductions were compared between vaccine treatment groups for each dilution by using a Wilcoxon rank-sum test. Linear regression was applied to a log-transformation of the serum dilutions per individual to facilitate linear interpolation of their actual 60 and 90 % PRNT titres. For those individuals who achieved 60 % neutralization beyond a 1 : 1280 dilution, a 60 % PRNT titre was extrapolated based on the six dilution points. These interpolated titres were compared between vaccine treatment groups by using a Wilcoxon rank-sum test. For further information, the geometric mean titres (GMTs) at 60 and 90 % neutralization were calculated for each vaccine treatment group, both pre- and post-vaccination. The proportions of vaccinees achieving 60 and 90 % neutralization post-vaccination at each dilution in the vaccine treatment groups were compared by using a Fisher's exact test (two-sided). Both four- and eightfold rises in 60 and 90 % PRNT titres were compared between treatment groups by using a Fisher's exact test (two-sided). A P-value of <0.05 was considered statistically significant.
Paired sera from 53 participants were analysed. From the Dryvax vaccination arm, 12 sera from time points prior to and 28–30 days post-primary vaccination were evaluated. Twenty-six individuals received MVA SC vaccination and 15 received MVA IM vaccination. In those individuals receiving MVA vaccination, neutralizing-antibody response was measured 14 days after the second dose of MVA. For positive-control sera, a formulation of VIG was used (Cangene, product no. 172, lot 1730403; 53 mg ml−1). All four experimentalists performing PRNTs obtained 60 % VAR PRNT titres at a 1 : 16 000 end point with VIG, and 90 % VAR PRNT titres at a 1 : 2000 end point with VIG. Two negative-control sera were used (Karem et al., 2005). With one negative-control serum, three of three experimentalists performing PRNTs obtained 60 % PRNT titres at a 1 : 20 end point and 90 % PRNT titres at a <1 : 10 dilution end point. With the other negative-control serum, two of three experimentalists obtained 60 % PRNT titres at a 1 : 20 end point and the other obtained the 60 % PRNT titre at a 1 : 10 end point; all three found the 90 % PRNT titre to occur at a <1 : 10 dilution end point.
At peak times post-vaccination, all participants exhibited antibody responses able to neutralize >60 % of the variola virus used per neutralization (mean±sd, 268±27 p.f.u.) at dilutions >1 : 40 (Supplementary Fig. S1, available in JGV Online). Participants vaccinated with the two-dose MVA SC or IM regimens had a greater capability to neutralize variola virus at all dilutions tested compared with those vaccinated once with Dryvax (Table 1); however, these differences were only statistically significant at the 1 : 40 dilutions (P=0.020).
Table 1.
Aggregate mean percentage plaque reductions at each dilution by vaccine treatment group
| Vaccine treatment | n | Dilution | |||||
|---|---|---|---|---|---|---|---|
| 1 : 40 | 1 : 80 | 1 : 160 | 1 : 320 | 1 : 640 | 1 : 1280 | ||
| MVA SC | 26 | 90.86* | 85.63 | 78.47 | 69.53 | 59.98 | 52.42 |
| Dryvax | 12 | 86.77 | 82.23 | 74.68 | 64.58 | 54.99 | 44.05 |
| MVA IM | 15 | 91.10* | 86.61 | 78.79 | 71.34 | 60.09 | 47.26 |
*MVA SC and IM vaccinees have a significantly greater capability to neutralize variola virus at a 1 : 40 dilution compared with Dryvax vaccinees (P=0.02).
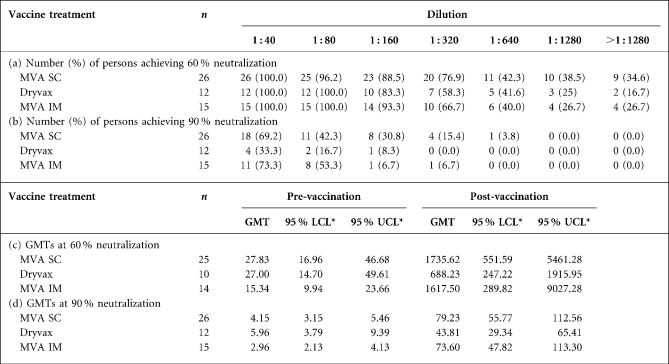
When the individuals at peak times post-vaccination are scored for the ability to demonstrate a 60 or 90 % VAR PRNT titre at various serum dilutions (Table 2a, b), the ability to neutralize variola virus elicited by the MVA regimens is as robust as that elicited by Dryvax. In fact, 90 % VAR PRNT titres at serum dilutions >1 : 160 are only seen in the MVA regimens; none were demonstrable at peak times post-Dryvax immunization at serum dilutions >1 : 160. With this sample dataset, the trend for a higher proportion of vaccinees achieving 90 % neutralization at each dilution in the two MVA regimen groups (SC and IM) compared with the Dryvax group approaches significance only at the 1 : 40 dilution (P=0.057 and 0.075, respectively).
Table 2.
Number of persons achieving 60 and 90 % neutralization at each dilution by vaccine treatment group, and geometric mean titres (GMTs) using log-linear transformation for 60 and 90 % neutralization at pre- and post-vaccination by vaccine treatment group
*LCL, Lower 95 % confidence limit; UCL, upper 95 % confidence limit.
Individual variability may also be important in the evaluation of vaccination responses. Some individuals' sera demonstrated pre-vaccination evidence of variola virus neutralization (Table 3). Two persons in the Dryvax arm and one each in the MVA SC and MVA IM arms had 60 % VAR PRNT titres ≥1 : 40 prior to vaccination. Therefore, we also evaluated individual rises in PRNT titre as another indication of vaccination response. We found a four- or eightfold rise in VAR PRNT end-point dilutions in the individual paired sera from participants in each of the vaccination study arms. End-point response levels of 60 and 90 % VAR PRNT titres were evaluated (Table 3). After excluding four individuals who had 60 % PRNT titres >1 : 40 pre-immunization (i.e. extrapolated titres could potentially bias the data analysis), Dryvax and MVA regimens appeared equivalent in the ability to achieve four- or eightfold rises in individual responses when using 60 % VAR PRNT titre as the outcome. However, when using 90 % VAR PRNT titre, MVA vaccination regimens appeared superior in the elicitation of four- or eightfold rises in titre (Table 3). A significantly higher proportion of MVA SC vaccinees (100 %) achieved a fourfold rise in 90 % VAR PRNT titre compared with Dryvax vaccinees (75 %) (P=0.03). The other comparisons (MVA IM versus Dryvax at four- and eightfold and MVA SC versus Dryvax at eightfold) approached statistical significance (P=0.06–0.08).
Table 3.
Number (%) of persons achieving a four- and eightfold increase at 60 and 90 % neutralization by vaccine treatment group
| Vaccine treatment | 60 % neutralization | 90 % neutralization | ||||
|---|---|---|---|---|---|---|
| n* | 4-fold increase | 8-fold increase | n | 4-fold increase | 8-fold increase | |
| MVA SC | 25 | 24 (96.0) | 22 (88.0) | 26 | 26 (100.0)† | 23 (88.5) |
| Dryvax | 10 | 10 (100.0) | 10 (100.0) | 12 | 9 (75.0)† | 7 (58.3) |
| MVA IM | 14 | 14 (100.0) | 13 (92.9) | 15 | 15 (100.0) | 14 (93.3) |
*Two persons in the Dryvax arm and one each in the MVA SC and MVA IM arms had 60 % VAR PRNT titres ≥1 : 40 prior to vaccination and were not included in the analysis.
†A statistically significantly higher proportion of MVA SC vaccinees achieved a fourfold rise compared with Dryvax vaccinees (P=0.03).
Finally, using log-linear transformation, GMTs were calculated at the 60 and 90 % VAR PRNT levels for each of the vaccination regimens (Table 2c, d). The four individuals who had a 60 % PRNT titre >1 : 40 pre-immunization were dropped from the 60 % variola virus neutralization GMT calculations. Although there is a trend towards higher ‘peak’ 60 % variola virus neutralization GMTs post-MVA regimen than post-Dryvax, this does not achieve statistical significance (Table 2c; Supplementary Table S1, available in JGV Online). However, in the more stringent 90 % variola virus neutralization GMT analysis, titres are significantly higher with each MVA regimen compared with those with Dryvax (Table 2d; Supplementary Table S1). Of note, there is a significant difference when comparing the pre-vaccination 60 % PRNT titres in the Dryvax versus MVA IM groups, with the Dryvax group being significantly higher (Table 2c; Supplementary Table S1).
Overall, this study suggests that the two-dose MVA vaccination regimens are as effective as the standard Dryvax vaccination regimen in eliciting variola virus-neutralizing responses, and some analyses suggest that the MVA regimens, especially using SC administration, may be superior. The reasons for these observations may be related to the fact that a two-dose vaccination regimen is used with MVA, with more highly antigenic inocula, and a one-dose regimen is used with Dryvax. Recent data suggest that the MVA regimen may be superior to the Dryvax regimen in elicitation of L1 and D8 responses (Davies et al., 2008); these are two of the MV proteins to which neutralizing responses have been ascribed. Future studies, using standardized methods and analyses, may be of interest to compare vaccinia and variola PRNT responses, and also to assess EV neutralization. These, in turn, may be used to provide data to assess whether bridging studies using variola, vaccinia or expressed variola proteins, or other surrogates for variola virus, are necessary or sufficient for evaluation of novel smallpox vaccines, which may not elicit the historic clinical correlate of success – the ‘take’.
Supplementary Material
Acknowledgments
The authors would like to acknowledge the assistance of Mark Challberg and Robert Johnson of DMID/NIAID for their assistance in facilitating this study. The findings and conclusions in this report are those of the authors and do not necessarily reflect the views of the CDC. Funding: N01-AI-25464.
Footnotes
A supplementary figure and table are available with the online version of this paper.
References
- Antoine, G., Scheiflinger, F., Dorner, F. & Falkner, F. G. (1998). The complete genomic sequence of the modified vaccinia Ankara strain: comparison with other orthopoxviruses. Virology 244, 365–396. [DOI] [PubMed] [Google Scholar]
- Davies, D. H., Liang, X., Hernandez, J. E., Randall, A., Hirst, S., Mu, Y., Romero, K. M., Nguyen, T. T., Kalantari-Dehaghi, M. & other authors (2005a). Profiling the humoral immune response to infection by using proteome microarrays: high-throughput vaccine and diagnostic antigen discovery. Proc Natl Acad Sci U S A 102, 547–552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davies, D. H., McCausland, M. M., Valdez, C., Huynh, D., Hernandez, J. E., Mu, Y., Hirst, S., Villarreal, L., Felgner, P. L., Crotty, S. & other authors (2005b). Vaccinia virus H3L envelope protein is a major target of neutralizing antibodies in humans and elicits protection against lethal challenge in mice. J Virol 79, 11724–11733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davies, D. H., Molina, D. M., Wrammert, J., Miller, J., Hirst, S., Mu, Y., Pablo, J., Unal, B., Nakajima-Sasaki, R. & other authors (2007). Proteome-wide analysis of the serological response to vaccinia and smallpox. Proteomics 7, 1678–1686. [DOI] [PubMed] [Google Scholar]
- Davies, D. H., Wyatt, L. S., Newman, F. K., Earl, P. L., Chun, S., Hernandez, J. E., Molina, D. M., Hirst, S., Moss, B. & other authors (2008). Antibody profiling by proteome microarray reveals the immunogenicity of the attenuated smallpox vaccine modified vaccinia virus Ankara is comparable to that of Dryvax. J Virol 82, 652–663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fogg, C. N., Americo, J. L., Lustig, S., Huggins, J. W., Smith, S. K., Damon, I., Resch, W., Earl, P. L., Klinman, D. M., Moss, B. & other authors (2007). Adjuvant-enhanced antibody responses to recombinant proteins correlates with protection of mice and monkeys to orthopoxvirus challenges. Vaccine 25, 2787–2799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frey, S. E., Newman, F. K., Cruz, J., Shelton, W. B., Tennant, J. M., Polach, T., Rothman, A. L., Kennedy, J. S., Wolff, M. & other authors (2002). Dose-related effects of smallpox vaccine. N Engl J Med 346, 1275–1280. [DOI] [PubMed] [Google Scholar]
- Frey, S. E., Newman, F. K., Yan, L., Lottenbach, K. R. & Belshe, R. B. (2003). Response to smallpox vaccine in persons immunized in the distant past. JAMA 289, 3295–3299. [DOI] [PubMed] [Google Scholar]
- Frey, S. E., Newman, F. K., Kennedy, J. S., Sobek, V., Ennis, F. A., Hill, H., Yan, L. K., Chaplin, P., Vollmar, J. & other authors (2007). Clinical and immunologic responses to multiple doses of IMVAMUNE (modified vaccinia Ankara) followed by Dryvax challenge. Vaccine 25, 8562–8573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karem, K. L., Reynolds, M., Braden, Z., Lou, G., Bernard, N., Patton, J. & Damon, I. K. (2005). Characterization of acute-phase humoral immunity to monkeypox: use of immunoglobulin M enzyme-linked immunosorbent assay for detection of monkeypox infection during the 2003 North American outbreak. Clin Diagn Lab Immunol 12, 867–872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lane, J. M. & Goldstein, J. (2003). Adverse events occurring after smallpox vaccination. Semin Pediatr Infect Dis 14, 189–195. [DOI] [PubMed] [Google Scholar]
- Lawrence, S. J., Lottenbach, K. R., Newman, F. K., Buller, R. M., Bellone, C. J., Chen, J. J., Cohen, G. H., Eisenberg, R. J., Belshe, R. B. & other authors (2007). Antibody responses to vaccinia membrane proteins after smallpox vaccination. J Infect Dis 196, 220–229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lehmann, E. L. (1975). Nonparametrics: Statistical Methods Based On Ranks. San Francisco: Holden-Day Inc.
- Meyer, H., Sutter, G. & Mayr, A. (1991). Mapping of deletions in the genome of the highly attenuated vaccinia virus MVA and their influence on virulence. J Gen Virol 72, 1031–1038. [DOI] [PubMed] [Google Scholar]
- Newman, F. K., Frey, S. E., Blevins, T. P., Mandava, M., Bonifacio, A., Jr, Yan, L. & Belshe, R. B. (2003). Improved assay to detect neutralizing antibody following vaccination with diluted or undiluted vaccinia (Dryvax) vaccine. J Clin Microbiol 41, 3154–3157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Panchanathan, V., Chaudhri, G. & Karupiah, G. (2008). Correlates of protective immunity in poxvirus infection: where does antibody stand? Immunol Cell Biol 86, 80–86. [DOI] [PubMed] [Google Scholar]
- Pütz, M. M., Alberini, I., Midgley, C. M., Manini, I., Montomoli, E. & Smith, G. L. (2005). Prevalence of antibodies to Vaccinia virus after smallpox vaccination in Italy. J Gen Virol 86, 2955–2960. [DOI] [PubMed] [Google Scholar]
- Pütz, M. M., Midgley, C. M., Law, M. & Smith, G. L. (2006). Quantification of antibody responses against multiple antigens of the two infectious forms of Vaccinia virus provides a benchmark for smallpox vaccination. Nat Med 12, 1310–1315. [DOI] [PubMed] [Google Scholar]
- Stickl, H., Hochstein-Mintzel, V., Mayr, A., Huber, H. C., Schafer, H. & Holzner, A. (1974). MVA vaccination against smallpox: clinical tests with an attenuated live vaccinia virus strain (MVA). Dtsch Med Wochenschr 99, 2386–2392 (in German). [DOI] [PubMed] [Google Scholar]
- Tscharke, D. C., Karupiah, G., Zhou, J., Palmore, T., Irvine, K. R., Haeryfar, S. M., Williams, S., Sidney, J., Sette, A. & other authors (2005). Identification of poxvirus CD8+ T cell determinants to enable rational design and characterization of smallpox vaccines. J Exp Med 201, 95–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Viner, K. M. & Isaacs, S. N. (2005). Activity of vaccinia virus-neutralizing antibody in the sera of smallpox vaccinees. Microbes Infect 7, 579–583. [DOI] [PubMed] [Google Scholar]
- Vollmar, J., Arndtz, N., Eckl, K. M., Thomsen, T., Petzold, B., Mateo, L., Schlereth, B., Handley, A., King, L. & other authors (2006). Safety and immunogenicity of IMVAMUNE, a promising candidate as a third generation smallpox vaccine. Vaccine 24, 2065–2070. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.